Abdominal Cavity And Peritoneum Question And Answers
Question 1. Give a brief description about the contents, attachments, and functions of greater Omentum and why is it called as policeman of abdomen.
Answer:
The Contents, Attachments, And Functions Of Greater Omentum
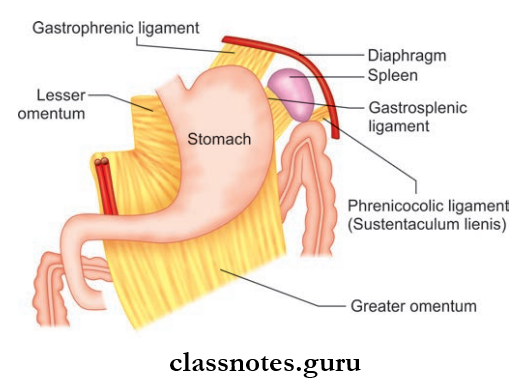
- Large thick fold of peritoneum
- Greater Omentum Hangs Down From:
- Greater curvature of the stomach
- The first part of the duodenum
- Greater Omentum hangs down in the shape of an apron and covers the loops of intestine to a variable extent
- Formed by 4 layers of peritoneum (anterior two layers and posterior two layers)
- These 4 layers get fused to form a thin fenestrated membrane
Read And Learn More: Abdomen And Pelvis
Greater Omentum Contents:
- Adipose tissue or fat
- Right and left gastroepiploic vessels anastomoses between the first two layers
- Macrophage aggregates, seen as dense milky spots
Peritoneum Anatomy Important Questions
Greater Omentum Attachments:
- Anterior Two Layers
- Hangs from greater curvature of the stomach to a variable extent
- They fold upon themselves to form the posterior two layers
- The Mode Of Folding Is Such That:
- The first layer becomes the fourth layer
- Second layer becomes the third layer
- Posterior Two Layers
- They ascend up to the transverse mesocolon
- The fourth layer loosely blends with the peritoneum on the anterior surfaces of the transverse colon and mesocolon.
Greater Omentum Functions
- When there is an infection in the peritoneal cavity, the greater omentum moves to the site of infection and seals it of from its surrounding thus limiting the spread of infection
- When there is any perforation of the gut, greater omentum plugs the gap to prevent the leakage of contents
For These Reasons, It Is Termed As Policeman Of Abdomen
- Storehouse of fat
- Macrophages present in the omentum protect the peritoneal cavity from infection.
Question 2. Describe Lesser Omentum.
Answer:
Lesser Omentum
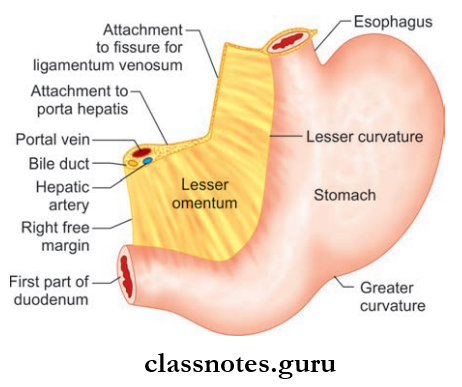
- The double-layered fold of peritoneum
- Extent: From lesser curvature of the stomach and first part of the duodenum to the inferior surface of the liver
Lesser Omentum Attachments
- Superiorly
- Attached to the liver (margins of fissure for ligamentum venosum and porta hepatis)
- In an inverted L-shaped manner
- Inferiorly
- Lesser curvature of the stomach
- Upper border of first 2 cm of duodenum.
Lesser Omentum Parts
- Lesser Omentum Is Divided Into Two Parts, They Are:
- Hepatogastric Ligament: Part of lesser omentum between the stomach and liver
- Hepatoduodenal Ligament: Part of lesser omentum between duodenum and liver
- Right margin of lesser omentum is free and it forms the anterior boundary of the epiploic foramen
- The anterior and posterior layers of the peritoneum become continuous at the right margin.
