Front Of Leg And Dorsum Of Foot
Question 1. Briefly explain the superficial and deep fascia of the front of leg and dorsum of the foot. How deep fascia divides leg into compartments?
Answer:
The Superficial And Deep Fascia Of The Front Of Leg And Dorsum Of The Foot
Front Of Leg Superficial Fascia
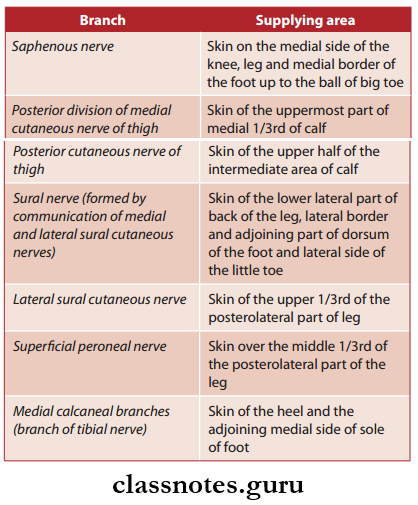
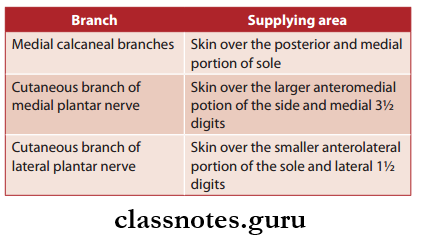
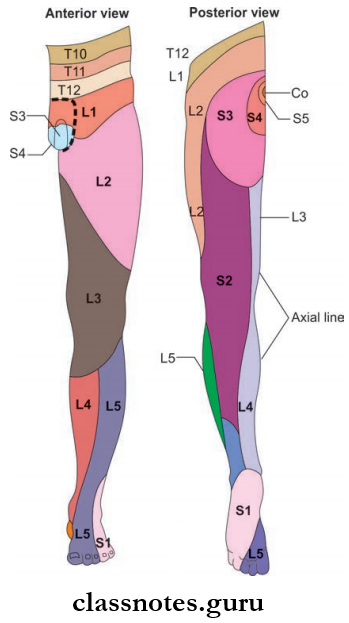
Superficial fascia over the front of leg and dorsum of foot contains:
- Superficial vein
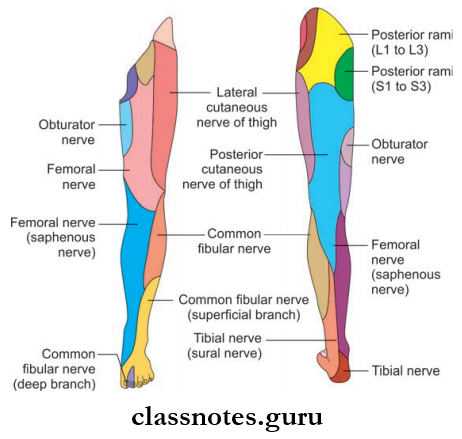
- Cutaneous nerves
- Lymphatics
- Unnamed arteries
Front Of Leg Deep Fascia
- The deep fascia of leg is very strong and encloses the leg like a tight sleeve.
- However, at places, the tibia and fibula is subcutaneous and covered by the periosteum only.
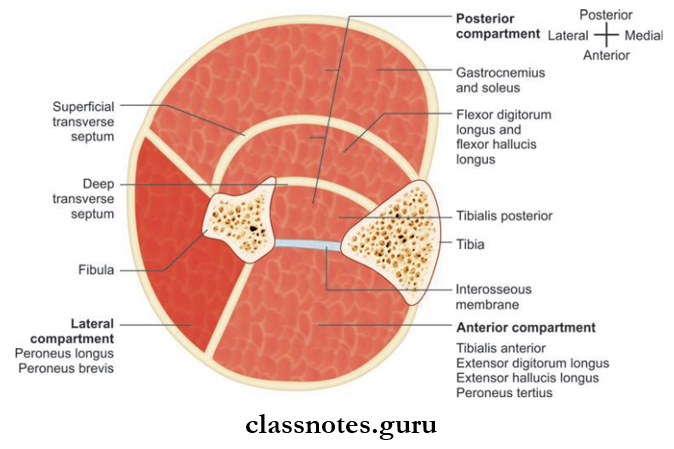
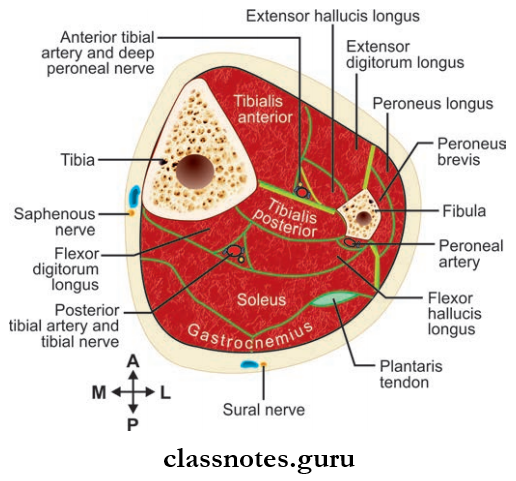
- Extensions of the deep fascia form intermuscular septa that divide the leg into compartments.
