
Thorax
Thoracic Duct Anatomy
Trachea Esophagus And Thoracic Duct Question And Answers
Question 1. Describe the features and relations of the esophagus.
Answer:
Esophagus Anatomy
Esophagus Structure
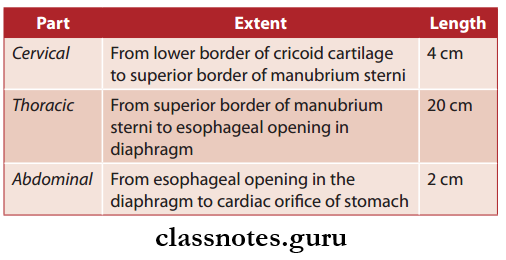
- Esophagus is a long muscular tube
- Esophagus Length: 25 cm
- Esophagus Width: 2 cm
- Esophagus Function: Transport of food from pharynx to the stomach
- Parts of esophagus.
Read And Learn More: Thorax Anatomy
Esophagus Gross Features
- Esophagus Extent: Pharynx to cardiac orifice of stomach
- Esophagus Lumen:
- It is flattened anteroposteriorly
- Normally it is in a collapsed state but dilates during the passage of food
Esophagus Course
Esophagus Anatomy
Esophagus Curvatures: The Esophagus during its course shows few curves
- Two anteroposterior curvatures
- Two side-to-side curvatures.
Esophagus Anatomy
Esophagus Constrictions There are four sites of constrictions present in the esophagus
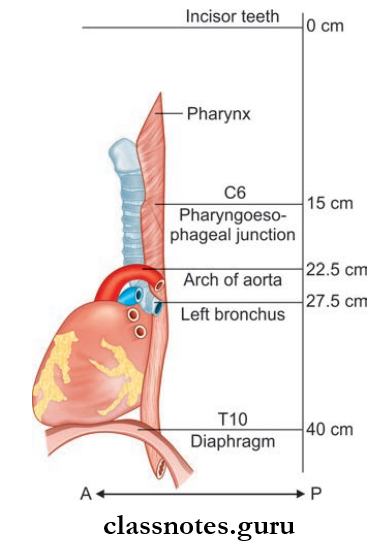
- First Constriction: It is at a distance of 15 cm, at the pharyngoesophageal junction
- Second Constriction: It is at a distance of 22.5 cm at the place where it is crossed by the arch of the aorta
- Third Constriction: It is at a distance of 27.5 cm, at a place where it is crossed by the left principal bronchus
- Fourth Constriction: It is at a distance of 40 cm, at a place where it pierces the diaphragm.
Thoracic duct anatomy
Esophagus Applied Anatomy: Constrictions of the esophagus act as potential sites at which the swallowed foreign bodies can get stuck.
Esophagus Relations:
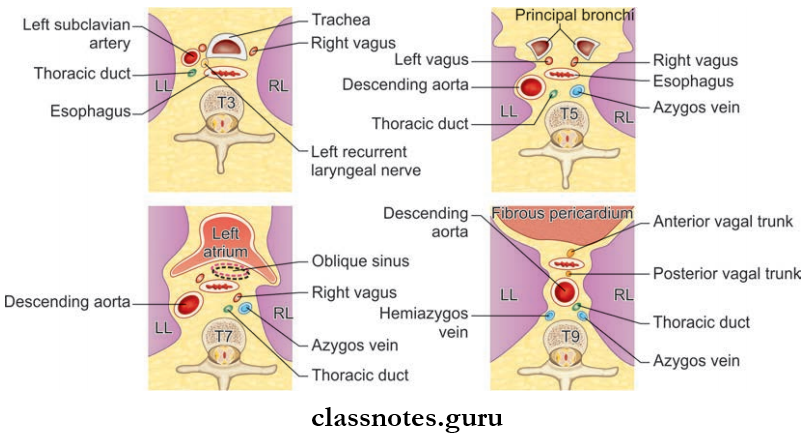
1. Esophagus Relations Cervical part
- Anteriorly
- Trachea
- Recurrent laryngeal nerve
- Posteriorly
- Prevertebral fascia
- Vertebral column
- Laterally
- Common carotid artery
- Lateral lobe of the thyroid
- Left Side
- Thoracic duct
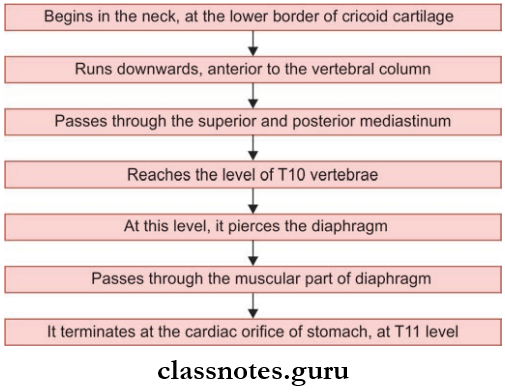
2. Esophagus Relations Thoracic Part
- Anteriorly
- Trachea
- Arch of aorta
- Right principal bronchus
- Fibrous pericardium
- Oblique sinus
- Diaphragm
- Posteriorly
- Vertebral column
- Right posterior intercostal arteries
- Thoracic duct
- Azygos and hemiazygos veins
- Descending thoracic aorta
- Right
- Pleura
- Right lung
- Right vagus
- Azygos
- Left
- Arch of aorta
- Left subclavian artery
- Thoracic duct
- Pleura
- Left lung
Thoracic duct function
3. Esophagus Relations Abdominal Part
- Anteriorly
- The posterior surface of the left lobe of the liver
- Left gastric nerve
- Posteriorly
- Left crus of the diaphragm
- Right gastric nerve
Question 2. Write a note on blood supply, lymphatic drainage, and nerve supply of the esophagus.
Answer:
Esophagus Arterial Supply
- Cervical Part: Inferior thyroid arteries
- Thoracic Part: Descending thoracic aorta and bronchial arteries
- Abdominal Part: Left gastric artery and left phrenic artery
Esophagus Venous Drainage
- Cervical Part: Inferior thyroid
- Thoracic Part: Azygos and hemiazygos veins
- Abdominal Part: Hemiazygos and left gastric vein
Esophagus Lymphatic Drainage
- Cervical Part: Deep cervical lymph nodes
- Thoracic Part: Posterior mediastinal nodes
- Abdominal part: Left gastric nodes
Esophagus Nerve Supply
- Sympathetic Supply:
- These nerves reach it through splanchnic branches of the sympathetic trunk.
- Esophagus Parasympathetic Supply:
- The Upper Half Of The Esophagus: Recurrent laryngeal nerve
- Lower Half Of Esophagus: Esophageal plexus
Question 3. Write a brief on the development of the esophagus.
Answer:
- Developed from posteriormost part of the foregut
- It is short in the beginning but it lengthens quickly due to the descent of the heart and lungs
- Musculature is derived from the splanchnic mesenchyme surrounding the foregut.
Question 4. Write a note on the thoracic duct.
Answer:
Esophagus Disease
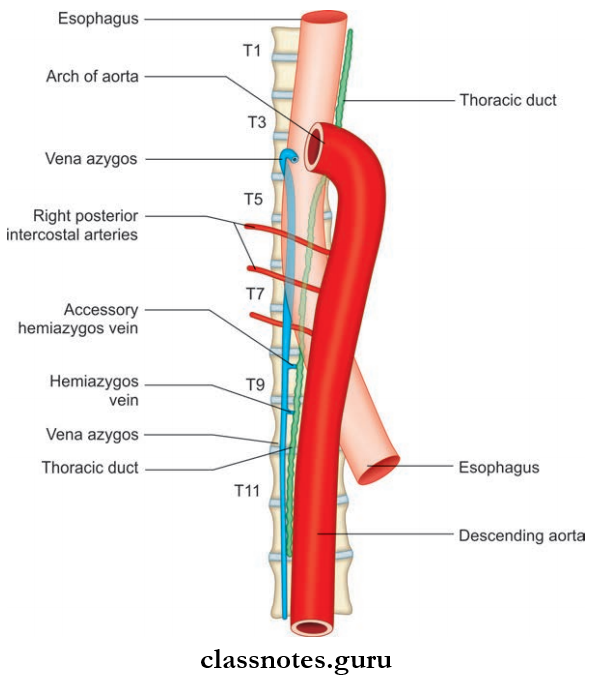
Thoracic Duct Features
- Largest lymph vessel in the body
- It is 40–45 cm long
- Extent: From the upper part of the abdomen to the lower part of the neck.
Thoracic Duct Gross Features
Thoracic Duct has a characteristic beaded appearance due to the presence of numerous valves.
Thoracic Duct Course
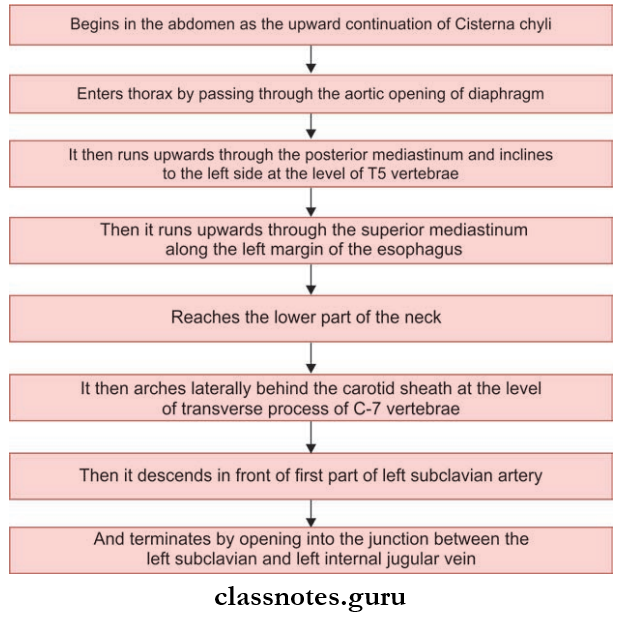
Mnemonic: Thoracic duct: Relation to azygos vein and esophagus.
‘The duck between two geese: Thoracic duct (duck) is between two geese, azygos and esophagus
Esophagus Disease
Question 5. Write a note on the trachea.
Answer:
Trachea Structure
- Wide tube
- Lying more or less in the midline, in the lower part of the neck
- Length: 10–15 cm
- External Diameter:
- Males – 2 cm
- Females – 1.5 cm
- Internal diameter – 12 mm
- The upper end of the trachea is the continuation of the larynx
- The laryngotracheal junction lies at the level of the 6th cervical vertebrae
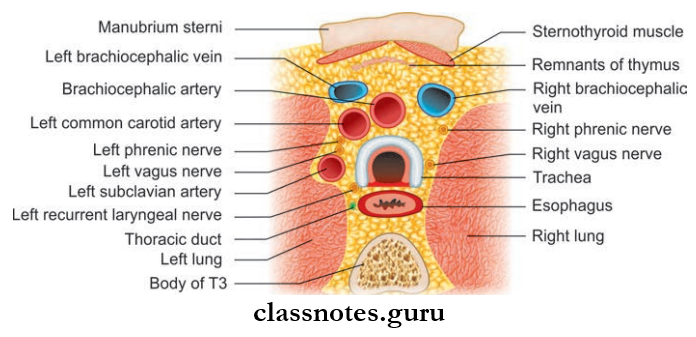
- The trachea enters the thorax through the superior thoracic inlet and occupies the superior mediastinum
- Lower end of trachea end by bifurcating into right and left principal bronchi
- The level of bifurcation corresponds to the lower border of the T4 vertebrae or the lower border of the manubrium sterni.
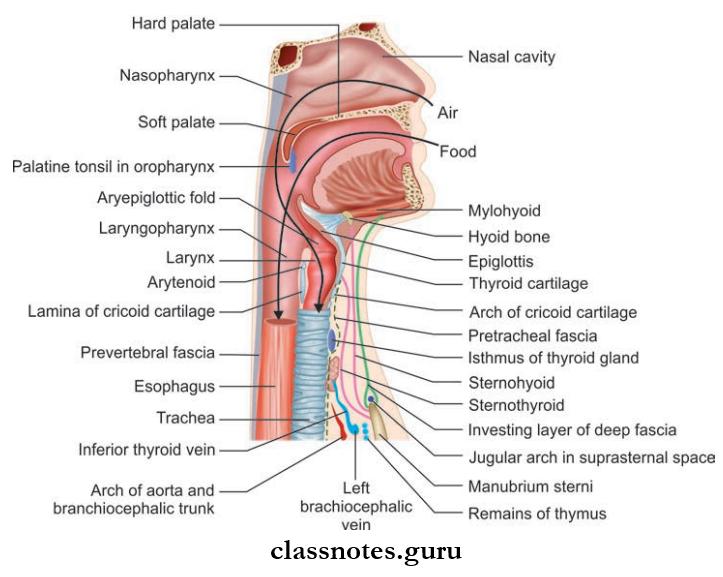
Trachea Relations:
1. Trachea Relations Anteriorly
- Manubrium sterni
- Sternothyroid muscle
- Left brachiocephalic veins
- Arch of aorta
- Brachiocephalic trunk
2. Trachea Relations Posteriorly
- Esophagus
- T1–T4 vertebrae
3. Trachea Relations Right side
- Right lung
- Right vagus
- Azygos vein
4. Trachea Relations Left side
- Arch of aorta
- Left subclavian artery
- Left common carotid artery
- Left recurrent laryngeal nerve
- Arterial Supply: Inferior thyroid arteries
- Venous Drainage: Left brachiocephalic vein
- Lymphatic Drainage: Pretracheal and paratracheal nodes
Trachea Nerve Supply:
- Sympathetic Supply: From middle cervical ganglion
- Parasympathetic Supply: From vagus and recurrent laryngeal nerves.
Thoracic duct drainage
Trachea Esophagus And Thoracic Duct Multiple Choice Questions And Answers
Question 1. Trachea bifurcates at the level of:
- Lower border of T4 vertebrae
- The lower border of T5 vertebrae
- The upper border of T3 vertebrae
- The upper border of T4 vertebrae
Answer: 1. Lower border of T4 vertebrae
Question 2. One should watch for _____________ while passing a Ryle’s tube for gastric analysis:
- Structures anterior to the esophagus
- Constrictions of the esophagus
- Pericardium
- Trachea
- None of the above
Answer: 2. Constrictions of the esophagus
Question 3. The length of the esophagus in an adult is:
- 15 cm
- 20 cm
- 25 cm
- 30 cm
Answer: 3. 25 cm
Thoracic duct location
Question 4. What is true of the anatomy of the trachea?
- Starts at the level of C4
- Drains to axillary lymph nodes
- Is supplied by the glossopharyngeal nerve
- Is marked at its lower end by the sternal angle
Answer: 4. Is marked at its lower end by the sternal angle
Question 5. The esophagus is narrowest at:
- Level of cricopharyngeus
- C6
- At cardiac orifice
- C4
Answer: 1. Level of cricopharyngeus
Vena Cava: Function and Anatomy
Superior Vena Cava And Aorta Question And Answers
Question 1. Describe briefly on the formation, course, relations, and tributaries of superior vena cava.
Answer:
Superior Vena Cava
- Large venous channel
- Receives blood from upper half of body and drain it into the upper end of right atrium
- 7 cm long, 1.25 cm in diameter
- Valve less
Read And Learn More: Thorax Anatomy
- Location:
- Extrapericardial part: Superior mediastinum
- Intrapericardial part: Middle mediastinum.
