Bacterial Infections Important Notes
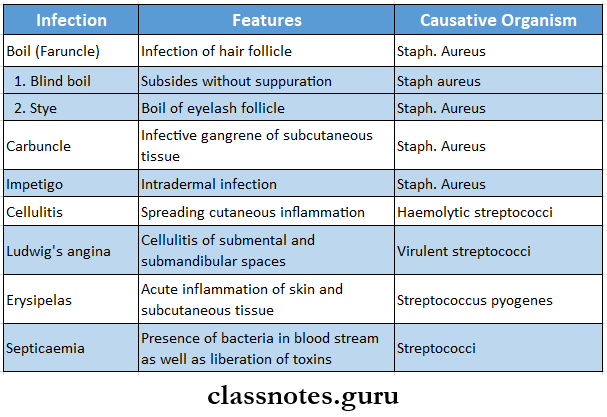
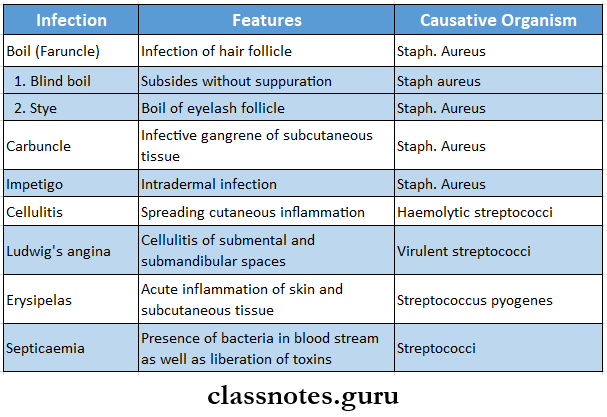
- Different Infections
Bacterial infections questions and answers
- Pyaemia
- A condition characterized by formation of secondary foci of suppuration in various parts of the body
- Bacteraemia
- Indicates bacteria circulating in the bloodstream
- Septicaemia
- Indicates presence of bacteria in bloodstream as well as liberation of toxins
- Toxaemia
- Condition in which toxins circulates in the bloodstream
- Classification Of Granuloma
- Caseous
- Gummatous
- Suppurative
- Fibrinoid
- Lymph Nodes In Different Infections
- Rubbery in syphilis
- Matted in tuberculosis
- Abscess
- It is a cavity filled with pus and lined by a pyogenic membrane
- Types
- Pyaemic abscess
- Pyogenic abscess
- Cold abscess
- Principle of treatment
- Drainage of pus
- Culture and sensitivity test
- Use of proper antibiotics
- Tuberculosis
- Causative organism – mycobacterium tuberculosis
- Routes of inhalation of tubercle bacilli
- Direct spread to the lungs
- Through tonsils
- Enter the bloodstream
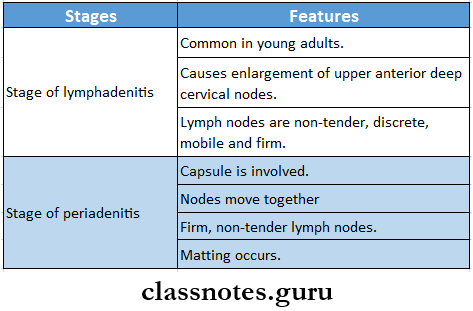
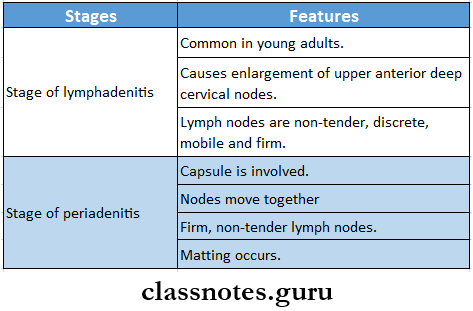
- Stages of tubercular lymphadenitis
- Stage of lymphadenitis
- Stage of periadenitis
- Stage of cold abscess
- Stage of collar stud abscess
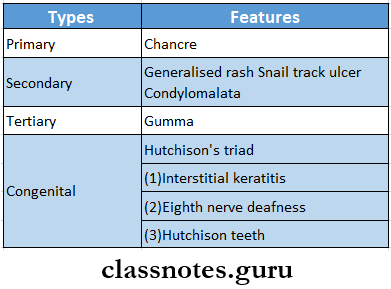
- Syphilis
- Causative agent – Treponema pallidum
- Types:
- Tetanus
- Causative agent – Clostridium tetani
- Toxins produced – tetanolysin, tetanospasmin
- The interval between the first symptom and first reflex spasm is known as period of onset
- If it is less than 48 hours, the condition is almost fatal
- Incubation period is followed by period of onset
- Types
- Tetanus neonatal/ eighth day disease
- Occurs usually around 6-8 day of birth due to contamination of the umbilical cord
- Post-abortal/ puerperal tetanus
- Due to unsterile manipulation during abortion or during labor
- Postoperative tetanus
- Following elective surgery
- Latent tetanus
- Develops after few months to years following wound
- Bulbar tetanus
- Involves muscles of deglutition and respiration
- Cephalic tetanus
- Occurs after wound of face and neck
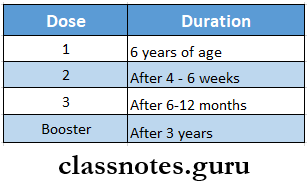
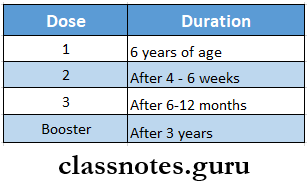
- DPT Vaccine
- Involves Diphtheria, Pertussis and Tetanus toxoid
- 3 doses are given at 6,10 and 14 weeks of age
- Booster dose is given at 18 months and 5 years of age
- Gas Gangrene
- Etiological agent – cl. Perfringes
- Toxins produced by it are
- Alpha toxin
- Beta toxin
- Theta toxin
- Hyaluronidase
- Collagenase
- Leucocidin
Bacterial infections Questions & Answers for students
Read And Learn More: General Surgery Question and Answers
Bacterial Infections Long Essays
Question 1. Describe the etiology, pathology, clinical features, and management of Bacterial Infections.
