Epidemiological Methods Definitions
Epidemiology
- Epidemiology is defined as the study of the distribution & determinants of health-related states or events in specified populations and the application of this study to the control of health problems
Incidence
- Incidence is defined as the number of new cases of a specific disease occurring in a defined population during a specified time
Prevalence
- The total number of all individuals who have an attribute or disease at a particular time divided by the population at risk of having the attribute or disease at this point in time or midway through the period
Matching
- Matching is defined as the process by which we select controls in such a way that they are similar to cases with regard to certain pertinent selection variables which is known to influence the outcome of the disease and which if not adequately matched for comparability could distort or confound the results.
Read And Learn More: Percentive Communitive Dentistry Question And Answers
Cohort
- A cohortis defined as a group of people who share a common characteristic or experience within a defined time period
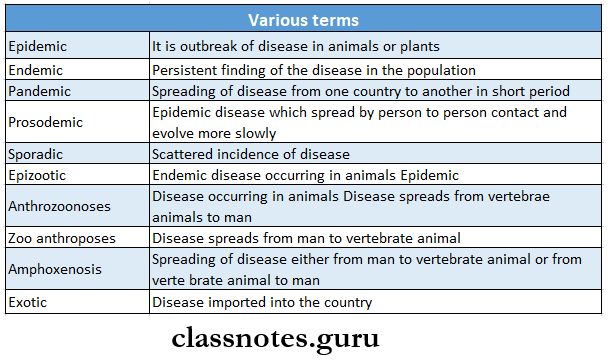
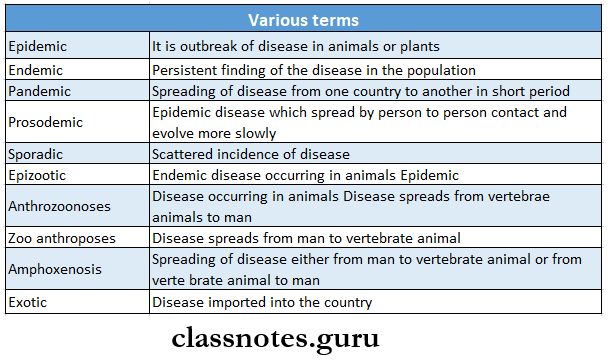
Epidemic
- It is an unusual occurrence in a community or region of disease, specific health-related behavior, or other health-related events clearly in excess of excepted occurrence.
Epidemiological Methods Questions And Answers
Pandemic
- A pandemicis an epidemic usually affecting a large proportion of the population and occurring over a wide geographic area such as a nation, a continent, or a world
Attributable risk
- Attributable risk is the difference in incidence rates of disease between an exposed group and a nonexposed group
Endemic
- Endemic is the constant presence of a disease or infectious agent within a given geographic area or population group without importation from outside.
Epidemiological Methods Important Notes
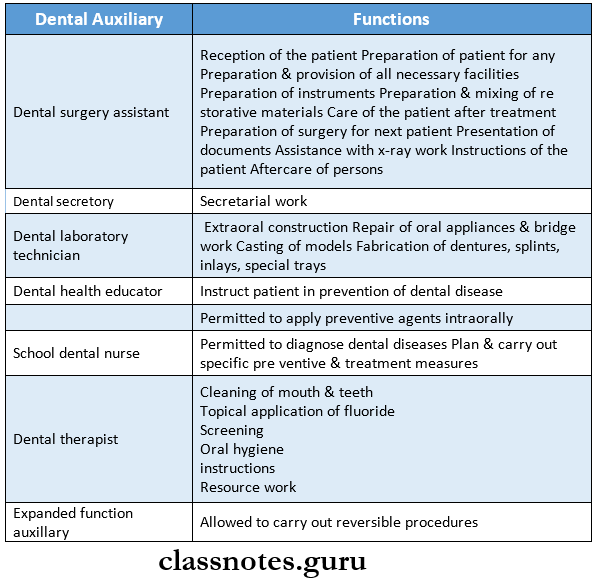
1. Classification of epidemiology:
- Descriptive
- Analytical
- Ecological study
- Cross-sectional
- Case-control
- Cohort study
- Experimental
2. Types of study
3. Odds ratio
- Odds ratio is an indirect method of estimating the relative risk
- Odds ration = \(\frac{\begin{array}{c}\text { Exposed with disease } \times \\\text { unexposed without disease }\end{array}}{\begin{array}{c}\text { Exposed without disease } \times \\\text { unexposed with disease }\end{array}}\)
- The odds ratio is used for case-control studies
- The odds ratio takes a value between zero to infinity.
- Derived from case-control studies
- An odds ratio of 2.25 means that the risk of oral cancer is 2.25 times higher in people who smoke than those who do not smoke
4. Blinding is done to reduce bias
- Blinding is done to reduce bias can be done in 3 ways
- Single-blind trial
- Single-blind trial is so planned that the participants are not aware whether they belong to the study group or control group
- Double-blind trial
- Double-blind trial is so planned that neither the doctor nor the participants know to which group of patients are given drugs and which group is given a placebo
- Double-blind trial is the most frequently used method of blinding.