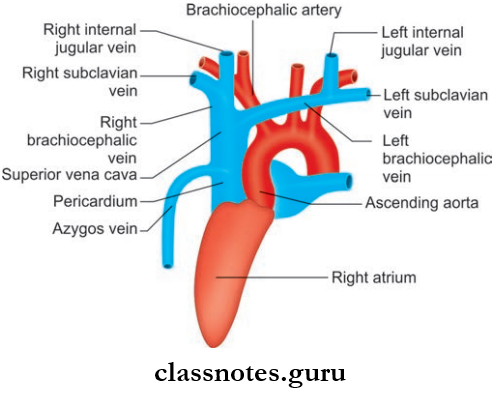
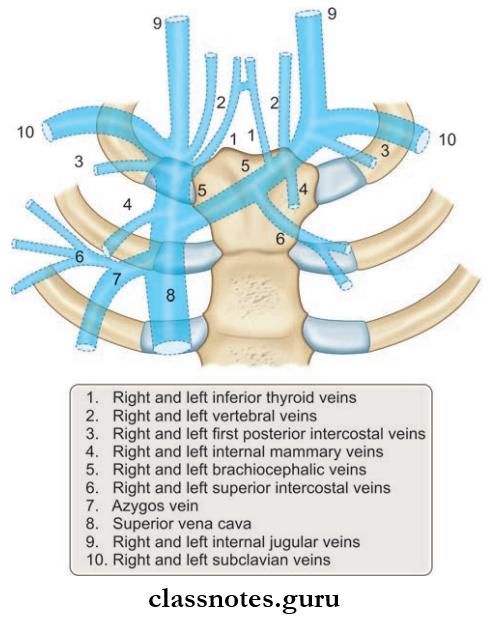
Superior Vena Cava Formation
- Formed by the union of right and left brachiocephalic veins
- The point of formation lies at the lower border of the sternal end of the fist costal cartilage.
Superior Vena Cava Course
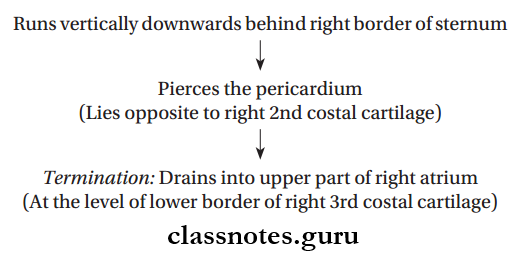
Superior Vena Cava Relations:
- Anterior
- Chest wall
- Right internal thoracic vessels
- Anterior margin of right lung and pleura
- Medial
- Ascending aorta
- Brachiocephalic artery
- Posterior
- Right pulmonary artery
- Right bronchus
- Trachea
- Right vagus
- Lateral
- Right pleura
- Right lung
- Right phrenic nerve
- Pericardiophrenic vessels
Superior Vena Cava Tributaries
- Right and left brachiocephalic veins
- Azygos vein: At the lower end of extra pericardial part
- Mediastinal veins
- Pericardial veins.
Vena cava anatomy
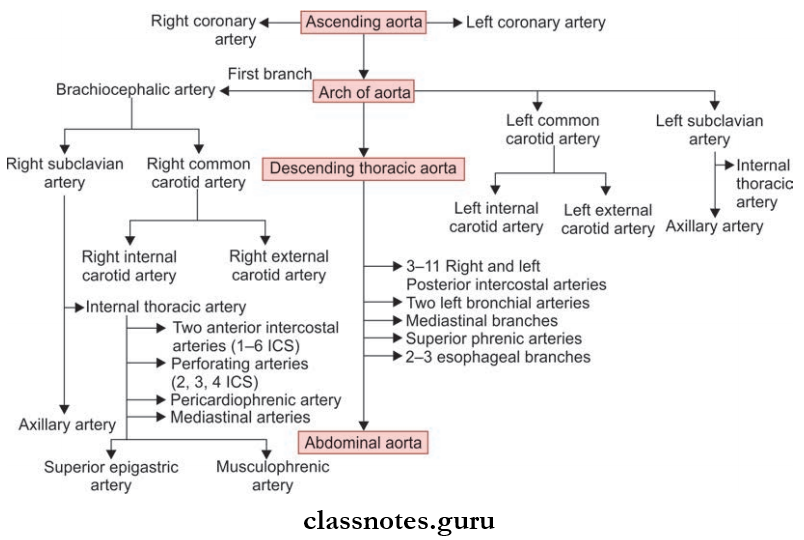
Question 2. What are the parts of aorta?
Answer:
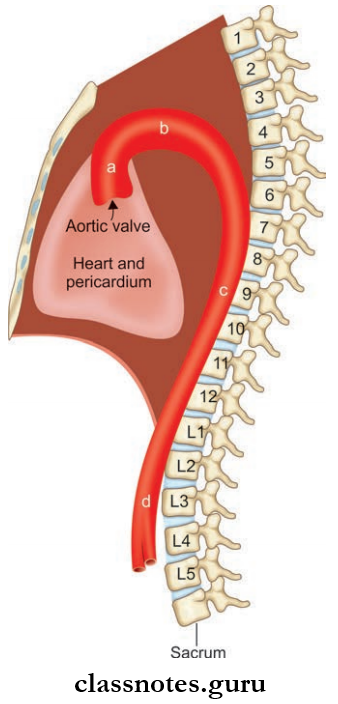
Parts of Aorta
- Largest artery
- Receives oxygenated blood from left ventricle
- Aorta can be divided into four parts:
- Ascending aorta
- Arch of aorta
- Descending thoracic aorta
- Abdominal aorta.
Question 3. Write a note on ascending aorta.
Answer:
Structure ascending aorta is 5 cm long, 3 cm in diameter, enclosed in a pericardium.
Ascending Aorta Origin
- From the upper end of left ventricle
- At the lower border of 3rd costal cartilage behind the left half of the sternum
Ascending Aorta Course: Runs upwards, forward, and to the right
Ascending Aorta Termination: At the level of sternal angle, it continues as the arch of the aorta
Ascending Aorta Branches: Right coronary artery and left coronary artery.
Question 4. What are aortic sinuses?
Answer:
- They are dilatations of the vessel wall at the roots of the aorta, just above the cusps of the aorta
- They Are Three In Number:
- Anterior: Gives rise to the right coronary artery
- Right Posterior And Left Posterior: Gives rise to the left coronary artery.
Aortic Sinuses Relations:
- Anteriorly
- Sternum
- Pericardium
- Pulmonary trunk
- Infundibulum of right ventricle.
- Posteriorly
- Right principal bronchus
- Right pulmonary artery
- Left atrium
- Transverse sinus.
Vena cava function
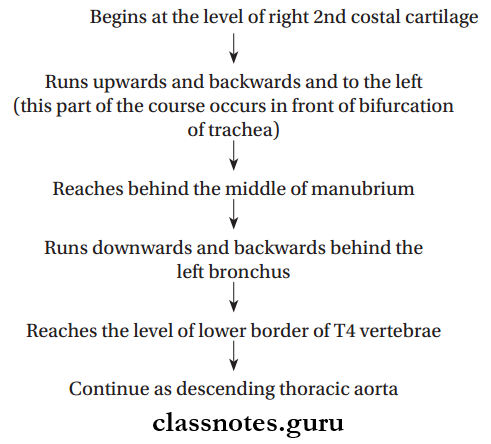
Question 5. Write a note on the arch of the aorta.
Answer:
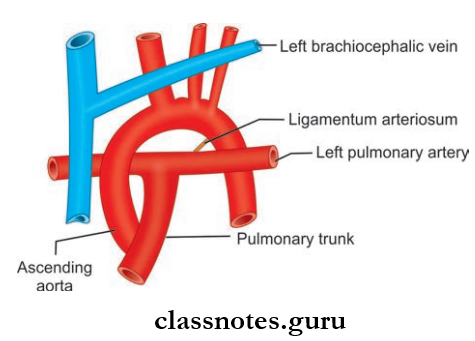
Arch Of Aorta Introduction
- Location: Superior mediastinum
- Level: Lower half of manubrium sterni
- It is the continuation of the ascending aorta at the sternal angle and also ends at the level of sternal angle (Both origin and termination at the same level)
- Derived from the ventral part of the aortic sac, its left horn and left arch artery
Arch Of Aorta Course:
Arch Of Aorta Relations:
- Anterior And To The Left
- Left pleura and lung
- Left superior intercostal vein
- Nerves:
- Left phrenic nerve
- Left vagus nerve
- Left cardiac nerves
- Posterior And To The Left
- Trachea
- Esophagus
- Left recurrent laryngeal nerve
- Thoracic duct
- Vertebral column.
- Superior
- Brachiocephalic trunk
- Left common carotid artery
- Left subclavian artery
- Left brachiocephalic vein
- Thymus.
- Inferior
- Bifurcation of the pulmonary trunk
- Left branches
- Ligamentum arteriosum
- Superfiial cardiac plexus
- Left recurrent laryngeal nerve.
Arch Of Aorta Branches
- Brachiocephalic artery
- Left common carotid artery
- Left subclavian artery.
Vena cava circulation
Superior Vena Cava And Aorta Multiple Choice Questions
Question 1. Which of the following statements concerning the relations of the arch of the aorta is incorrect?
- The ascending aorta arches backward to reach the body of the fourth thoracic vertebra
- The arch is crossed on its left side by the phrenic and vagus nerves
- The left recurrent laryngeal nerve passes upwards on the left side of the arch of the aorta
- Ends by becoming the thoracic aorta posterior to the 2nd left sternocostal joint
Answer: 3. The left recurrent laryngeal nerve passes upwards on the left side of the arch of the aorta
Question 2. The arch of the aorta is related to:
- Jugular notch
- Angle of Louis
- The midline of the manubrium sterni
- Second costal cartilage
Answer: 3. Midline of manubrium sterni
Question 3. Which of the following is false about the arch of the aorta?
- It starts from the 2nd right sternocostal joint
- It arches over the anterior surface of the trachea while ascending diagonally posteriorly
- It is a content of superior and posterior mediastinum
- It is crossed anteriorly by the left phrenic nerve and left vagus nerve
Answer: 3. It is a content of superior and posterior mediastinum
Pericardium Anatomy
Pericardium And Heart Question And Answers
Question 1. Write a short note on the pericardium.
Answer:
Pericardium
- The Pericardium is a firoserous sac, which surrounds the heart and the root of great vessels
- Located in the middle mediastinum
- Pericardium Has Two Parts:
- Fibrous Pericardium: The outer layer of the pericardium formed by tough connective tissue
- Serous Pericardium: The inner layer, it is subdivided into:
- Parietal layer
- Visceral layer.
Read And Learn More: Thorax Anatomy
Pericardium Contents
- Heart
- Great vessels: Ascending aorta, pulmonary trunk, superior vena cava, inferior vena cava, and pulmonary veins.
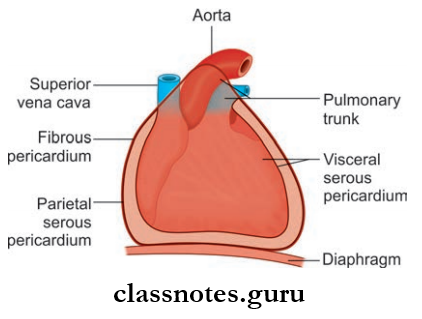
Fibrous Pericardium
- Fibrous Pericardium is a cone-shaped sac
- Fibrous Pericardium Has An:
- Apex
- Blunt
- Continuous with the adventitia of great vessels
- Lies at the level of the sternal angle
- Base
- Broad
- Attached is the central tendon of the diaphragm
Pericardium Relations:
- Anteriorly: Attached to the sternum through sternopericardial ligaments (This attachment helps to retain the position of the heart in the thoracic cavity)
- Posteriorly: Principal bronchi, esophagus, descending thoracic aorta
- Blood supply: Pericardiophrenic vessels
- Nerve supply: Phrenic nerves.
Serous Pericardium: The inner layer. It has two parts:
- Parietal Layer
- It is fused with the inner surface of the fibrous pericardium
- It is continuous with a visceral layer around the roots of great vessels
- Visceral Layer (Epicardium)
- It is fused with the heart
- Deficient only at the cardiac grooves, where it is separated from the heart by the cardiac blood vessels.
Pericardial Cavity
- The Pericardial Cavity is a narrow space formed between the fibrous and serous pericardium
- Capacity—300 ml
- The Pericardial Cavity contains a small amount of serous fluid
- This serous fluid acts as a lubricant, which lubricates the opposed surfaces of fibrous and serous pericardium.
- The arterial supply of fibrous pericardium and the parietal layer of the serous pericardium is by branches of:
- Internal thoracic artery
- Musculophrenic artery
- Descending thoracic aorta
- The visceral layer of the serous pericardium is supplied by coronary arteries
- Venous Drainage
- Veins Drain Into:
- Azygos system of veins
- Internal thoracic vein
- Nerve Supply:
- Fibrous pericardium and parietal pericardium:
- Phrenic nerve (sensitive to pain)
- Visceral pericardium: Autonomic nerves of the heart (insensitive to pain).
- Veins Drain Into:
Pericardium Applied Anatomy
- Pain sensation from the parietal pericardium is carried by somatic afferent fiers of phrenic nerves, so pain during pericarditis or any other irritation to the pericardium is referred to:
- Supraclavicular region of the shoulder
- Lateral part of the neck
- Pericardial Effusion: Accumulation of flid in the pericardial sac.
Pericardium anatomy and function
Question 2. What are the sinuses of the pericardium and what is its use?
Answer:
Sinuses Of Pericardium: The visceral layer of serous pericardium/epicardium is arranged at the roots of great vessels in the form of two tubes:
- Arterial Tube: Arterial tube encloses the pulmonary trunk and ascending aorta
- Venous Tube: Venous tube encloses the superior and inferior vena cava and pulmonary veins.
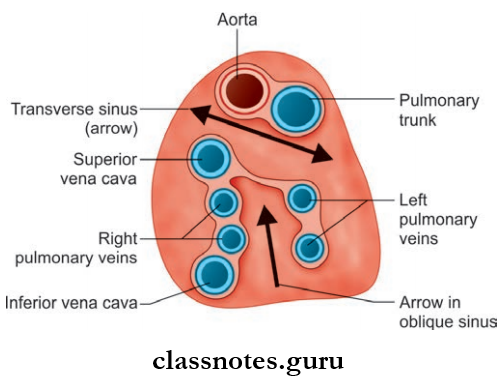
Transverse Sinus
- There is a horizontal passage present between the arterial and venous ends of the heart tubes, known as transverse sinus
- Located on the upper part of the posterior surface of the heart
- It is a tubular recess between the right and left sides of the pericardial cavity posteriorly
Transverse Sinus Boundaries:
- Anteriorly: Ascending aorta, pulmonary trunk
- Posteriorly: Superior vena cava, pulmonary veins
- Inferiorly: Upper surface of left atrium
- Superiorly: Bifurcation of the pulmonary trunk
- On Each Side: Opens into the pericardial cavity.
Oblique Sinus
- Oblique Sinus is a space located on the posterior surface of the heart between the venous tubes of four pulmonary veins
- The oblique Sinus is called a cul de sac (a passage with access only at one end) since it is closed on all sides except inferiorly
- Oblique Sinus lies behind the left atrium
Oblique Sinus Boundaries:
- Anteriorly: Left atrium
- Posteriorly: Parietal pericardium
- Right side: Right pulmonary veins and inferior vena cava
- Left side: Left pulmonary vein
- Superiorly: Upper margin of the left atrium
- The presence of an oblique sinus allows free pulsation of the left atrium.
Sinuses Applied Anatomy
During cardiac surgery, the transverse sinus provides the space to clamp the ascending aorta and pulmonary trunk, in order to insert tubes of heartlung machines.
Question 3. Describe the external features of the heart.
Answer:
External Features Of Heart
- The heart is a conical hollow muscular pump
- Structurally and functionally it consists of two halves right and left
- Each half has an atrium and ventricle, thus it has 4 chambers.
