- Sterilisation and Infection Control Question and Answers
- Isolation Question and Answers
- Instruments Question and Answers
- Separation Question and Answers
- Matricing Question and Answers
- Dental Caries Question and Answers
- Pulp Protection Question and Answers
- Fundamentals of Cavity Preparation Question and Answers
- Amalgam Question and Answers
- Pin-Retained Restoration Question and Answers
- Direct Filling Gold Question and Answers
- Cast Metal Restorations Question and Answers
- Composite Restoration Question and Answers
- Glass Ionomer Cement Question and Answers
- Veneers Question and Answers
- Ceramics Question and Answers
- Bonding Question and Answers
- Non-Carious Lesion Question and Answers
- Dentinal Hypersensitivity Question and Answers
- Minimal Intervention Dentistry Question and Answers
- Conservative and Operative Dentistry Miscellaneous Question and Answers
 Sainavle
Sainavle
Oral Radiology Question and Answers
- Radiation Physics Question and Answers
- Properties of X Ray Question and Answers
- Production of X Ray Question and Answers
- Radiation Biology Question and Answers
- Radiation Protection Question and Answers
- X Ray Film & Accessories Question and Answers
- Film Processing Question and Answers
- Ideal Radiograph Question and Answers
- Faulty Radiographs Question and Answers

- Intraoral Radiographic Techniques Question and Answers
- Panoramic Radiography Question and Answers
- Occlusal Radiographs Question and Answers
- Object Localisation Techniques Question and Answers
- Specialized Radiographic Techniques Question and Answers
- Normal Anatomic Structures Question and Answers
- Periapical Radiolucency and Radiopacity Question and Answers
- Radiographic Interpretations Question and Answers
- Oral Radiology Miscellaneous Question and Answers
Oral Medicine Question and Answers
- Investigations Question and Answers
- Red & White Lesions Question and Answers
- Dermatological Diseases Question and Answers
- Infections Question and Answers
- Oral Medicine Infections Of Oral Cavity Short Essays
- Developmental Disorders Question and Answers
- Salivary Glands Question and Answers
- Orofacial pain Long and Short Essays
- Temporomandibular Joint Question and Answers
- Cysts Question and Answers
- Tumours Question and Answers
- Pulpal Diseases Question and Answers
- Periodontal Disease Question and Answers
- Bone Disorders Question and Answers
- Blood Disorders Question and Answers
- Bacterial Infections Question and Answers
- Herpangina In Adults Question and Answers
- Oral Medicine Aids Question And Answers
- Oral Medicine Specific Systemic Short Essay Question And Answers
- Endocrine Disorders Question and Answers
- Syndromes Question and Answers
- Antiviral Drugs Classification Question and Answers
Oral Pathology Question and Answers
- Development Disturbances Oral and Paraoral Structures Essay Question And Answers
- Benign and Malignant Tumours of the Oral Cavity Essay Question And Answers
- Tumours of Salivary Glands Essay Question And Answers
- Cysts and Tumours of Odontogenic Origin Essay Question And Answers
- Bacterial Infections of Oral Cavity Essay Question And Answers
- Viral Infections of Oral Cavity Essay Question And Answers
- Mycotic Infections of Oral Cavity Essay Question And Answers
- Diseases of Periodontium Question and Answers
- Dental Caries Essay Question And Answers
- Diseases of Pulp and Periapical Tissues Essay Question And Answers

- Spread of Oral Infections Essay Question And Answers
- Physical and Chemical Injuries of Oral Cavity Essay Question And Answers
- Regressive Alterations of the Teeth Essay Question And Answers
- Healing of the Oral Wounds Essay Question And Answers
- Oral Aspects of Metabolic Diseases Essay Question And Answers
- Allergic & Immunological Diseases of Oral Cavity Essay Question And Answers
- Diseases of Bone and Joints Essay Question And Answers
- Diseases of Blood and Blood – Formal Organs Essay Question And Answers
- Diseases of the Skin Essay Question And Answers
- Diseases of Nerves and muscles Essay Question And Answers
- Oral Pathology Miscellaneous Essay Question And Answers
General Surgery Question and Answers
- General Principles Of Operative Surgery Essay Question And Answers
- Wound Sinus And Fistula Notes Important Essay Question And Answers
- Bacterial Infections Question and Answers
- Hemorrhage, Shock and blood Transfusion Question and Answers
- Diseases of the Arteries, Veins and Lymphatic System Question and Answers
- Burns, Skin Grafting and Flaps Question and Answers

- Cleft Lip and Cleft Palate Question and Answers
- Diseases Of Salivary Glands Short And Long Essay Question And Answers
- Diseases Of The Nervous System Short Essay Question And Answers
- Diseases Of The Oral Cavity Short Essay Question And Answers
- Diseases of Thyroid and Parathyroid Glands Question and Answers
- Fractures – General Principles Question and Answers
- Infections and Diseases of the Larynx and Nasopharynx Question and Answers
- Tumour, Cyst and Neck-Swelling Question and Answers
- General Surgery Ulcers Short Essay Question And Answers
- General Surgery Miscellaneous Short And Long Essay Question And Answers
Developmental Disorders Short Essays
Oral Medicine Developmental Disorders Short Essays
Question 1. Dysgeusia.
Answer:
Dysgeusia
- Dysgeusia refers to a foul taste in the mouth
- Dysgeusia Causes:
- Genetic factors
- Smoking
- Lower esophageal sphincter abnormalities
- Defective gastric emptying
- Increased abdominal pressure
- Dietary behavior
Dysgeusia Clinical Features:
- It is more common in adults in the third decade of life
- Water brash is a very common complaint
- There is a sudden burst of salivation in the mouth
Dysgeusia Management:
- Patients should be encouraged to consume small frequent meals along with antacids instead of large meals
- They should be educated not to go to bed immediately after a heavy meal
- H2blockers: cimetidine 400 mg QID for 4 weeks
- Proton pump inhibitors: omeprazole 20 mg once daily for 4 weeks
- Half a teaspoon of baking soda is added to 250 ml of water, this solution is used as mouth rinse
Read And Learn More: Oral Medicine Question and Answers
Question 2. Regional odontodysplasia.