- The anterior intermuscular septa are attached to anterior border of the fibula whereas the posterior intermuscular septa are attached to the posterior border of the fibula.
- They divide the leg into anterior, posterior, and lateral compartments.
- Around the ankle, they are thickened and form the extensor, peroneal and flxor retinaculum.
Read And Learn More: Anatomy Question And Answers
Question 2. Write a note on the extensor retinaculum of the lower limb.
Answer:
Extensor Retinaculum Of The Lower Limb
- It is the thickened part of deep fascia in front of ankle
- It is of 2 in number.
- Superior extensor retinaculum
- It is band-shaped
- Attached
- Medially: To the lower part of anterior border of the tibia
- Laterally: To the lower part of anterior border of fibula
- Inferior extensor retinaculum
- It is ‘Y’ shaped
- The stem of ‘Y’ lies laterally while the upper and lower bands medially.
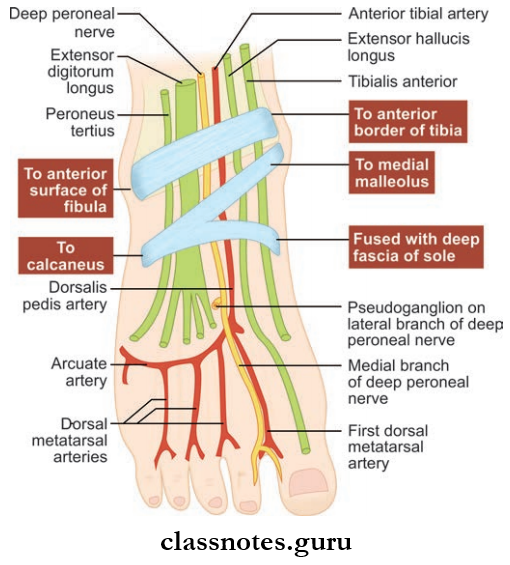
- Attachments
- The stem is attached laterally to the anterior nonarticular part of the superior part of the calcaneus in front of the sulcus calcanei.
- The upper band is attached to the anterior border of the medial malleolus.
- Lower band is attached to the plantar aponeurosis.
- Structures Passing Undercover
- Tibialis anterior
- Extensor hallucis longus
- Anterior tibial vessels
- Deep peroneal nerve
- Extensor digitorum longus
- Peroneus tertius.
- Function
- Stabilizing the tendon passing beneath it.
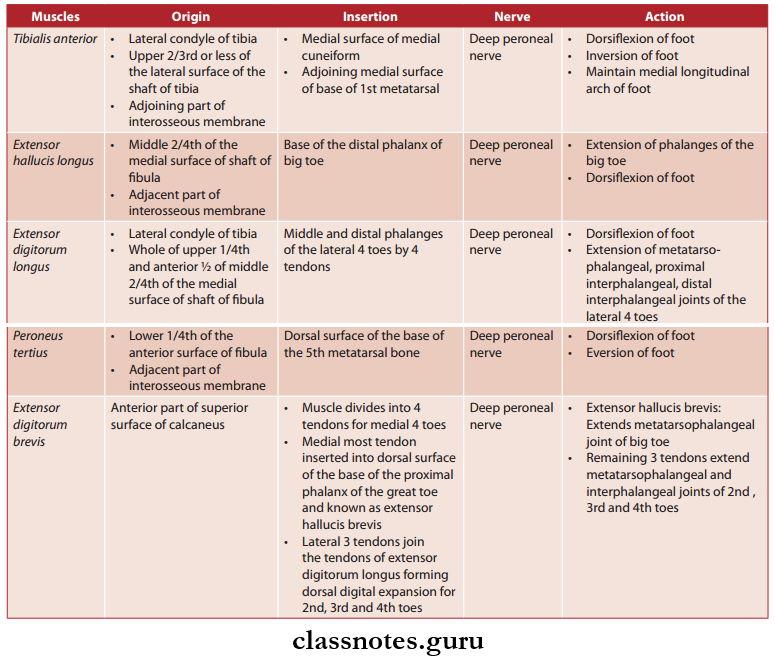
Question 3. List the muscles of the dorsum of foot. Write their origin, insertion, nerve supply, and actions.