Lesser Omentum Contents
Contents Of Right Free Margin
- Portal vein
- Hepatic artery
- Bile duct
- Hepatic plexus of nerves
- Lymphatics and lymph nodes
Contents Along The Lesser Curvature Of The Stomach
- Right and left gastric vessels
- Branches of left gastric nerve
- Gastric group of lymph nodes and lymphatics
Lesser Omentum DevelopmDent: derived from ventral mesogastrium.
Abdominal Cavity And Peritoneum Notes
Question 3. Write a note on the Mesentery of the small intestine. Describe root of the Mesentery and the free border of the mesentery.
Answer:
Mesentery Of The Small Intestine
- The broad fan-shaped fold of peritoneum
- Mesentery suspends the coils of the small intestine (jejunum and ileum) from the posterior abdominal wall
- Mesentery is wider at the central and narrow at the proximal and distal ends
- The average width of the mesentery is 6 inches and at the center, it is 8 inches
- Mesentery Presents With Two Borders:
- The root of the mesentery or attached border
- Intestinal border or free border.
Root Of Mesentery
- It is 15 cm long
- Attached to an oblique line across the posterior abdominal wall
Mesentery Extent: Duodenojejunal flexure (lies on the left side of L2) to an ileocecal junction (lies at the upper part of the right sacroiliac joint)
- Directed obliquely downwards and to the right
- Mesentery Crosses The Following Structures:
- The third part of the duodenum
- Abdominal aorta
- Inferior vena cava
- Right gonadal vessels
- Right ureter
- Right psoas major
- The root of mesentery divides the infrasonic compartment into two parts namely right and left
- Right Part: Small, this part terminates in the right iliac fossa
- Left Part: Large, this part passes into true pelvis.
Lesser Omentum Intestinal Border/Free Border
- Lesser Omentum Intestinal is 6 m long
- Thrown into pleats
- Lesser Omentum Intestinal covers the jejunum and ileum
- Lesser Omentum Intestinal is attached to the gut and forms a serous coat.
Contents Of Mesentery
- Jejunal and ileal branches of superior mesenteric nartery and vein
- Autonomic nerve plexus
- Lacteals (lymphatics)
- Lymph nodes (100–200)
- Connective tissue and fat
- Jejunum and ileum.
Peritoneum And Abdominal Cavity MCQs
Question 4. Write a note on Transverse Mesocolon.
Answer:
Transverse Mesocolon
- Transverse Mesocolon is a broad transverse fold of the peritoneum
- Transverse Mesocolon suspends the transverse colon from the posterior abdominal wall.
Transverse Mesocolon Attachments
- Root of the transverse mesocolon is attached horizontally to the posterior abdominal wall, with an upward inclination towards the left
- Root Of Transverse Mesocolon Is Also Attached To:
- Pancreas: Anterior surface of the head of the pancreas and anterior border of body of pancreas
- Second part of the duodenum.
Transverse Mesocolon Contents
- Middle colic vessels
- Lymphatic and lymph nodes of the transverse mesocolon
- Nerves.
Question 5. Write a note on Sigmoid Mesocolon.
Answer:
Sigmoid Mesocolon
- Sigmoid Mesocolon is a triangular fold of the peritoneum
- Sigmoid Mesocolon suspends the sigmoid colon from the pelvic wall
- The root of the sigmoid mesocolon is attached to the pelvic wall in the shape of an inverted ‘V’
- The apex of inverted ‘V’ lies over the left ureter at the point of termination of left common iliac artery
- Left limb of inverted ’V’ has an attachment along the upper half of left external iliac artery
- Right limb is directed downwards and medially from the apex towards the median plane up to the level of S3 and is attached to the posterior pelvic wall.
Sigmoid Mesocolon Contents
- Right limb: Superior rectal vessels
- Left limb: Sigmoid vessels
- Lymphatics And Lymph Nodes Of Sigmoid Mesocolon
- Nerves.
Question 6. Describe in brief about the Peritoneal Cavity and write a note on its divisions.