- Triple blind trial
- In this, the participant, investigator, and the person analyzing the data are all blind
5. Tools of measurement in epidemiology
- Rates – It is the frequency of a disease expressed per unit size of a population or group in which it is observed.
- Ratio – Denotes the relation in size between two random quantities
- Proportions – it is a ratio that expresses the relation in the magnitude of art of the whole. Expressed in percentage.
6. Principles of epidemiology
- Exact observation
- Correct interpretation
- Rational explanation
- Scientific construction
7. Basic measurements in epidemiology
- Measurement of mortality
- Measurement of morbidity
8. Epidemiological methods
- Descriptive epidemiology
- Analytical epidemiology
- Experimental epidemiology
9. Attributable risk
- Derived from a cohort study
- Expressed as percentage
- Indicates to what extent the disease under study can be attributed to exposure.
Observational Studies In Epidemiology
10. Relative risk
- Relative risk is the ratio between incidence among exposed and incidence among non-exposed
- Relative risk is a direct measure of the strength of the association.
11. Various terms
Epidemiological Methods Long Essays
Question 1. Define epidemiology. Write about its principles. Discuss briefly the agent and host factor in periodontal disease.
Answer:
Epidemiology Definition:
Epidemiology is defined as the study of the distribution & determinants of health-related states or events in specified populations and the application of this study to the control of health problems
Epidemiology Principles:
- Exact observation- strict, vigorous, accurate, precise
- Correct interpretation- free from error
- Rationale explanation- intelligent, sensible
- Scientific construction- by expert knowledge & technical skill
Read And Learn More: Percentive Communitive Dentistry Question And Answers
Epidemiology Of Periodontal Disease:
Epidemiology Agent:
- Dental plaque
- Dental plaque is a primary etiological factor for periodontal disease
- Dental plaque is defined as a structured, resilient, yellow-grayish substance that adheres tenaciously to the intraoral hard surfaces, including removable and fixed restoration
- Dental plaque is composed of bacteria in a matrix of salivary glyphosate in and extracellular polysaccharides
- Dental plaque is because of this matrix, that it cannot be removed by rinsing
- Classified into
- Supragingival plaque: at or coronal to marginal gingiva
- The agent is responsible for gingivitis
- Subgingival plaque: apical to gingival margin
- The agent is responsible for calculus & root caries
- Accumulation of plaque is found more on the gingival 1/3rd of the tooth surfaces, cracks, pits, and fissures, over-hanging restoration & around malaligned teeth
- Calculus
- Calculus is a hard-to deposit that forms by mineralization of dental plaque and is usually covered by a layer of unmineralized plaque
- Calculus is classified into
- Supragingival calculus
- Located coronal to the gingival margin
- Supragingival calculus is white or whitish-yellow
- Supragingival calculus has a hard, clay-like consistency
- Supragingival calculus can be easily detached from the tooth
- Subgingival calculus
- Supragingival calculus is located below the crest of the marginal gingiva
- Supragingival calculus is a dark brown or greenish black
- Supragingival calculus is hard and dense
- Supragingival calculus is firmly attached to the tooth structure
- Calculus provides a fixed nidus for the continued accumulation of plaque
Epidemiology Host Factors:
Age:
- The prevalence of periodontal disease increases with age due to the cumulative progression of the lesions over time
Gender:
- Based on epidemiological studies, the prevalence and severity are higher in males than in females
Race:
- Blacks are more affected than the whites
Epidemiology Socioeconomic Status:
- Lower socioeconomic status results in poor diet, poor oral hygiene, and a general lack of dental awareness
- Whereas those who are well-educated, wealthier, and live in better circumstances visit dentists frequently
- Thus periodontal disease prevalence increases in low socioeconomic status
Epidemiology Diet And Nutrition:
- Sticky foods adhere to the teeth and are difficult to remove thus interfering with the natural cleansing mechanism and leading to periodontal disease
- The nutrients associated with periodontal tissues are vitamin A, B complex, C, D, calcium, and phosphorous
- Prevalence and severity of periodontal disease increases in protein malnutrition and vitamin A deficient
Epidemiology Anatomy:
- The normal contour of the tooth protects the underlying tissues
Epidemiology Tooth:
- Sharp cusps, uneven marginal ridges, lack of contact between teeth, and crowding can cause food impaction
Epidemiology Soft Tissue:
- When the frenum is inserted close to the marginal gingival, the pull of attachment may cause recession of the papilla along with interfering with the proper use of a toothbrush
Epidemiology Habits:
- Thread biting, holding nails between teeth, bruxism, lip, cheek, and nail-biting can cause traumatic effects on the periodontium
Epidemiology Mechanical:
- Faulty toothbrushing causes abrasion or recession of the gingival tissues
- Faulty restoration impinges on gingival and irritates them
- Faulty orthodontic treatment results in root resorption as well as alveolar bone loss and Mobility
Epidemiology Chemical:
- Alcohol, tobacco, and condiments lower tissue resistance and increase susceptibility to gingivitis and periodontitis
Epidemiology Atmospheric:
- Because of obstruction in the nasal passage patient breath from the mouth leading to dehydration of the mucous membrane
- Atmospheric lowers tissue resistance
Epidemiology Systemic factors:
- Systemic diseases act locally to reduce the resistance to periodontal destruction and the local periodontal pathogens act systemically to produce an impact on the general health
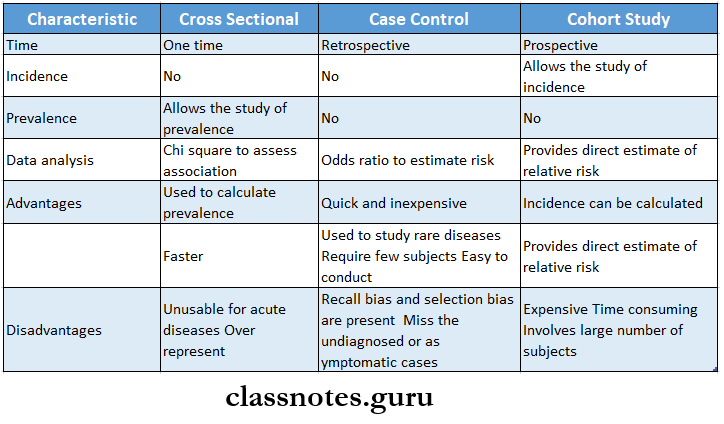
Descriptive And Analytical Epidemiology
Question 2. Describe in brief the types of epidemiology studies.