Answer:
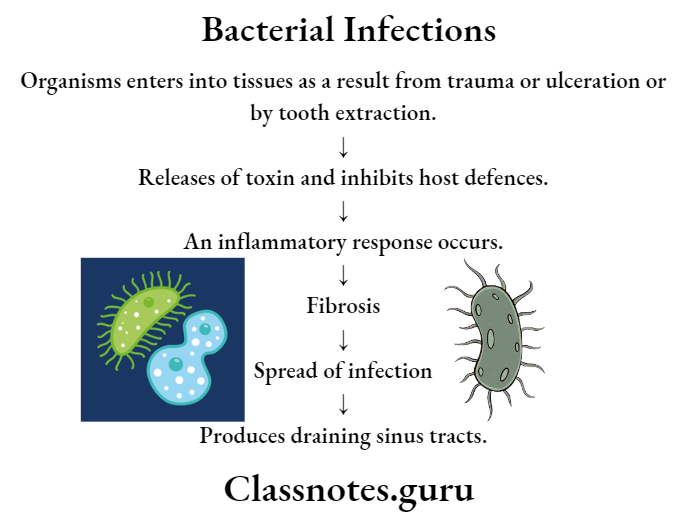
Actinomycosis:
- Actinomycosis is a chronic, suppurative granulomatous disease.
Bacterial Infections Etiology:
- Actinomyces israelii, an anaerobic gram-positive filamentous organism causes it.
Bacterial Infections Pathology:
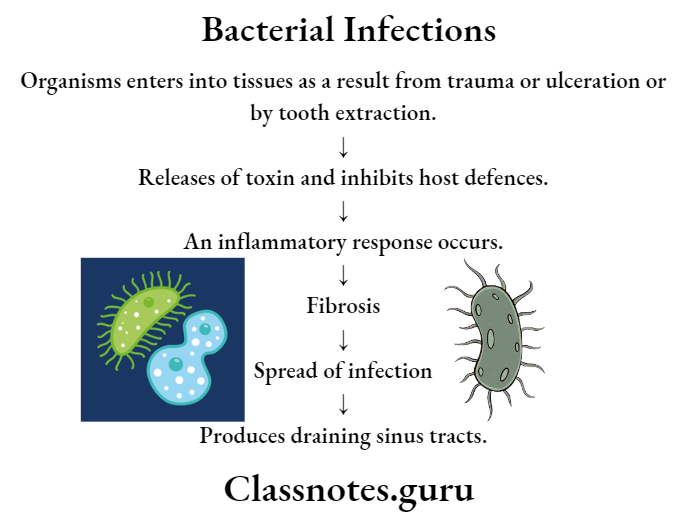
Bacterial diseases MCQs with answers
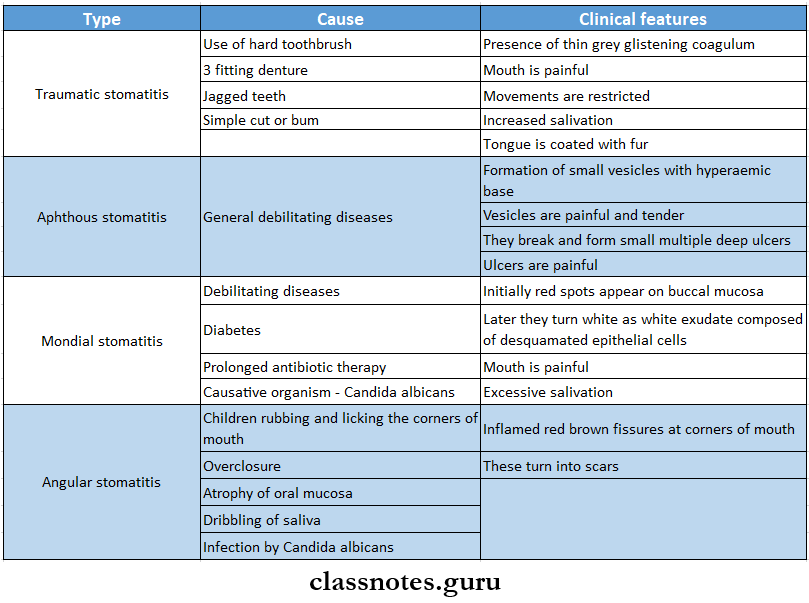
Bacterial Infections Clinical Features: Three clinical forms of actinomycosis are identified.
- Facio-cervical actinomycosis.
- Frequently involves lower jaw.
- Present as a painless firm mass called lumpy jaw.
- Underlying .connective tissue, muscle, and bone are destroyed and replaced by granulation tissue.
- Gradually softening occurs at some places forming abscess.
- It later burst to form sinuses.
- Overlying skin becomes indurated and bluish in colour.
- Pus contains sulphur granules.
- Lymph nodes are not involved.
- Abdominal form.
- Mainly affects the caecum or appendix.
- Submucosa contains flat grey nodules which later enlarges.
- Suppuration within it leads to abscess formation.
- Later abdominal wall is involved with multiple discharging sinuses.
- Liver is involved through portal vein.
- Lesion is a honeycomb mass.
- Lungs.
- It is common in children.
- Involves direct spread from neck or from the abdomen.
- Lungs becomes jumbled with multiple abscesses cavity surrounded by abundant fibrous tissue.
Bacterial Infections Management:
- As it is a chronic disease, it is difficult to treat.
- In crystalline penicillin – 10 lakh units once a day for 6 -12 months is given.
- Later it is reduced to 4 lakh units.
- Tetracycline and lincomycin are other alternatives.
- Actinomycosis of the abdomen needs. Hemocolectomy.
- Surgical treatment includes incisions and drainage of abscesses, excision of the sinus tract, and relieving obstruction.
Common bacterial infections and their treatment Q&A
Question 3. Discuss pathogenesis, clinical features, and treatment of gas gangrene.
Answer:
Gas Gangrene:
- Gas Gangrene is a rapid spreading infective gangrene of the muscle characterized by a collection of gas in the muscles and subcutaneous tissue.
Gas Gangrene Pathogenesis:
Gas gangrene is caused by an anaerobic, gram-positive, spore-forming bacillus, Clostridium per-fringes.
Develops in wounds where there is heavy contamination.
This causes low oxygen tension.
↓
Multiplication of Clperfringes.
↓
Release of exotoxins by them.
↓
Causes lysis of erythrocytes, leucocytes, platelets, fibroblasts, and muscle cells.