Answer:
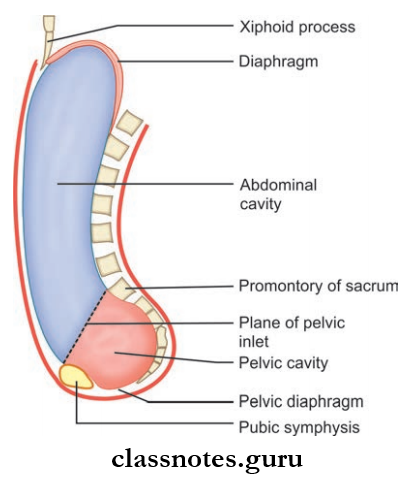
The Peritoneal Cavity
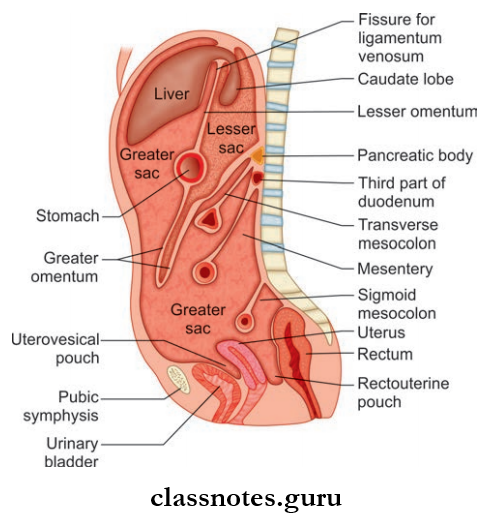
- Largest serous sac in the body, formed between the parietal and visceral layers of the peritoneum
- Secretes 30 ml of fluid/day
- Derived from coelomic cavity
- It is closed in males but open in female
- In females it communicates with the exterior through uterine tubes, uterus, and vagina
- Peritoneal Cavity Can Be Divided Into Two Parts:
- Greater Sac
- Lesser Sac.
Important Questions On Peritoneum
Peritoneal Cavity Greater Sac
- Main or larger compartment of the peritoneal cavity
- Extents across the entire area of the abdomen (from diaphragm to pelvic floor)
- Peritoneal Cavity Has 5 Recesses:
- Hepatorenal Recess: It is the peritoneal pocket between liver and kidney
- Subhepatic Recess: It is the peritoneal pocket between the liver and transverse colon
- Subphrenic Recess: It is the peritoneal pocket between the diaphragm and the anterior part of the liver
- Paracolic Recess: Lies lateral to ascending and descending colon
- Morrison’s Pouch.
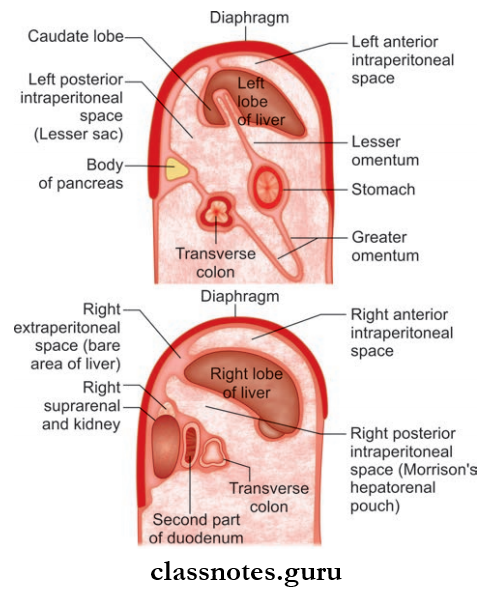
Peritoneal Cavity Subphrenic Spaces
- There are six recesses/spaces in the peritoneal cavity
- Situated between the diaphragm and the anterior part of the liver
- Three spaces are on the right and three are on the left
- On each side:
- One space: Extraperitoneal
- Two spaces: Intraperitoneal
- Peritoneal Cavity Are Namely:
- Right anterior intraperitoneal compartment
- Right posterior intraperitoneal compartment
- Right extraperitoneal compartment
- Left anterior intraperitoneal compartment
- Left posterior intraperitoneal compartment
- Left extraperitoneal compartment.
