Beta Lactum Antibiotics Important Notes
1. Beta lactam antibiotics are
- Penicillins
- Cephalosporins
- Monbactem
- Carbepenems
2. Penicillin
- Has a wide therapeutic range
- Is the safest drug
- Penicillin Classification
- Natural – penicillin G, procaine penicillin, Benzathine penicillin
- Acid resistance penicillin – penicillin V, phenoxy ethyl penicillin
- Penicillinase resistance penicillin
- Acid labile – methicillin, cloxacillin, nafcillin
- Acid resistant – fucloxacillin
- Broad spectrum penicillin – ampicillin, amoxicillin, talampicillin
- Extended-spectrum penicillin – carbenicillin, ticarcillin
- Beta-lactamase inhibitors – augmentin, sulbactam
Read And Learn More: Pharmacology Question and Answers
- Penicillin Adverse effects
- Anaphylaxis
- Angioedema
- Superinfection
- JarischHerxheimer reaction
- Penicillin Uses
- Syphilis
- Actinomycosis
- Gonorrhoea
- Streptococcal infection
- Abscess
- Cellulitis
3. Carbenicillin
- It is neither Penicillinase resistance nor acid resistance
- It is inactive orally
- Rapidly excreted in urine
- It is active against Pseudomonas aeruginosa and indole-positive Proteus
Beta-lactam antibiotics examples
4. Benzathine penicillin
- It is a long-acting drug
- Given every 2-4 weeks
- Remains effective for prophylactic purposes for up to 4 weeks
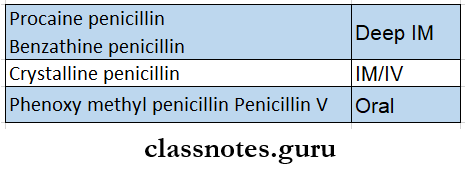
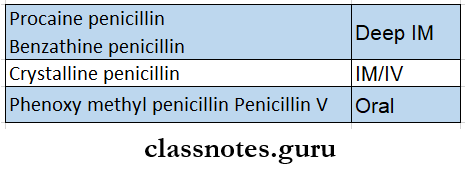
5. Drugs and their route of administration
6. Cephalosporins
- They have a 7-amino cephalosporin acid nucleus, which bears a close resemblance to the 6-APA nucleus of penicillin.
- They are effective against both Gram-positive and Gram-negative organisms
- They inhibit bacterial cell wall synthesis
- Doesn’t undergo any metabolism in the body except for cefotaxime
- Excreted by the kidneys except for cefoperazone
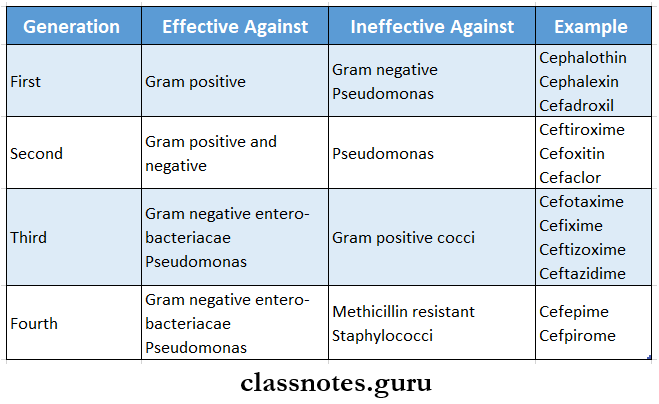
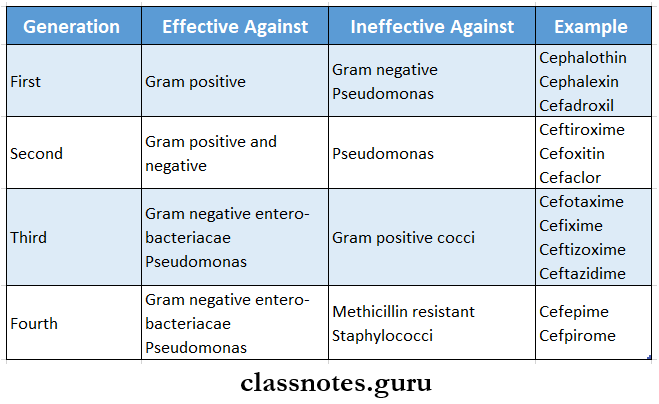
- Generations:.
Beta Lactum Antibiotics Long Essays
Question 1. Define antibiotic. Classify penicillin. Explain their mechanism of action, toxicity, and uses of penicillin G or Benzylpenicillin.
Answer:
Antibiotics:
These are substances produced by micro-organisms that selectively suppress the growth or kill other micro-organisms at very low concentrations.