Answer:
Regional Odontodysplasia
Regional Odontodysplasia is an uncommon but unique non-hereditary developmental disturbance of teeth characterized by defective formation of enamel and dentin in addition to abnormal pulp and follicle calcification
Etiology:
- Local ischaemic changes in the tissue during odontogenesis
Regional Odontodysplasia Clinical Features:
- Both the dentition and are affected
- There is no sex predilection
- The maxilla is more affected than the mandible
- It frequently occurs unilaterally
- The centra! and lateral incisors arc rfTrrtrd
- They have a soft leathery surface
- They are yellowish-brown in color
Regional Odontodysplasia Radiographic Features:
- There is a marked decrease in radiodensity
- The enamel and dentin are very thin
- Pulp chambers are extremely large and open
- They often contain pulp stones
Question 3. Enamel hypoplasia.
Answer
Enamel Hypoplasia
Enamel Hypoplasia is an incomplete defective formation of organic enamel matrix
Enamel Hypoplasia Classification:
- Mild: There may be only a few small grooves, pits, and fissures on the enamel surface
- Moderate: They exhibit rows of deep pits arranged horizontally across the surface
- Severe: A considerable portion of enamel may be absent
Enamel Hypoplasia Types:
- Hypoplasia Due To Nutritional Deficiency
- Horizontal pitting occurs in rows on the teeth undergoing matrix formation at the time of dietary deficiency or during a febrile episode
- Pitting picks up stains and discoloration occurs
- Hypoplasia Due To Exanthematous Disease
- There is a temporary elevation of body temperature
- Ameloblasts may be adversely affected
- Syphilitic Hypoplasia
- It involves maxillary and mandibular permanent incisors and 1!’ molars
- Upper incisors are screw-shaped with a central notch called” Hutchinson’s incisors”
- Hypoplasia Due To Hypocalcemia
- Tetany induced by decreased level of calcium in the blood
- There is a defective formation of the enamel
- It is usually a pitting type
- Hypoplasia Due To Birth Injury
- Involves maxillary primary ln< Isom
- It is due to T.i r rlisturbarx or mrtahollf dhordet
- A wide band or line of enamel affects the primary truth of children associated with premature birth or low birth weight
- It may affect the process of amelogenesis
- Turner’s Hypoplasia
- Turner’s Hypoplasia results in Hue to focal enamel hypoplasia
- Tire trauma or the infection in the existing deciduous tooth may cause damage to the ameloblast cells forming the crown of the underlying permanent suc¬cessor
- The tooth affected in this process is called “Turner’s tooth”
Enamel Hypoplasia Types: Based On The Severity Of The Defect
- Slight pitting observed
- Smooth surface with pitted areas
- Grossly deformed with yellowish or brownish discoloration of the surface
- Dental fluorosis:
- It is due to disturbance in tootle formation caused by excessive intake of fluoride, during the formation period of dentition
- Tetracycline hypoplasia
- Tetracycline may be Inrorpocatcd in calcifying enamel matrix by the formation of tetracycline calcium orthophosphate complex
- Varying degree of hypocakificatlon of teeth exists
Enamel Hypoplasia Management:
- Restoration: to confine the area of involvement
- Crown: in severe hypoplasia
- Bleaching with 30% H2O2
- Calcium sucrose phosphate gel
- Desensitizing paste
Question 4. Anodontla.
Answer:
Anodontla Types:
- True: It is a congenital absence of teeth
- False: It is due to the extraction of teeth
- Pseudo: It is due to multiple unerupted teeth in the jaw
Anodontla Etiology:
- Genetic causes: Hereditary syndrome
- Radiation
Anodontla Clinical Features:
- Sex: it is common in women
- Site: it may be unilateral or bilateral
- Commonly missing teeth are 3rd molar, maxillary lateral incisor, maxillary or mandibular 2nd premolar
Anodontla Features:
- Microdontia
- Reduced alveolar development
- Increase freeway space
- Retained primary teeth
Anodontla Management:
- Orthodontic treatment: to correct malocclusion
- Prosthesis:
- Traditional fixed prostheses and resin-bonded bridges are given
Question 5. Glossopyrosis.
Answer:
Glossopyrosis
Glossopyrosis refers to a burning sensation in the tongue
Etiology:
- Local factors:
- Habits: excessive use of tobacco Dental causes- ill-fitted dentures
- Referred pain from infected teeth Local tongue disorders Electrogalvanic discharge
- Allergy to denture base materials
- Systemic factors
- Multiple myeloma
- Amyloidosis
- Pernicious anemia
- Diabetes
- Vitamin B deficiency
- Neurological disorders
- Trigeminal neuralgia
- Damage to the lingual nerve
Glossopyrosis Management:
- Removal of local cause
- Muscle relaxants
- Management of systemic causes
- Topical analgesics 0.5% of Diphenhydramine
- A mixture of 0.5% dyclonine or lidocaine with Diphenhydramine.

Question 6. Hairy tongue.
Answer:
Hairy Tongue Etiology:
- Formation of excess keratin causes elongation of the filiform papillae on the dorsal tongue
- May be infected with Candida albicans
Hairy Tongue Features:
- Elongation of the filiform papillae
- White to yellow
- Located on the posterior dorsal tongue
- Patients often have poor oral hygiene
- Patients may complain of bad taste
Hairy Tongue Treatment:
- Elimination of predisposing factors
- Cleaning the dorsal tongue with a soft toothbrush
- Treat Candidiasis if present
Question 7. Dentigerous imperfect.