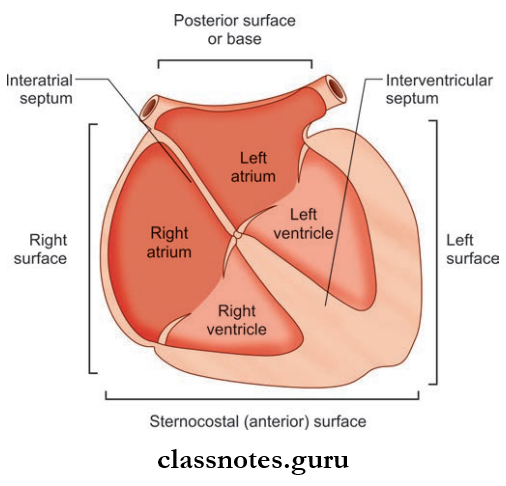
External Features of Heart Margins
- Right Margin: Formed by the rounded surface of the right atrium
- Left Margin: Formed by the rounded surface of the left ventricle.
External Features of Heart Surfaces
- Anterior/Sternocostal Surface
- Posterior Surface/base
- Right And Left Surface
- Diaphragmatic Surface/Inferior Surface.
1. Anterior/Sternocostal Surface
- Anterior/Sternocostal Surface Formed By:
- Right atrium
- Right ventricle
- Left ventricle (minor contribution)
- The right atrium and ventricle are separated from each other by the atrioventricular groove or the coronary sulcus (lodges the coronary artery)
- Ventricles are separated anteriorly by the anterior interventricular groove
- The sternocostal surface is separated from the diaphragmatic surface by a sharp border (Inferior border)
- The point where the inferior border meets the left border is known as the apex
- The upper border is formed by the left atrium.
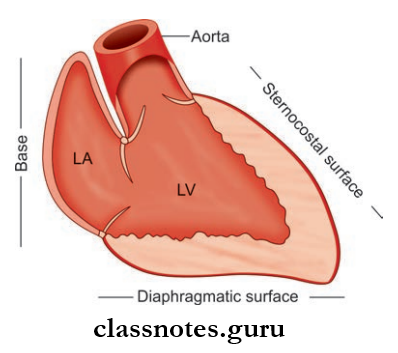
2. Posterior Surface/Base
- Posterior Surface/Base Formed by:
- Left atrium
- Posterior part of the right atrium (small contribution).
3. Diaphragmatic Surface
- Diaphragmatic Surface Formed by:
- Left ventricle (2/3rd contribution)
- Right ventricle (1/3rd contribution)
- Two ventricles are separated by the posterior interventricular groove.
Anterior Part of Coronary Sulcus
- Right Hhalf: It is easily visible on the sternocostal surface
- Course: Runs downwards and to the right between right atrium and right ventricle
- Left Half: Its view is hidden by the aorta and pulmonary trunk.
Posterior Part of Coronary Sulcus
Lies in the diaphragmatic surface at the junction of the right ventricle and right atrium and left ventricle and left atrium.
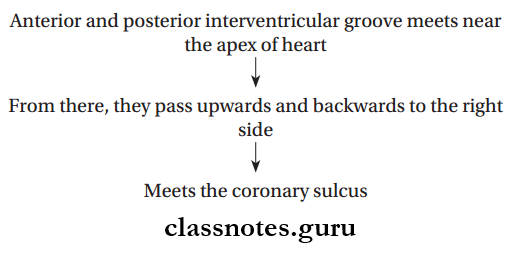
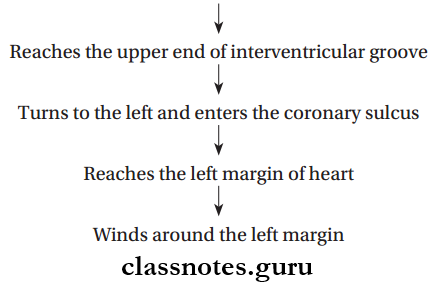
The Course Of Interventricular Grooves
Fibrous and serous pericardium
Question 4. Write a note on the development of the heart tube.
Answer:
Development Of Heart Tube
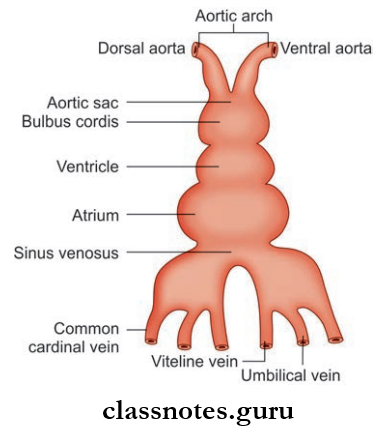
- Mesodermal in origin
- During 3rd week angioblastic cords are formed from intraembryonic mesoderm
- Angioblastic cords are paired endothelial strands formed in the cardiogenic area
- Cords undergo canalization and form heart tubes
- Firstly heart has right and left endothelial tubes which fuse together to form a single tube
- Single tube undergoes dilatation separated by constrictions from top to bottom
- These dilatations from above to below are later identified as:
- Bulbus Cordis Has Three Parts:
- Truncus Arteriosus: Distal 1/3rd part, forms ascending aorta and pulmonary trunk. It is continuous with the aortic sac distally.
- Conus: Middle 1/3rd, forms outflow tracts of ventricles
- The proximal 1/3rd part forms the primitive right ventricle
- The primitive ventricle forms the trabeculated part of the left ventricle
- Primitive atrium
- Sinus Venous:
- Sinus venous has prolongations at the caudal end called right and left horns
- Each horn is joined by a vitelline vein, umbilical vein, and common cardinal vein.
Question 5. Explain in detail the external and internal features of the right atrium.
Answer:
Features Of Right Atrium
- The right upper chamber of the heart
- It Receives Venous Blood Mainly From:
- Superior vena cava
- Inferior vena cava
- Coronary sinus
- It pumps blood into the right ventricle through the tricuspid valve
- The tricuspid opening is guarded by the tricuspid valve or atrioventricular valve
- Right Atrium Forms:
- The sternocostal surface of the heart
- Base of heart
- Right border
- A portion of the upper border.
External Features Of Right Atrium
- The right atrium is a vertically elongated chamber
- An ear-like projection arises from an anterosuperior part of the right atrium, known as the right auricle
- The right auricle has a notched margin and it covers the ascending aorta and infundibulum of the right ventricle
- The Interior of the right auricle is sponge-like
- Right atrium receives a superior vena cava at its upper end and an inferior vena cava at its lower end
- On the right border of the atrium, a sulcus passes from the superior vena cava to the inferior vena cava, known as sulcus terminalis
- The upper part of this sulcus lodges the SA node
- Sulcus terminalis is formed by an internal muscular ridge known as crista terminalis.
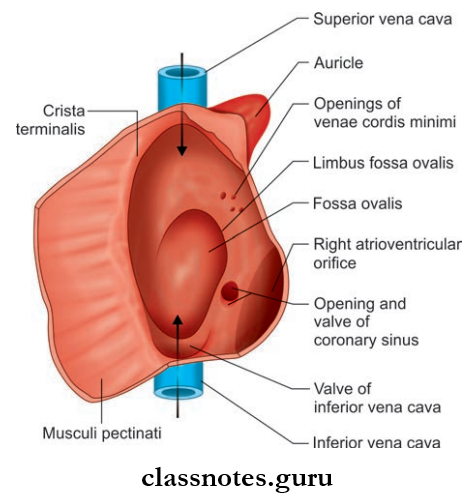
Internal Features Of Right Atrium: The Interior of the heart can be divided into two parts:
- Sinus venarum/Smooth posterior part: Derived from right horn of sinus venosus
- Atrium proper/Rough anterior part: Derived from the primitive atrial chamber.
- Sinus Venarum/Smooth Posterior Part
- The superior vena cava opens at its upper end and the inferior vena cava at its lower end
- Opening of the inferior vena cava is bounded by a semilunar valve called as eustachian valve/valve of the inferior vena cava
- It is actually rudimentary
- In embryonic life, it transmits blood directly from the inferior vena cava to the left atrium through the foramen ovale
- Opening for coronary sinus is present between openings of inferior vena cava and right atrioventricular orifice, which is also guarded by a valve known as the valve of the coronary sinus
- Venae cordis minimi opens into the right atrium through numerous small openings in the wall of the atrium.
- Atrium Proper/Rough Anterior Part
- Also called the pectinate part
- It contains the right auricle
- Its wall shows the presence of transversely running muscular ridges called the musculi pectinate
- Ridges arise from the crista terminalis, run forward and downward towards the av orifice (teeth of a comb-like appearance)
- Some of them enter the right auricle and form a network.
Tributaries Of Right Atrium
- Superior vena cava
- Inferior vena cava
- Coronary sinus
- Anterior cardiac veins
- Venae cordis minimi
- Right marginal vein
Question 6. From where does the right atrium develop?
Answer:
Development Of Right Atrium
- Mainly formed from the right half of the primitive atrium
- The rough anterior part develops from the right horn of the sinus venosus
- The sinus venous and right half of the atrioventricular canal get absorbed into the right atrium
- The smooth posterior part along with the right auricle develops from the primitive atrium.
Question 7. What are the features of the interatrial septum and how is it formed?
Answer:
Interatrial Septum
- Interatrial Septum is derived from septum primum and secundum
- When looked at from the right atrium, this septum shows some gross features:
- Fossa Ovalis
- Oval depression on the lower part
- Represents the site of embryonic septum primum
- Annulus Ovalis/Limbus Fossa Ovalis
- Prominent margin of fossa ovalis
- Represents the lower curved edge of the septum secundum.
- Fossa Ovalis
Development of Interatrial Septum
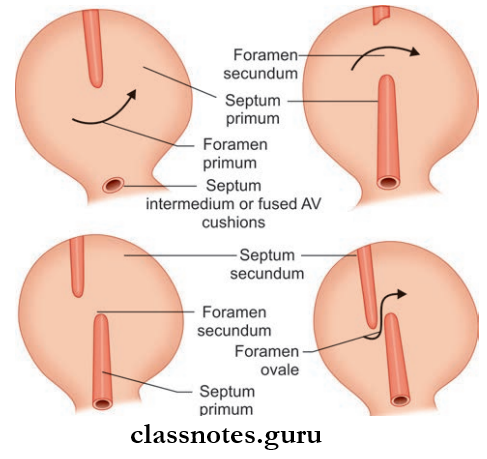
- Interatrial Septum develops from two septa (septum primum and septum secundum) arising from the roof of the atrial chamber
- Septum primum arises from the roof of the atrial chamber and grows downward towards the septum intermedium
- Initially, there will be a gap between septum primum and septum intermedium known as foramen primum
- Finally, septum primum fuses with septum intermedium
- Before the fusion, the upper part of the septum primum breaks down leaving a free upper edge
- A new foramen is created known as foramen secundum
- Another septum called septum secundum starts to grow from the right of the septum primum, towards the septum intermedium
- Septum secundum overlaps the upper margin of septum primum, creating an oblique passage between septum primum and secundum called foramen ovale
- In fetal life, foramen ovale allows the blood to flow from right to left atrium
- Finally, by the fusion of septum secundum and septum primum, the foramen ovale is obliterated
- The upper and lower half of the interatrial septum are formed by the septum secundum and primum respectively.
Question 8. Write briefly about the gross features of the left atrium.
Answer:
left atrium Gross Features
- Quadrangular shaped thin-walled cavity
- Situated posteriorly
- Also contains the left auricle
- The Left Atrium Forms The Part Of:
- The upper border of the heart
- The sternocostal surface of the heart
- Left surface and left border
- Left 2/3rd of the base of the heart.
Internal Features Of Left Atrium
- Most of the wall is smooth, this part derived from absorbed pulmonary veins
- Musculi pectinate only present in the left auricle, derived from the primitive atrial chamber of the heart tube
- It receives 4 pulmonary veins in its upper lateral part
- Anteroinferiorly, the left atrium opens into the left ventricle through the left atrioventricular orifice
- This orifice is guarded by the mitral valve.
Pericardial cavity anatomy
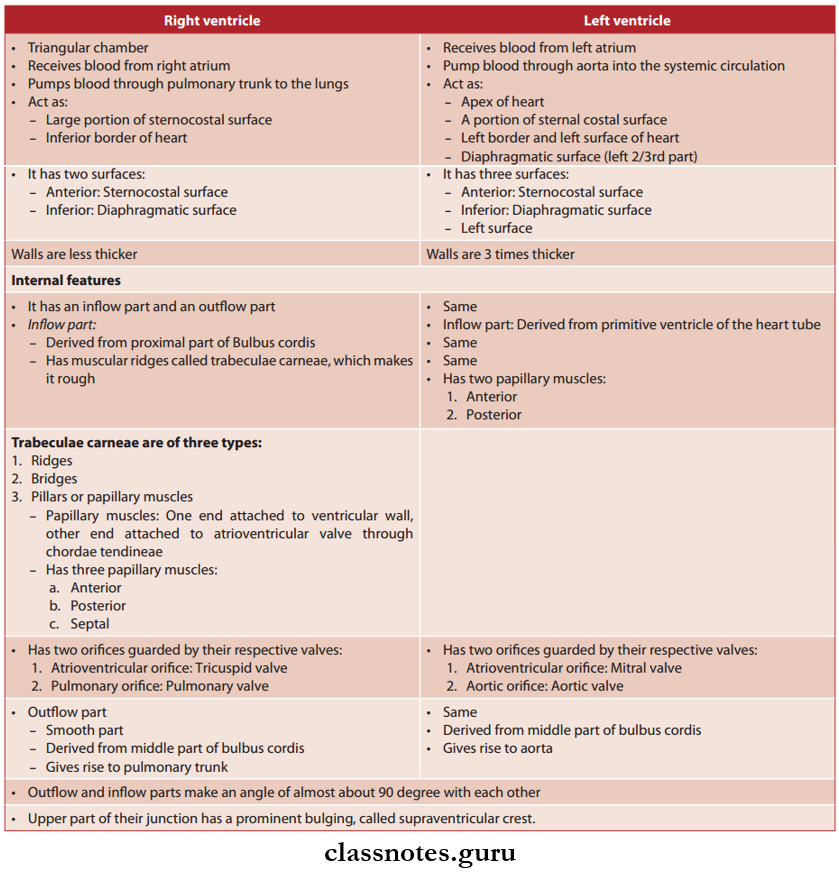
Question 9. What are the similarities and differences between right and left ventricles?
Answer:
Question 10. Write briefly on the valves of the heart.
Answer:
Heart Valves
- Valves Of Aortic Orifices: Tricuspid and mitral valve (Bicuspid valve)
- Valves Of Pulmonary And Aortic Valves/Semilunar Valves: Pulmonary valve and aortic valve
Tricuspid Valve Of Heart: Made up of three cusps attached to a fibrous ring
- Anterior Cusp: Attached to the superolateral part of the margin of the right AV orifice
- Posterior Cusp: Attached to the inferolateral part of the margin
- Septal Cusp: Attached to the medial margin
Bicuspid Value Of Heart: Made up of two cusps attached to a fibrous ring
- Anterior cusps: Attached to the upper right part of the margin of the left AV orifice
- Posterior cusp: Attached to the lower left part of the margin of the left AV orifice
Free margins and ventricular surfaces of cusps are connected to papillary muscles through chordae tendineae.
Pulmonary Orifice Of Heart
- Longer 3 cm in diameter
- Location: Superior and left to the tricuspid orifice (aortic orifice intervenes between pulmonary orifice and tricuspid orifice)
- Guarded by pulmonary valve
- Has three semilunar cusps:
- Cusps are triangular in shape
- Made up of a double fold of endocardium with fibrous tissue enclosed in it
- Has two free margins
- Free margins meet at the apex of the cusp
Aortic Orifice Of Heart
- Smaller, 2.5 cm in diameter
- Location: Anterior and right to mitral orifice
- Guarded by aortic valve
- Same
Question 11. Write a note on the interventricular septum.