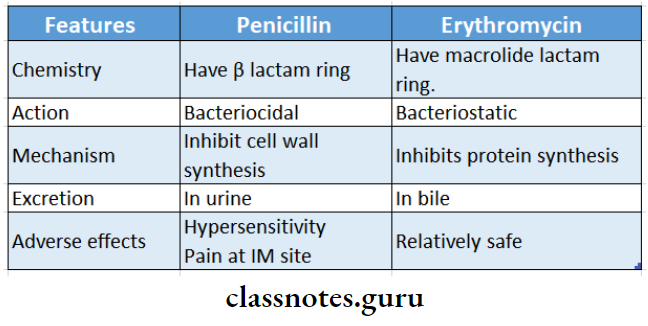
Penicillin:
Penicillin is a beta-lactam antibiotic.
Penicillin Classification:
1. Natural penicillin – penicillin G.
2. Semi-synthetic penicillin
- Acid resistant – penicillin V.
- Penicillinase-resistant penicillin.
- Methicillin, cloxacillin.
- Extended-spectrum penicillin.
- Aminopenicillin – Ampicillin, Bacampicillin.
- Carboxypenicillin – Carbenicillin, Ticarcillin.
- Ureidopenicillin – peperacillin, mezlocillin.
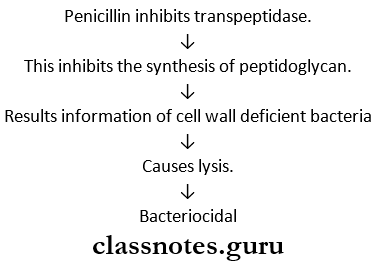
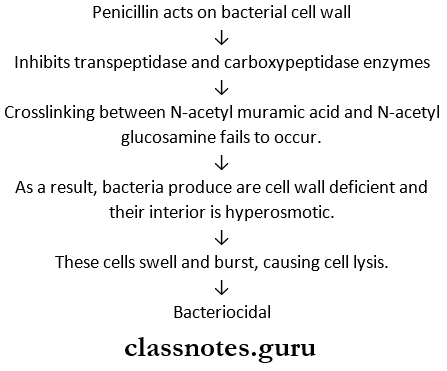
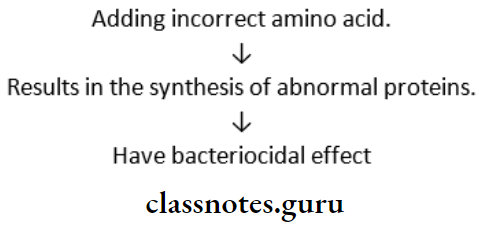
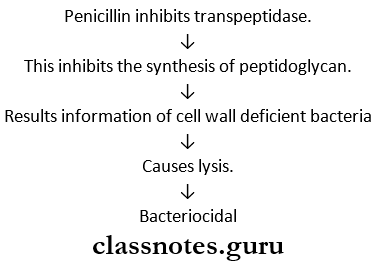
Penicillin Mechanism of action:
- Bacterial cell walls consist of peptidoglycan chains.
- These require transpeptidase enzymes.
Penicillin Toxicity:
- Pain and sterile abscess at the site of injection.
- Thrombophlebitis on IV injections.
- Hypersensitivity reactions.
- Frequently rashes, itching, urticaria, and fever occurs.
- Rarely wheezing, angioneurotic edema, serum sickness, and exfoliative dermatitis occur.
- Topical use of penicillin causes contact dermatitis.
- CNS effects – include confusion, muscle twitchings, convulsions, and coma.
- Suprainfections – occur rarely due to the narrow spectrum of activity of penicillin.
- Jarisch – Herxheimer reaction.
- When penicillin is injected into a syphilitic patient; there is sudden destruction of spirochaetes and release of its toxic products known as the Jarisch herxcheimer reaction.
- It is characterized by fever, myalgia, shivering, exacerbation of syphilitic lesions, and vascular collapse.
Penicillin Uses:
1. Therapeutic uses
- CO Orodental infections – caused by aerobic and anaerobic micro-organisms.
- Pneumococcal infections – like pneumonia, meningitis, and osteomyelitis.
- Streptococcal infections – like pharyngitis, sinusitis, pneumonia, meningitis.
- Meningococcal infections.
- Staphylococcal infections.
- Syphilis.
- Diphtheria.
- Anaerobic infections, like pulmonary, periodontal, and brain abscesses.
- Actinomycosis.
- Tetanus, gas gangrene, anthrax, trench mouth, rat-bite fever.
2. Prophylactic uses
- To prevent the recurrence of rheumatic fever.
- Prevent sexually transmitted diseases like gonorrhea and syphilis.
- Surgical prophylaxis.
- To protect against agranulocytosis.