Answer:
Dentigerous Imperfect
- Dentigerous Imperfect Classification:
- Shield Type 1: It occurs with osteogenesis imperfecta
- Shield Type 2: It is not associated with osteogenesis imperfect
- Shield Type 3: It has got shell teeth appearance and multiple pulp exposure
- Dentigerous Imperfect Clinical Features:
- Shield Type 1:
- Multiple bone fractures hyperextensible joints
- Blue sclera Progressive deafness
- Deciduous teeth are more affected
- The color of the teeth varies from blue to brownish-violet to yellowish brown
- Amber translucency of both the dentition
- Rapid attrition of the teeth is seen
- There is scalloping of DEJ
- In the incisor region the crowns are more squarish The posteriors are flatter
- Shield Type 2:
- Similar features but not associated with osteogenesis imperfect
- Shield Type 3:
- Both the dentition are affected
- The thickness of the enamel is normal
- Dentin is very thin
- Opalescent color, bell-shaped crown, and multiple pulp exposure
- Shield Type 1:
Question 8. Geographic tongue.
Answer:
Geographic Tongue
Geographic Tongue is defined as an irregularly shaped reddish area of depopulation and thinning of dorsal tongue epithelium which is surrounded by a narrow zone of regenerating papillae that are whiter than the surrounding tongue surface
Geographic Tongue Etiology:
- Immunological reaction
- Allergic reaction
- Emotional factors
- Hereditary factors
- Infections
- Nutritional deficiency
Geographic Tongue Classification:
- Type 1- Lesions are confined to the tongue
- Type 2- Lesions are also seen elsewhere in the mouth
- Type 3- Lesions on the tongue that are not typical and that may be accompanied by lesions elsewhere in the mouth
- Type 4- No tongue lesions are present but geographic areas are present in the mouth
Geographic Tongue Clinical Features:
- Age-5-84 years
- Sex- slight predilection to females
- Site- dorsal surface and lateral margins of the tongue
- Size- varies in diameter
Geographic Tongue Presentation
- It is asymptomatic
- The patient may complain of a burning sensation on spicy foods or intake of citrus fruits
- It appears as an erythematous, non-indurated, atrophic lesion
- Bordered by slightly elevated distinct rim
- Multiple areas of desquamation of filiform papilla in an irregular fashion are seen
- The central portion appears inflamed
- Fungiform papilla persists as elevated red dots
Geographic Tongue Differential Diagnosis:
- Psoriasis- skin lesions are present
- Lichen planus
Geographic Tongue Management:
- Topical application of anesthetic agents
- Balanced diet
- Elimination of irritants
- Psychological reassurance
- Topical corticosteroids
Question 9. Amelogenesis imperfecta.
Answer:
Amelogenesis Imperfecta
- Amelogenesis imperfecta is a developmental defect of the enamel with heterogenous etiology that affects the enamel of both the primary and permanent denti¬tion
Amelogenesis Imperfecta Etiology:
- Genetic mutation
- It is an autosomal dominant trait
Amelogenesis Imperfecta Clinical Features:
- It has a wide range of clinical appearance
- Enamel appears pitted with horizontal and vertical ridges
- There is defective maturation of the crystal structure
- Affected teeth are mottled, and opaque with white-brown yellowish discoloration
- They have enlarged pulp chambers
Amelogenesis Imperfecta Types:
- Hypocalcified type
- Hypomaturation type
- Hypoplastic type
Amelogenesis Imperfecta Treatment:
- Veneering or capping of teeth
Developmental Disturbances Of Oral And Paraoral Structures Short Question And Answers
Developmental Disturbances Of Oral And Paraoral Structures Short Question And Answers
Question 1. Gardener’s syndrome
Answer:
Gardener’s syndrome
It is a hereditary disorder characterized by colorectal polyps in association with various other lesions involving skin, eyes, teeth, and skeletal system
Gardener’s Syndrome Clinical Features:
- Multiple intestinal polyps
- Multiple osteomas of the skin, paranasal sinuses, and jaw
- Facial deformity
- Difficulty in mouth opening
- Multiple supernumerary teeth, impacted teeth, and odontomas
- Desmoid tumors of soft tissue and dermoid cysts of skin are present
- Pigmented lesion in ocular fundus
Gardener’s Syndrome Treatment:
- Prophylactic colectomy
- Surgical removal of osteomas and dermoid cyst
Question 2. Ramsay Hunt syndrome
Answer:
Ramsay Hunt syndrome
It is a zoster infection of geniculate ganglion with involvement of external ear and oral mucosa
Read And Learn More: Oral Pathology Questions and Answers
Ramsay Hunt syndrome Clinical Features:
- Facial paralysis
- The pain of external auditory meatus
- Pinna of the ear
- Vesicular eruption in the oral cavity and oropharynx
- Hoarseness of voice
- Tinnitus
- vertigo
Question 3. Melkersson-Rosenthal syndrome
Answer:
Melkersson-Rosenthal syndrome
- The melkersson-Rosenthal syndrome consists of
- Recurrent attacks of facial paralysis identical to Bell’s palsy
- Nonpitting, non-inflammatory painless edema of the face
- Chelitis granulomatosa
- Scrotal tongue
- Persistent unilateral edema of orbit and eyelid
Question 4. Hairy tongue
(or)
Black hairy tongue
Answer:
Black hairy tongue Etiology:
- Formation of excess keratin
- Infections- like candidiasis
Black hairy tongue Clinical Features:
- Elongation of filiform papillae
- Color- white to yellow
- Located on the posterior dorsal surface of the tongue
- Poor oral hygiene
- Bad taste in the mouth
Black hairy tongue Treatment:
- Elimination of predisposing factors
- Cleaning of the dorsal surface of the tongue with a soft toothbrush
- Treat candidiasis
Question 5. PeutJeghers syndrome
Answer:
PeutzJeghers syndrome Features:
- Recurrent abdominal pain due to familial intestinal polyps
- Cutaneous pigmentation in the perioral region
- Precocious puberty
- Gastrointestinal bleeding