Answer:
Interventricular Septum
- Separates right and left ventricle
- The position corresponds to anterior and inferior interventricular grooves
- The right side is convex, it bulges into the right ventricle
- The right side of the septum is directed anteriorly and to the right, and the left side is directed backward and to the left
- Right and left AV orifices are separated by the posterosuperior border of the septum
- The septum is thick and muscular, except at a small area near the posterior margin, where it is membranous
- The septal cusp of the tricuspid valve is attached to the membranous part and separates the septum into:
- Anterior part: Separating right and left ventricle
- Posterior part: Separating left ventricle from right atrium.
Interventricular Septum Applied Anatomy
- Fallot’s Tetralogy Congenital condition is characterized by:
- Stenosis of the pulmonary trunk
- Large ventricular septal defect
- Overriding of aortic orifice above VSD
- Right ventricular hypertrophy due to high BP in RV
- Leading to the right to the left shunt of blood through VSD, resulting in severe cyanosis.
Question 12. Describe in detail the blood supply of the heart. What is cardiac dominance?
Answer:
Blood Supply Of Heart
- Coronary arteries supply blood to the heart
- There are two of them:
- Right coronary artery
- Left coronary artery
- Originate from the ascending aorta
- Run in the coronary sulcus
- They can be called the largest vasa vasorum if we consider the heart as a modified blood vessel
- The pattern of branching of coronary arteries shows variation in different individuals.
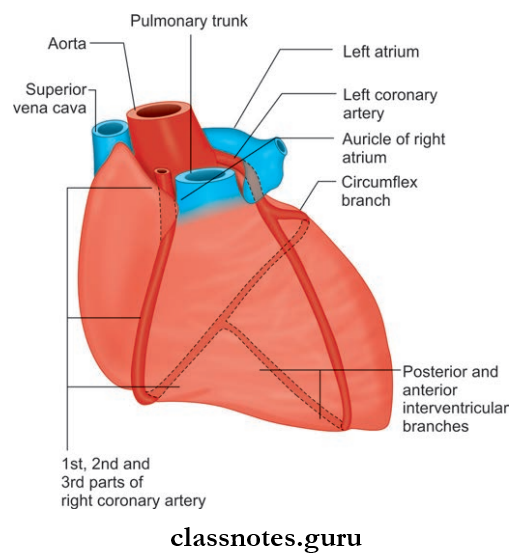
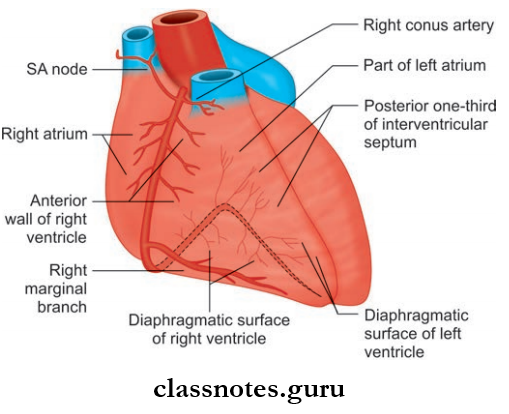
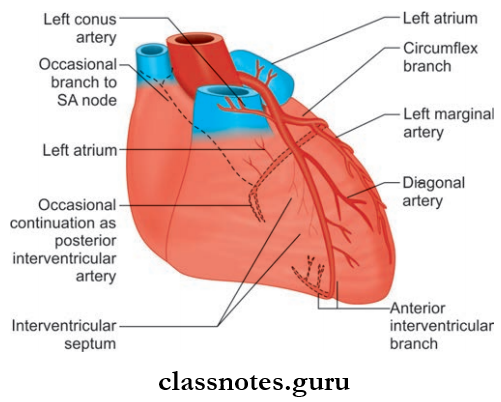
The Most Common Pattern Is Described Below:
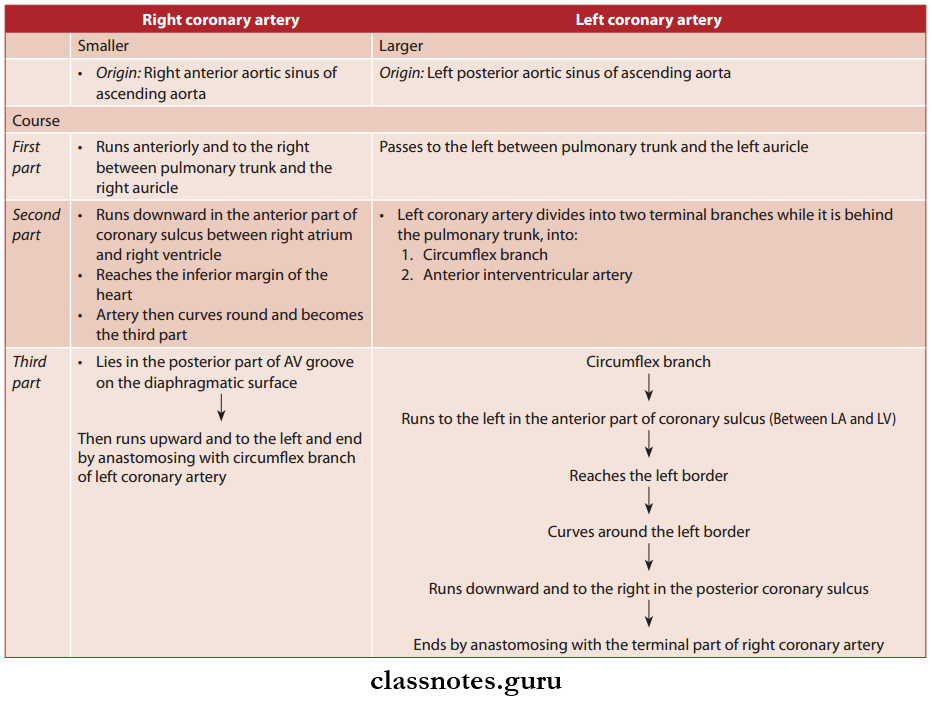
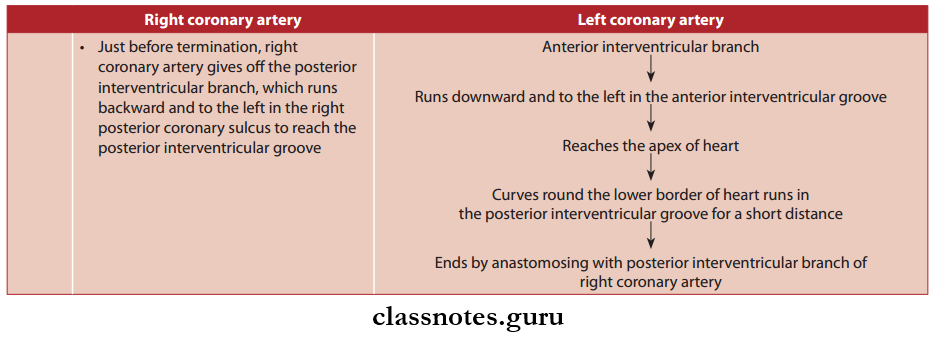
Branches Of Coronary Arteries
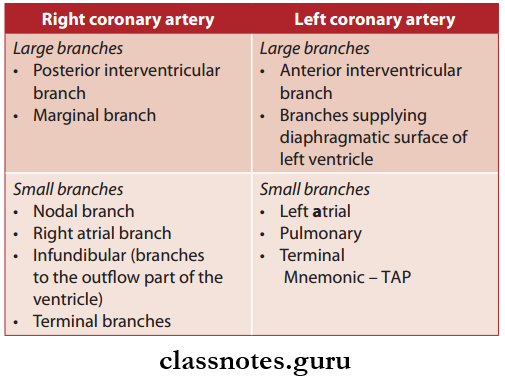
Areas of Distribution
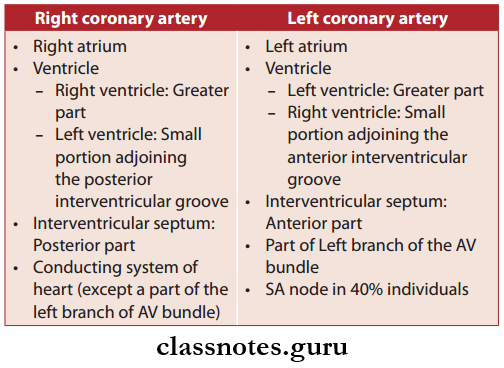
Cardiac Dominance
- Normally, in 90% of the cases, the right coronary artery gives off the posterior interventricular branch, such hearts are called right dominant heart
- But in 10% of the population, the left coronary artery gives off the posterior interventricular branch, such hearts are called the left dominant heart.
Cardiac Dominance Applied Anatomy
- The left coronary artery is more prone to blocks, so in left-dominant individuals, blocks may be fatal
- Coronary Angiography: Coronary arteries and their branches are visualized by this technique, to determine the sites of narrowing.
Question 13. Write a short note on the veins of the heart.
Answer:
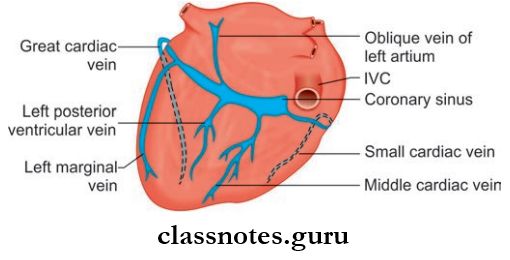
Veins Of The Heart They Are Namely:
Coronary sinus, Great cardiac vein, middle cardiac vein, small cardiac vein, right marginal vein, an oblique vein of the left atrium, a posterior vein of the left ventricle, anterior cardiac vein, and vena cordis minimi.
1. Veins Of The Heart Coronary Sinus
- The largest vein of the heart
- 3 cm long
- Most of the veins draining the heart open into the coronary sinus
- Located in the left posterior coronary sulcus
- Its right end opens into the posterior wall of the right atrium
- Tributaries:
- Great Cardiac Vein
- Small Cardiac Vein
- Middle Cardiac Vein
- Posterior Vein Of The Left Ventricle
- Oblique Vein Of Left Atrium
- Right Marginal Vein (Sometimes).
- Tributaries:
Great Cardiac Vein
- Seen mainly on the sternocostal surface
- It ascends in the anterior interventricular groove, parallel to the anterior interventricular branch of the left coronary artery
Small Cardiac Vein:
- It runs in the right posterior coronary sulcus, accompanying the right coronary artery
- Opens into the right end of the coronary sinus.
Middle Cardiac Vein:
- Begins near the apex of the heart
- Runs backward on the diaphragmatic surface
- It lies in the posterior interventricular groove accompanying the posterior interventricular branch of the right coronary artery
- Opens into the middle part of the coronary sinus.
Posterior Vein Of The Left Ventricle:
- Runs backward on the diaphragmatic surface of the ventricle
- Opens into the middle of the coronary sinus.
Oblique Vein Of Left Atrium:
- Derived from left common cardinal vein
- Runs in the posterior surface of the left atrium
- Opens into the left end of the coronary sinus.
Right Marginal Vein: Opens into the coronary sinus or into a small cardiac vein.
2. Anterior Cardiac Vein
- 3 or 4 in number
- Runs parallel to each other on the anterior wall of the right ventricle
- Opens through the anterior wall of the right atrium.
3. Venae Cordis Minimi
- Smallest cardiac vein or the Thbesian vein
- Present in all chambers of the heart
- More on the right side
- Drain directly into the chambers of the heart.
Pericardium histology
Quetsion 14. What are cardiac plexuses?
Answer:
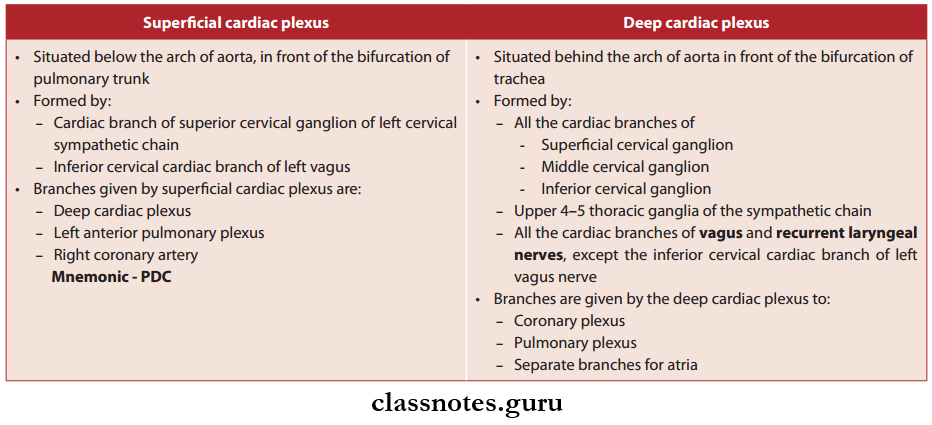
Cardiac Plexuses
- The heart has both sympathetic and parasympathetic supply
- Sympathetic Fibers:
- Derived from upper 4–5 thoracic spinal segments
- Cardioacceleratory (increase HR)
- Also dilates coronary arteries.
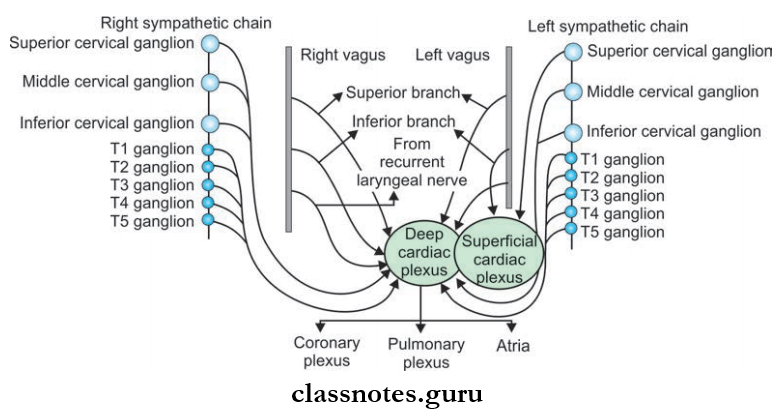
- Parasympathetic Fibers:
- Derived from the vagus nerve
- Cardioinhibitory
- Constricts coronary arteries.
- Both sympathetic and parasympathetic fibers supply the heart through the superficial and deep cardiac plexus
- Branches from the cardiac plexus run along the coronary arteries and supply the myocardium.
Question 15. What is the lymphatic drainage of the heart?
Answer:
Heart Drainage
- Lymphatics from the heart accompany coronary arteries
- Forms two trunks:
- The right trunk, drains into brachiocephalic nodes
- Left trunk, drains into inferior tracheobronchial nodes.
Question 16. Write briefly on the conduction system of the heart.
Answer:
Conduction System
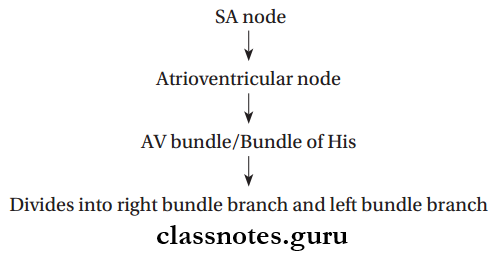
- Right bundle branch → Pass through the right side of the interventricular septum → Reaches the right ventricle → Divides into Purkinje fibers
- Left bundle branch → Pass through the left side of the interventricular septum → Reaches the left ventricle→ Divides into Purkinje fibers.