Beta-lactam antibiotics pharmacology
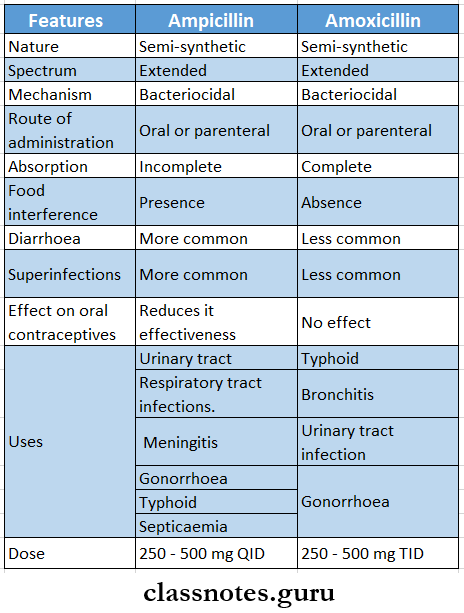
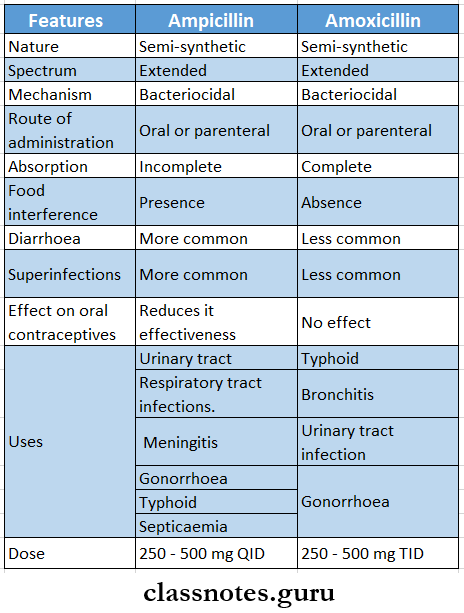
Question 2. Describe the antibacterial spectrum and therapeutic uses of ampicillin.
Answer:
Ampicillin:
It is semisynthetic aminopenicillin.
Antibacterial spectrum:
- Cocci-strep viridians, enterococci, penumococci, gonococci, meningococci.
- Gram negative bacilli – H.influenza, E.coli, proteus, salmonella, shigella.
Ampicillin Uses:
- Urinary tract infections.
- Respiratory tract infections like bronchitis, sinusitis, and otitis media.
- Meningitis.
- Gonorrhoea.
- Bacillary dysentery.
- Typhoid fever.
- Cholecystitis.
- Subacute bacterial endocarditis.
- Septicaemia.
- Orodental infections.
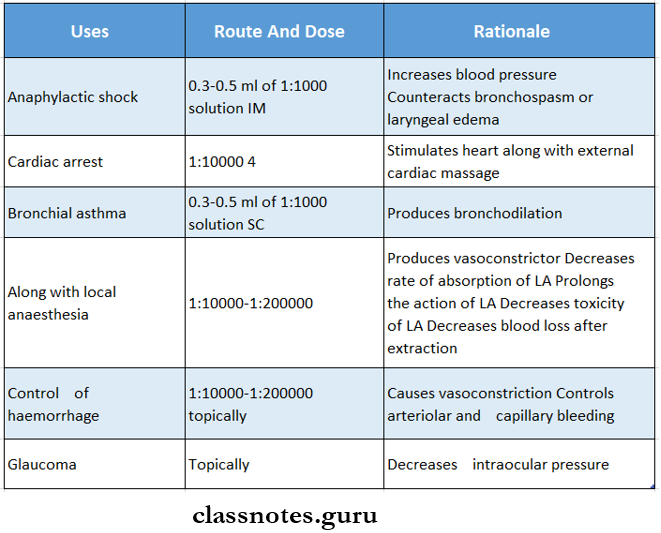
Question 3. Write the treatment of penicillin in anaphylactic shock.
Answer:
Treatment of Anaphylactic Shock:
- Penicillin causes anaphylactic reactions.
- It is more common following parenteral administration than oral.
- So the history of penicillin allergy must be elicited before injection.
- A scratch test or intradermal test with 2-10 units may be performed first
- Treatment of anaphylactic shock is as follows.
- Put the patient in a reclining position.
- Administer oxygen.
- Perform cardiopulmonary resuscitation.
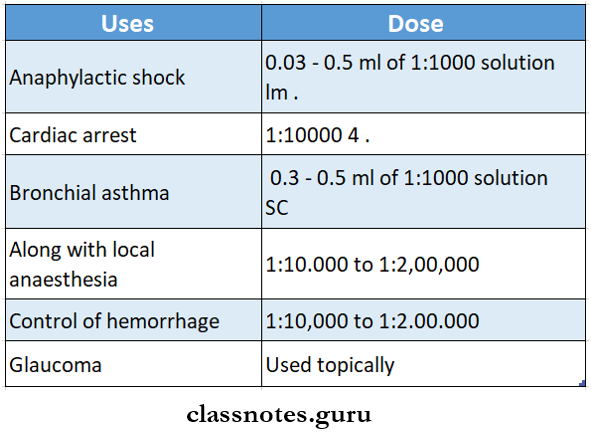
- Inject adrenaline 0.5 mg IM, repeat every 5-10 min or adrenaline diluted 1:10000 or 1:1,00,000 IV.