Answer:
Types Of Epidemiological Studies:
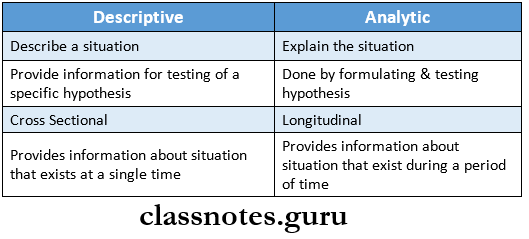
Descriptive Epidemiology:
- Descriptive Epidemiology is usually the first step in an epidemiological study
- Descriptive Epidemiology is concerned with the observation of the distribution of the disease or any health-related events in the human population and the identification of the characteristics with which the disease or condition under study seems to be associated
- Descriptive Epidemiology is used for the quantification of the disease status of the community
- The steps involved in it are
- Defining the population to be studied
- Defining the disease under study
- Describing the disease in terms of
- Measurement of the disease
- Compared with known indices
- Formulating an etiological hypothesis
Analytical Epidemiology:
- The focus here is the individual within the population
- Analytical Epidemiology is designed primarily to establish the causes of disease by investigating the association between exposure to a risk factor and the occurrence of disease
- The objective is to test the hypothesis
- Types
- Case-control study
- Cohort study
Experimental Epidemiology:
- Experimental Epidemiology is carried out under the direct control of the investigator
- Experimental Epidemiology involves some actions, interventions,s or manipulation in the experimental group while making no change in the control group
- Next, compare the outcome of the experiment in both groups
- Types
- Randomized controlled trials
- Non-randomized trials
Question 3. Describe the uses of epidemiology.
Answer:
Uses Of epidemiology:
- Community Diagnosis
- This consists of the collection, description, and analysis of information on the occurrence and distribution of disease in the population about characteristics of the agent, host, and environment
- The importance of the disease is usually determined by the extent of the incidence, prevalence, and mortality by age, sex, race, nativity, marital status, geographic area, temporal variation, and socioeconomic status
- Rise and fall of the disease
- It is done through repeated evaluation of the health care related matters
- Due to this, some diseases pale out in history while new ones emerge
- The seasonal nature of the disease may be revealed
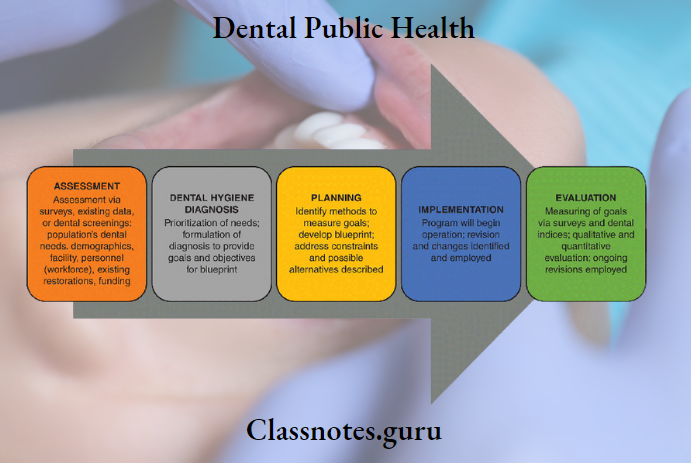
- Planning and Evaluation
- Planning is essential for a rational allocation of limited resources
- Evaluation is done to find out whether the measures undertaken to prevent disease are effective in reducing the frequency of the disease
- Evaluation of individual risk
- The purpose of this is to estimate the probable chances that certain types of individuals will, under certain conditions, suffer from specific illnesses, de- fects, or accidents
- It is also an estimate of the probabilities of life and death expectancy
Question 4. Describe steps in descriptive epidemiology.