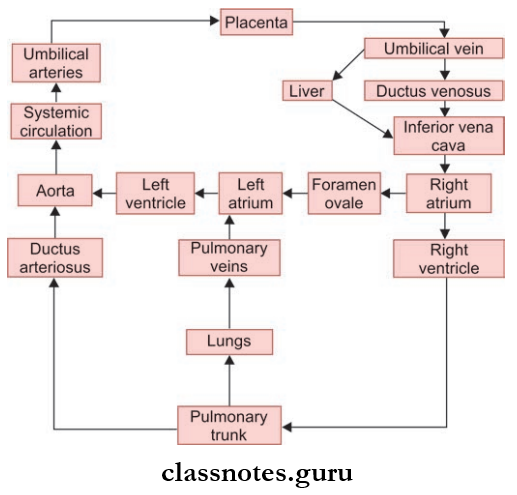
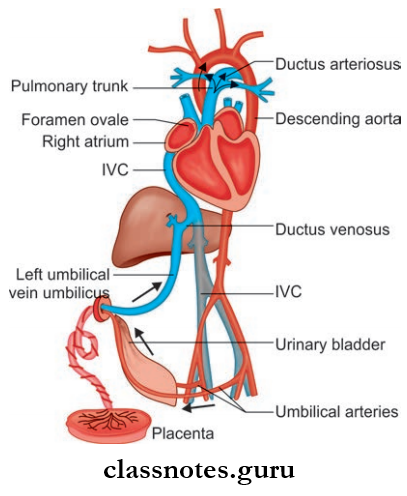
Question 17. Draw a flowchart depicting fetal circulation.
Answer:
Pericardium And Heart Multiple Choice Questions
Question 1. The only part of the heart not covered by serous pericardium is:
- The posterior wall of the left atrium
- The right wall of the oblique sinus
- Infundibulum of the pulmonary trunk
- The floor of the transverse sinus
Answer: 4. Floor of the transverse sinus
Question 2. Which of the following does not open into the right atrium?
- Anterior cardiac vein
- Small cardiac vein
- Coronary sinus
- Venae cordis minimi
Answer: 2. Small cardiac vein
Pericardium histology
Question 3. The apex of the heart is:
- Entirely formed by the left ventricle
- Formed by the right ventricle
- The greater part by the right ventricle
- The greater part formed by the left ventricle
Answer: 1. Entirely formed by the left ventricle
Question 4. All the following openings in the right atrium are guarded by valves except:
- Coronary sinus
- Superior vena cava
- Inferior vena cava
- Atrioventricular opening
Answer: 2. Superior vena cava
Question 5. The atrioventricular node lies at:
- Membranous interventricular septum
- Crista terminalis
- Interatrial septum
- Muscular interventricular septum
Answer: 3. Interatrial septum
Thoracic Cage Anatomy
Wall Of Thorax And Thoracic Cavity Question And Answers
Question 1. What is the thoracic cage?
Answer:
It is an osseocartilaginous skeletal framework.
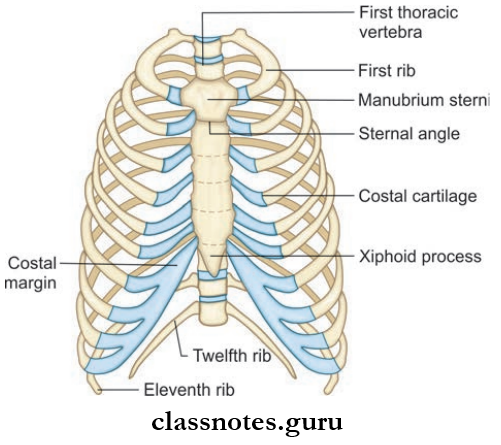
- Formed By
- Anteriorly: All 3 parts of the sternum (manubrium, body, and xiphoid)
- Posteriorly: All 12 thoracic vertebrae and intervertebral discs between them
- Laterally: 12 ribs and the costal cartilages to which the ribs are attached.
Read And Learn More: Thorax Anatomy
- The first 7 ribs (true ribs) articulate with the sternum through bicoastal cartilage.
- The 8th–10th ribs (false ribs) end by getting attached to the next higher cartilage.
- The anterior ends of the 11th and 12th ribs are free, so-called floating ribs.
- Ribs are attached posteriorly to the corresponding thoracic vertebrae.
- Atypical ribs: 1, 2, 10, 11, 12
- Typical ribs : 3, 4, 5, 6, 7, 8
- Costal cartilage : Hyaline cartilage.
Ossification Centers Of A Typical Rib
- Primary Center: Forms at the completion of the second month of fetal life
- Secondary Center: Forms at puberty.
Thoracic Cage Applied Anatomy
- Accessory ribs may sometimes be present
- Rib Attached To 7th Cervical Vertebrae: Cervical rib
- Rib Attached To Fist Lumbar Vertebrae: Lumbar rib
- Costal cartilages make the thorax more elastic, in old age costal cartilage calcifies and loses elasticity.
Thoracic Cage Joints
- First Cartilage With Manubrium Sternum: Synchondrosis
- 2nd-7th Cartilage With Sternum: Synovial joint
- 8th, 9th, 10th Cartilage With Next Higher Cartilage: Synovial joint
Question 2. What is a thoracic inlet?
Answer:
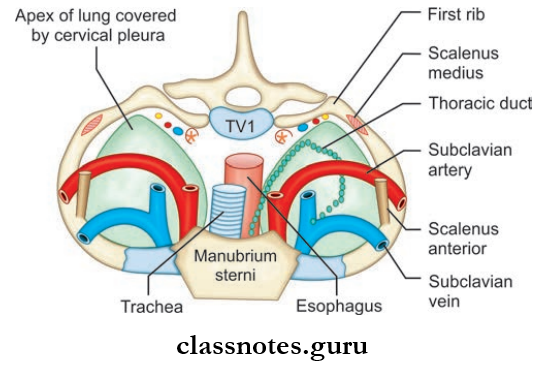
Thoracic Inlet
- The Thoracic Inlet is the upper end of the thorax
- Also known as superior thoracic aperture
- Thoracic Inlet is a kidney-shaped, narrow opening
- Its size corresponds to the diameter of the neck
Thoracic Inlet Boundaries
- Anteriorly: Upper border of manubrium sterni
- Posteriorly: Upper end of the body of T1 vertebrae
- Laterally: Inner border of the first rib and its cartilage
- The thoracic inlet is divided into two halves, each half is formed by a subpleural membrane (it is fused with conical pleura inferiorly)
- There is a central cleft in between both halves.
Important Structures Passing Through The Inlet
- Trachea, Esophagus, lung apices
- Muscles: Sternohyoid, sternothyroid
- Blood vessels
- Brachiocephalic artery
- Left common carotid and left subclavian artery
- Internal thoracic artery
- Brachiocephalic veins
- Nerves: Phrenic nerves, vagus nerves, sympathetic trunk.
Question 3. What is a thoracic outlet?
Answer:
Thoracic Outlet
- The Thoracic Outlet is the inferior aperture of the thorax.
- The Thoracic Outlet is separated from the abdominal cavity by the diaphragm.
- Its size corresponds to the diameter of the upper part of the abdomen.
Thoracic Outlet Boundaries
- Anteriorly: 7th–10th costal cartilages
- Posteriorly: Lower border of 12th thoracic vertebrae
- Laterally: 11th and 12th pairs of ribs.
Since the inferior aperture is closed by the diaphragm, structures from the thorax to the abdomen have to pass through large and small openings in the diaphragm.
Bones of thoracic cage
Question 4. Write briefly about the boundaries and contents of the scalene triangle.
Answer:
Scalene Triangle
- Narrow triangular space
- Boundaries
- Anteriorly: Scalenus anterior
- Posteriorly: Scalenus medius
- Inferiorly: Upper surface of first rib
- Contents
- Subclavian artery
- Lower trunk of brachial plexus.
Scalene Triangle Applied Anatomy
- Cervical rib syndrome: Due to the presence of a cervical rib or a congenitally hypertrophied scalenus anterior muscle.
- The scalene triangle gets narrowed and results in compression of the lower trunk of the brachial plexus and subclavian artery.
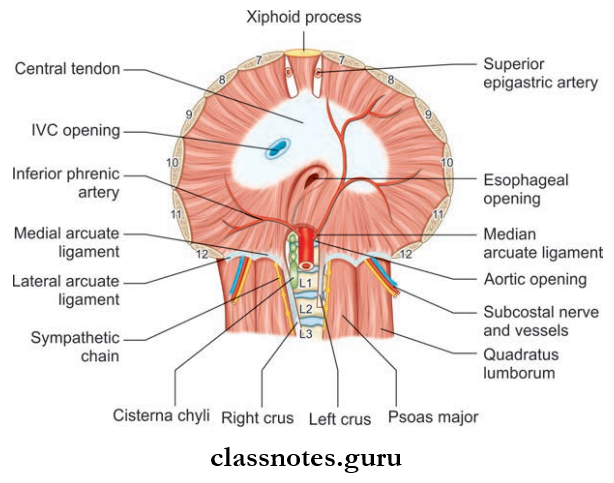
Question 5. Describe in detail about the origin and insertion of the diaphragm. What is meant by the dome of the diaphragm?
Answer:
It is a large muscle that closes the thoracic outlet
Diaphragm Formation: It has 3 points of origin
- Sternal Part: Arise from the back of the xiphoid process as two slips, right and left
- Costal Part: Consisting of broad slips arising from the inner surface of 7th–12th ribs and their costal cartilage
- Lumbar Part: Consists of right and left crura, which arises from
- The anterolateral surface of a body of lumbar vertebrae
- Medial and lateral arcuate ligaments
- Medial arcuate ligament: Fascia covering psoas major
- Lateral arcuate ligament: Fascia covering quadratus lumborum
- Medial margins of two crura are joined to each other to form a median (not medial) arcuate ligament at the level of the lower border of T-12 vertebrae
Diaphragm Insertion
All muscular fibers of the diaphragm run upwards and converge to get inserted into the flat central tendon (located below the pericardium)
Dome Of Diaphragm
- It is the upper convex part of the diaphragm
- The central part of the dome is made of central tendon
- And peripheral part by muscular fibers.
Question 6. What are the openings of the diaphragm? What are the structures passing through it?
Answer:
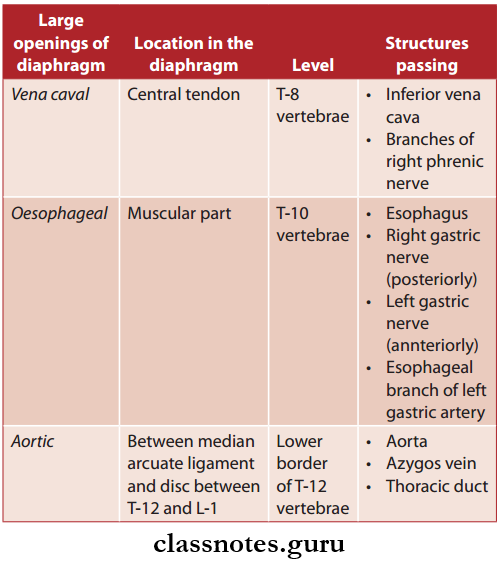
Mneumonic—Voice Of America (VOA)
Structures Passing Through Small Openings
- Superior epigastric artery
- Musculophrenic artery
- 8th–11th intercostals nerves and vessels
- Subcostal nerves and vessels
- Sympathetic trunk
- Splanchnic nerves.
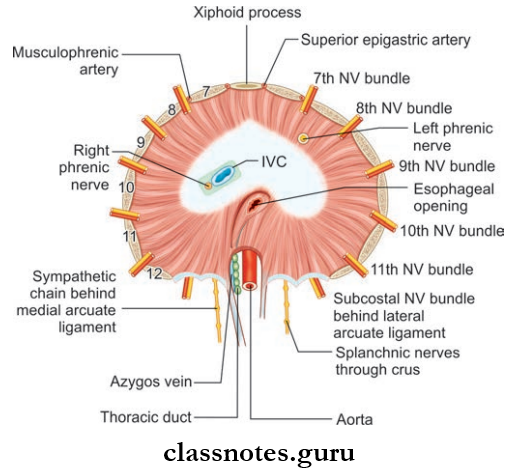
Abbreviation: IVC = Inferior vena cava; NV = Neurovascular
Question 7. What is the nerve supply of the diaphragm?
Answer:
Nerve Supply of Diaphragm
- Sensory supply: Lower six intercostals nerves, right and left phrenic nerves
- Motor supply: Right and left phrenic nerves.
Question 8. Write a note on the development of the diaphragm.
Answer:
Development Of Diaphragm
- Central tendon from septum transversum
- A dorsal-paired portion of the diaphragm from the pleuroperitoneal membrane. A circumferential portion from the lateral thoracic wall
- A dorsal unpaired portion from the dorsal mesentery of the esophagus.
Question 9. Write a note on intercostal space–muscles, nerves, blood supply, and lymphatic drainage.
Answer:
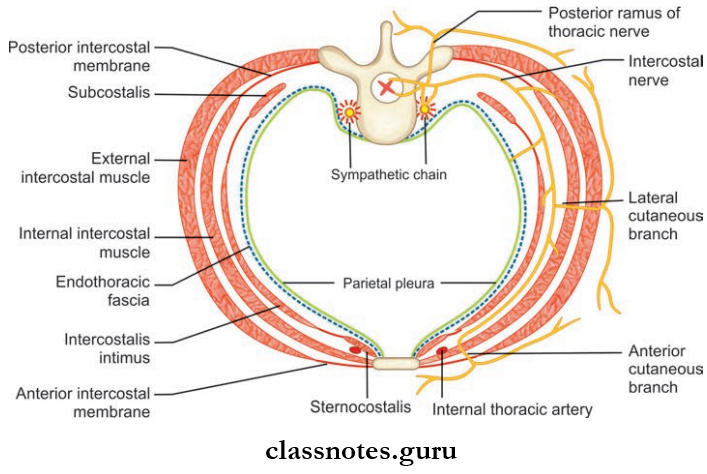
Intercostal Space
- The space between two adjacent ribs and their costal cartilages is called intercostal space
- There are 11 intercostal spaces between 12 ribs on both sides:
- Intercostal space contains
- Intercostal muscles
- Intercostal nerves, vessels, and lymphatics
- Intercostal space contains
- 3rd–6th intercostal spaces formed between the typical ribs are traversed by vessels and nerves which are confined only to the thorax. As a result, these intercostal spaces are called typical intercostal spaces.
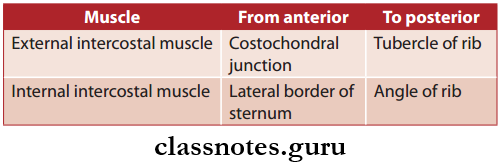
Intercostal Muscles They are arranged in three layers:
- External intercostal muscles
- Internal intercostal muscles
- Innermost muscles: Sternocostalis, intercostalis intimi, subcostalis.
1. External Intercostal Muscles: Takes origin from the lower margins of ribs 1 to 11, and is inserted on the upper margin of the rib just below it.
- External Intercostal Muscles Parts It has 2 parts, namely:
- Fleshy interosseous part: Located between the ribs
- Membranous interchondral part: Located between the adjacent costal cartilages.
2. Internal Intercostal Muscles: Takes origin from the lower margins of ribs and costal cartilage and to the floor of the costal groove, and are inserted on the upper margin of the rib and costal cartilage just below it
- Internal Intercostal Muscles Parts: It also has 2 parts, namely:
- Fleshy Part: Long part, located between the anterior end of intercostal space to the angle of the rib
- Membranous Part: Short part, located beyond the angle of the rib.
- Internal Intercostal Muscles Extent
- External intercostal muscle is replaced by an external intercostal membrane, between the costochondral junction and sternum but posteriorly it is continuous with the posterior fibers of the superior costotransverse ligament
- The internal intercostal muscle is continuous posteriorly as an internal intercostal membrane.