- Administer chlorpheniramine 10 – 20 mg IM.
- IV hydrocortisone succinate 100 – 200 mg.
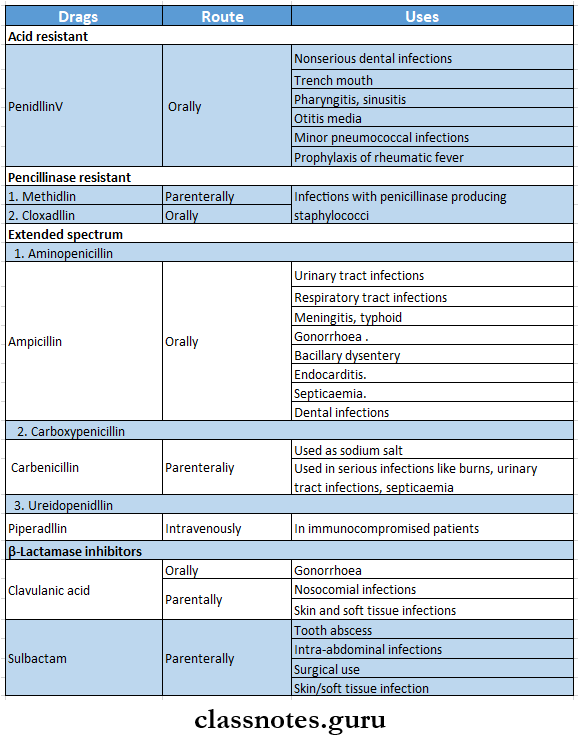
Question 4. Define chemotherapeutic agents. Describe newer penicillins.
Answer:
Chemotherapeutic agents:
A chemical of natural or synthetic origin used for its specific action against disease, usually against infection is called a chemotherapeutic agent.
Newer penicillins:
It includes:
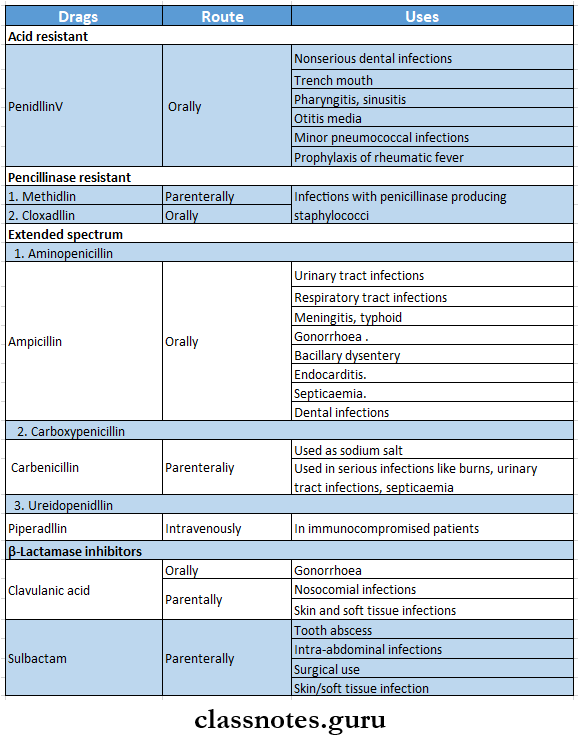
1. Acid-resistant penicillin – phenoxymethyl penicillin – penicillin V.
2. Penicillinase-resistant penicillin – methicillin, cloxacillin.
3. Extended-spectrum penicillins
- Aminopenicillin – Ampicillm, Bicampicillin.
- Carboxypenidllm – carbenicillin, ticarcillin.
- UreidopenidlJin – piperacillin.
4. P-Lactamase inhibitors
Clavulanic acid, sulbactam.
Newer penicillins AIMS:
- To overcome the disadvantages of penicillin G like.
- Poor oral efficacy.
- Susceptibility to penidllanse
- Narrow spectrum
- Hypersensitivity reactions.
- p-lactamase inhibitors.
Question 5. Classify Penicillins. Write the spectrum of action, mechanism of action, therapeutic uses, and adverse effects of Amoxicillin.
Answer:
Penicillin Classification:
- Natural – penicillin G, procaine penicillin, Benzathine penicillin.