- Pigmentation of buccal mucosa
Question 6. Xerostomia
Answer:
Xerostomia
It refers to the subjective sensation of dry mouth associated with salivary hypofunction
Xerostomia Etiology:
- Developmental- salivary aplasia
- Water or metabolic imbalance
- Iatrogenic causes
- Medications- antihistamines, decongestants, antidepressants, antihypertensives
- Radiation
Xerostomia Clinical Features:
- Reduction in salivary secretion
- Residual saliva is foamy or thick
- Fissured dorsum of the tongue
- Atrophy of filiform papilla
- Difficulty in mastication and swallowing
- Susceptibility to infection
- Dry mouth
- More prone to dental caries
Question 7. Turner’s hypoplasia
Answer:
Turner’s hypoplasia
- Turner’s hypoplasia is enamel hypoplasia occurring due to trauma or infection to the deciduous dentition
- Commonly affects incisors or premolars
- Periapical infection of deciduous teeth affects the ameloblastic layer of underlying permanent teeth
- As a result, permanent teeth get discolored or pitted
Question 8. Dilaceration
Answer:
Dilaceration
It refers to an angulation or sharp bend or curve anywhere along the root portion of the tooth
Dilaceration Clinical Features:
- Involves both dentition
- Seen at the coronal portion of the teeth
- The tooth looks like hook-shaped due to bending in the root
Treatment: - Extraction of involved teeth
Question 9. Talons cusp
Answer:
Talons cusp
It is an anomalous projection from the lingual aspect of the maxillary and mandibular permanent incisors
Talons cusp Clinical Features:
- It arises from the cingulum area of the tooth which extends to the incisal edge as a prominent T-shaped projection
- Asymptomatic
- Cosmetic problems
- Susceptible to caries
- Consist of normal-appearing enamel, dentin, and vital pulp tissue
Associated Syndrome:
Rubinstein Taybi syndrome
Talons cusp Treatment:
Restorative measures- to prevent caries
Question 10. Taurodontism
Answer:
Taurodontism
Taurodontism is a peculiar developmental condition in which the crown of the tooth is enlarged at the expense of its roots
Taurodontism Pathgenesis:
- It occurs due to failure of the Hertwig’s epithelial root sheath to invaginate at the proper horizontal level
Taurodontism Clinical Features:
- It involves both the sex
- It commonly affects multi-rooted permanent molar teeth and sometimes premolar
- It rarely occurs in primary dentition
- Common in Neanderthal men
- The affected tooth exhibits an elongated pulp chamber with rudimentary roots
- Teeth are usually rectangular with minimum constriction at the cervical area
- The furcation area of the teeth is more apically placed
- Teeth often have a greater apical-occlusal height
Question 11. Unerupted teeth
Answer:
Unerupted teeth
- It is an uncommon condition
- Causes delayed eruption of permanent teeth
Unerupted teeth Causes:
- Retained deciduous teeth
- Failure of eruption of permanent teeth
- Lack of eruptive force
- Cleidocranial dysplasia
Question 12. Amelogenesis imperfecta
Answer:
Amelogenesis imperfecta
It is a developmental anomaly characterized by defective enamel formation
Amelogenesis imperfecta Clinical Features:
- Affects both dentition
- Color- chalky white to yellow
- Prone to disintegration
- Open contact points due to loss of enamel
- Abraded occlusal surfaces and incisal edges
- Abrasion of dentin
- Cheesy consistency of enamel
- Alteration in the eruption process
- Anterior open bite
- Presence of grooves and wrinkles on enamel surfaces
- The presence of some white opaque flecks at incisal margins gives Snow-capped teeth appearance
Question 13. Shell teeth
Answer:
Shell teeth
- In type 3 dentinogenesis imperfect the dentin appears very thin and pulp chambers and root canals are extremely large
- Because of this, the teeth appear thin shells of enamel and dentin
- Thus it is described as shell teeth
- Seen in association with enamel aplasia
Question 14. Ghost Teeth
Answer:
Ghost Teeth
- It is a radiographic feature of regional odontodysplasia
- It involves both dentition
- Permanent teeth show delayed eruption and defective mineralization
- There is a marked decreased radiodensity
- Enamel and dentin are very thin
- Pulp chambers are extremely large and open
- This results in the ghostly appearance of the involved teeth
Question 15. Tooth ankylosis
Answer:
Tooth ankylosis
Fusion between the tooth and bone is called ankylosis
Tooth ankylosis Clinical Features:
- Asymptomatic
- Produces dull, muffled sound on percussion
- Loss of periodontal ligament
- Mild sclerosis of the bone
- Blending of bone with tooth root
- This leads to difficulty in the extraction
Question 16. Submerged teeth
Answer:
Submerged teeth
Submerged teeth are ankylosed deciduous teeth
Submerged teeth Causes:
- Trauma
- Infection
- Disturbed local metabolism
- Genetic factor
Submerged teeth Clinical Features:
- Commonly affects mandibular second molars
- It prevents the exfoliation of deciduous teeth and the eruption of their successor
- It is located below the occlusal level of other teeth
- There is a lack of physiological mobility in the teeth
- It imparts solid sound on percussion
Radiographic Features:
- Absence of periodontal ligament
- Blending of tooth root and bone
Question 17. Enameloma
Answer:
Enameloma
- The ectopic formation of enamel in the form of globule on the root surface is referred to as Enameloma
- It is usually located in the cementoenamel junction or the cervical third of the root surface
Enameloma Clinical features
- It appears as yellowish white, spherical, or globular structure adherent to the furcation areas of the root surface
- Diameter ranges from 1-3 mm
- More common in the roots of maxillary molars
- May produce localized periodontal destruction in molars
- Radiological features
- Appears as hemispherical dense radio parities projecting from the root surface.