Answer:
Steps In Descriptive Epidemiology:
Defining The Population to Be Studied:
- The population has to be defined in terms of the total number and the composition of the individuals within the population in terms of characteristics such as age, sex, occupation, culture, socio-economic status
- The defined population can either be the total population in a geographic area or a representative sample taken from the population
- The defined population provides a denominator for calculating rates
- The population of the community selected for the study should always remain stable, without any migration into or out of the area
Defining The Disease Under Study:
- It should be precise and valid to enable the investigator to identify those who have the disease from those who do not
- The disease needs to be defined with an operational definition which is a definition with which the disease or condition can be identified and measured in the fined population with a degree of accuracy
- The diagnostic methods adopted for the study should be acceptable and applicable to the population to be studied
Describing the Disease Under Study:
This step is used to describe the occurrence and distribution of the disease by the time of its occurrence, the place of occurrence, and the persons who are affected by the disease
1. Time Distribution:
- Time may be measured in terms of hours, days, weeks, months, years, etc.
Time Distribution Types:
- Short-term fluctuation ex. Epidemic
- Common source epidemic
- A single exposure or point source epidemic. Ex. Food poisoning
- Continuous or multiple exposure. Ex. Contaminated water
- Person-to-person transmission
- Arthropod vector
- Animal reservoir
- Periodic fluctuation
- Seasonal trends: example: Measles and varicella
- Cyclic trends.
- Certain diseases appear in cycles, which may spread over short periods like days, weeks, months, or years
- Example: Automobile accidents
- Long term fluctuation
- Implies changes in disease occurrence over a long period, generally several years.
Example: Lung cancer
2. Place Distribution:
- Variation in the frequency of different diseases from place to place has long been identified
- International variation
- There exist differences in the incidence of various diseases in different parts of the world
- Example: Stomach cancer is very common in Japan and unusual in the USA
- National variation
- Distribution of endemic goiter, fluorosis, leprosy, and malaria have shown variation in their distribution in India
- Urban and rural variation
- Chronic bronchitis, lung cancer, and CVS disorder are more common in urban than rural areas Local distribution
- Inner and outer city variations in disease frequency are well-known
3. Person Distribution:
- The factors that influence the disease pattern in an individual are
- Age: certain diseases are more frequent in certain age groups
- Sex: obesity is common in females while lung cancer in males
- Ethnicity
- Marital status
- Occupation
- Social class
- Behavior
- Stress
- Migration
Measurement Of Disease:
- The measurement of disease is done in terms of mortality and morbidity indicators
- The morbidity is expressed in terms of incidence and prevalence
Comparing With Known Indices:
- It helps to conclude about the disease etiology
- Identify groups and subgroups which are potentially at high risk for the development of certain diseases
Formulation Of An Etiological Hypothesis:
- Formulation Of An Etiological Hypothesis is defined as ” a supposition arrived at by observation or by reflection”
- The formulation Of An Etiological Hypothesis can be tested using the techniques of analytical epi- epidemiology after which it may be accepted or rejected
- Formulation Of An Etiological Hypothesis should specify the population, specific cause, ex-expected outcome, dose-response relationship, and time response relationship
Cohort Study Vs Case-Control Study
Question 5. What are the aims of epidemiology? Explain. It is defined as the process by which we select control case-control studies in detail.
Answer:
Aims Of Epidemiology:
- To describe the size and distribution of the disease problems in the human population
- To provide the data essential for the planning, implementation, and evaluation of health services for the pre-prevention, control, and treatment of diseases and for setting up priorities among those services
- To identify etiological factors in the pathogenesis of disease
Epidemiology Features:
- Both exposure and outcome occurred before the start of the disease
- The study proceeds from effect to cause
- Epidemiology uses a control or comparison group to support to refuse a hypothesis
Epidemiology Steps:
Epidemiology Selection Of Cases And Controls:
- Selection of cases
- Definition of a case
- Diagnostic criteria: the diagnostic criteria of the disease Epidemiology and the stage of the disease to be included in the study must be specified before the study is under- taken
- Eligibility criteria: only newly diagnosed cases within a specified period are eligible than old cases or cases in advanced stages of disease
- Sources of cases
- Hospitals
- General population
- Selection of controls
- The control must be free from disease under study
- They must be as similar to the case as possible
- Sources of control
- Hospital
- Relatives
- Neighborhood
- General population
- Number of control
- If many cases are available and a large study is contemplated, one tends to use one control for each
- case
- If the study group is small, 2,3 or even 4 controls can be selected for each study subject
Epidemiology Matching:
- In such a way that they are similar to cases about certain pertinent selection variables which is known to influence the outcome of the disease and which if not adequately matched for comparability could distort or confound the results
- While matching it should be borne in mind that the suspected etiological factor or the variable we wish to measure should not be a match
Epidemiology Types:
- Group matching
- Pair matching
Epidemiology Measurement Of Exposure:
- Obtained by
- Interviews
- Questionnaires
- Records
- Clinical or laboratory examination
Epidemiology Analysis:
- Final step
- It is to find out
- Exposure rates among cases and controls to suspected factor
- Estimation of disease risk associated with exposure
Epidemiology Advantages:
- Easy to carry out
- Rapid and Inexpensive
- Few subjects are required
- Rare diseases can be studied
- No risk to subjects
- Allows study of several etiological factors
- Risk factors can be identified
- No attrition problems
- Minimal ethical problems
Epidemiology Disadvantages:
- Problem of bias
- Selection of appropriate control group
- Incidence cannot be measured
- Not distinguishing between causes and associated factors
- Not suited to the evaluation of therapy
- The concern is the representativeness of cases and controls
Epidemiological Study Designs
Epidemiological Methods Short Essays
Question 1. Uses of epidemiology.