↓
Further tissue damage occurs.
Gas Gangrene Clinical Features:
1. General:
- Anaemia anxiety.
- Low-grade fever.
- Rapid pulse.
- Hypotension – due to toxin production.
- Nausea, vomiting.
2. Local:
- Sudden onset of pain in affected part.
- Pain worsens as time passes.
- Gradual swelling and gross edema of the part.
- Profuse discharge of brownish and foul swelling fluid.
- Discoloration of skin – khaki to greenish due to hemolysis.
- Crepitus follows gas production.
- Muscle becomes green to black in color.
Gas Gangrene Treatment:
- Surgery.
- Multiple longitudinal incisions for decompression and drainage.
- Aggressive surgical debridement in the form of excision of all devitalized tissues.
- In severe type of gas gangrene, amputation is carried out.
- Supportive treatment.
- Penicillin 10 lac units every 4 hours.
- Supplemented by tetracycline 2 g daily or chloramphenicol 2g or streptomycin 1 – 2g.
- Blood transfusion.
- Administration of anti-gas-gangrene serum.
- Hyperbaric oxygen.
Question 4. Define carbuncle. Mention its etiology, clinical features, and treatment of carbuncle.
Answer:
Carbuncle Definition: Carbuncle is infective gangrene of the subcutaneous tissue.
Carbuncle Etiology:
- Staphylococcus aureus.
- Gram-negative bacilli.
- Streptococci.
Carbuncle Clinical Features:
- Sites involved are.
- Commonly back, nape of the neck.
- Rarely – cheek, shoulders, dorsum of the hand.
- Age and sex: generally affects males above 40 years of age.
- Presentation.
- Painful, stiff swelling.
- Spreads very rapidly.
- Overlying skin becomes red, dusky, and oedematous
- Central part softens and multiple vesicles appear on the skin.
- Vesicles transform into pustules.
- Pustule burst and allow the discharge to come out over the skin through various openings.
- This results in a cribiform appearance.
- Openings enlarge, coalesce, and form ulcers containing ashy-grey slough.
- Patient in diabetic.
Carbuncle Treatment:
- Improvement of the general health of the patient.
- Diabetic control through insulin injections.
- Antibiotics are administered, like cloxacillin, flucloxacillin, erythromycin, and some cephalosporin.
- Surgery required if.
- Toxaemia and pain persist even after the antibiotic course.
- When the carbuncle is more than 2xh inch in diameter.
- Cruciate incision is preferred which extends the opto margin of the inflammatory zone.
Question 5. Describe signs, symptoms, and treatment of alveolar abscess.
Answer:
Alveolar Abscess
An abscess is a collection of pus. Alveolar abscess is an abscess in the alveolar ridge of the jaw, usually caused by the spread of infection from a non-vital tooth.
Alveolar Abscess Clinical features:
- Produced severe pain in the affected tooth.
- Localized swelling.
- Reddening of the overlying mucosa.
- Pain aggrevates on application of pressure.
- Application of heat intensifies pain while application of cold may relieve pain.
- Elevated body temperature.
- Affected tooth is non-vital and can be mobile.
- Pus discharging sinus are formed.
Alveolar Abscess Treatment:
- Incision and drainage of pus
- Pulpectomy.
- Analgescis – for relieving pain.
- Antibiotic – to treat infection.
- Extraction of offending tooth,
Question 6. Describe the etiology, clinical features, diagnosis, and treatment of chronic osteomyelitis of the jaw.
Answer:
Osteomyelitis:
- Osteomyelitis is defined as an inflammation of bone and bone marrow along with the surrounding periosteum.
Osteomyelitis Types:
- Acute
- Sub-acute
- Chronic
Chronic Osteomyelitis Of Jaw:
- The disease persisting for more than a mouth is called chronic osteomyelitis.
Osteomyelitis Etiology:
- Fracture of mandible.
- Alveolar abscess.
- Radiation
- Chemical necrosis.
- Rarely tuberculosis, syphilis, and actinomycosis.
Osteomyelitis Clinical Features:
- Local osteitis:
- Formation of a cavity due to osteolytic lesion with surrounding sclerosis.
- It is called Brodie’s abscess.
- Sequestrum may or may not be present.
- Bone necrosis occurs.
- Mandible is more often affected than maxilla.
- Pain is mild and dull in nature.
- Jaw swelling with sinus tract formation occur.
Osteomyelitis Diagnosis:
- Radiology:
- Shows periosteal reaction.
- Brodie’s abscess is seen on X-rays.
- Sequestrum is present can be detected.
- Involucrum is identified.
Osteomyelitis Treatment:
- Medical therapy.
- Systemic antibiotics – given for 2 – 4 months.
- Penicillin.
- Metronidazole.
- Clindamycin.
- Topical antibiotics.
- Used as systemic cannot reach the site.
- Surgical management.
Suitable incision is made at dependent part.
↓
Involucrum is chiselled out
↓
Cavity is made open
↓
Sequestrum is removed.
↓
Cavity is packed with petroleum jelly gauze
↓
Antibiotics are administered.
Bacterial infections pharmacology questions and answers
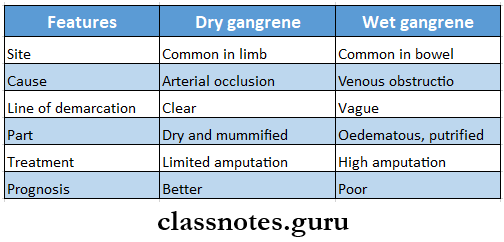
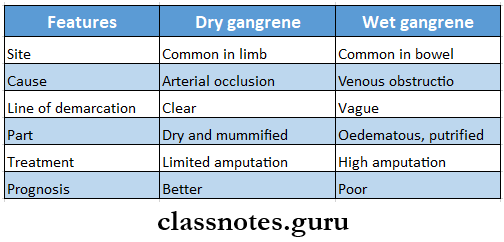
Question 7. Define gangrene. Write types, causes, and management of gangrene.