Answer:
The Muscles Of The Dorsum Of Foot
- Intrinsic Muscles: Only one
- Extensor digitorum brevis.
- Extrinsic Muscles:
- Tibialis anterior
- Extensor hallucis longus
- Extensor digitorum longus
- Peroneus tertius.
Muscles Of The Anterior Compartment Of The Leg And Dorsum Of The Foot
Mnemonics
- Leg: Anterior muscles of leg ‘The Hospitals Are Not Dirty Places’:
- T: Tibialis anterior
- H: Extensor hallucis longus
- A: Anterior tibial artery
- N: Deep fiular nerve
- D: Extensor digitorum longus
- P: Peroneus tertius.
Lateral Compartment Of Leg
Question 4. Give the boundaries and contents of the lateral compartment of leg.
Answer:
Lateral Compartment Of Leg Boundaries
- Anterior: Anterior intermuscular septum
- Posterior: Posterior intermuscular septum
- Medial: Lateral surface of fibula
- Lateral: Deep fascia of the leg.
Lateral Compartment Of Leg Contents
- Muscles: Peroneus longus, peroneus brevis
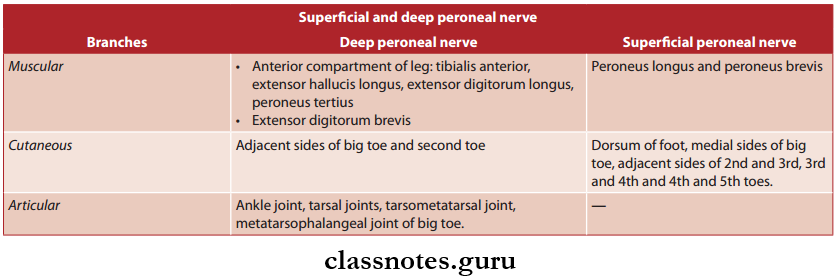
- Nerves: Superficial peroneal nerve
- Arteries: Small branches supplying muscles
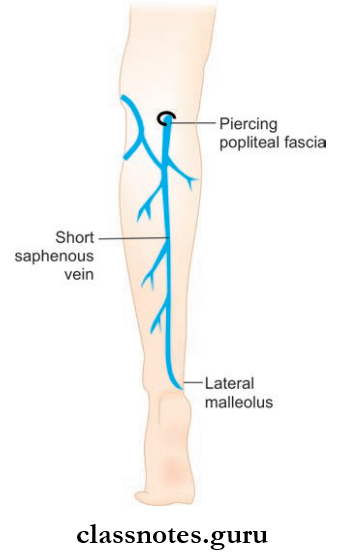
- Venous Branches: Draining into short saphenous veins.
Question 5. Write a note on the peroneal retinaculum.
Answer:
Peroneal Retinaculum
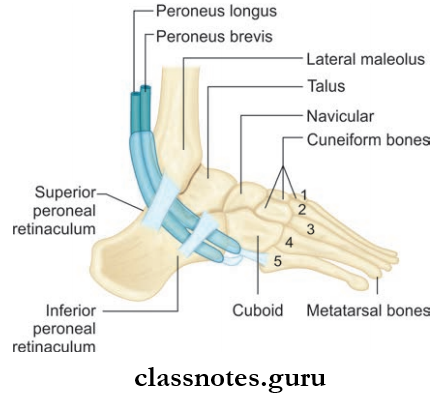
Deep fascia over the lateral side of the ankle is modified to form two thick bands known as the superior and inferior peroneal retinaculum.
Superior Peroneal Retinaculum
- Attached
- Anteriorly: To the back of the lateral malleolus
- Posteriorly: To the lateral surface of the calcaneus and superficial transverse septum of the leg.
Inferior Peroneal Retinaculum
- Attached
- Superiorly: To the anterior part of the superior surface of the calcaneus, close to the stem of the inferior extensor retinaculum
- Inferiorly: To the lateral surface of the calcaneus.
- Structures Under Peroneal Retinaculum
- Tendons of peroneus longus and peroneus brevis
- Under superior peroneal retinaculum, both tendons are enclosed in a single synovial sheath, whereas under inferior peroneal retinaculum, they are enclosed in a separate synovial sheath.
- Function
- Stabilizing the tendons of peroneus longus and peroneus brevis.
Medial Side Of Leg
- It is formed by the medial surface of the shaft of tibia.
- Most of the part is subcutaneous.