Answer:
Epidemiology Community Diagnosis:
- This consists of the collection, description, and analysis of information on the occurrence and distribution of disease in the population about characteristics of the agent, host, and environment
- The importance of the disease is usually determined by the extent of the incidence, prevalence, and mortality by age, sex, race, nativity, marital status, geographic area, temporal variation, and socio-economic status
Epidemiology Rise And Fall Of The Disease:
- The rise and fall of the disease is done through repeated evaluation of the health. It occurs when other factors that are associated with care-related matters
- Due to this, some diseases pale out in history while new ones emerge
- The seasonal nature of the disease may be revealed
Epidemiology Planning And Evaluation:
- Planning is essential for a rational allocation of the differences in admission rates and resources
- Evaluation is done to find out whether the measures undertaken to prevent a disease are effective in reducing the frequency of the disease
Evaluation Of Individual Risk:
- The purpose of this is to estimate the probable chances that certain types of individuals will, under certain conditions, suffer from specific illnesses, defects, or accidents
- Individual risk is also an estimate of the probabilities of life and death expectancy
Question 2. Bias in case-control studies.
Answer:
Selection Bias:
- Selection Bias occurs when a group studied does not reflect the same characteristics like age, sex, occupation, race, etc as in the general population
- Selection Bias can be reduced by careful selection of individuals for inclusion in the study
- The selection bias can be best controlled by the prevention
Information Bias:
- Information Bias occurs when there is an error in the classification of individuals concerning the outcome variable
Confounding Bias:
- The outcome and exposure variables do not have the same distribution in the exposed and unexposed groups
- Confounding Bias can be removed by matching
Berkesonian Bias:
- Of people in hospitals with different diseases
Interviewer’s Bias:
- Interviewer’s Bias occurs when the interviewer knows the hypothesis and also knows who the cases are
Memory Bias:
- When the cases and controls are asked questions about their history it may be more likely for the cases to recall the existence of certain events or factors than the controls who are healthy persons
Telescopic Bias:
- If a question refers to the recent past, episodes that occurred longer ago may also be reported
Prevalence-Incidence Bias:
- If the exposure occurred years before, then mild cases that improved or severe cases that died would have been missed and not counted among the cases
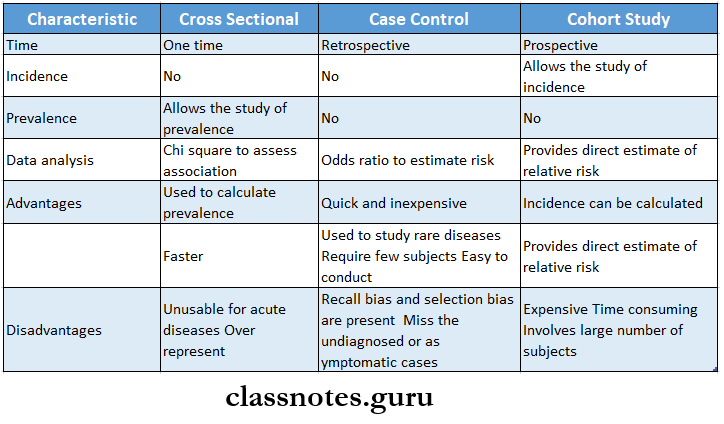
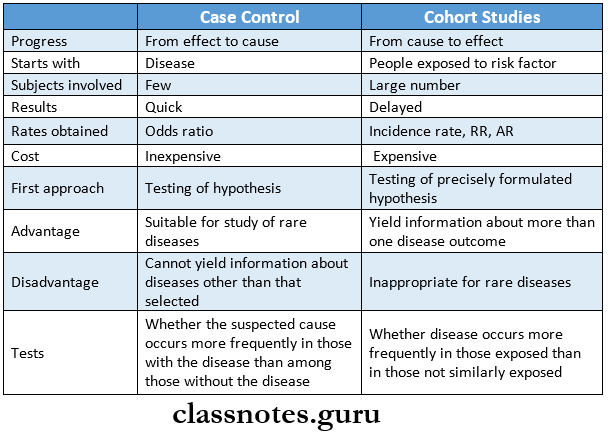
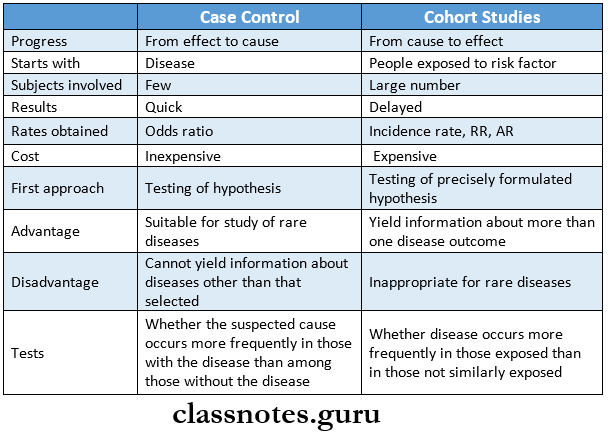
Question 3. Comparison of case-control and cohort studies.
