Trauma From Occlusion Short Answers
Question 1. Primary and secondary trauma from occlusion.
Answer:
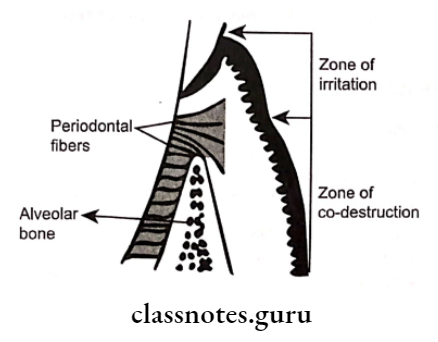
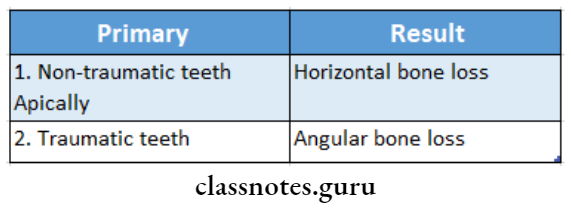
1. Primary:
- When trauma from occlusion results from alteration of occlusal forces, it results in primary trauma from occlusion
- It does not alter the level of connective tissue attachment
- It does not initiate pocket formation because su- parental gingival fibres are not affected which prevents apical immigration of junctional epithelium
2. Secondary:
- It is trauma from occlusion that results due to re- reduced ability of tissues to resist occlusal forces
- Adaptive capacity is impaired by bone loss resulting from marginal inflammation
- Reduces periodontal attachment
- Alters leverage on remaining tissues
Read And Learn More: Periodontics Question and Answers
Question 2. Lipping.
Answer:
- Excessive forces lead to the resorption of bone
- When bone is resorbed in such cases, the body attempts to reinforce trabeculae to form new bone
- This process is called buttressing
Types:
1. Central buttressing:
- In it, endosteal cells deposit new bone
- It restores bony trabeculae
- Reduces the size of bone marrow
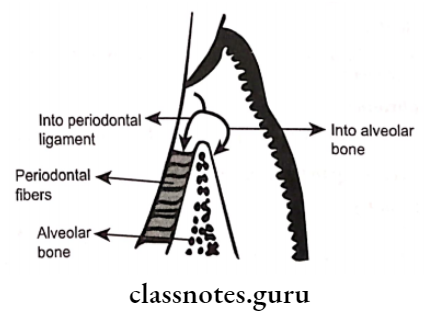
2. Peripheral buttressing:
- Occurs on facial and lingual surfaces of bone
- May produce shelflike thickening of the alveolar margin called lipping
- It is pronounced bulge in the contour of the facial or lingual bone
Question 3. Define trauma from occlusion.
Answer:
- When occlusal forces exceed the adaptive capacity of the periodontal tissues, the tissue injury results
- This resultant injury is termed trauma from occlusion
Question 4. Diagnosis of trauma from occlusion.
Answer:
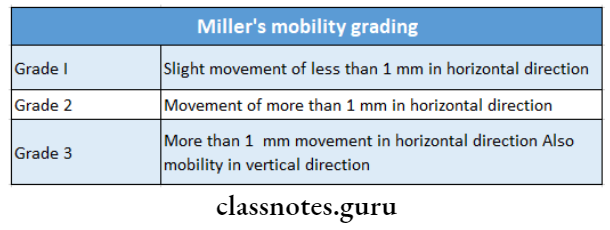
1. Fremitus test:
Procedure:
Ask the patient to contact the teeth together in the maximum intercuspal position
↓
Place dampened index finger over the buccal surface of maxillary teeth
↓
Examine the teeth which are displaced
Result:
- Class 1- Mild vibration
- Class 2- Easily palpable but no visible movements
- Class 3- Movements visible with the naked eye
2. Radiographic features:
- Increase in width of PDL space
- Thickening of lamina dura along lateral borders of root, apical and bifurcation areas
- Vertical bone loss
- Radiolucency occurs due to condensation of alveolar bone
- Root resorption
Question 5. Causes and changes produced by primary trauma from occlusion.
Answer:
Causes:
- High filling restoration
- Prosthetic replacement
- Drifting movement or extrusion of teeth
- Unreplaced missing teeth
- Orthodontic movement of teeth
Changes Produced:
- Does not alter the level of connective tissue attachment
- Do not initiate the pocket formation
- As suprarenal fibres are not affected it prevents apical migration of junctional epithelium
Question 6. Define acute and chronic trauma from occlusion
Answer:
1. Acute trauma from occlusion:
- It results from an abrupt occlusal impact such as that produced by biting on a hard object
2. Chronic trauma from occlusion:
- It develops from gradual changes in occlusion produced by tooth wear due to drifting movement and extrusion of teeth combined with parafunctional habits such as bruxism and clenching
Question 7. Facets.
Answer:
- Facets are shiny and irregular
- They indicate tooth-to-tooth wear that is associated with bruxism
- These worn and abraded teeth are invariably firm with no sign of mobility
Question 8. Buttressing bone formation
Answer:
- Excessive forces lead to the resorption of bone
- When bone is resorbed in such cases, the body attempts to reinforce trabeculae to form new bone
- This process is called buttressing
Types:
- Central buttressing
- In it, endosteal cells deposit new bone
- It restores bony trabeculae
- Reduces the size of bone marrow
- Peripheral buttressing
- Occurs on facial and lingual surfaces of bone
- May produce shelf-like thickening of the alveolar margin called lipping
- It is a pronounced bulge in the contour of the facial or lingual bone
Question 9. Primary and secondary trauma from occlusion
Answer:
Primary:
- When trauma from occlusion results from alteration of occlusal forces, it results in primary trauma from occlusion
- It does not alter the level of connective tissue attachment
- It does not initiate pocket formation because supracre- stal gingival fibres are not affected which prevents apical migration of junctional epithelium
Secondary:
- It is trauma from occlusion that results due to reduced ability of tissues to resist occlusal forces
- Adaptive capacity is impaired by bone loss resulting from marginal inflammation
- Reduces periodontal attachment Alters leverage on remaining tissues