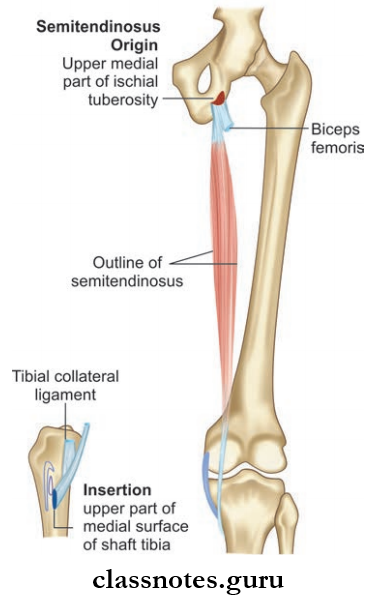
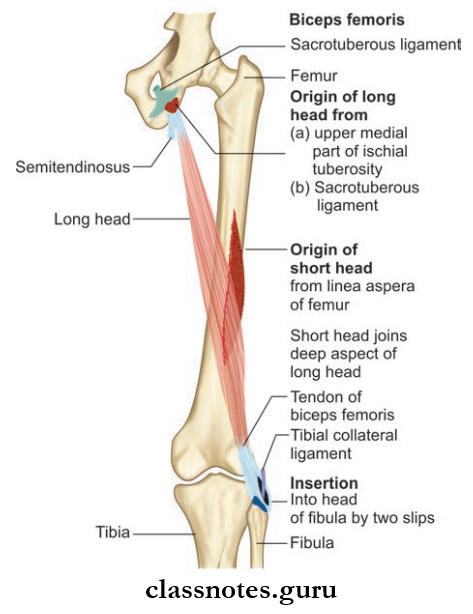
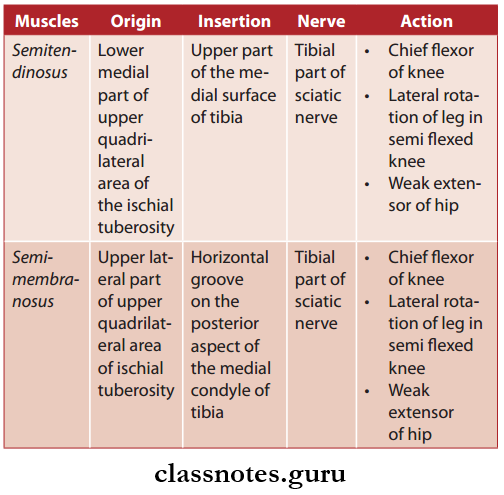
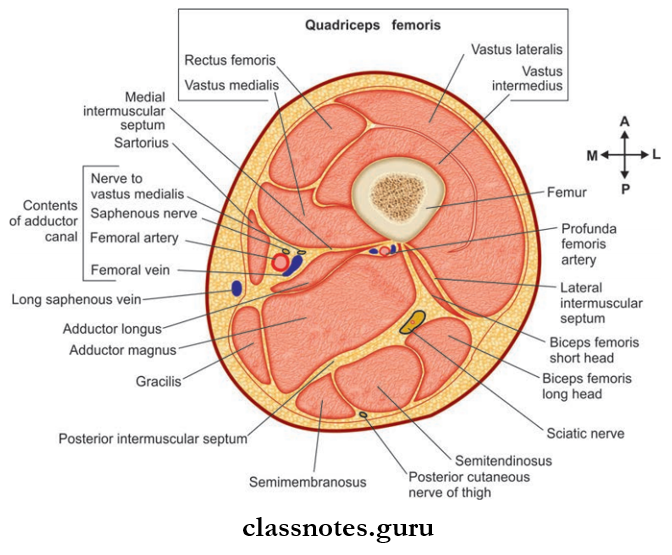
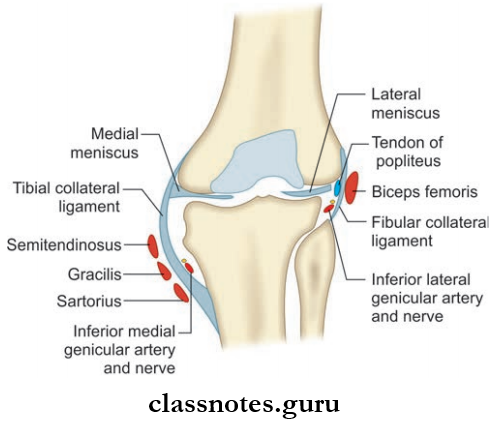
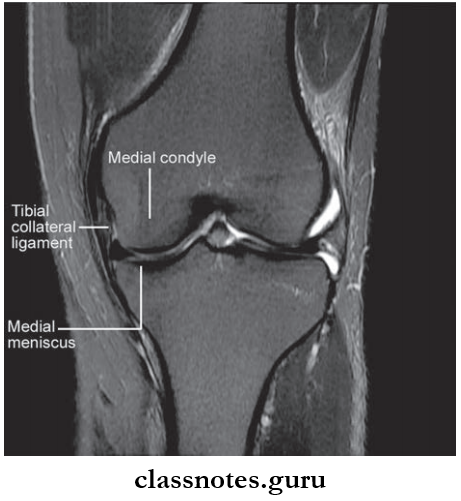
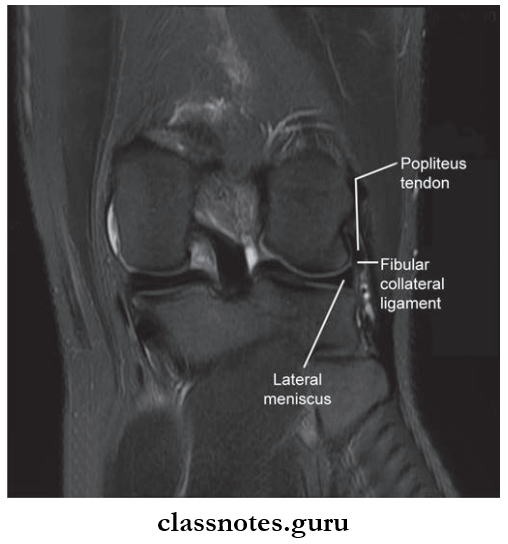
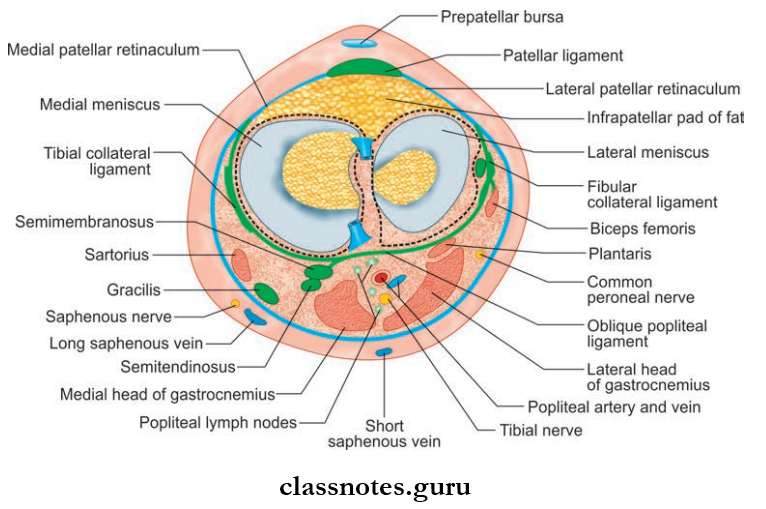
- But in the upper part, the tibial collateral ligament and three muscles namely sartorius, gracilis, and semitendinosus are inserted.
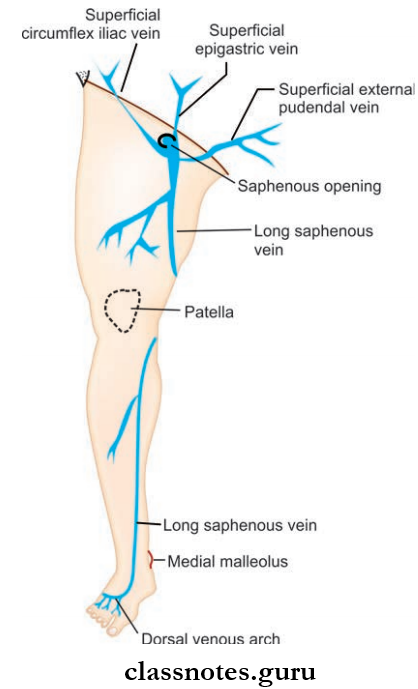
- A great saphenous vein and saphenous nerve runs through this compartment.
Question 6. What is guy ropes?
Answer:
Guy Ropes
The muscles which are inserted into one point over the upper part of the medial side of the tibia are however originate wide apart from the hip bone and represent different compartments. They act as 3 strings of a tent and stabilize the bony pelvis known as ‘guy ropes’.
Question 7. What is anserine bursa?
Answer:
Anserine Bursa
- It is a complicated synovial bursa several diverticula present over the upper part of the medial surface of the tibia.
- It helps to separate and reduce frictions (between the tendons of sartorius, gracilis, and semitendinosus and separates this from the tibial collateral ligament).