Answer:
Comparison Of Case-control And Cohort Studies
Question 4. Incidence and prevalence.
Answer:
Incidence:
- Incidence is defined as the number of new cases of a specific disease occurring in a defined population during a specified period
- Incidence can range from zero to infinity
- Incidence can be represented by the formula
- Number of new cases of specific disease during a given period x 1000
The Population At Risk:
Incidence Types:
- Episode incidence
- Episode incidence is the rate of occurrence of new episodes of a disease Identify the potential high-risk population
- Cumulative incidence
- Similar to incidence the time interval is expressed as a fixed period.
Incidence Uses:
- Provide a clue for the etiology and pathogenesis of the disease
- Study the distribution of the study
- Control the disease
- Evaluate the efficacy of preventive and therapeutic measures.
Incidence Significance:
- Indicative of failure or preventive program
- Suggest the need for a new disease control program
- Suggest a change in the etiology of the disease
Prevalence:
- The total number of all individuals who have an attribute or disease at a particular time divided by the population at risk of having the attribute or disease at this point or midway through the period
Prevalence Types:
- Point prevalence
- It is the number of all current cases of a specific disease at one point in time with a defined population
- Period prevalence
- It is defined as the total number of existing cases of a specific disease during a defined period ex- pressed concerning a defined population
Prevalence Uses:
- Estimate the magnitude of disease or health problems in the community
- the disease under investigation
- Useful in administrative and planning purposes like assessing manpower needs in health services, etc
Relation Between Incidence and Prevalence:
- Prevalence is dependent on the incidence and duration of the disease
- Prevalence = incidence x Mean duration
- (P=IxD)
- Relation Between Incidence and Prevalence reveals that as the duration of the disease increases, the greater will be its prevalence
- Changes in prevalence from one time to another can result from changes in incidence, changes in duration of disease or both
Experimental Studies In Epidemiology
Question 5. Cohort studies.
Answer:
Cohort Studies
- Prospective study
- Longitudinal study
- Incidence study
- Forward-looking study
Cohort Studies Features:
- The cohorts are identified before the appearance of
- The study groups are observed over some time to determine the frequency of the disease among them
- The disease proceeds forward from cause to effect
Cohort Studies Indications:
- When a good association occurs between exposure and disease
- When exposure is rare
- When attrition of the study population can be minimized
- When ample funds are available
Cohort Studies Types:
- Prospective
- Retrospective
- Combination
Cohort Studies Elements:
- Selection of study subjects
- Obtaining data on exposure
- Selection of comparison group in terms of
- Internal comparison
- External comparison
- Comparison with general population rates
Question 6. Blinding.
Answer:
Blinding
- In order to reduce the problem of bias a technique called blinding is adopted
- It can be done in three ways
- Single-blind trial
- The trial is so planned that the participant is unaware of whether he belongs to the study group or the control group
- Double-blind trial
- The trial is so planned that neither the investigator nor the participant is aware of the group allocation and the treatment received
- The most frequently used method
- Triple blind trial
- The participant, the investigator, and the person analyzing the data are all blind
- Ideally used method
Question 7. Case-control studies
Answer:
Case-Control Studies
Case-Control Studies Features:
- Both exposure and outcome occurred before the start of the disease
- The study proceeds from effect to cause
- It uses a control or comparison group to support to re-fuse a hypothesis
Selection Of Cases And Controls:
- Selection of cases
- Definition of a case
- Diagnostic criteria: the diagnostic criteria of the disease and the stage of the disease to be included in the study must be specified before the study is under- taken
- Eligibility criteria: only newly diagnosed cases within a specified period of time are eligible than old cases or cases in advanced stages of disease
- Sources of cases
- Hospitals
- General population
- Selection of controls
- The control must be free from disease under study
- They must be as similar to the case as possible
- Sources of control
- Hospital
- Relatives
- Neighbourhood
- General population
- Number of control
- If many cases are available and a large study is contemplated, one tends to use one control for each case
- If the study group is small, 2,3 or even 4 controls can be selected for each study subject
Case-Control Studies Matching:
- Case-control studies Matching is defined as the process by which we select controls in such a way that they are similar to cases with regard to certain pertinent selection variables which is known to influence the outcome of the disease and which if not adequately matched for comparability could distort or confound the results
- While matching it should be borne in mind that the suspected etiological factor or the variable we wish to measure should not be a match
Case-Control Studies Types:
- Group matching
- Pair matching
Case-Control Studies Measurement Of Exposure:
- Obtained
- Interviews
- Questionnaires
- Past records
- Clinical or laboratory examination
Case-Control Studies Analysis:
- Final step
- Case-control studies Analysis is to find out
- Exposure rates among cases and controls to suspected factor
- Estimation of disease risk associated with exposure
Case-Control Studies Advantages:
- Easy to carry out
- Rapid and Inexpensive
- Few subjects are required
- Rare diseases can be studied
- No risk to subjects
- Allows study of several etiological factors
- Risk factors can be identified
- No attrition problems
- Minimal ethical problems
Case-Control Studies Disadvantages:
- Problem of bias
- Selection of appropriate control group
- Incidence cannot be measured
- Not distinguishing between causes and associated factors
- Not suited to the evaluation of therapy
- The concern is the representativeness of cases and controls
Types Of Epidemiological Studies
Question 8. Descriptive epidemiology.