3. Innermost Intercostal Muscles
- Innermost Intercostal Muscles Sternocostalis:
- The anterior part of the innermost muscles
- Lies behind the sternum and costal cartilage
- Innermost Intercostal Muscles Intercostalis intimi
- Present on the middle two fourth of intercostal space
- Innermost Intercostal Muscles Subcostalis
- Present over the posterior part of intercostal space.
Diaphragm Nerve Supply All intercostal muscles are supplied by intercostal nerves of the corresponding space.
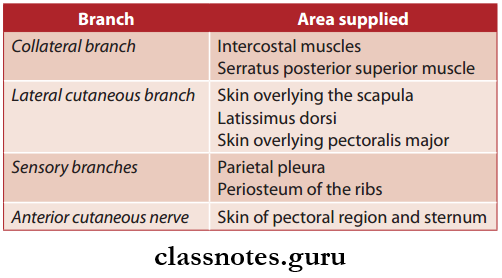
Intercostal Nerves
- They are derived from the anterior primary rami of T1 to T11 spinal nerves
- They are eleven in number
- Anterior primary rami of T 12 spinal nerve gives rise to the subcostal nerve (It runs in the abdominal wall below the 12th rib)
Classification Of Intercostal nerves are classified into:
- Typical Intercostal Nerves
- They are confined to their own intercostal spaces in the thoracic wall
- 3rd, 4th, 5th and 6th intercostal nerves.
- Atypical Intercostal Nerves
- They extend beyond the thoracic wall and partly or completely supply other areas
- 1st, 2nd, 7th, 8th, 9th, 10th and 11th intercostal nerves.
The Course Of A Typical Intercostal Nerve
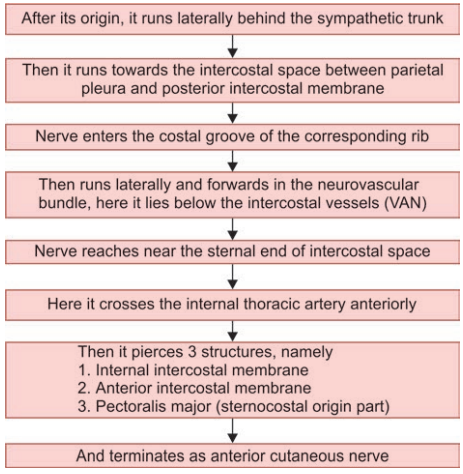
Branches of Typical Intercostal Nerves
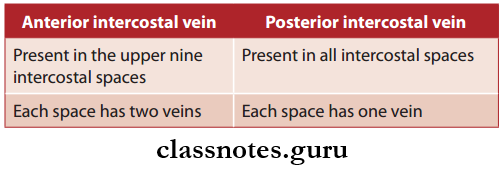
Intercostal Arteries
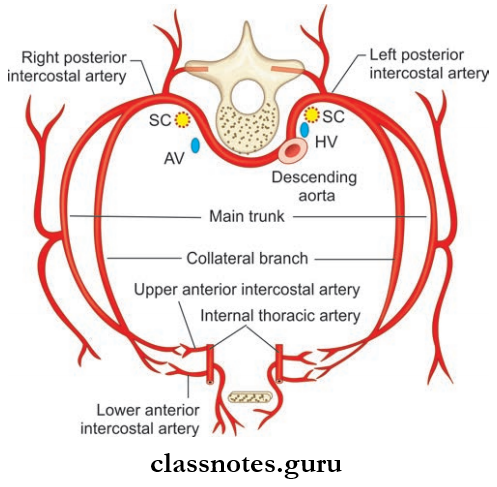
The Upper Nine Intercostal Spaces Contain Three Arteries:
- Single large posterior intercostal artery
- Two small anterior intercostal arteries
- The 10th and 11th spaces only contain a single posterior intercostal artery.
Posterior Intercostal Arteries
In the upper two intercostal spaces, the posterior intercostal arteries are branches of the superior intercostal artery.
Drainage Origin
- In the lower nine intercostal spaces, the posterior intercostal arteries arise from the descending thoracic aorta
- Right intercostal arteries in the lower nine intercostal spaces are longer than left since the descending thoracic aorta lies near the left of the vertebral column.
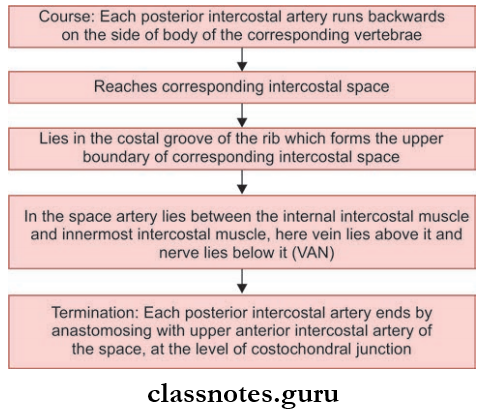
Drainage Branches
- Muscular Branches: Supply intercostal, pectoral, and serratus anterior muscle.
- Dorsal Branches: Supply vertebrae, spinal cord, muscles, and skin of the back.
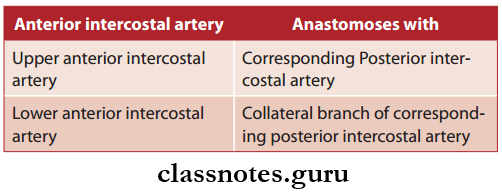
Anterior Intercostal Arteries: There are two anterior intercostal arteries each in the upper nine intercostal spaces.
Anterior Intercostal Arteries Origin
- Upper six spaces: Internal thoracic artery.
- 7th–9th spaces: Musculophrenic artery.
Anterior Intercostal Arteries Termination
Lymphatic Drainage of Intercostal Space
Lymphatics From The Anterior Part Of Intercostal Space: Anterior Intercostal Nodes.
Lymphatics from the anterior part of intercostal space: Posterior intercostal nodes.
Structure of thoracic cage
Question 10. Describe the origin, course, and branches of the internal thoracic artery. Write a brief on the internal thoracic vein.
Answer:
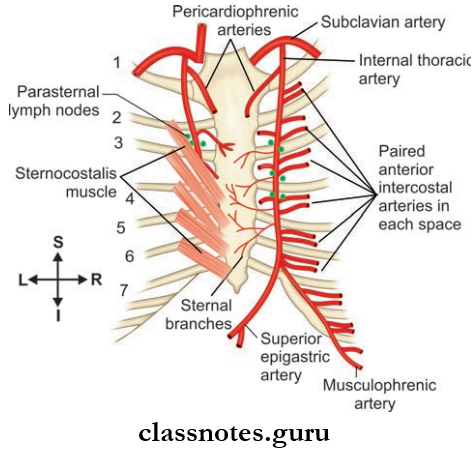
The internal thoracic artery is also known as the internal mammary artery.
Internal Thoracic Artery Origin
Two cm above the sternal end of the clavicle, from the inferior part of the first part of the Subclavian artery.
Internal Thoracic Artery Course
- Runs medially and downwards behind the sternal end of the clavicle and fist costal cartilage
- The runs downwards behind the fist to sixth costal cartilage (about 1 cm lateral to sternal margin). And terminates in the 6th intercostal space by dividing into two arteries.
- Musculophrenic artery
- Superior epigastric artery
- In its course, the internal thoracic artery also has several other branches, namely:
Anterior Intercostal Arteries
- Two anterior intercostal arteries are given off to each upper six intercostal spaces.
- In each intercostal space, two anterior intercostal arteries anastomoses with posterior intercostal artery.
Pericardiophrenic Branches
- Pericardiophrenic is given near the upper end of the internal thoracic artery.
- Pericardiophrenic runs downwards along with the phrenic nerve and reaches the diaphragm, supplying the pericardium and pleura.
Perforating Branches
- Given in the upper six intercostal spaces.
- Supplies Pectoralis major muscle and Breast.
- From 2nd to 4th intercostal spaces, these branches are found to be larger in females (to supply breasts).
1. Musculophrenic Artery
- The lateral terminal branch of the internal thoracic artery.
- Course: From the origin, it runs downward and laterally deep into the coastal margin.
- Reaches the abdominal wall by passing through a small opening in the diaphragm.
- Branches: Anterior intercostal branches to the 7th, 8th, and 9th intercostal spaces.
2. Superior Epigastric Artery
- The medial terminal branch of the internal thoracic artery
- Course: Runs downwards through the gap between coastal and xiphoid origin of the diaphragm into the abdomen
- It supplies the anterior mediastinum, pericardium, and diaphragm.
3. Applied Anatomy
The internal thoracic artery is the commonly used coronary graft since it is less prone to develop atherosclerosis due to its histological peculiarity (its wall contains elastic tissue only).
Internal Thoracic Vein
- The internal thoracic artery is accompanied by a number of small veins.
- These veins eventually join each other forming one large vessel, the internal thoracic vein.
- Course: Runs upwards through the medial aspect of the internal thoracic artery.
- Termination: Drain into Brachiocephalic vein.
- Tributaries: Corresponds to branches of the internal thoracic artery.
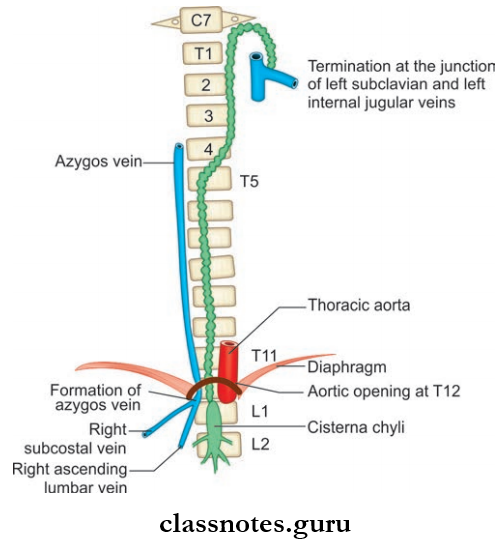
Question 11. Write a note on the azygos vein.
Answer:
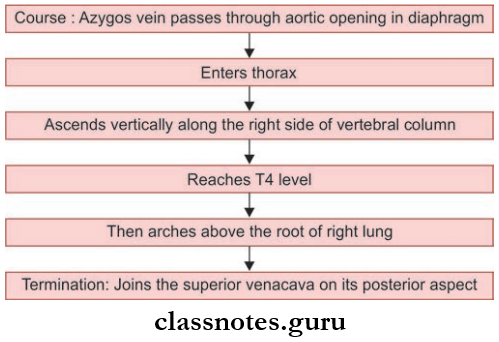
Azygos Vein
- It is present only on the right side (azygos means unpaired)
- Arises opposite to L1 or L2 vertebrae
Azygos Vein Formation: Formed by the union of the lumbar azygos vein, right subcostal vein, and right ascending lumbar vein.
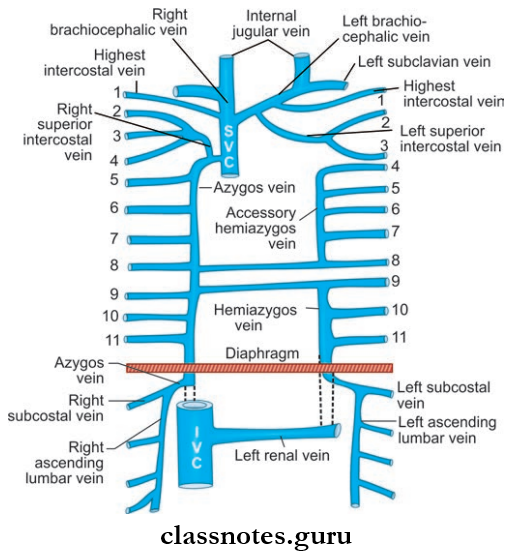
- Lumbar Azygos Vein:
- It lies right of the lumbar vertebrae
- Its lower end communicates with the inferior vena cava
- Its upper end joins with other veins of the azygos system to form the azygos vein
- Right Subcostal Vein:
- It accompanies the corresponding artery
- Right Ascending Lumbar Vein:
- It is a vertical channel connecting lumbar veins (Sometimes, the lumbar azygos vein may be absent, then the azygos vein is formed by the subcostal vein and ascending lumbar vein)
Thoracic skeleton
- Applied Anatomy
- Since the azygos vein forms a channel between the superior vena cava and inferior vena cava, in the case of the superior vena cava obstruction acts as the main channel through which blood from the upper half of the body is transmitted to the inferior vena cava.
Question 12. Write a note on the hemiazygos vein.
Answer:
Hemiazygos Vein
- Also known as the inferior azygos vein, since it is the mirror image of the lower part of the azygos vein.
- Present only on the left side.
- Formation: By union of left ascending lumbar vein and left subcostal vein.
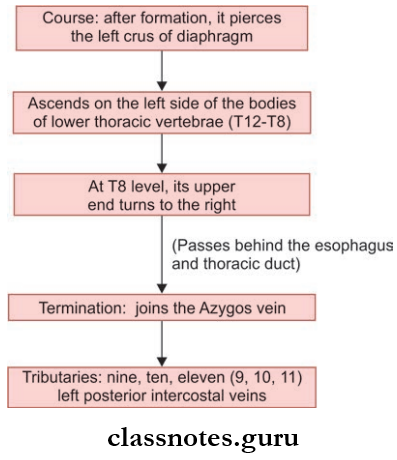
Question 13. Write a note on the accessory hemiazygos vein.
Answer:
- Also known as the superior azygos vein, since it is the mirror image of the upper part of the azygos vein.
- It is also connected superiorly to the left superior intercostal vein.
- Sometimes it joins the hemiazygos vein or has a connection to both the azygos and hemiazygos vein.
Tributaries:
4th to 8th left posterior intercostal veins.(Sometimes left bronchial veins also join with it).
Question 14. What is thoracic sympathetic trunk and what are its branches?
Answer:
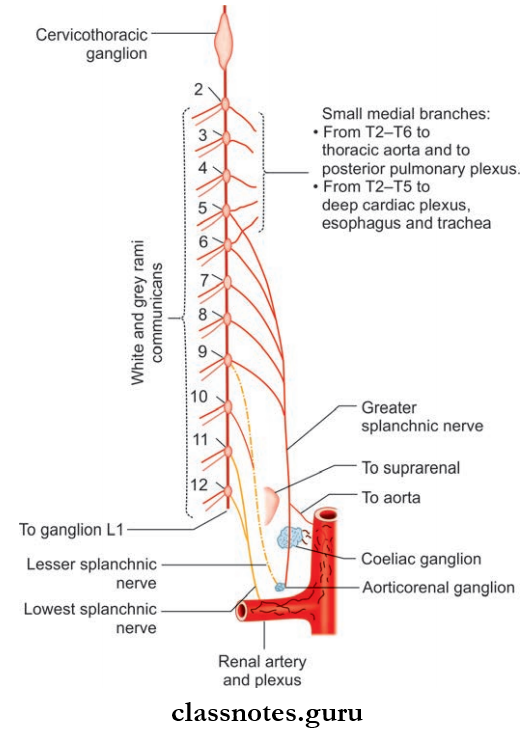
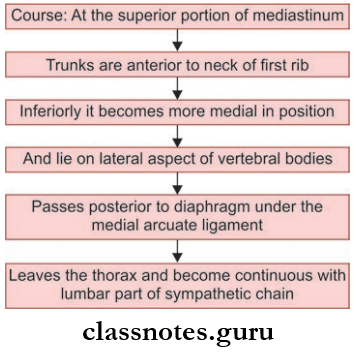
Thoracic Sympathetic Trunk
- The sympathetic trunk is a long nerve cord extending from the base of the skull to the coccyx.
- The thracic part of the sympathetic trunk is situated on both sides of the thoracic vertebral column (one each per side), in front of the heads of ribs, and is a ganglionated chain.
- It is considered a component of the posterior mediastinum since they pass through it.
- There are 12 thoracic ganglia, but the fist thoracic ganglion is fused with the inferior cervical ganglion, to form a cervicothoracic ganglion
- So the lower eleven (T2-T12) thoracic ganglia are considered as true thoracic ganglia.