Anatomy Question and Answers
Section 1: Upper Limb
- Upper Limb Introduction Question and Answers
- Pectoral Region Question and Answers
- Axilla Question and Answers
- Back of the Body Question and Answers
- Arm Question and Answers
- Antebrachium/Forearm Question and Answers
- Wrist and Hand Question and Answers
- Joints of Upper Limb Question and Answers
- Blood Supply and Lymphatic Drainage of Upper Limb Question and Answers
- Nerves of Upper Limb Question and Answers
Section 2 Lower Limb
- Lower Limb Introduction Question and Answers
- Front of Thigh Question and Answers
- Medial side of Thigh Question and Answers
- Gluteal Region Question and Answers
- Bank of Thigh Question and Answers
- Leg and Dorsum of Foot Question and Answers
- Sole of Foot Question and Answers
- Joints of Lower Limb Question and Answers
- Blood Supply and Lymphatic Drainage of Lower Limb Question and Answers
- Never Supply of Lower Limb Question and Answers

Section 3: Thorax
- Wall of Thorax and Thoracic Cavity Question and Answers
- Pleurae Question and Answers
- Lungs Question and Answers
- Mediastinum Question and Answers
- Pericardium and Heart Question and Answers
- Superior Vena Cava and Aorta Question and Answers
- Traches, Esophagus and Thoracic Duct Question and Answers
Section 4: Abdomen and Pelvis
- Anterior Abdominal Wall Question and Answers
- Male Genital Organs Question and Answers
- Abdominal Cavity and Peritoneum Question and Answers
- Stomach Question and Answers
- Small and Large Intestines Question and Answers
- Spleen, Pancreas and Liver Question and Answers
- Billary Apparatus Question and Answers
- Kidney, Ureter and Suprarenal Gland Question and Answers
- Posterior Abdominal Wall Question and Answers
- Urinary Bladder and Urethra Question and Answers
- Male and Female Reproductive Organs Question and Answers
- Perineum and True Pelvis Question and Answers
- Rectum and Anal Canal Question and Answers
- Large Blood Vessels of the Gut Question and Answers
Section 5: Head and Neck
- Scalp, Temple and Face Question and Answers
- Side of Neck Question and Answers
- Structures in Anterior Median Region of Neck Question and Answers
- Deep Structures of Neck Question and Answers
- Back of Neck Question and Answers
- Parotid Region Question and Answers
- Submandibular Region Question and Answers
- Temporal and Infratemporal Region Question and Answers
- Nose and Paranasal Sinuses Question and Answers
- Contents of Orbit and Eye Question and Answers
- Ear Question and Answers
- Oral Cavity and Tongue Question and Answers
- Pharynx Question and Answers
- Larynx Question and Answers
- Vertebral Canal and Contents Question and Answers
- Cranial Cavity Question and Answers
- Blood Vessels of Head and Neck Question and Answers
- Nerves of Head and Neck Question and Answers
Section 6: Neuroanatomy
- Cerebrospinal Fluid Question and Answers
- Spinal Cord Question and Answers
- Brainstem Question and Answers
- Celebellum and Fourth Ventricle Question and Answers
- Cerebrum Question and Answers
- Ventricles of Brain Question and Answers
- Blood Supply of Brain and Spinal Cord Question and Answers
- Cranial Nerves Question and Answers
Dental Caries Short Essays
Dental Caries
Question 1. Zinc polycarboxylate cement.
Answer:
Zinc polycarboxylate cement Composition:
1. Powder:
- Zinc oxide Basic ingredient
- Magnesium oxide
- Modifier
- Aids in sintering
- Bismuth and aluminum oxide occur in small amounts
- Stannous fluoride
- Increase strength
- Modifies setting time
- Imparts anti-cariogenic properties
2. Liquid:
- Polyacrylic acid
- The copolymer of acrylic acid with other unsaturated carboxylic acids
Zinc Polycarboxylate Cement Properties:
1. Physical Properties:
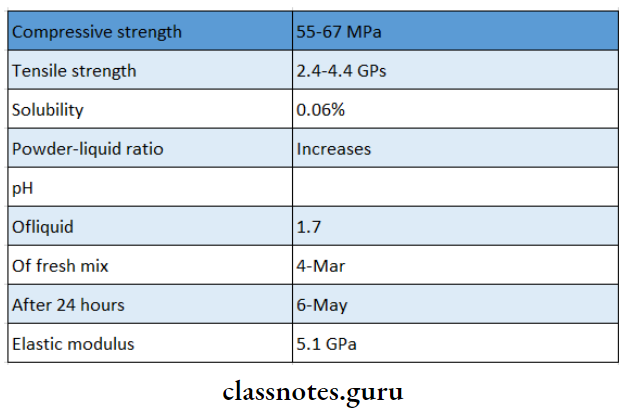
2. Biocompatibility:
- Mild pulpal response
3. Adhesion:
- Excellent adhesion
- Polyacrylic acid reacts with calcium ions via car¬boxyl groups on the surface of enamel and dentin
- The bond strength of enamel is greater
4. Optical Properties:
- Optical Properties are very opaque
5. Thermal Properties:
- Thermal Properties is a thermal insulator
Zinc Polycarboxylate Cement Uses:
- Cementation of restoration
- As bases and liners
- As intermediate restoration
- Luting of permanent restoration
- In orthodontics cementation of bands
- In endodontics as root canal filling material
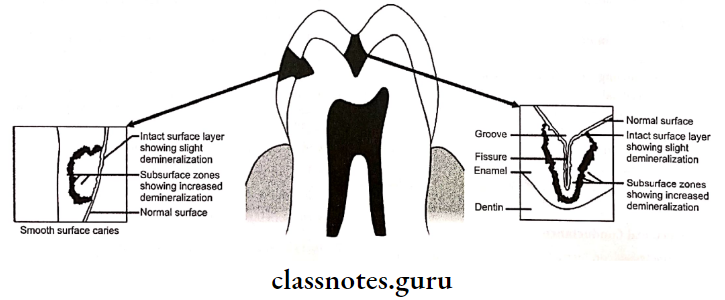
Question 2. Define and classify caries. Add a note on the diagnosis of caries.