Answer:
Descriptive Epidemiology Steps:
Defining The Population To Be Studied:
- The population has to be defined in terms of the total number and the composition of the individuals within the population in terms of characteristics such as age, sex, occupation, culture, socio-economic status
- The defined population can either be the total population in a geographic area or a representative sample taken from the population
- The defined population provides a denominator for calculating rates
- The population of the community selected for the study should always remain stable, without migration into or out of the area
Defining The Disease Under Study:
- The Disease should be precise and valid to enable the investigator to identify those who have the disease from those who do not
- The disease needs to be defined with an operational definition which is a definition with which the disease or condition can be identified and measured in the fined population with a degree of accuracy
- The diagnostic methods adopted for the study should be acceptable and applicable to the population to be studied
Describing The Disease Under Study
- This step is used to describe the occurrence and distribution of the disease by the time of its occurrence, the place of occurrence, and the persons who are affected by the disease
Time Distribution:
- Time may be measured in terms of hours, days, weeks, months, years, etc.
- Types
- Short-term fluctuation ex. Epidemic
- Common source epidemic
- A single exposure or point source epidemic. Example: Food poisoning
- Continuous or multiple exposure. Example: Contaminated water
- Propagated epidemic
- Person-to-person transmission
- Arthropod vector
- Animal reservoir
- Periodic fluctuation
- Seasonal trends: ex. Measles and varicella
- Cyclic trends.
- Certain diseases appear in cycles, which may spread over short periods of time like days, weeks, months, or years Example: Automobile accidents
- Long term fluctuation
- Implies changes in the occurrence of disease over a long period of time, generally several years.
- Example: Lung cancer
Place Distribution:
- Variation in the frequency of different diseases from place to place has long been identified
- There exist differences in the incidence of various diseases in different parts of the world
- Example: Stomach cancer is very common in Japan and usual in the USA
- National variation
- Distribution of endemic goiter, fluorosis, leprosy, and malaria have shown variation in their distribution in India
- Urban and rural variation
- Chronic bronchitis, lung cancer, and CVS disorder are more common in urban than rural areas
- Local distribution
- Inner and outer city variations in disease frequency are well-known
Person Distribution:
- The factors that influence the disease pattern in an individual are
- Age:
- certain diseases are more frequent in certain age groups
- Sex: obesity is common in females while lung cancer in males
- Ethnicity
- Marital status
- Occupation
- Social class
- Behavior
- Stress
- Migration
Measurement Of Disease:
- The measurement of disease is done in terms of mortality and morbidity indicators
- The morbidity is expressed in terms of incidence and prevalence
Comparing With Known Indices:
- Comparing With Known Indices helps to conclude the disease. The total number of all individuals who have an attrib- etiology
- Identify groups and subgroups which are potentially at high risk for the development of certain diseases
Formulation Of An Etiological Hypothesis:
- Formulation Of An Etiological Hypothesis is defined as “a supposition arrived at by observation or by reflection”
- The formulation Of An Etiological Hypothesis can be tested using the techniques of analytical epi- epidemiology after which it may be accepted or rejected
- V should specify the population, specific cause, and example. pected outcome, dose-response relationship and
- time response relationship
Principles Of Epidemiological Methods
Question 9. Case-control studies
Answer:
Case-Control Studies
- In it, the same individuals are examined on repeated occasions over a prolonged period using follow-up examination
Case-Control Studies Uses:
- Study the natural history of the disease & its outcome
- Identify the risk factor associated with the disease
- Calculate the incidence rates of the disease
Case-Control Studies Disadvantage:
- Difficult to organize
- More time consuming
Epidemiological Methods Short Question And Answers
Question 1. Attributable risk (AR).
Answer:
Attributable risk (AR)
- Attributable risk is often expressed as a percent
- Attributable risk indicates to what extent the disease under study can be attributed to the exposure
- AR= Incidence of disease rate among exposed Inci- dence of disease rate among non-exposed/Incidence rate among exposed
Question 2. Cohort Studies.
Answer:
Cohort Studies Features:
- The cohorts are identified prior to the appearance of the disease under investigation
- The study groups are observed over a period of time to determine the frequency of the disease among them
- The disease proceeds forward from cause to effect
Cohort Studies Indications:
- When a good association occurs between exposure & disease
- When exposure is rare
- When attrition of the study population can be minimized
- When ample funds are available
Cohort Studies Types:
Question 3. Cohort.
Answer:
Cohort
- Thus a group of people born on the same day or in the same period of time form a “birth cohort”
- which the cohort is derived or it may be another cohort. It can be represented by the formula little or no exposure to the substance in question
Question 4. Single-blind trial.
Answer:
Single-Blind Trial
- In order to reduce the problem of bias a technique called blinding is adopted
- Single-blind trial
- The trial is so planned that the participant is unaware of whether he belongs to the study group or the control group
Question 5. Long-term/secular trends.
Answer:
Long-Term/Secular Trends
- It refers to changes in disease frequency that occur gradually over a long period of time generally several years or decades
- Examples: Coronary heart disease, lung cancer & diabetes
- Oral cancer has shown a consistent upward trend during the last 50 years in developed countries
Question. 6. Prevalence.