Answer:
Gangrene It is death of a portion of the body with putrefaction
Gangrene Types:
- Dry gangrene – due to slow occlusion of arteries
- Wet gangrene – due to sudden occlusion of arteries
Gangrene Causes
- Arterial occlusion – atherosclerosis, embolism, Raynaud’s disease, Buerger’s disease, cervical rib
- Venous obstruction – deep vein thrombosis
- Nervous disease – peripheral neuritis, hemiplegia, paraplegia
- Traumatic gangrene – direct injury to main artery, indirect injury
- Infective gangrene – carbuncle, cancrumoris, gas gangrene
- Physical gangrene
- Heat – bums and scalds
- Cold – frostbite
- Escharotics – acids and alkalis
- Electricity
- X-ray
Gangrene Treatment
- General treatment
- Nutritious diet
- Control of diabetes
- Relief of pain
- Local treatment
- Conservative
- Affected part is
- Kept dry
- Kept elevated
- Not heated
- Protected from local pressure
- Carefully observed and toileted
- Surgical
- Sympathectomy
- Amputation
- Direct arterial surgery
- In chronic occlusion of artery
Bacterial Infections Short Essays
Question 1. Ludwig’s Angina.
Answer:
Ludwig’s Angina:
Ludwig’s angina refers to rapidly spreading cellulitis involving simultaneously all three spaces – submandibular, sublingual, and submental spaces.
Ludwig’s Angina Etiology:
- Odontogenic infection.
- Traumatic injuries.
Ludwig’s Angina Clinical Features:
- Brawny hard swelling of neck involving all three spaces.
- Reddening of the overlying skin.
- Local rise in temperature.
- Oedema of the floor of the mouth which pushes tongue upwards and results in difficulty in swallowing.
- Dehydration.
- High-grade fever.
- Hoarseness of voice.
- Putrid halitosis.
- Increased salivation.
Ludwig’s Angina Treatment:
- Airway maintenance.
- Administration of antibiotics.
- Pencillin G- 24 million units number 4, 4 – 6 hourly.
- Gentamycin – 80 mg IM BD.
- Metronidazole – 400 mg 8 hourly.
- 4 fluids – to correct dehydration.
- Removal of causative agent.
- Surgical management.
General anaesthesia.
↓
Curved incision over most prominent part of the sub-mandibular gland.
↓
Mylohyoid muscle is divided
↓
Pus is drained.
↓
Irrigate the cavity.
↓
Place drainage tube.
↓
Close the woimd with loose sutures.
Bacterial infection short and long answers
Question 2. Trismus Or Lockjaw.
Answer:
Trismus Or Lockjaw:
Trismus: It is defined as the inability to open the mouth.
Trismus Or Lockjaw Etiology:
- Pericoronitis.
- Inflammation of masseter muscle.
- Peritonsillar abscess.
- TMJ disorders.
- Submucous fibrosis.
- Treatment:
- Treat the cause
- Analgesic – to relieve pain.
- Muscle relaxant – for masseter muscle.
- Hot fomentation.
- Physiotherapy.
Question 3. Boil.
Answer:
Boil Definition: It is an acute staphylococcal infection of a hair follicle with perifolliculitis.
Boil Clinical Features:
- Common on the back and neck.
- Boil of the external auditory meatus is very painful.
- Starts with a painful and indurated swelling.
- Later softening occurs at the centre which leads to pustule formation.
- It burst to discharge a greenish small amount of slough.
- Next a deep cavity develops lined by granulation tissue.
Boil Complication:
- Cellulits:
- Infection of neighboring hair follicles.
- Secondarily infect lymph nodes.
Boil Treatment:
- Improvement of general health of patient.
- Drainage of pus.
- Clean the area with suitable disinfectant.
- Antibiotic cloxacillin is given if necessary.
Question 4. Erysipelas.
Answer:
Erysipelas Definition: It is an acute inflammation of the lymphatics of the skin and mucous membrane.
Erysipelas Etiology: Streptococcus haemolyticus group A is the causative organism.
Erysipelas Clinical Features:
- Poor general health.
- Starts as a rose-pink rash which spreads to adjacent normal skin.
- Vesicles appears which burst to discharge serous secretion.
- Fever
- Toxaemia.
- Oedema of eyelids or scrotum.
- When it involves pinna, it is described as Millian’s ear sign positive.
Erysipelas Complication:
- Gangrene of skin and subcutaneous tissue.
- Septicaemia.
- Rarely lymphoedema.
Erysipelas Treatment:
- Inj. Crystalline penicillin 10 Ink units 6 hourly IM/IV for 5 -10 days.
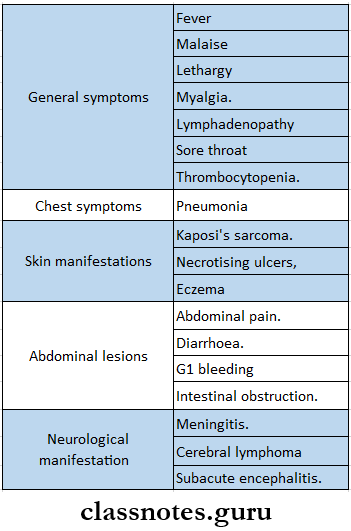
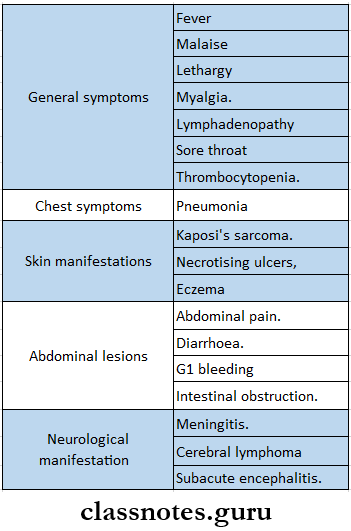
Question 5. HIV or AIDS.
Answer:
HIV or AIDS:
- Human Immunodeficiency virus (HIV) is the causative agent for AIDS (Acquired immune deficiency syndrome).
- HIV has the capability of destroying T-cells and thus harms the entire immune system.
HIV Or AIDS Spread Of Infection:
- Through sexual contact.
- Through blood transfusion.
- From infected mother to foetus.
HIV or AIDS Clinical Features:
- Patients remains asymptomatic for 1 – 2 months.
- Later it may have following symptoms.
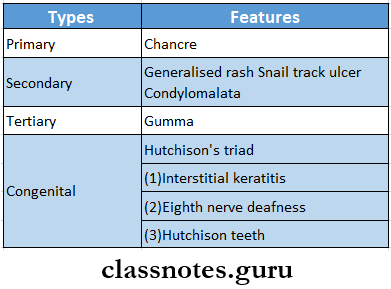
Question 6. Syphilis.