Anserine Bursa Clinical Anatomy
- Anserine bursitis is the inflammation of the anserine bursa
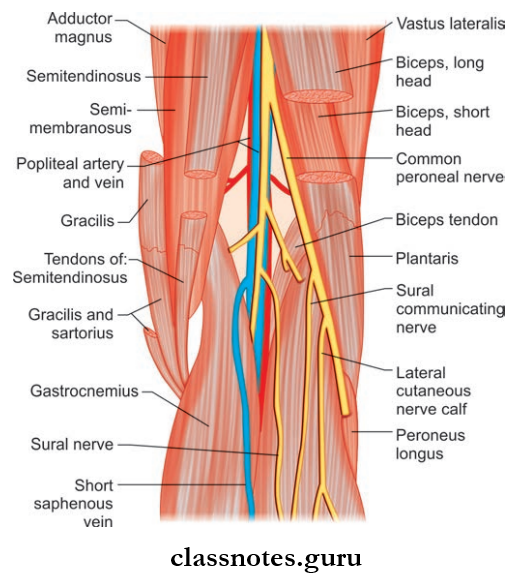
Question 8. Give a brief description of calf region mentioning about boundaries and subdivision of the posterior compartment of leg.
Answer:
Calf Region Mentioning About Boundaries And Subdivision Of The Posterior Compartment Of Leg
Corresponds to the front of the forearm. It extends from the popliteal fossa above to the ankle below.
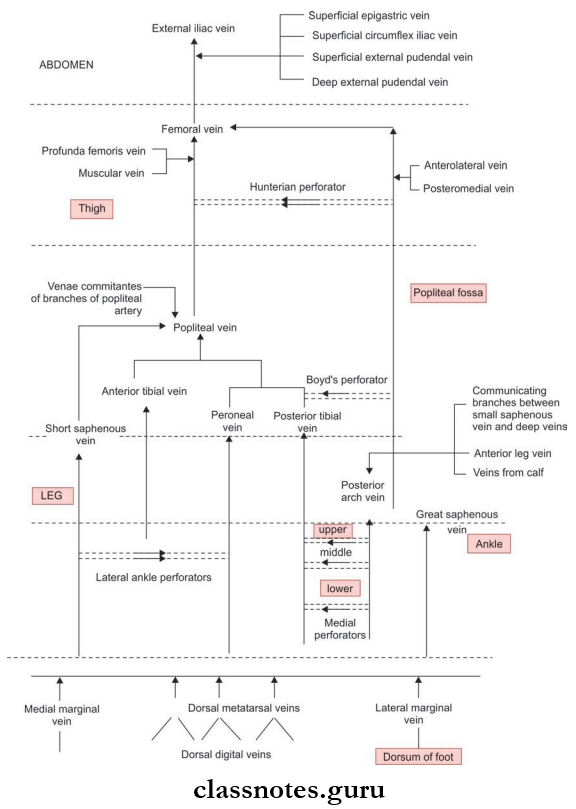
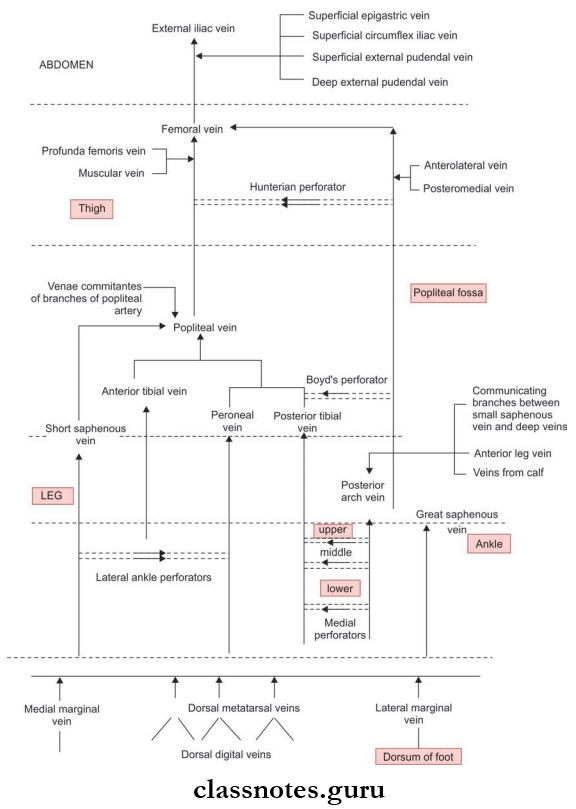
- Superficial Fascia
- It contains:
- Small or short saphenous vein
- Great saphenous vein
- Cutaneous nerves.
- It contains:
- Deep Fascia
- Deep fascia bounds and subdivides the posterior compartment of leg.