Arteries of Thorax
Thoracic Sympathetic Truck Branches
- Laterally: Sympathetic ganglia is connected to adjacent
- Thoracic spinal nerves by white and grey rami communicans.
Medially: It supplies the viscera.
Medial branches arising from T1-T5 ganglia are postganglionic, they are connected to the nerve plexus supplying viscera
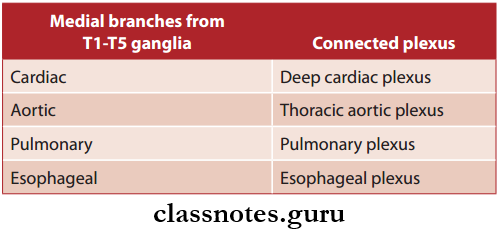
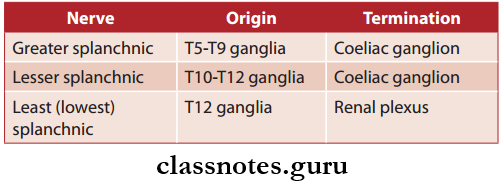
Medial branches from T6-T12 are preganglionic, they join together and form three nerves, they are:
Wall Of Thorax And Thoracic Cavity Multiple Choice Questions
Question 1. Which is considered a ‘false’ rib?
- 1
- 2
- 3
- 11
Answer: 4. 11
Question 2. All the following structures pass through the superior aperture of thorax except:
- Left common carotid artery
- Left sympathetic trunk
- Right recurrent laryngeal nerve
- Thoracic duct
Answer: 3. Right recurrent laryngeal nerve
Question 3. Which rib usually articulates with more than one vertebral body?
- Rib 1
- Rib 2
- Rib 11
- Rib 12
Answer: 2. Rib 2
Rib cage anatomy
Question 4. Azygos vein:
- Formed by the arch of the aorta
- Arches the groove of the left lung
- Opens in to inferior vena cava
- Ascends through the aortic opening in the diaphragm
Answer: 4. Ascends through the aortic opening in the diaphragm
Question 5. The external intercostal membrane is a continuation of the:
- Internal intercostal muscle
- Posterior intercostal muscle
- External intercostal muscle
- None of the above
Answer: 3. External intercostal muscle
Superior Mediastinum Anatomy
Mediastinum Question And Answers
Question 1. What are the boundaries of mediastinum and how is it divided?
Answer:
Boundaries of Mediastinum
- It lies between two lungs
- Boundaries
- Anteriorly: Sternum
- Posteriorly: Thoracic vertebral column (T1–T12)
- Superiorly: Thoracic inlet
- Inferiorly: Diaphragm
- Laterally: Mediastinal pleura
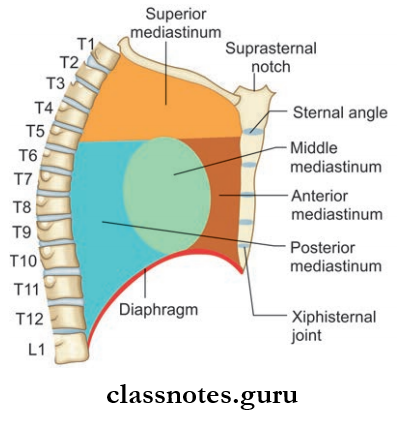
- Mediastinum is divided into:
- Superior mediastinum
- Inferior mediastinum
Read And Learn More: Thorax Anatomy
By a transverse plane passing through the sternal angle and the intervertebral disc between T4 and T5.
Superior mediastinum anatomy
Question 2. Write a note on superior mediastinum and what are its contents.
Answer:
Superior Mediastinum Boundaries:
- Anteriorly: Manubrium part of sternum
- Posteriorly: T1-T4 vertebrae and intervertebral discs between them
- Superiorly: Thoracic inlet
- Inferiorly: Transverse plane passing through the sternal angle and the intervertebral disc between T4 and T5
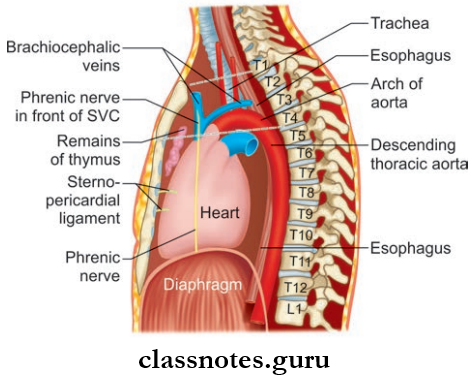
Superior Mediastinum Contents
- Phrenic nerve
- Vagus nerve
- Thoracic duct
- Left recurrent laryngeal nerve
- Brachiocephalic veins
- Aortic arch and its 3 branches (Brachiocephalic artery, left common carotid artery, left Subclavian artery)
- Mnemonic: PVT Left BAttle
- Muscles: Sternothyroid, sternohyoid
- Other veins left superior intercostal vein, superior vena cava (upper part)
- Trachea and esophagus
- Thmus.
Question 3. Write a note on inferior mediastinum and what are its divisions and contents.
Answer:
Inferior Mediastinum Boundaries:
- Anteriorly: Body of sternum
- Posteriorly: T5-T12 vertebrae and intervertebral discs between them
- Superiorly: Transverse plane passing through the sternal angle and the intervertebral disc between T4 and T5
- Inferiorly: Diaphragm (superior surface)
- Laterally (on both sides): Mediastinal pleura.
The inferior mediastinum is further subdivided into:
- Anterior mediastinum
- Middle mediastinum
- Posterior mediastinum.
- By the Pericardial sac.
Anterior Mediastinum Boundaries:
- Anteriorly: Body of sternum
- Posteriorly: Pericardium
- Laterally (on both sides) : Mediastinal pleura
- Superiorly: Transverse plane passing through the sternal angle and the intervertebral disc between T4 and T5
- Inferiorly: Diaphragm (superior surface).
Anterior Mediastinum Contents:
- Mediastinal branches of internal thoracic artery
- Sternopericardial ligaments
- Lymphatics and lymph nodes
- Thus.
Middle Mediastinum Boundaries:
- Anteriorly: Sternopericardial ligaments
- Posteriorly: Azygos vein, descending aorta,
- Esophagus
- Laterally (on both sides): Mediastinal pleura
- Superiorly: Transverse plane passing through the sternal angle and the intervertebral disc between T4 and T5
- Inferiorly: Diaphragm (superior surface).
Middle Mediastinum Contents
- Pericardium and the heart
- Arteries: Ascending aorta, pulmonary trunk and pulmonary arteries
- Veins: Superior vena cava, azygos vein, pulmonary veins
- Nerves: Deep cardiac plexus and phrenic nerve
- Tracheobronchial lymph nodes
- Bifurcation of trachea and principal bronchi.
Posterior Mediastinum Boundaries:
- Anteriorly
- Pericardium
- Pulmonary vessels
- Bifurcation of trachea
- Posteriorly: T5–T12 vertebrae and the intervertebral discs between them
- Laterally (on both sides): Mediastinal pleura
- Superiorly: Transverse plane passing through the sternal angle and the intervertebral disc between T4 and T5
- Inferiorly: Diaphragm (superior surface).
Posterior Mediastinum Contents:
- Arteries: Descending thoracic aorta and its branches
- Veins: Azygos, hemiazygos, and accessory hemiazygos veins
- Nerves: Vagus nerve, splanchnic nerve
- Posterior mediastinal lymph nodes
- Esophagus
- Thoracic duct.
Mnemonic: Posterior mediastinum structures. There are four birds:
- The esophagus (esophagus)
- The vaGOOSE nerve
- The azyGOOSE vein
- The thoracic DUCK (duct).
Anatomy of superior mediastinum
Mediastinum Multiple Choice Question
Question 1. The contents of the anterior mediastinum in an adult are all except:
- Thymus gland
- Phrenic nerve
- Branches of internal thoracic artery
- Areolar tissue
Answer: 1. Thymus gland
Question 2. The posterior mediastinum has the following except:
- Esophagus
- Thoracic duct
- Inferior vena cava
- Right descending thoracic aorta
Answer: 4. Right descending thoracic aorta
Structures in superior mediastinum
Question 3. Which of the following structures is/are located entirely within the mediastinum?
- Thoracic duct
- Phrenic nerves
- Pericardial sac
- Vagus nerves
Answer: 3. Pericardial sac
Question 4. A tumor growing in the posterior mediastinum could directly affect which of the following structures?
- Azygos vein
- Superior vena cava
- Aortic arch
- Right atrium of the heart
Answer: 1. Azygos vein
Question 5. The thymus is located in:
- Posterior mediastinum
- Anterior mediastinum
- Middle mediastinum
- Superior mediastinum
Answer: 2. Anterior mediastinum
Pleurae Anatomy
Pleurae Question And Answers
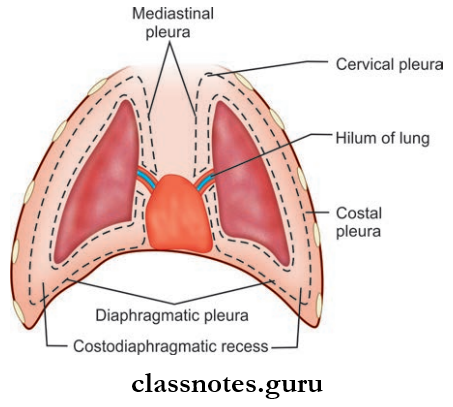
Question 1. Write a short note on pleural cavities and the types of pleura.
Answer:
Pleural Cavities
- Pleural cavities are present on both sides of the mediastinum
- They envelop the lungs.
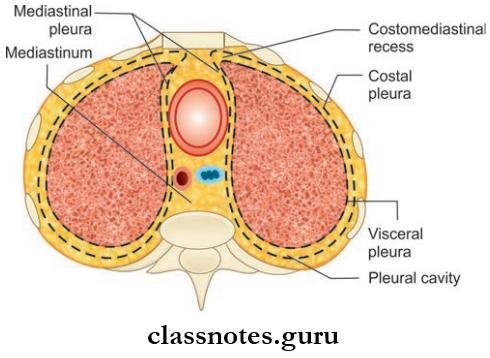
Pleural Cavities Extent:
- Superiorly: Above the fist rib (4 cm above fist costal cartilage)
- Inferiorly: Up to a level, just above the costal margin
- Medially: Related to the mediastinum.
Read And Learn More: Thorax Anatomy
Pleura
- Pleura are thin serous membranes
- Pleura is formed by:
- Mesothelium (single layer of fat cells)
- Connective tissue
- Pleura is divided into two, based on the location
- Parietal Pleura: Outer layer of pleural cavity
- Visceral Pleura (Pulmonary Pleura): Firmly attached to lung surfaces and fissures
- The pleural cavity is actually the space between the parietal and visceral pleura
- It is filled with a thin layer of serous fluid, this helps to reduce friction between the visceral and parietal pleura, so that the visceral pleura can freely slide over the parietal pleura.
Parietal Pleura
- Due to its close relation with the thoracic wall
- It is divided into four parts, based on the part of the thoracic wall to which it is related:
- Costal Pleura:
- Costal Pleura lines the inner aspect of ribs and intercostal spaces and also an inner aspect of the sternum
- The Costal Pleura is loosely attached to the corresponding surfaces through the endo thoracic fascia.
- Diaphragmatic Pleura:
- The diaphragmatic Pleura covers the upper surface of the diaphragm.
- Mediastinal Pleura
- Mediastinal Pleura is part of the pleura covering the mediastinum
- Between T 5 and T 7 levels, the mediastinal pleura extends as a sleeve-like tube over the structures passing between the mediastinum and the lung (pulmonary vessels, bronchus)
- The tubular covering of the mediastinal pleura along with the structures passing through it forms the root of the lung
- Mediastinal pleura becomes continuous with the visceral pleura at the hilum of the lung.
- Cervical Pleura
- Also known as the Dome of Pleura
- Cervical Pleura is a dome-shaped layer
- Cervical Pleura extends 5 cm above the first costal cartilage and 2.5 cm above the medial 1/3rd of the clavicle
- The cervical pleura is covered superiorly by the Suprapleural membrane
Parietal Pleura Relations:
- Anteriorly
- Scalenus anterior muscle
- Subclavian artery
- Posteriorly
- First rib
- Cervicothoracic ganglion
- Superior intercostal artery
Nerve Supply Of Parietal Pleura:
They are supplied by somatic afferent fibers through intercostal nerves and phrenic nerves
Costal Pleura: Intercostal nerve
Diaphragmatic pleura and mediastinal pleura: Phrenic nerve.
Parietal Pleura Applied Anatomy
- Since the costal pleura is innervated by intercostal nerves, its pain is felt to the thoracic wall
- Since diaphragmatic and mediastinal pleura are innervated by phrenic nerves, pain is felt on the supraclavicular region and lateral surface of the neck.
Visceral Pleura
- Also known as the pulmonary pleura
- It is firmly attached to the surfaces and fissures of the lung
- It is continuous with the parietal pleura at the hilum
- Nerve supply: By visceral afferent nerves, so, as a result, its pain is insensitive.
Anatomy of pleura
Question 2. What is the pulmonary ligament?
Answer:
Pulmonary Ligament
- The parietal pleura runs downwards as a thin fold from the root of the lung and extends beyond the hilum up to the mediastinum, known as the pulmonary ligament
- It contains loose areolar tissue and few lymphatics
- It stabilizes the position of the inferior lobe and also acts as a space for pulmonary veins to expand during increased venous return.
Question 3. Write a note on pleural recess.
Answer:
Pleural Recess
- In normal quiet respiration, the lungs do not fully occupy the anterior and inferior regions of the pleural cavity
- These regions/spaces are called a pleural recess
- They are spaces provided for the lungs to expand during deep inspiration
- Costomediastinal Recess
- Anterior recess, formed by costal and mediastinal pleura
- Lies behind sternum and costal margin
- The left costomediastinal recess is larger than the right
- In normal quiet respiration, the right costomediastinal recess is filed, but a part of the left costomediastinal recess is free due to the presence of cardiac notch.
- Costodiaphragmatic Recess
- Largest recess
- Recess used for clinical purposes
- Formed between costal and diaphragmatic pleura
- Lies inferiorly
- Extent: From 8th to 10th ribs in the mid-axillary line
- Vertically it is about 5 cm long
- Only gets filed during deep inspiration.
- Pleural Recess Applied Anatomy
- Pneumothorax: The pleural cavity sometimes gets filled with air
- Traumatic Pneumothorax: It can be due to injury to the thoracic wall or lung, leading to leakage of air into the pleural cavity
- Spontaneous pneumothorax: Occurs by leakage of air from the lung, resulting from rupture of cysts or lesions, it is associated with pulmonary tuberculosis.
Question 4. Write a brief on the blood supply and lymphatic drainage of the pleura.
Answer:
Parietal Pleura
1. Arterial Supply:
- Intercostal arteries
- Internal thoracic artery
- Musculophrenic artery.
2. Venous Drainage: Azygos vein and internal thoracic vein.
Visceral/Pulmonary Pleura
- Arterial supply: Bronchial arteries
- Venous drainage: Bronchial veins.
Lymphatic Drainage Of Pleura
1. Parietal Pleura
- Intercostal lymph nodes
- Internal mammary lymph nodes
- Posterior mediastinal lymph nodes
- Diaphragmatic lymph nodes.
2. Visceral/Pulmonary Pleura:
Bronchopulmonary Lymph Nodes
Pleural cavity anatomy
Pleurae Multiple Choice Questions
Question 1. ‘Pulmonary cavity’ and ‘pleural cavity’ are different names for the same thing:
- True
- False
Answer: 2. False
Question 2. The lowest extent of the pleural cavity into which tissue does not extend is known as:
- Costodiaphragmatic recess
- Costomediastinal recess
- Cupola
- Inferior mediastinum
Answer: 1. Costodiaphragmatic recess
Question 3. At which location is the parietal pleura continuous with visceral pleura?