- Acid resistance penicillin – penicillin V, phenoxy ethyl penicillin
- Penicillinase resistance penicillin
- Acid labile – methicillin, cloxacillin, nafcillin
- Acid resistant – fucloxacillin
- Broad spectrum penicillin – ampicillin, amoxicillin, talampicillin
- Extended-spectrum penicillin – carbenicillin, ticarcillin
- Beta-lactamase inhibitors – augmentin, sulbactam
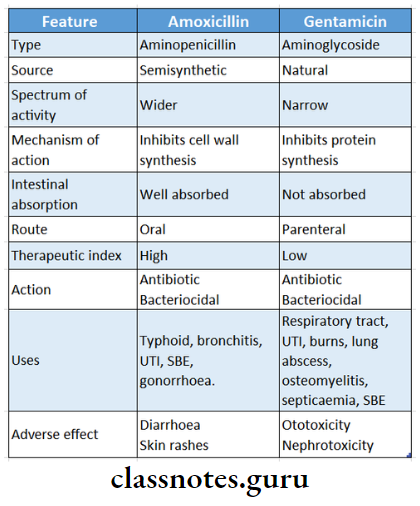
Amoxicillin:
It is aminopenicillin
Amoxicillin Spectrum Of Action:
- Cocci – streptococcus viridians, enterococci, pneumococci, gonococci, meningococci
- Gram negative bacteria – E.coli, proteus, salmonella
Amoxicillin Mechanism Of Action:
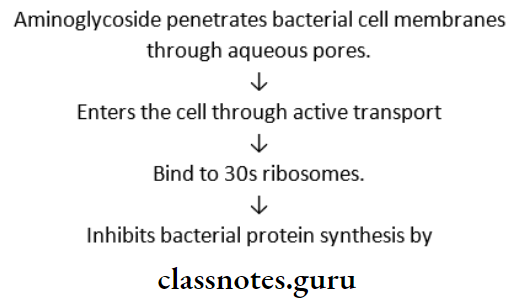
- The bacterial cell wall consists of peptidoglycan chains
- These require transpeptidase enzymes
- Penicillin inhibits transpeptidase → which inhibits the synthesis of peptidoglycan → results in the formation of cell wall deficient bacteria → causes lysis bacteriocidal
Amoxicillin Uses:
- Typhoid
- Respiratory infections
- Urinary tract infection
- Gonorrhoea
- Subacute bacterial endocarditis
- The most commonly used antibiotics for dental use
- Drug of choice for prophylaxis for endocarditis
Amoxicillin Adverse Effects:
- Adverse effects are rare
- Diarrhea – due to irritation of the lower part of the intestine and alteration of bacterial flora
- Skin rashes
Beta-lactam antibiotics classification
Beta Lactum Antibiotics Short Essays
Question 1. Adverse effects of penicillin.
Answer:
1. Penicillin Hypersensitivity reactions
- It is the more common adverse effect of penicillin.
- Frequent manifestations are – rashes, itching, urti- cariaand fever.
- Rarely wheezing, angioneurotic edema, serum sickness, and exfoliative dermatitis occur rarely.
- An anaphylactic reaction may rarely occur but may create a serious problem.
- Adrenaline injection is kept loaded to treat anaphylaxis.
- It is more common with parenteral administration than oral.
- To prevent it, a history of penicillin allergy is elicited.
- A scratch test or intradermal test with 2-10 units is done before the use of penicillin.
2. Penicillin Local effects
- Pain – at the site of injection
- Nausea – on oral ingestion.
- Thrombophlebitis – on IV injection occurs.
3. Penicillin CNS effects
- Large doses cause mental confusion, muscular twitching convulsions, and coma, especially in patients with renal insufficiency IV infections.
4. Penicillin Jarlsch – Herxheimer miction
- It occurs when penicillin is injected into a syphilitic patient
- It is due to the release of endotoxins from dead organisms.
- It is due to the release of endotoxins from dead organisms.
- It is characterized by shivering, fever, myalgia, exacerbation of lesions, and vascular collapse.
- It lasts for 12 – 72 hours.
- Aspirin and corticosteroids provide symptomatic relief.
5. Penicillin Superinfections
It occurs rarely due to a narrow spectrum of activity.
Question 2. Uses of benzylpenicillin (PnG).
Answer:
1. Orodental infections
- Parenteral penicillin is more effective.
- It is given at ordinary doses of 0.5 – 2 MU IM-6 hourly in cases of periodontal abscess, periapical abscess, pericoronitis, ANUG, oral cellulitis, etc.
2. Streptococcal infections
- 0.5 – 5 MU IV 8 hourly for 7-10 days given for pharyngitis, otitis media, scarlet fever, and rheumatic fever.
- High doses of 10 – 20 MU IV daily for 2 – 6 weeks are used in subacute bacterial endocarditis.
3. Pneumococcal infections
If the organism is sensitive, PnG 3-6 MU IV every 6 hours is used.