Answer:
Caries Definition:
- Dental caries is defined as a multifactorial, transmissible, infectious oral disease caused primarily by the complex interaction of cariogenic oral flora with fermentable dietary carbohydrates on the tooth surface over time
Caries Classification:
1. According To Location
- Primary Caries
- Pit and fissure caries
- Smooth surface caries
- Root caries
- Secondary Caries
2. According To The Direction
- Forward caries
- Backward caries
3. According To The Extent
- Incipient caries
- Cavitated caries
4. According to Rate
- Acute caries
- Chronic caries
5. According To A Histological Depth Of Penetration
- Enamel caries
- Dentinal caries
Diagnosis Of Caries
1. Visual Tactile Examination:
- Visual Method:
- Cavitation
- Opacification
- Discoloration
- Surface roughness
- Tactile Method:
- Softness of enamel
- Catch obtained by an explorer
- Illumination:
- UV light creates decreased fluorescent in carious lesions as compared to healthy tissue
- Cavitation produces echoes of higher amplitude
2. Caries Detecting Dyes:
- Dyes For Enamel Caries:
- Procion Staining is irreversible
- Reacts with nitrogen and hydroxyl groups
- Calcein Bounds with calcium
- Zyglo ZL22 Visible by UV illumination
- Dyes For Dentin Caries:
- Infected and affected dentin layers are present
- Basic Fuschia in propylene glycol stains only the infected dentin
- Radiographic Methods:
- Requires 50% tooth destruction
- Seen as a radiolucent lesion
Caries Types
1. Caries Conventional:
- IOPA
- Bitewing For proximal caries
- Occlusal
- Xeroradiography
- Edge enhancement
2. Caries Advanced:
- Digital radiography
- Subtraction radiography
- RVG
3. Caries Electrical Conductance:
- Electrical conductivity is directly proportional to the amount of demineralization
4. Lasers:
Question 3. Methods of Diagnosis of Proximal Caries.
Answer:
1. Bitewing Radiograph:
- It includes occlusal surfaces of both arches in the same radiograph
- It must be differentiated from cervical bum out
- It describes the extent of the carious lesion
- 0 Normal
- 1 – Only enamel is involved
- 2- Caries extends upto DEJ/Dentinoenamel junction
- 3 – Caries involve the whole of the enamel and the outer half of the dentin
- 4 – Caries involve complete enamel and dentin
2. – Separation Of Teeth:
- With the help of separators, teeth are moved apart and viewed for carious lesions
3. Dental Floss:
- Dental floss is used through the proximal surface
- Fraying of it indicates the presence of a lesion
4. Transillumination:
- It is based on the refractory index between the carious and sound tooth
- Carious tooth appears as a dark shadow when compared to normal tooth
Question 4. Pit and fissure Caries.
Answer:
- The shape of pit and fissure make it more susceptible to caries
Pit And Fissure Caries Features:
- Initial Brown/Black in color
- Catch with an explorer
- DecalciFication of enamel
- Enamel involvement in the direction of the rod
- Shape Triangular, base towards DE
- Progress to the involvement of dentinal tubules
- Result in cavitation
- Undermining of enamel
Question 5. Root Caries/Cemental Caries.
Answer:
- Root Caries is a soft, progressive lesion that is found anywhere on the root surface that has lost its connective tissue attachment and is exposed to the environment
Root Caries Features:
- Periodontal attachment loss
- Soft, irregular lesion
- Round or oval in shape
- Irregular outline
- Common in males
- Common in mandibular molars
Root Caries Etiology:
- Streptococcus mutants
- Lactobacillus
- Actinobacillus
Root Caries Prevention:
- Plaque removal
- Diet modification
- Use of topical fluoride
- Soft tissue management
- Use of xylitol-containing chewing gum
Question 6. Roles of fluoride in caries prevention
Answer:
1. Increased Enamel Resistance/ Reduction In enamel Solubility
- Dental caries involves the dissolution of enamel by acid formation
- This dissolution is inhibited by fluoride as the fluoride forms fluorapatite which reduces enamel solubility
- Fluoride reduces enamel solubility also by promoting the precipitation of hydroxyapatite and phosphate mineral
- Fluoride inhibits demineralization by
- Reducing bacterial acid production
- Reducing equilibrium solubility of apatite
- By fluoridation of apatite crystal
2. Increased Rate Of Post-Eruptive Maturation
- Newly erupted teeth have hypomineralised areas and the enamel surface is also prone to dental caries
- Fluoride increases the rate of mineralization of these areas
- Organic material is also deposited over the enamel surface which increases its resistance to dental caries
3. Remineralization Of Incipient Lesions
- Fluoride enhances remineralization by the deposition of minerals into the damaged areas
- This reduces enamel solubility through the growth of crystals which are more resistant to acid
- Fluoride enhances remineralization from calcium phosphate solution by the formation of calcium fluoride which prevents hydroxyapatite crystal growth
4. Interference With Microorganisms
In Two Ways
- In High-Concentration Bacteriocidal
- By reducing plaque
- In low-concentration bacteriostatic
- Inhibits enzymes responsible for acid metabolism
5. Modification In Tooth Morphology
- If fluoride is ingested during tooth development it results in the formation of
- More caries-resistant tooth
- A tooth with smaller and shallow fissures
- Smaller diameter and cusp depth
- All these make them more self-cleansing
Question 7. Zones of enamel caries
Answer:
1. Zone 1 Translucent zone
- It is the deepest zone
- It is slightly more porous
- Contains 1% by volume
- Pores are larger than usual pores seen in normal enamel
- Dissolution of mineral occurs at the junction of prismatic and interprismatic enamel
2. Zone 2 Dark zone
- Located superficial to the translucent zone
- Excessive demineralization of enamel occurs
- It is narrow in rapidly advancing caries and wide in slowly advancing caries
- Contains 24% pore volume
- Pores are smaller than that of the translucent zone
- There is some degree of remineralization
3. Zone 3 Body Of The Lesion
- Present between dark zone and surface zone
- Represents the area of greatest demineralization
- Pore volume is between 525%
- Contains larger apatite crystals
- Reprecipitation of minerals occurs
- Dissolution of minerals occurs
- Lost minerals are replaced by unbound water and organic matters
4. Zone 4 Surface Zone
- Zone 4 Surface Zone remains unaffected
- Zone 4 Surface Zone is 40 pm thick
- Surface remineralization occurs due to the active precipitation of mineral ions
Question 8. Zones of dentinal caries.