Peritoneal Cavity Lesser Sac
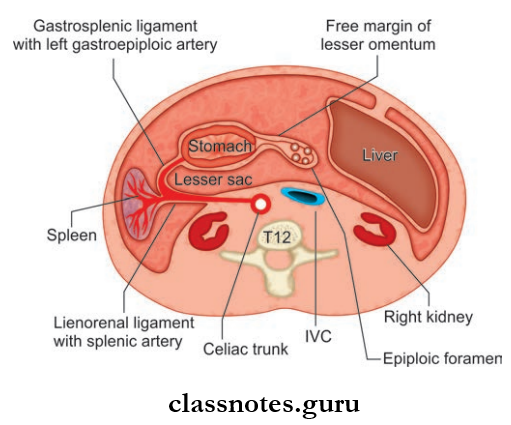
- Also known as omental bursa
- It is the left posterior intraperitoneal compartment
- This large recess of the peritoneal cavity is located behind:
- Stomach
- Lesser omentum
- Caudate lobe of liver
- It is closed all around, except in the upper part of its right border
- Here, there is a slit-like opening called the epiploic foramen through which it communicates with the greater sac.
Peritoneal Cavity Boundaries
- Anterior Wall
- Anterior two layers of greater omentum
- Stomach
- Lesser omentum
- Caudate lobe of liver
- Posterior Wall
- Diaphragm
- Left suprarenal gland
- Upper part of left kidney
- Pancreas
- Transverse mesocolon
- Transverse colon (How to remember: Structures forming stomach bed—spleen)
- Posterior two layers of greater omentum
- Upper Border
- Peritoneal reflction (from esophagus to diaphragm)
- Fissure for ligamentum venosum (its upper end)
- Caudate lobe of liver (its upper border)
- Lower Border
- Continuation of 2nd layer with the 3rd layer of greater omentum
Peritoneum Anatomy Viva Questions
Lesser Sac Has 3 Recesses
- Superior Recess: Lies posterior to lesser omentum and liver
- Inferior Recess: Lies between anterior two layers and posterior two layers of greater omentum
- Splenic Recess: Lies between lienorenal ligaments and gastrosplenic ligaments.
Question 7. Write a note on epiploic foramen.
Answer:
Epiploic Foramen
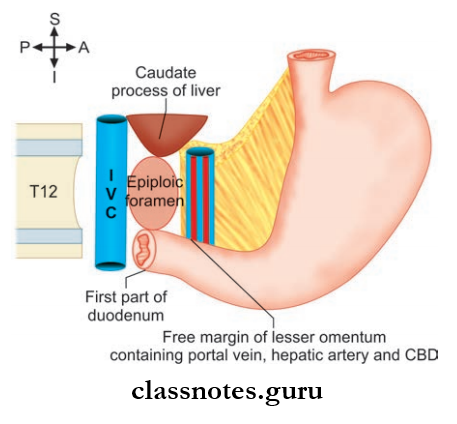
- Also known as foramen of Winslow
- Epiploic Foramen is a vertical slit like opening of the lesser sac through which it communicates with the greater sac
- Epiploic Foramen is located at the level of T12 vertebrae
- Situated behind the right free margin of lesser omentum.
Epiploic Foramen Boundaries
- Anteriorly
- Right free margin of lesser omentum and its contents
- Posteriorly
- Inferior vena cava
- Right suprarenal gland
- T12 vertebrae
- Superiorly
- Caudate process of liver
- Inferiorly
- First part of the duodenum
- Horizontal part of hepatic artery
Question 8. Describe about Morrison’s pouch or hepatorenal pouch.