4. Meningococcal infections
High doses are needed.
5. Gonorrhoea
6. Penicillin
- Early and latent syphilis – 1.2 MU of procaine penicillin daily for 10 days.
- Late syphilis – 2.4 MU of benzathine penicillin weekly for 4 weeks.
7. Diphtheria – 1 – 2 MU procaine penicillin daily for 10 days
8. Tetanus and gas gangrene – 6 – 12 MU dialy.
9. Anthrax – 4 MU 6 hourly for 2 weeks.
10. Actinomycosis – 2 – 4 MU IV 6 hourly for 4 weeks.
Benzylpenicillin Prophylactic use:
- Penicillin G is used «s prophylactic In.
- Rheumatic fever
- Gonorrhoea and syphilis
- Valvular heart disease
- Surgical procedures.
- Agranulocytosis.
Question 3. Extended-spectrum penicillin.
Answer:
- Amlnopenicillin – Amptclllln, Bacamplclllln, Amoxicillin
- Carboxypenicillin – Carbenicillin, Ticarcillin
- Ureidopenicillin -Piperacillin, Mezlocillin.
Extended-spectrum penicillin Uses:
Amlnopenicillin – Urinary tract Infection
- Respiratory tract infection
- Dental infections > Meningitis
- Typhoid
- Septicaemia
- Gonorrhoea
- Bacillary dysentery
- Cholecystitis
- Carboxypenicillin – Used as sodium salt.
- In serious infections like burns, septicemia
- Ureidopenicillin – In gram-negative infections
- caused in immunocompromised patients
Extended-spectrum penicillin Adverse effects:
- Aminopenicillin – Diarrhoea, skin rashes
- Carboxypenicillin – Edema, CLF, bleeding
- Ureidopenicillin – Relatively safe.
Mechanism of action of beta-lactam antibiotics
Question 4. Penicillins act as bacteriocidal agent.
Answer:
Penicillin inhibits the synthesis of bacterial cell walls.
It is more lethal in the phase of rapid multiplication when cell wall synthesis takes place.
Penicillins act as bacteriocidal agent Mechanism:
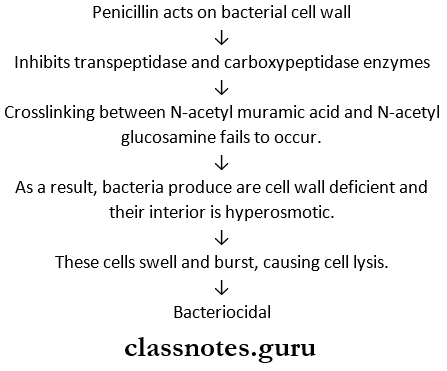
Penicillin also depresses bacterial autolysins which usually function during bacterial cell division.
Question 5. Cloxacillin and staphylococcal infections.
Answer:
Cloxacillin is penicillinase-resistant penicillin.
- It is resistant to hydrolysis by penicillinase produced by bacteria.
- It is also acid resistant
- It is more active against penicillinase-producing staphylococci.
- It is incompletely absorbed from the oral route especially when taken on an empty stomach.
- It is more than 90% plasma bound.
- The plasma half-life is 1 hour.
- It is given in doses of 0.25 – 0.5 g orally 6 hourly.
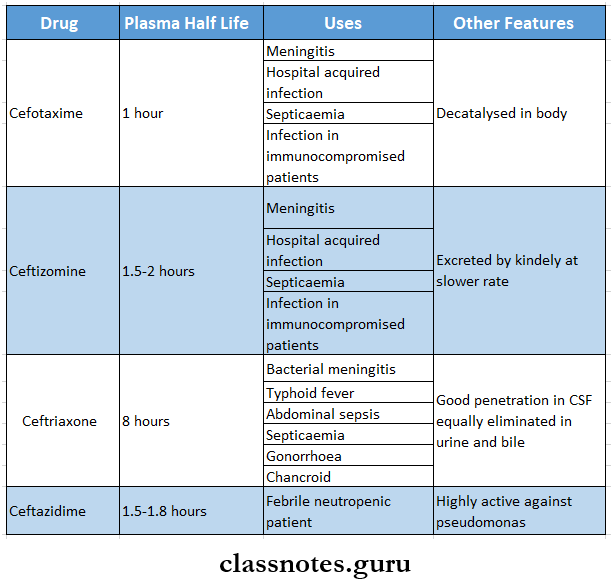
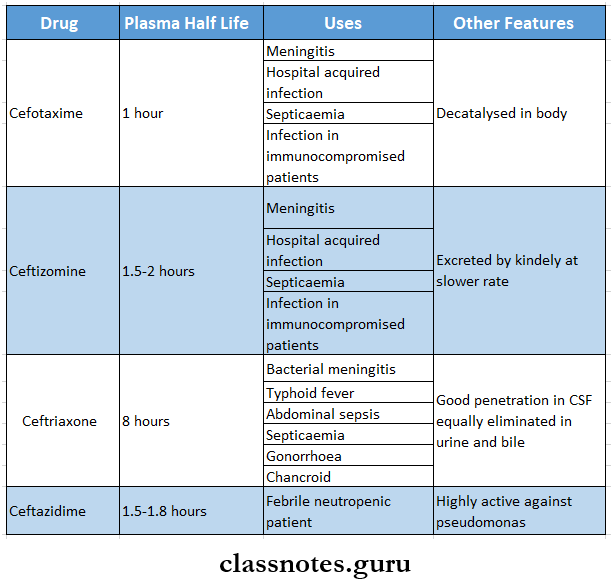
Question 6. Cephalosporins.