Answer:
Syphilis:
- Syphilis is a venereal disease caused by treponema pallidum.
Syphilis Clinical Features: Disease is divided into four stages.
- Primary syphilis.
- Hard chancre gradually develops at the site of entry of organisms.
- Initially, it appears as a papule which gradually becomes eroded and forms an ulcer.
- Edges of ulcer are raised.
- Surrounding skin is oedematous.
- Occurs over the glans of the penis and coronal sulcus in males and the inner side of the labia minora and cervix in females.
- Extra genital chancres occur in the anal or perianal region, lip, tongue, nipple, etc.
- Regional lymph nodes are involved.
- They are enlarged with a rubbery consistency.
- Secondary syphilis.
- Appears in 2 – 3 months after primary syphilis.
- Produces generalized rash – dull red in color.
- Snail track ulcers appear.
- There are wart-like growths called condylo-malta.
- Generalized painless lymphadenopathy occurs.
- Other symptoms include:
- Sore throat.
- Alopecia.
- Bone and joint pain.
- Hepatitis.
- Malaise
- Headache, backache.
- Pyrexia.
- Tertiary syphilis.
- Affects the blood vessels.
- There is a perivascular collection of lymphocytes and plasma cells.
- Gumma is another characteristic feature.
- It is an accumulation of granulation tissue with central necrosis.
- Latent syphilis.
- It is asymptomatic.
- Serum tests are positive.
Syphilis Treatment:
- Early syphilis.
- Procaine penicillin G 6 lacs units daily for 15 days,
- Late syphilis.
- Procaine penicillin G 6 lacs units daily for 3 weeks.
- Patient is allergic to penicillin.
- Doxycycline 100 mg thrice daily for 15 days.
Question 7. Precautions for surgeons in HIV-infected patients.
Answer:
In OPD:
- Any patient with open wounds, examine after wearing gloves.
- Use disposable instrument.
- Reusable instrument clean with soap and water and immerse in glutaraldehyde.
In The Operating Room:
- Dental chair is covered with single sheet of polythene.
- Minimize the number of personnel in room.
- Any staff member with abrasions or lacerations is not allowed.
- All staff members should wore shoes, gloves, gowns, and protective glasses.
- Use sterilization techniques.
- AZT should be given to health workers following exposure.
Question 8. Active immunity.
Answer:
Active Immunity: Active immunity is the resistance developed by an individual as a result of antigenic stimulus.
Active Immunity Mechanism: it stimulates humoral and cell-mediated immunity.
Active Immunity Types:
- Natural active immunity.
- Acquired by natural subclinical or clinical infectious.
- Artificial active immunity.
- It is produced by vaccination.
- Vaccines are prepared from live, attenuated, or killed micro-organisms or their antigens or toxoids.
- Vaccines stimulate a primary response against the antigen without causing symptoms of the disease.
Question 9. Passive immunity.
Answer:
Active Immunity:
- It is received passively by the host.
- It is induced by preformed antibodies against infective agent or toxin.
- Protection starts immediately after the transfer of immune serum.
- It is short lasting.
Active Immunity Types:
- Natural.
- Transferred from mother to foetus or infants.
- To foetus – transplacentally and to infant through milk.
- Artificial.
- Transferred through parenteral administration of antibodies.
Active Immunity Uses:
- To provide immediate short-term protection in a nonimmune host.
- For suppression of active immunity.
- For treatment of serious infection.
Medical microbiology bacterial diseases Questions & Answers
Question 10. Diagnostic tests for HIV.
Answer:
- Specific Tests:
- Screening Tests.
- ELISA Test.
- Enzyme-linked immunosorbent assay is most widely used test.
- It requires only microlitre quantities of specimen to detect.
- In it an enzyme acts on substrate to produce a color in a positive test.
- Most laboratory uses a commercial ELISA -kit.
- Rapid Tests.
- Requires less than 30 minutes.
- Includes.
- Dot-blot assay.
- Praticle agglutination.
- HIV spot
- Comb tests.
- Supplemental Tests.
- Western Blot Test:
- HIV proteins are separated by electrophoresis.
- These are then blotted on strips of nitrocellulose paper.
- These stips are reacted with test sera.
- Position of the colour band on the strip indicates fragment of antigen with which antibodies have reacted.
- Indirect immunofluorescence test.
- HTV-infected cells are fixed on glass slide.
- Reacted with serum and then with fluoresain conjugated antihuman gammaglobulin.
- Positive test produces apple-green fluorescence.
- Non-Specific Test:
- Total leucocyte count.
- Lymphocyte count is less than 400 per mm3 in AIDS patients.
- T-lymphocyte subset assays.
- In normal individual CD4 : CDS is 2:1
- In AIDS patients -CD4 : CD8 is 0.5:1
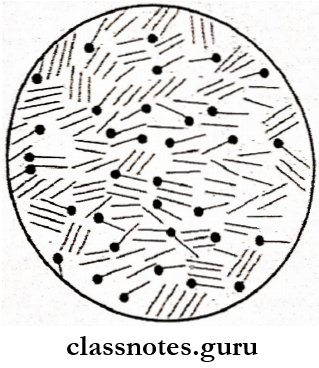
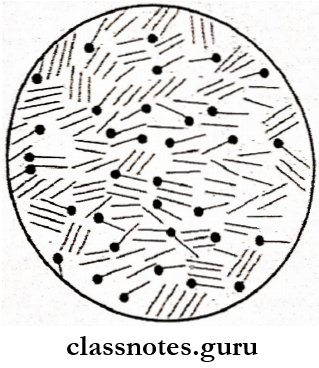
Question 11. Tubercle bacilli/Koch’s bacilli.
Answer:
Tubercle Bacilli:
- Tubercle bacilli is slender, straight or slightly curved bacillus with rounded ends.
- Arrangement – occurs singly, in pairs, or in small clumps.
- Size -1 – 4 pm x 0.2 – 0.8 pm
- They are acid-fast, non-sproing, non-capsulated & non-motile bacilli.
- With Zienl – Neelsen staining, tubercle bacilli are seen bright red in color.
- It is called Koch’s bacilli on the name of its dis- corver.
Tubercle Bacilli Types:
- Human type – M tuberculosis.