Boundaries And Subdivision Of Posterior Compartment Of Leg
Posterior Compartment Of Leg Boundaries:
- Anteriorly: Tibia, interosseous membrane, fibula, posterior intermuscular septum
- Posteriorly: Deep fascia of the leg
Posterior Compartment Of Leg Subdivision:
- It is subdivided into 3 by the deep fascia. They are:
- Superficial
- Middle
- Deep
Contents of the posterior compartment are distributed in these three divisions.
Question 9. Write a note on the flexor retinaculum of lower limb.
Answer:
Flexor Retinaculum Of Lower Limb
The Flexor Retinaculum Of the Lower Limb is a band formed at the medial side of the ankle by the thickening of the deep fascia of leg.
- Attachments
- Anterior: To the posterior border and hip of the medial malleolus
- Posterolaterally: To the medial tubercle of the calcaneus.
- Structures Passing Deep To Retinaculum
- The septa passes to the underlying bone from the retinaculum and divides it into 4 compartments.
- Structures passing from medial to lateral are:
- Function
- Stabilizing the tendons passing underneath it.
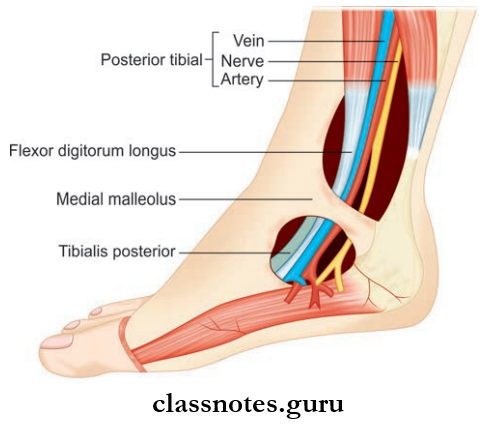
Flexor Retinaculum Of Lower Limb Clinical Anatomy
These structures are passing through tarsal tunnel and if the nerve get compressed, it leads to tarsal tunnel syndrome.
Mnemonics
- Medial malleolus: Order of tendons, artery, nerve behind it.
- ‘Tom, Dick, And Nervous Harry’:
- From anterior to posterior:
- Tibialis
- Digitorum
- Artery
- Nerve
- Hallicus
Full names for these are Tibialis Posterior, Flexor Digitorum Longus, Posterior Tibial Artery, Posterior Tibial Nerve, and Flexor Hallicis Longus.
Question 10. List the muscles of the posterior compartment of the leg. Write their origin, insertion, nerve supply, and actions.
Answer:
Posterior Compartment Of The Leg They Are Categorized Into:
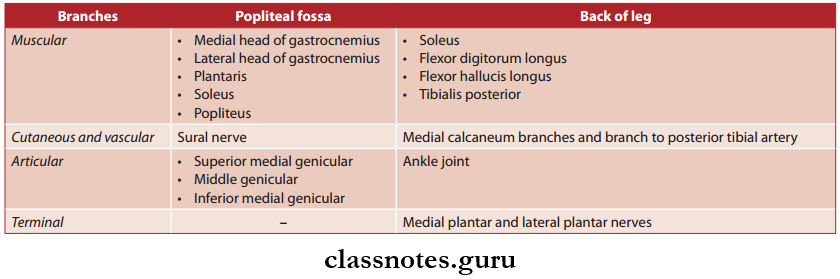
- Superficial Muscles:
- Gastrocnemius
- Soleus
- Plantaris
- Deep Muscles:
- Popliteus
- Flexor digitorum longus
- Flexor hallucis longus
- Tibialis posterior.