Answer:
Cephalosporins are semisynthetic antibiotics with a beta-lactam ring.
They have a wider spectrum of activity.
Cephalosporins Classification:
1. Cephalosporins First generation
- Parenteral – cephalothin, cefazolin.
- Oral – cephalexin, cefadroxil.
- They are very effective against gram-positive organisms and less against gram-negative.
2. Cephalosporins Second generation
- Parenteral – cefamandole, cefuroxime.
- Oral-cefachlor.
- They are more active against gram-negative or, paganism and some are active against anaerobes
3. Cephalosporins Third generation
- Parenteral – cefotaxime, ceftriaxone.
- Oral – cefixime.
- They are highly resistant to beta-lactamase.
- Have good activity against gram-negative organisms.
- They are rarely used in dentistry.
4. Cephalosporins Fourth generation
- Parenteral – cefepime, cefpriome.
- Active against gram-positive and gram-negative organisms.
- More resistant to b-lactamases.
- Used in septicemia, nosocomial, and in infections in immune-compromised patients.
Cephalosporins Adverse reactions
- Pain at the site of injection.
- Hypersensitivity reactions.
- Nephrotoxicity.
- Bleeding diarrhoea
- Neutropenia – low WBC count
- Disulfiram-like reaction with alcohol.
Cephalosporins Uses:
- Dental infections.
- Used as an alternative to penicillin.
- Urinary, respiratory, and soft tissue infections.
- Surgical prophylaxis.
- Gonorrhoea
- Meningitis
- Septicaemia.
- Typhoid.
- Mixed aerobic – anaerobic infections.
- Nosocomial or hospital-acquired infections
- Prophylaxis and treatment of infections in neutropenic patients.
Beta-lactamase inhibitors
Question 7. Semi-synthetic penicillin.
Answer:
Semi-synthetic penicillin Classification:
1. Acid-resistant penicillin – Penicillin V
2. Penicillinase-resistant penicillin – methicillin, clock- oxacillin.
3. Extended-spectrum penicillin.
- Aminopenicillin – ampicillin, amoxicillin.
- Carboxypenicillin – carbenicillin, ticarcillin.
- Ureidopenicillin – peracillin.
4. p-lactamase inhibitors.
- Clavulanic acid, sulbactam.
Semi-synthetic penicillin Advantages over natural penicillin:
- Effective orally.
- Have a wider spectrum of activity
- Resistance to b-lactamases
- Hypersensitivity reactions are less.
Question 8. Compare amoxicillin and ampicillin.
Answer:
Question 9. 3rd generation cephalosporins.
Answer:
- They are highly resistant to beta-lactamase
- Active against Gram-negative and pseudomonas
- Less active against Gram-positive and anaerobes
3rd generation cephalosporins Example
Question 10. Amoxicillin.
Answer:
It is aminopenicillin
Amoxicillin Spectrum of Action:
- Cocci – streptococcus viridians, enterococci, pneumococci, gonococci, meningococci
- Gram negative bacteria – E.coli, proteus, salmonella
Amoxicillin Mechanism of Action:
- The bacterial cell wall consists of peptidoglycan chains
- These require transpeptidase enzymes
- Penicillin inhibits transpeptidase → which inhibits the synthesis of peptidoglycan → results in the formation of cell wall deficient bacteria → causes lysis → bacteriocidal
Amoxicillin Uses:
- Typhoid
- Respiratory infections
- Urinary tract infection
- Gonorrhoea
- Subacute bacterial endocarditis
- The most commonly used antibiotics for dental use
- Drug of choice for prophylaxis for endocarditis
Amoxicillin Adverse Effects:
- Adverse effects are rare
- Diarrhea – due to irritation of the lower part of the intestine and alteration of bacterial flora
- Skin rashes
Side effects of beta-lactam antibiotics
Beta Lactum Antibiotics Short Question And Answers
Question 1. Probenecid and penicillin are used in chemotherapy.
Answer:
Probenecid is combined with penicillin because.