- Bovine type – M bovis.
- Vole type – M microti.
- African type – M africanum.
Question 12. Tetanus bacilli.
Answer:
Tetanus Bacilli: Clostridium tetani causes tetanus.
- It is gram-positive, slender bacilli.
- Size- 4 – 8 pm x 0.5 pm
- It has spherical, terminal spores.
- The spore is about 3-4 times wider than the bacillary
- body, giving rise to a drumstick appearance.
- It is non-capsulated and motile with peritrich flagella.
- It is mainly found in manure and soil.
- It is a normal inhabitant of the intestines of human beings and animals.
Question 13. Endotoxins.
Answer:
Endotoxins: Endotoxins are lipopolysaccharides in nature.
- They form an integral part of cell wall of bacteria.
- Produced by gram negative bacteria.
- They are released from the bacterial surface by natural lysis of the bacteria or by the disintegration of the cell wall.
- They are heat stable.
- Is toxicity depends on the lipid component
- They cannot be toxoided.
- Poor antigenic.
- Has no enzymatic action.
- They are non-specific in their action.
- Usually produces fever.
- Thus, this area is called the dangerous area of the face.
Question 14. Septicaemia.
Answer:
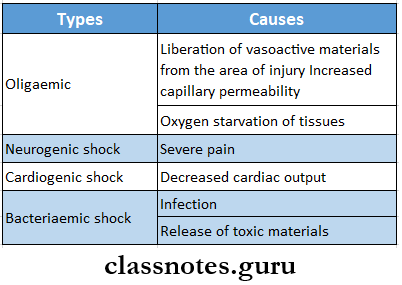
Septicaemia: Septicaemia is a condition in which bacteria circulate and actively multiply in the bloodstream and liberate toxins produced by them.
Septicaemia Clinical Features:
- Pyrexia.
- Rigors
- Hypotension.
- Intravascular coagulation defects.
- Petechial hemorrhages.
- Jaundice due to liver damage.
- Septic shock.
- Peripheral circulatory failure.
- Decrease/Absence 6f Urine output.
Septicaemia Routes of Spread:
- Streptococcus, are main causative organism.
- It spread to other organs by.
- Direct extension into open vessels.
- Release of infected emboli.
- Discharge of infected lymph.
Septicaemia Treatment:
- 4 administration of antibiotics – aminoglycosides and metronidazole.
- Blood transfusion.
- Plasma expanders.
- Inj. Hydrocortisone is given.
Antibiotics used for bacterial infections questions
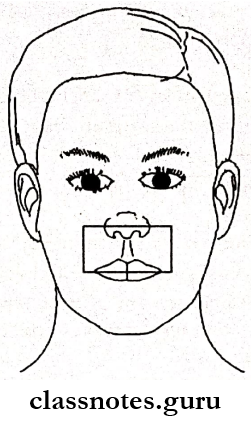
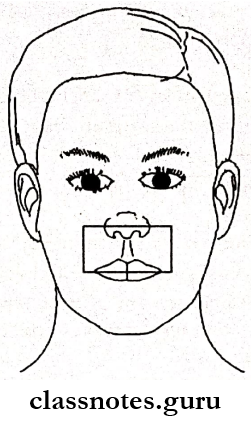
Question 15. Dangerous Area Of Face.
Answer:
Dangerous Area Of Face:
- The area from the corners of the mouth to the bridge of the nose including the nose and maxilla forms the dangerous area of the face.
- The facial vein communicates with the cavernous sinus through communication between the supraorbital and pterygoid plexus via a deep facial vein.
- The cavernous sinus is present in the cranial cavity between the layers of the meninges.
- Infections from the face especially from the upper lip and lower part of the face can spread in a retrograde direction and cause thrombosis of the cavernous sinus.
- Thus this area is called a dangerous area of the face.
Question 16. Boundaries of the back of the neck.
Answer:
Back Of Neck Boundaries:
- Anteriorly – posterior border of sternocleidomastoid.
- Posteriorly – anterior border of trapezius.
- Inferiorly/base-middle third of clavicle.
- Apex lies on the superior nuchal line where the trapezius and sternocleidomastoid meet.
- Roof – investing layer of deep cervical fascia.
- Floor.
- Splenius capitus.
- Levator scapulae.
- Scalenusmedius.
- Back Of Neck Contents.
- Occipital triangle.
- Nerves.
- Spinal accessory.
- Four cutaneous branches of cervical plexus.
- Muscular branches.
- C5, C6 roots of branchial plexus.
- Third and fourth cervical nerves.
- Dorsal scapular nerve.
- Vessels.
- Transverse cervical artery and vein.
- Occipital artery.
- Lymph nodes.
- Subclavian triangle.
- Nerves.
- Three trunks of branchial plexus.
- Nerve to serratus anterior.
- Nerve to subclavius.
- Suprascapular nerve.
- Vessels.
- Third part of subclavian artery and vein.
- Suprascapular artery and vein.
- Commencement of transverse cervical artery and termination of the corresponding vein.
- Lower part of the external jugular vein.
- Lymph nodes.
- Few members of the supraclavicular chain.
- Posteroinferior group of the deep cervical lymph node.
Question 17. TB cervical lymphadenitis.
Answer:
TB Cervical Lymphadenitis:
TB Cervical Lymphadenitis Etiopathogenesis:
1. In the anterior triangle of the neck.
Mycobacteria pass through tonsillar crypts.
↓
Affects tonsillar node or jugulodigastric node.
2. In posterior triangle.
- Lymph nodes are affected due to the involvement of adenoids.
3. Spread from the apex of the lung.
- Organisms penetrate Sibson’s fascia and cause enlargement of supraclavicular nodes.
Question 18. dry gangrene
Answer:
Dry Gangrene:
- Dry Gangrene is a form of gangrene occurring due to ischemia
Dry Gangrene Causes:
- Ischaemia
- Atherosclerosis
- Buerger’s disease
- Raynaud’s disease
- Trauma
- Ergot poisoning
Dry Gangrene Features:
- Begins in the distal part of the limb
- Occurs in one of the toes which is far from the blood supply where bacteria fail to grow
- Spreads slowly upwards
- The line of demarcation is seen between the gangrenous part and viable part as a bright red line
- Color changes from greenish to black due to hemolysis of RBCs
Dry Gangrene Treatment:
- General
- Nutritious diet
- Relief of pain
- Conservative
- Affected part is
- Kept dry
- Kept elevated
- Not heated
- Protected from local pressure
- Carefully observed and toileted
- Surgical
Gram-positive bacterial infections questions
Bacterial Infections Short Answers
Question 1. Cellulitis.