Answer:
- Zone 1: Normal dentin
- Zone of fatty degeneration of odontoblast
- Represents thinner most layer of carious dentin
- No crystals are present in the lumen of tubules
- No bacteria present in tubules
- Intertubular dentin has normal collagen
Zone 2: Subtransparent dentin
- Zone of dentinal sclerosis characterized by deposition of calcium salts in dentinal tubules
- The superficial layer shows areas of demineralization and damage of odontoblastic processes
- Subtransparent dentin is capable of remineralization
- No bacteria is present in tubules
Zone 3: Transparent dentin
- Zone of decalcification of dentin, a narrow zone preceding bacterial invasion
- Transparent dentin is softer than normal dentin
- Large crystals are present within the lumen of dentinal tubules
- No bacteria is present in tubules
- Transparent dentin is capable of self-repair and remineralization
Zone 4: Turbid dentin
- Zone of bacteria] invasion of decalcified but intact dentin
- Widening and distortion of dentinal tubules
- Cannot undergo self-repair or remineralization
- Must be removed before restorative treatment
Zone 5: Infected dentin
- Zone of decomposed dentin
- Infected dentin is the outermost zone of carious dentin
- Characterized by complete destruction of dentinal tubules
- Areas of decomposition of dentin occur along the direction of dentinal tubules called liquefaction foci of Miller
- Transverse clefts are seen due to the decomposition of dentin
- Bacteria invade and destroy peri and intertubular dentin
Dental Plaque Short Question and Answers
Question 1. Specific plaque hypothesis.
Answer:
- The specific plaque hypothesis states that not all plaque is pathogenic and its pathogenicity depends on the presence of certain specific microbial pathogens in plaque
- Specific microorganisms responsible for periodontal diseases release certain damaging factors called virulence factors which lead to host tissue destruction
Example: A.a. contains causes aggressive periodontitis
Question 2. Define dental plaque.
Answer:
- It is soft deposits that form biofilm adhering to the tooth surface or other hard surface in the cavity including removable and fixed restoration
Read And Learn More: Periodontics Question and Answers
Question 3. Composition of dental plaque.
Answer:
1. Micro-organisms:
- Bacteria
- Mycoplasm
- Fungi
- Protozoa
- Virus
2. Intracellular matrix:
- Organic:
- Carbohydrates
- Glycoproteins
- Lipids
- Inorganic:
- Calcium
- Phosphorous
- Magnesium
- Potassium
- Sodium
Question 4. Difference between Supragingival and Subgin. It is for the identification of causative agents given Plaque.
Answer:
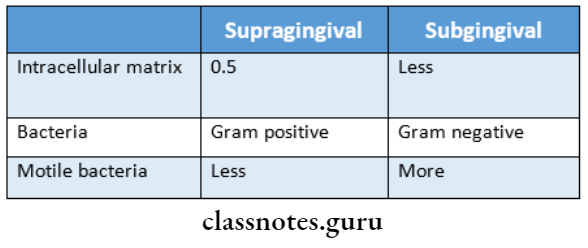
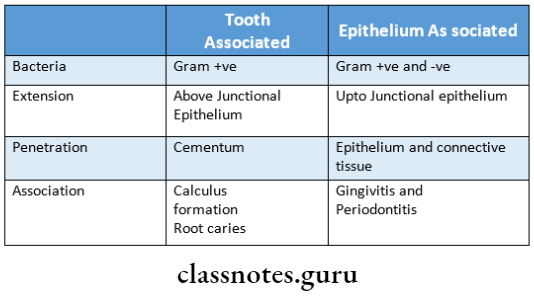
Question 5. Difference between Tooth associated and Epi- thelium-associated plaque.
Answer:
Question 6. Pellicle.
Answer:
Derived From:
- Components of saliva
- GCF
- Debris, bacterial, and host tissue cell products
Formed by: Selective adsorption of environment macromolecules
Functions:
- Acts as a protective barrier
- Lubricates surfaces to prevent tissue desiccation
- Provide substrate for bacterial attachment
Question 7. Socransky postulate.
Answer:
- It is for the identification of causative agents
- No. of etiologic organisms in the diseased site must be increased
- While it should be reduced in healthy sites
- If the etiologic organism is eliminated then disease pro-aggression ceases
- Presence of antibodies in organisms
- Presence of virulence factors
- In vitro, experiments should demonstrate the disease process
Question 8. Nonspecific Plaque Hypothesis.
Answer:
- It states that it is the total bulk of plaque that determines the pathogenicity rather than the individual species in it
- According to it. If a small amount of plaque is present then the products released by it can be neutralized by the host
- But if it is present in large quantity then it alters the host response
- It forms the basis of recent treatment and prevention modalities
Question 9. P. Gingivalis.
Answer:
- Porphyromonas gingivalis is a Gram-negative, anaerobic non-motile organism
- It is coccal to short rod shape
- It possesses fimbriae that facilitate adhesion and coag- aggregation
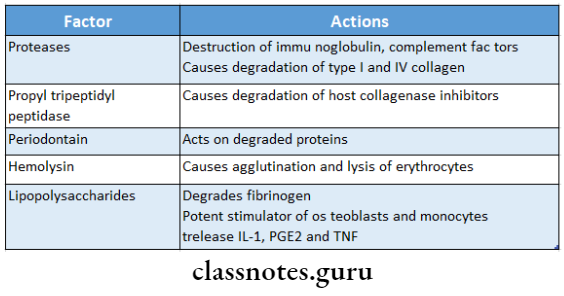
Virulence Factors:
Question 10. A.a. contains.