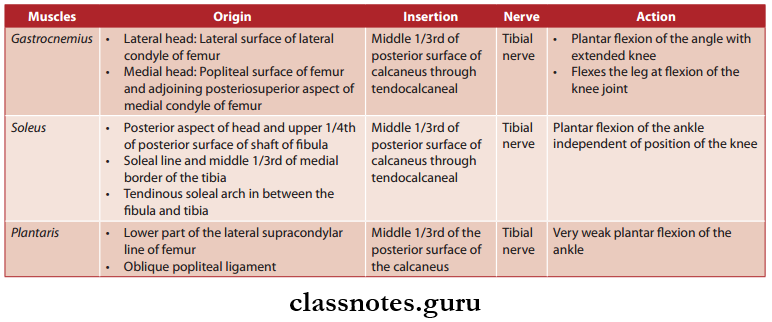
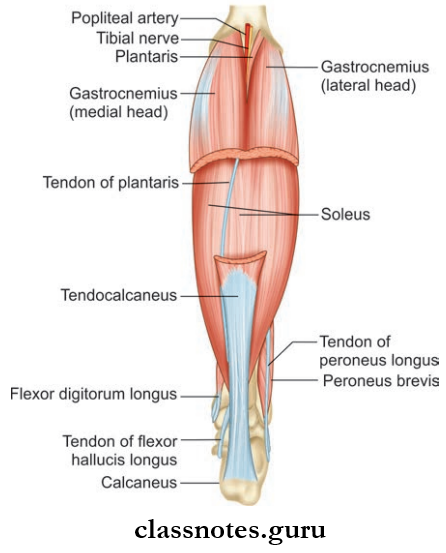
Superfiial Muscles of Back of Leg
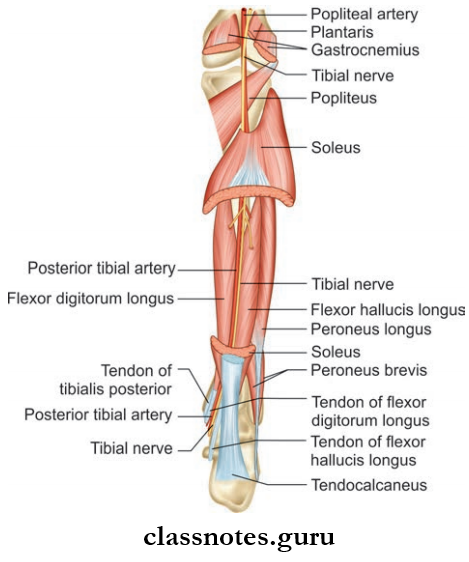
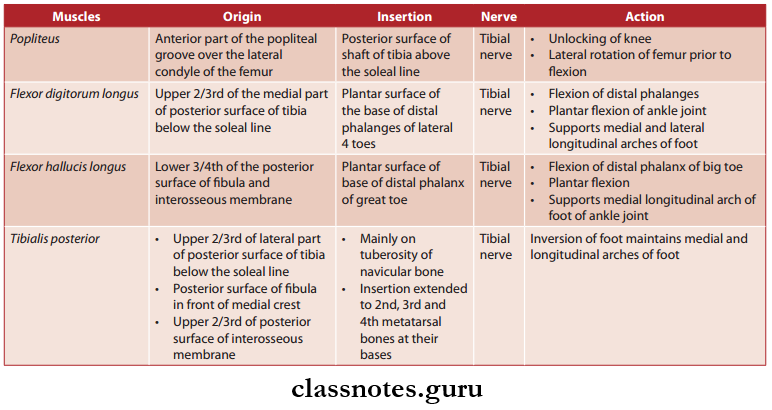
Deep Muscles of Back of Leg
Posterior Compartment Of The Leg Clinical Antomy
- Calf muscles are very important in circulation. There are valveless venous sinuses in these muscles and blood is filled in these sinuses. When these muscles contract, blood is pumped out, and when the muscle relaxes, blood is sucked in from superficial veins through perforators. So they act as peripheral hearts.
- When the calf muscles are at rest for a long time, especially in bed-ridden patients, the venous sinuses can develop thrombosis, which eventually dislodges and block arteries.
- Tendocalcaneal, otherwise known as the Achilles tendon is very strong, however can get ruptured in tennis players.
- Tendocalcaneal reflux is usually tested to assess deep tendon reflexes in CNS examination.
Leg And Dosum Of Foot Multiple Choice Questions
Question 1. Which of the following is not attached to fibula?
- Tibialis anterior
- Extensor hallucis longus
- Extensor digitorum longus
- Peroneus tertius
Answer: 1. Tibialis anterior
Question 2. Violent inversion of foot will lead to the avulsion of a tendon that is inserted into the tuberosity of the fifth metatarsal bone. Identify the tendon:
- Peroneus Brevis
- Peroneus longus
- Peroneus Tertius
- Tibialis posterior
Answer: 1. Peroneus Brevis
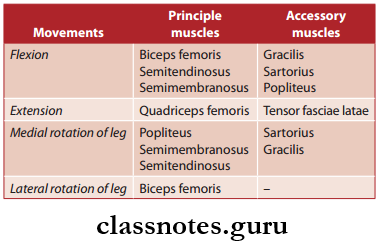
Question 3. Which of the following muscles act on both knee and ankle joints?
- Soleus
- The short head of biceps
- Gastrocnemius
- Long head of biceps femoris
Answer: 3. Gastrocnemius
Question 4. Pes anserine is the term used for insertion of the following muscles:
- Semitendinosus
- Semimembranosus
- Sartorius
- Gracilis
Answer: 2. Semimembranosus