Answer:
Cellulitis Definition: It is a nonsuppurative inflammation spreading along the subcutaneous tissues and connective tissue planes and across interstitial spaces.
Cellulitis Etiology:
- Causative organisms are
- Streptococcus pyogenes.
- Variety of aerobic and anaerobic bacteria.
Cellulitis Clinical features:
- Fever
- Toxaemia.
- Diabetic patient are commonly affected.
- Affected part is warm, swollen and tender.
- Pitting edema with brawny induration is present.
- Enlargement and tenderness of regional lymph nodes.
- Common sites are
Cellulitis Treatment:
- Diabetic control by insulin.
- Rest and elevation of the part.
- Glycerine MgSO4 dressing to reduce edema.
- Antibiotics.
- Crystalline penicillin 10 lac units IM/IV 6 hourly for 5-7 days or.
- Ciprofloxacin 500 mg twice daily.
- If antibiotics fail, incision and drainage of pus are carried out.
Question 2. Complications of cellulitis.
Answer:
Complications Of Cellulitis:
- Abscess
- Necrotizing fasciitis
- Toxaemia.
- Septicaemia.
- Precipitates ketoacidosis.
Question 3. Alveolar abscess.
Answer:
Alveolar Abscess:
- An alveolar abscess is an abscess in the alveolar ridge of the jaw, usually caused by the spread of infection from non-vital tooth.
Alveolar Abscess Clinical Features:
- Dull and constant pain.
- Seen in childhood and early adult life.
- Swelling of the cheek.
- Redness and oedema of overlying mucosa.
- Inflamed and tender regional lymph nodes.
- Complications:
- Osteomyelitis.
- Ludwig’s angina.
Types of bacterial infections with examples
Question 4. Apical abscess/Root abscess.
Answer:
Apical Abscess:
Apical Abscess Definition: It can be defined as a localized, acute or chronic suppurative infection in the periapical region of the tooth.
Apical Abscess Synonyms:
- Dentoalveolar abscess.
- Periapical abscess.
Apical Abscess Clinical features:
- Severe pain in the affected tooth.
- The tooth is non-vital and mobile.
- Swelling and redness of overlying mucosa.
- Extrusion of tooth.
- Fever.
- Localized lymphadenitis.
- Pus discharging sinus may develop.
Question 5. Cold abscess.
Answer:
Cold Abscess: A cold abscess is non-reacting in nature.
- Cold Abscess is a sequel of tubercular infection.
- Cold Abscess occurs due to caseation necrosis of lymph nodes resulting in fluctuant swelling in the neck.
Cold Abscess Clinical features:
- Sites involved.
- Neck and axilla.
- Loin from caries spine.
- Chest wall-side and back.
- Caseation of lymph nodes.
- Nodes are soft and matted.
- Cystic and fluctuant swelling.
- Transillumination is negative.
Cold Abscess Treatment:
- Antitubercular regimen.
- Oblique aspiration,
- Excised as a whole
Question 6. Osteomyelitis
Answer:
Osteomyelitis Classification:
- According to duration and severity,
- Clinical types,
- Acute suppurative
- Primary chronic,
- Secondary chronic,
- Non-suppurative,
- Presence of pm.
- Suppurative,
- Non-suppurative.
Osteomyelitis Treatment:
- Administration of antibiotics,
- Sequestromy,
- Hyperbaric oxygen therapy.
Question 7. Sequestrum.
Answer:
Sequestrum:
- Sequestrum is a fragment of dead tissue usually bone that has separated from healthy tissue as a result of injury/disease,
- Sequestrum is avascular.
Sequestrum Types:
- Primary sequestrum.
- Completely separated from bone,
- Secondary sequestrum.
- Partially separated from bone.
Sequestrum Management:
Bacterial pathogenesis questions and answers
Question 8. Pyaemia.
Answer:
Pyaemia:
Pyaemia is a condition clmmUtfamni by formation of secondary foci of suppuration in various parts of the body by pyogenic bacteria,
- These foci are caused by the lodgement of septic emboli formed as a result of breaking up of an infected thrombus.
- It is occasionally associated with,
- Acute osteomyelitis,
- Acute Inflammation of intracranial sinus,
- Acute bacterial endocarditis.
Question 9. Hilton’s method of drainage.
Answer:
Hilton’s Method Of Drainage:
Hilton’s Method Of Drainage Indication: When there are plenty of important structures Jike nerves and vessels around the abscess cavity.
Hilton’s Method of Drainage Technique:
Incision of skin and subcutaneous tissue on the most prominent and most dependent part,
↓
Sinus forceps is forced through the deep fasica into the abscess cavity,
↓
Blades are gradually opened.
↓
Pus drains out.
↓
Forcep is taken out with jaws open,
↓
Abscess cavity is explored by finger.
Question 10. Tetanus prophylaxis.
Answer:
Tetanus Prophylaxis:
1. Active immunization.
- Tetanus toxoid either as plain toxoid or adsorbed on aluminum phosphate APT is used.
- 0.5 ml is given intramuscularly.
- It is given as DPT vaccine i.e., along with toxoid of diphtheria and pertusis vaccine.
2. Passive immunization.
- Antitetanus toxoid prepared from horse serum is used (ATS).
- 1500 TU is given intramuscularly immediately after wounding.
- To avoid the risk of hypersensitivity, human anti-tetanus immune globulins (HTIG) is used.
- Dose – 250 units.
3. Combined prophylaxis.
- First dose of tetanus toxoid in one site with administration of ATS or HTIG in another arm.
4. Proper debridement of the wound.
5. Penicillin 10 lacs IM twice daily.
Diagnosis and management of bacterial diseases Questions & Answers
Question 11. Gangrene.
Answer:
Gangrene Definition: Gangrene is the death of a portion of the body with putrefaction.
Gangrene Types:
- Dry gangrene.
- Wet gangrene.
Gangrene Causes:
- Arterial occlusion.
- Venous obstruction.
- Nervous diseases.
- Traumatic gangrene.