Answer:
Morrison’s Pouch
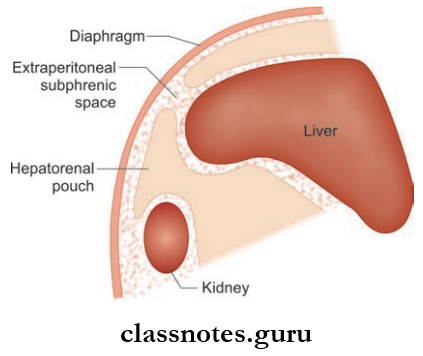
- Right posterior intraperitoneal compartment
- The most dependent part of the peritoneal cavity
- Morrison’s Pouch Is Situated Between:
- Anterior aspect of right kidney
- The posteroinferior surface of the liver.
Morrison’s Pouch Or Hepatorenal Pouch Boundaries
- Anteriorly
- Visceral surface of the liver
- Gallbladder
- Posteriorly
- The second part of the duodenum
- Hepatic flexure of colon
- Transverse mesocolon
- Right suprarenal gland
- The upper part of right kidney
- Head of the pancreas
- Superiorly
- Inferior layer of coronary ligament
- Inferiorly
- Opens into the general peritoneal cavity
Morrison’s Pouch Or Hepatorenal Pouch Applied Anatomy
- It is the common site for subphrenic abscess
- Since it is open inferiorly to the general peritoneal cavity, infections from this pouch can easily enter the peritoneal cavity
- Usually, this recess is not filled with fluid but during conditions like hemoperitoneum, flids can get collected in this space or recess.
Abdominal Cavity And Peritoneum PDF
Question 9. Describe Rectouterine Pouch (pouch of Douglas).
Answer:
Rectouterine Pouch (pouch of Douglas)
- Peritoneal pouch present in females
- Situated behind the rectum and uterus
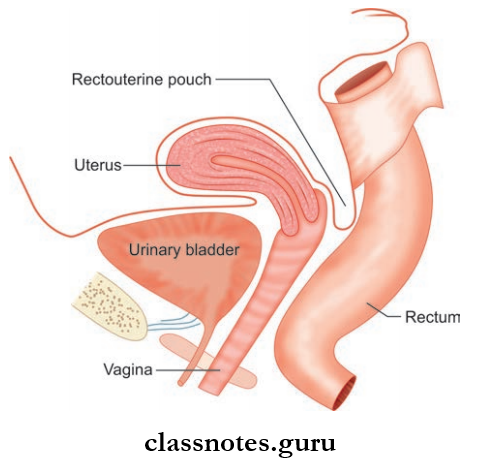
Rectouterine Pouch Features:
- In The Upright Position: Most dependent part of the peritoneal cavity
- In The Supine Position: Most dependent part of the pelvic cavity
Rectouterine Pouch Boundaries
- Anteriorly: Uterus and upper 1/3rd of vagina
- Posteriorly: Rectum
- Floor: Rectovaginal fold of peritoneum.
Abdominal Cavity And Peritoneum Multiple Choice Questions
Question 1. Which ligament is NOT part of the greater omentum?
- Gastrocolic ligament
- Hepatogastric ligament
- Gastrosplenic ligament
- Splenorenal ligament
Answer: 2. Hepatogastric ligament
Question 2. Which structure is the remnant of the umbilical vein?
- Ligament of Treitz
- Falciform ligament
- Round ligament (Teres)
- Coronary ligament
Answer: 3. Round ligament (Teres)
Question 3. Which of the following structures is most likely to get affected by a posteriorly perforating peptic ulcer?
- Hepatorenal pouch
- Greater sac
- Lesser sac
- Pouch of Douglas
Answer: 3. Lesser sac
Question 4. What is the posterior boundary of the epiploic foramen?
- Caudate lobe of the liver
- First part of the duodenum
- Common bile duct
- Inferior vena cava
Answer: 4. Inferior vena cava
Abdominal Cavity And Peritoneum Questions And Answers
Question 5. Foramen of Winslow is bounded:
- Superiorly by the left lobe of liver
- Anteriorly by lesser omentum
- Posteriorly by the inferior vena cava
- Inferiorly by the pylorus of stomach
Answer: 4. Inferiorly by the pylorus of stomach