- On the surface of the mediastinum
- Throughout the entire pulmonary cavity
- At the hilum of the lungs
- On the diaphragm
Answer: 3. At the hilum of the lungs
Pleura histology
Question 4. The portion of the parietal pleura that extends above the first rib is called the:
- Costodiaphragmatic recess
- Costomediastinal recess
- Costocervical recess
- Cupola
Answer: 4. Cupola
Question 5. The pleural cavity near the cardiac notch is known as the:
- Costodiaphragmatic recess
- Costomediastinal recess
- Cupola
- Hilum
- Pulmonary ligament
Answer: 2. Costomediastinal recess
Lung Anatomy
Lungs Questions and Answers
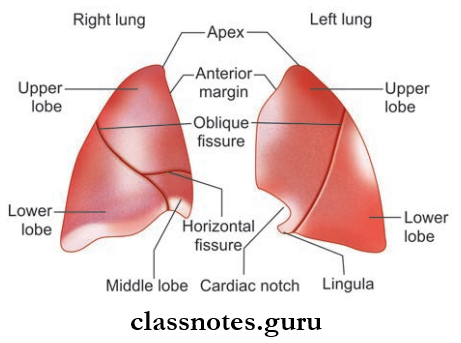
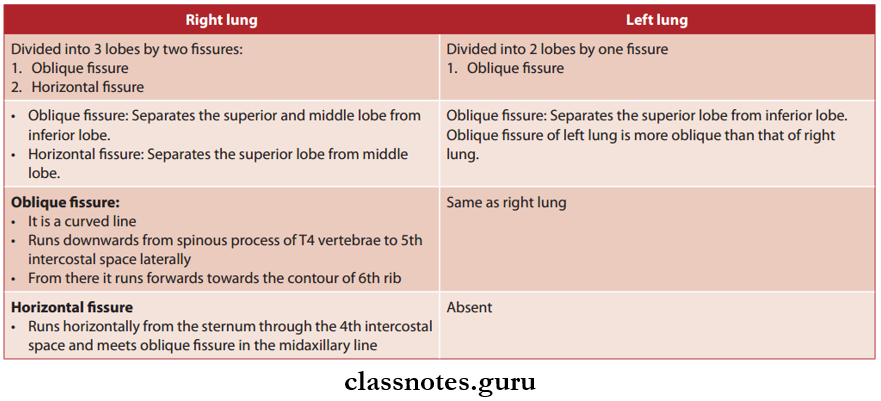
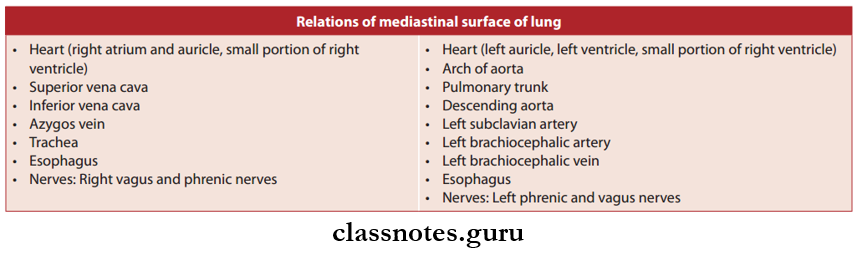
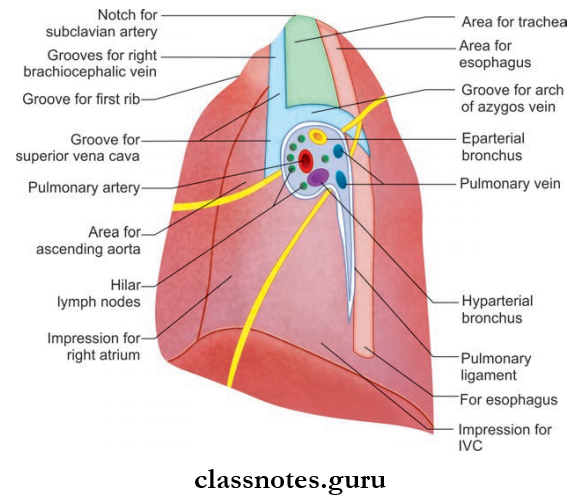
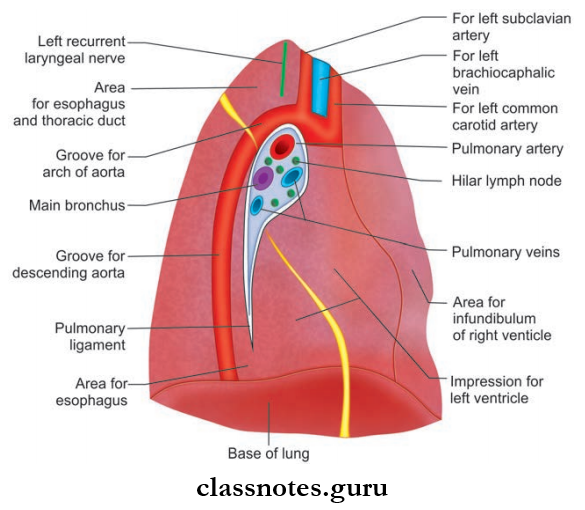
Question 1. Describe the gross features of the right and left lungs. Mention the relations of mediastinal surface of both lungs.
Answer:
Right And Left Lungs
- Paired organs of respiration
- Lie on either side of the mediastinum
- They are covered by pleura
Read And Learn More: Thorax Anatomy
- Lungs receive air through the bronchi, which are the continuations of the trachea
- The right lung is larger than the left (since the heart bulges more to the left)
- At birth it is grey in color, later it becomes black due to the deposition of carbon particles through inhalation
- Weight: Right lung – 700 g, left lung 600–650 g
- Shape: Cone-shaped
- It has:
- Apex: Upper end, 2.5 cm above the medial 1/3rd of the clavicle
- Base (Broader inferior surface): Sits on the diaphragm
- Two surfaces:
- Costal Surface
- Rounded lateral surface
- It is in relation to ribs and intercostal spaces
- Mediastinal Surface
- Medial surface
- Mediastinal Surface Relations:
- Anteriorly: Mediastinum
- Posteriorly: Thoracic vertebral column
- Three borders
- Anterior Border: Sharp border
- Lies anteriorly
- It separates costal and mediastinal surfaces
- Posterior Border: Smooth rounded border
- It separates the vertebral and costal surfaces
- Inferior Border: Sharp border
- It separates the base from the other two surfaces.
- Anterior Border: Sharp border
- All the surfaces of the lung are covered by the visceral pleura except at an area in the mediastinal surface, called as the hilum
- The pulmonary artery and principal bronchus enter the lung and the pulmonary vein leaves the lung through the hilum.
Lung anatomy diagram
Lung structure and function
Right and Left Lungs Blood Supply of Lung
- Arterial Supply
- Right Side: One bronchial artery (Branch of 3rd posterior intercostal artery)
- Left Side: Two bronchial arteries (Branch of descending thoracic aorta).
- Venous Drainage
- Right Side
- Superior And Middle Lobes: Upper pulmonary vein
- Inferior Lobe: Lower pulmonary vein
- Left Side
- Superior Lobe: Upper pulmonary vein
- Inferior Lobe: Lower pulmonary vein
- Right Side
Right And Left Lungs Nerve Supply
- Receives autonomic nerves from the anterior and posterior pulmonary plexus.
- Sympathetic Nerves: Bronchial dilatation
- Parasympathetic Nerves: Bronchial constriction.
Lymphatic Drainage: Drained by two sets of vessels.
- Superficial
- Deep.
Right And Left Lungs Applied Anatomy
- Bronchitis: Inflmmation of the bronchi
- Pneumonia: Inflammation of the lung parenchyma
- Obstruction of the bronchus due to any cause can lead to the collapse of the part supplied by it.
Question 2. Write a note on the development of the lungs.
Answer:
Development Of Lungs
- Lungs develop from lung buds which develop at the caudal end of the laryngotracheal tube
- It divides into two knob-like bronchial buds, which grow into celomic ducts, the primordia of pleural cavities
- They are surrounded by splanchnic mesenchyme
- Each bronchial bud enlarges to form primary bronchus
- Primary bronchus on the right side forms superior and inferior secondary bronchi, and on the left side, forms two secondary bronchi for superior and inferior lobes
- The secondary bronchus forms the tertiary bronchus. Ten on the right and nine on the left side each And surrounding mesenchyme gives rise to a bronchopulmonary segment
- Cartilage, smooth muscles, connective tissue, and capillaries are derived from surrounding splanchnic mesenchyme
- Visceral pleura from splanchnic mesoderm and parietal pleura from somatopleuric mesoderm.
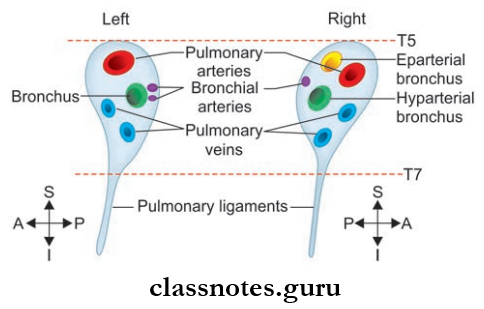
Question 3. What is the root of the lung?
Answer:
Root Of Lung
- The root Of the Lung is a short pedicle
- The root Of the Lung attaches the medial surface of the lungs to the mediastinum
- Root Of the Lung is formed by structures passing between the lungs and the mediastinum
- The root Of the Lung is covered by the mediastinal pleura, which is continuous with the visceral pleura at the hilum.
Structures Located At The Root
- Pulmonary artery
- Superior and inferior pulmonary veins
- Main bronchus
- Bronchial vessels: Arteries and veins (Arteries – one on the right side and two on the left side)
- Nerves
- Lymphatics
- Bronchopulmonary lymph nodes.
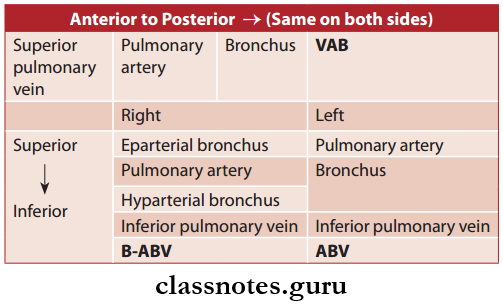
Arrangement Of Structures In The Root
Abbreviation: A = Artery; B = Bronchus; V = Vein
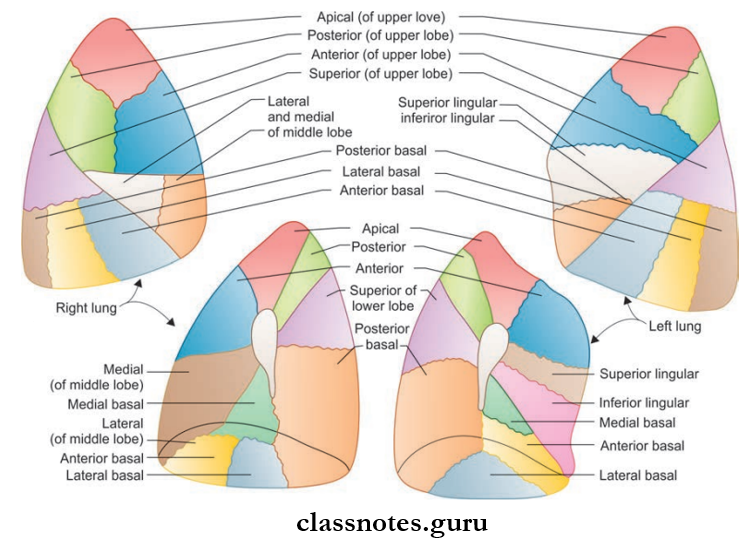
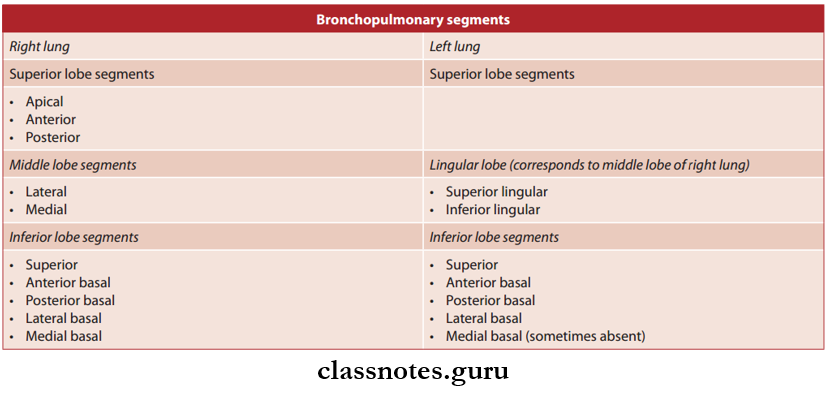
Question 4. Write a short note on bronchopulmonary segments.
Answer:
Bronchopulmonary Segments
- Bronchopulmonary segments are areas of the lung supplied by a single segmental bronchus.
- Each segmental bronchus is accompanied by a branch of the pulmonary artery.
- The artery lies in the dorsolateral aspect of the bronchus
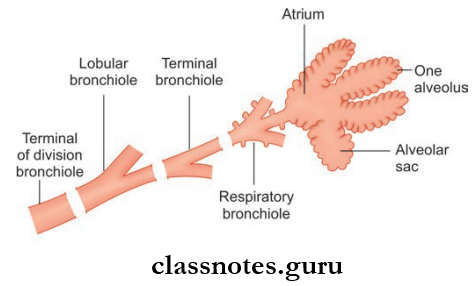
- The bronchopulmonary segment is functionally independent and is a well-defined anatomical and surgical segment of the lung
- That is, it is the smallest area of the lung that can be removed surgically without affecting adjacent areas of the lung
- There are 10 bronchopulmonary segments for each lung
- Each segment has the shape of an irregular cone
- It has:
- Apex: Present at the origin of segmental bronchus
- Base: Directed towards the surface of the lung
- Bronchopulmonary Segments Contents:
- Segmental bronchus
- Segmental artery
- Autonomic nerves
- Lymphatics
- Bronchopulmonary segments are drained by a segmental vein, which lies in the connective tissue between adjacent bronchopulmonary segments
- Pulmonary veins run between two segmental bronchus and thus drain more than one segment.
Human lung anatomy PDF
Bronchopulmonary Segments Applied Anatomy
Normally infection of bronchopulmonary segments remains confined to it, but tuberculosis can spread from one segment to another.
Lungs Multiple Choice Questions
Question 1. Above the hilum of the right lung, we find all except:
- Pulmonary artery and bronchial artery
- Bronchus
- Pulmonary vein
- Arch of aorta
Answer: 4. Arch of the aorta
Question 2. All the following options are true about bronchopulmonary segments except:
- They are surgically resectable
- Veins are present in between each segment
- Pyramidal in shape
- Secondary bronchus open into them
Answer: 4. Secondary bronchus open into them
Question 3. The right hilum of the lung consists of all the structures except:
- Pulmonary vein
- Pulmonary artery
- Bronchus
- Inferior vena cava
Answer: 4. Inferior vena cava
Lung anatomy for medical students
Question 4. Which one of the following structures passes posterior to the root of the right lung?
- hemiazygos vein
- Right vagus nerve
- Right phrenic nerve
- Thoracic aorta
- Right recurrent laryngeal nerve
Answer: 2. Right vagus nerve
Question 5. The lung is supplied by:
- Pulmonary artery
- Pulmonary vein
- Bronchial artery
- All the above
Answer: 3. Bronchial artery