- Infective gangrene.
- Diabetic gangrene.
- Physical gangrene -Heat, cold.
Question 12. Dry Gangrene.
Answer:
Dry Gangrene: Dry gangrene is a form of gangrene occurring due to ischemia.
Dry Gangrene Causes:
- Ischaemia.
- Atherosclerosis.
- Buerger’s disease
- Raynaud’s disease.
- Trauma.
- Ergot poisoning.
Dry Gangrene Features:
- Begins in the distal part of a limb.
- Occurs in one of the toes which is far from the blood supply where bacteria fails to grow.
- Spreads slowly upwards.
- A line of demarcation is seen between the gangrenous part and the viable part.
Question 13. Actinomycosis.
Answer:
Actinomycosis:
Actinomycosis is a chronic, suppurative granulomatous disease caused by actinomyces Isrealli.
Actinomycosis Clinical Forms:
- Cervicofacial.
- Abdominal form.
- Lungs.
Actinomycosis Treatment:
- In crystalline penicillin initially 10 lakh units once a day for 6-12 months, later 4 lakh units daily.
- Hemicolectomy for abdominal forms.
- Incision and drainage of abscess.
- Excision of sinus.
- Releiving obstruction.
Question 15. Syphilis.
Answer:
Syphilis:
Syphilis is a venereal disease caused by treponema-pallidum.
Syphilis Route of Transmission:
- Sexual contact.
- From mother to foetus.
- Through blood transfusion.
- Through infected needles.
Syphilis Stages:
- Primary syphilis.
- Secondary syphilis.
- Tertiary syphilis.
- Latent syphilis.
Questions on bacterial infections in the human body
Question 16. Congenital syphilis.
Answer:
Congenital Syphilis:
Congenital syphilis occurs in children born of an infected mother.
Congenital Syphilis Features:
- Hutchison’s triad which consists of.
- Hypoplasia of incisor and molar teeth.
- Eight nerve deafness and
- Interstitial keratitis in the eye.
- Mulberry molars with constricted and atrophic cusps.
- Screwdriver-shaped incisor.
- Fissuring and scarring of comer of mouth.
- Frontal bossing.
- Saddle nose.
- Short maxilla with high palatal arch.
- Mandibular prognathism.
- Delayed eruption of teeth.
Question 17. Hutchison’s teeth.
Answer:
Hutchison’s Teeth: It is a characteristic feature of congenital syphilis.
- In it, the affected permanent incisors exhibit tapering of mesial and distal surfaces towards the incisal edge rather than towards the cervical margin.
- This gives a typical screwdriver appearance.
- Such teeth also have a central notch at their incisal edge.
- Hence called Hutchison’s incisors.
- These changes are more pronounced in maxillary central incisors.
Question 18. HIV.
Answer:
HIV:
- The human immune deficiency virus belongs to the family retroviridae.
- It causes AIDS.
HIV Morphology:
- HIV is a spherical enveloped virus.
- Size – 90 – 120 nm in diameter.
- The envelope contains projecting spikes.
- HIV contains two identical copies of the single-stranded RNA genome.
- The core is surrounded by a nucleocapsid composed of proteins.
HIV Modes of Transmission:
- Sexual contact.
- From mother to fetus or infant.
- Parenteral transmission.
- Blood transfusion.
- Contaminated needles and syringes.
- Intravenous drug abusers.
Question 19. Orbital cellulitis.
Answer:
Orbital Cellulitis: When cellulitis affects the eyes, it is called ocular cellulitis.
Orbital Cellulitis Forms:
- Periorbital.
- Orbital.
Orbital Cellulitis:
- It is an infection of the soft tissue in the eye socket.
- The disease starts in the ethmoid sinus arid the infection spreads into the subperiosteal lining of the orbit.
- It can cause permanent damage to eye.
- It is more common in children above 5 years.
- In severe cases, the infection can spread to the optic nerve, causing impaired vision.
Orbital Cellulitis Causes:
- Bacterial or fungal infections of the sinuses.
Question 20. Active immunity.
Answer:
Active Immunity:
Active immunity is the resistance developed by an individual as a result of antigenic stimuli.
Active Immunity Types:
- Natural.
- Acquired by natural subclinical or clinical infections.
- Artificial
Bacterial infection case-based questions
Question 21. Pressure sores/bedsores/Decubitus ulcer.
Answer:
Pressure Sores:
Pressure sores appear on the points of pressure when a patient is long bedridden. It occurs on the skin covering bony areas.
Pressure Sores Sites Involved:
Pressure Sores Cause:
- Undue pressure on the part.
- Lying in certain areas for long periods.
- Thinner skin is present next to bone or cartilage.
Pressure Sores Predisposing Factors:
- Old age.
- Sensory loss of the part.
- Malnutrition.
- Moisture.
- Anaemia.
- Improper nursing.
Pressure Sores Features:
- Discoloration of the skin.
- Pain in the affected area.
- Infection.
- Open skin.
- The skin may be softer or firmer than the surrounding skin.
Question 22. Cross Infection.
Answer:
Cross Infection:
Cross-infection refers to the transmission of a pathogenic organism from one person to another. When it occurs in hospitals, it is called nosocomial infection.
Cross Infection Causes:
- Streptococcal infection.
- Viral hepatitis.
- Fecal-oral infections
- Fungal infections.
Cross Infection Prevention:
- Maintain good personal hygiene
- Better sanitation.
- Better Nursing.
Question 23. Epltaxls.
Answer:
Epltaxls:
- Epltaxls is nasal bleeding.
Epltaxls Causes:
- Trauma.
- Exposure to warm, dry air for long time.
- Nasal and sinus infections.
- Allergic rhinitis.
- Nasal foreign body.
- Vigorous nose blowing.
- Deviated nasal septum.
- Cocaine use.
- Use of anti-coagulant.
- Hypertension.
- Bleeding disorders.
Antibiotic resistance questions and answers
Question 24. Antibiotic.
Answer:
Antibiotic:
- Antibioma is antibiotic-induced swelling.
- Due to continuous administration of antibiotics given after abscess formation, the following changes occurs.
- Wall becomes fibrosed.
- Pus becomes sterile.
- Whole mass becomes firm.
- This condition is known as antibioma.
Antibiotic Sites involved:
- Breast
- Thigh
- Ischiorectal fossa.