Answer:
- Actinobaillus actinomycetemcomitans is also known as aggregatibacter actinomycetemcomitans
- It is gram-negative, capnophilic,non-motile saccharolytic
- It occurs singly, in clumps, or in pair
- It is a small, short straight, or curved rod in shape
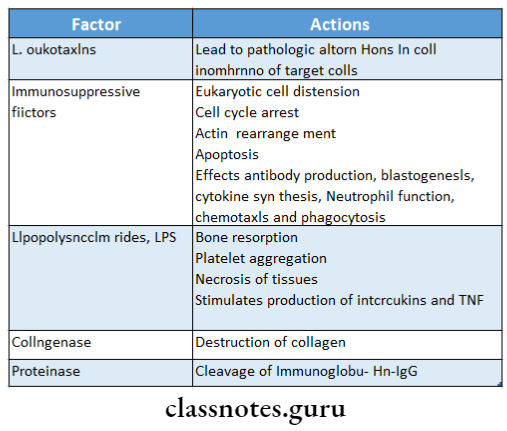
Virulence Factors:
Question 11. Name the stages of plaque formation.
Answer:
Stages Of Plaque Formation:
- Formation of pellicle on the tooth surface
- Initial adhesion and attachment of bacteria
- Colonization and plaque maturation
Question 12. Normal oral bacterial flora.
Answer:
- Normal bacterial flora associated with clinically healthy periodontium comprises of
- Gram-positive cocci
- Fusiform bacilli
- Motile rods
- Filaments
- Spirochaetes
Question 13. Coaggregation.
Answer:
- In the process of plaque formation, the bacterial adherence to one another is termed coaggregation
- In the early stages of plaque formation there is coaggre It leads to food impaction nation between gram-negative and gram-positive organisms such as F. nucleatum and A. viscous followed by coaggregation in later stages between gram-negative organisms, F.nucleatum, and P. gingivalis
Question 14. Spirochaetes.
Answer:
- Spirochaetes are corkscrew-like gram-negative anaerobic bacteria
- They are capable of immunosuppression
- They contain endotoxin that contributes to their path- Tends to accumulate on a gingival third of teeth genericity
- Treponema vincentii is responsible for necrotizing ulcerative gingivitis
- Increased levels of spirochetes occur in chronic and aggressive periodontitis
- Treponema pallidum is important in the pathogenesis of periodontal diseases
- A decrease in the levels of spirochaetes results in im- improvement in periodontal health
Question 15. Prevotella intermedia.
Answer:
- It is a Gram-negative, anaerobic organism
- It has short rods with rounded ends
- Possess fimbriae
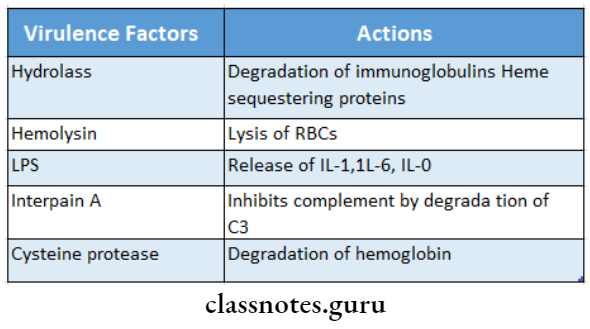
Virulence Factors:
Question 16. Plunger Cusps.
Answer:
- Cusps that tend to forcibly wedge food interproximal are called plunger cusps
- It leads to food impaction
- Further results in gingivitis, periodontitis, tooth mobility, and pocket formation
Question 17. Materia alba.
Answer:
- Yellow/grayish-white, soft, sticky deposit, less adherent
Composition:
- Micro-organisms, desquamated epithelial cells, leukocytes, a mixture of salivary proteins and lipids
They are capable of immunosuppression cytes, a mixture of salivary proteins and lipids - Clearly visible, flushed away easily with water
- Tends to accumulate on the gingival third of teeth
Question 18. Bacterial Adherence/Formation.
Answer:
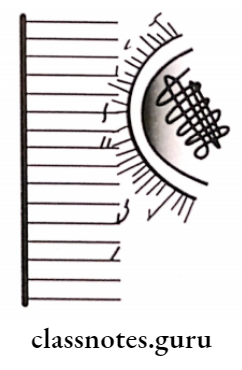
1. Via Electrostatic Interactions:
Negatively charged bacteria 11 calcium
↓↑
Negatively charged pellicle
2. Via Hydrophobic Interactions:
- Based on the fit of molecules of pellicle and plaque
- Lipoteichoic acid is responsible for this interaction by providing a long hydrophobic area
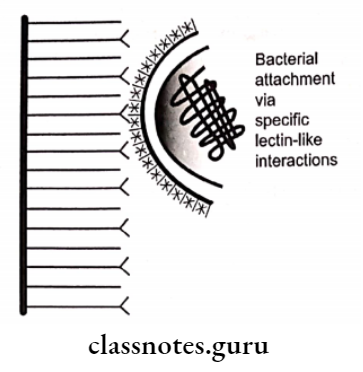
3. Via Lectin-like Substances:
- Lectin recognizes specific carbohydrates in the pellicle and becomes linked to it.
Question 19. Plaque Hypothesis.
Answer:
Non-Specific Plaque Hypothesis:
- States that the total bulk of plaque determines pathogenic- city rather than the species
- When only a small amount of plaque is present, it gets neutralized
- When a large amount of plaque is present, it causes disease
Specific Plaque Hypothesis:
- States that not all plaque is pathogenic and its path- genericity depends on the presence of certain specific pathogens in plaque
- Specific micro-organisms responsible for periodontal diseases release certain damaging factors
- This mediates the destruction of host tissue
Proof: Presence of A.a. contains in localized juvenile periodontitis
Question 20. Red complex
Answer:
- Secondary colonizers form red complex
- It consists of
- P. gingivalis
- T. denticola
- B. forsythias
- It is responsible for bleeding on probing