Answer:
Prevalence
The total number of all individuals who have an attribute or disease at a particular time divided by the population at risk of having the attribute or disease at this point in time or midway through the period
Prevalence Types:
- Point prevalence
- It is the number of all current cases of a specific disease at one point in time in relation to a defined population
- Period prevalence
- It is defined as the total number of existing cases of a specific disease during a defined period of time expressed in relation to a defined population
Prevalence Uses:
- Estimate the magnitude of disease or health problems in the community
- Identify the potential high-risk population
- Useful in administrative & planning purposes like assessing manpower needs in health services, etc
Question 7. Parkinsonian Bias.
Answer:
Parkinsonian Bias
- Parkinsonian Bias is named after Dr. Joseph Berkson
- Parkinsonian Bias arises when there are differences in admission rates of people in hospitals with different diseases
- The causes of bias include the burden of symptoms, ac- TELESCOPIC BIAS: cess to care & popularity of certain institutions
- It is more common in observational studies, particularly in case-control studies
Question 8. Bias.
Answer:
Selection Bias:
- Selection Bias occurs when a group studied does not reflect the same characteristics like age, sex, occupation, race, etc as in the general population
Interviewer’s Bias:
- Interviewer’s Bias occurs when there is an error in the classification of individuals with respect to the outcome variable
Confounding Bias:
- Confounding Bias occurs when other factors that are associated with the outcome & exposure variables do not have the same distribution in the exposed & unexposed groups
- Confounding Bias can be removed by matching
Berkesonian Bias:
- Berkesonian Bias arises when there are differences in admission rates of people in hospitals with different diseases
Information Bias:
- Information Bias occurs when the interviewer knows the hypothesis & also knows who the cases are
Memory Bias:
- When the cases & controls are asked questions about their history it may be more likely for the cases to recall the existence of certain events or factors than the controls who are healthy persons
Telescopic Bias:
- If a question refers to the recent past, episodes that occurred longer ago may also be reported
Prevalence-Incidence Bias:
- If the exposure occurred years before, then mild cases that improved or severe cases that died would have been missed & not counted among the cases
Uses Of Epidemiological Methods
Question 9. Double-blind trial.
Answer:
Double-Blind Trial
- In order to reduce the problem of bias a technique called blinding is adopted
- Triple blind trial
- The participant, the investigator & the person analyzing the data are all blind
- Ideally used method
Question 10. Randomized trial.
Answer:
Randomized Trial Steps:
- Drawing up a protocol
- Selecting reference & experimental population
- Randomization
- Manipulation or intervention
- Follow up
- Assessment of outcome
Randomized Trial Types:
- Clinical trials
- Prophylactic trials
- Therapeutic trial
- Safety trial
- Risk-factor trial
- Preventive trial
- Risk factor trials
- Cessation experiments
- Trial of etiological agents
- Evaluation of health services
- Community intervention trial
Question 11. Confounding factor.
Answer:
Confounding Factor
- A confounding factor is defined as one that is associated both with the exposure & disease & is unequally distributed in study & control groups
- A confounding factor is one that although associated with exposure under investigation is itself independent of any such association, a risk factor for the disease
- Example: role of alcohol in the etiology of esophageal cancer
- Smoking is a confounding factor because
- A confounding factor is associated with the consumption of alcohol
- A confounding factor is an independent risk factor for esophageal cancer
Epidemiological Methods Viva Voce
- Prevalence incidence mean duration
- The epidemic is the best example of short-term fluctuations
- Cohort studies are also called longitudinal studies
- A confounding factor is associated with both exposure and disease
- Carriers of avirulent organisms are called pseudo-carriers
- The science of the health of travelers is called emporia tics
- John Snow is the father of epidemiology
- Case-control study begins with the identification of jects with a specific disease and studies for risk factors
- Case-control studies proceed backward from effect to cause. So it is also known as a retrospective study
- In a cohort study, a group of the population who has been exposed to a risk factor is identified and followed over an extended period
- A cohort study proceeds from cause to effect so it is known as a prospective study.
- Panel study is another name for cohort study. Total number of cases of disease at a given time Estimated total population
- Prevalence =\(\frac{\begin{array}{c}\text { Total number of cases } \\\text { of disease at given time }\end{array}}{\begin{array}{c}\text { Estimated total population } \\\text { at same time }\end{array}} \times 100\)
- Incidence =\(\frac{\begin{array}{c}\text { Number of new cases of } \\\text { specific disease at given time }\end{array}}{\text { Population at risk }} \times 100\)
- Cross-sectional study measures the disease to assess the association between risk factors and disease
- The case-control study measures the prevalence of the disease
- In cross-sectional studies, different individuals of a particular group are studied only once
- In longitudinal studies, the same individual is studied at different ages
- Berkonsian bias occurs due to different rates of admission to hospitals for people with different diseases
- Confounding bias is reduced by matching
- Selection bias is controlled by the prevention
- The interviewer’s bias is eliminated by double-blinding
- Cross-sectional studies are useful for chronic diseases
- Hippocrates is the Father of medicine
- Alfred Fones is the Father of dental hygiene.