- Probenecid competes with penicillin for active tubular secretion.
- Retards their excretion.
- Increases plasma concentration of penicillin.
- Increases duration of action of penicillin. Thus, this combination is used in.
- Treatment of bacterial endocarditis.
- Gonococcal infections.
Question 2. Uses of benzylpenicillin or Penicillin G.
Answer:
1. Therapeutic uses:
- Orodental infections.
- Pneumococcal infections.
- Streptococcal infections.
- Meningococcal infections
- Staphylococcal infections
- Syphilis
- Diptheria
- Anaerobic infection
- Actinomycosis.
- Tetanus and gas gangrene.
2. Prophylactic uses.
- Rheumatic fever.
- Agranulocytosis
- Sexually transmitted diseases like syphilis and gonorrhea
- Surgical prophylaxis.
Question 3. The rationale for combining amoxicillin and clavulanic acid. Write one indication of this combination.
Answer:
Ciavulanic acid has a beta-lactam ring but no antibacterial activity.
- The combination of amoxicillin and clavulanic acid causes:
- Extension of the antibacterial spectrum.
- Inhibits beta-lactamase-producing organisms.
- After binding to the b-lactamase enzyme, clavulanic add itself gets inactivated, hence it is called a sudden inhibitor.
Amoxicillin and clavulanic acid Indications:
- Skin and soft tissue infections.
- Urinary tract infections.
- Respiratory tract infections.
- Orodental infections.
- Nosocomial infections.
- Gonorrhoea.
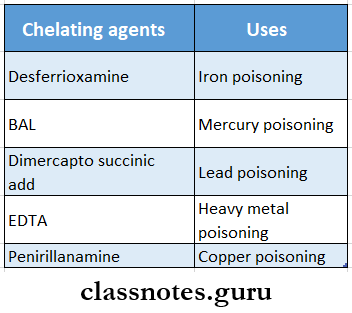
Question 4. D-penicillamine.
Answer:
D-penicillamine is a copper-chelating agent
D-penicillamine Uses:
- As chelating agent
- Use in rheumatoid arthritis.
D-penicillamine Adverse effects:
- Loss of taste.
- Systemic lupus erythematosus.
- Myasthenia gravis.
Question 5. Amoxicillin.
Answer:
Amoxicillin is a semi-synthetic penicillin.
Advantages over ampicillin:
- Good oral absorption.
- Food does not interfere with absorption.
- Diarrhea and skin rashes are less.
Amoxicillin Uses:
- Typhoid
- Respiratory tract infections.
- Urinary tract infections.
- Gonorrhoea.
- Subacute bacterial endocarditis.
Question 6. Adverse effects of penicillin.
Answer:
- Hypersensitivity reaction.
- Pain at the site of injection.
- Superinfection.
- CNS effects – hallucination, coma.
- Jewish Herxheimer reactions.
Question 7. β-lactamase inhibitors.
Answer:
Beta-lactamase inhibitors are the drugs that bind to inactive β-lactamases preventing the destruction of the β-lactam antibiotics.
Beta-lactamase inhibitors:
1. Clavulanic acid
- Competitively and irreversibly inhibits b-lactamases.
- It is a progressive inhibitor.
- It is combined with amoxicillin and ticarcillin.
2. Sulbactam
- It is combined with ampicillin.
- It is given parenterally for mixed aerobic-anaerobic infections.
3. Tazobactum
It is combined with piperacillin for parenteral administration.
Beta-lactam ring function
Question 8. Why penicillin is not combined with sulphonamide?
Answer:
Penicillin is bacteriocidal while sulphonamide is bacteriostatic.
- Sulphonamide retards the multiplication of bacteria.
- Penicillin acts on actively multiplying bacteria.
- Thus combining penicillin and sulphonamide causes antagonism instead of synergism of both drugs.
- Hence, penicillin is not combined with sulphonamides.
Question 9. Amoxicillin.
Answer:
It is aminopenicillin
Cefixime Mechanism of Action:
- The bacterial cell wall consists of peptidoglycan chains
- These require transpeptidase enzymes
- Penicillin inhibits transpeptidase → which inhibits the synthesis of peptidoglycan → results in the formation of cell wall deficient bacteria → causes lysis → bacteriocidal
Cefixime Uses:
- Typhoid
- Respiratory infections
- Urinary tract infection
- Gonorrhoea
- Subacute bacterial endocarditis
- The most commonly used antibiotics for dental use
- Drug of choice for prophylaxis of endocarditis
Cefixime Adverse Effects:
- Adverse effects are rare
- Diarrhea – due to irritation of the lower part of the intestine and alteration of bacterial flora
- Skin rashes
Penicillin group antibiotics
Question 10. Cefixime.
Answer:
- It is a third-generation cephalosporin
- Highly resistant to beta-lactamase
- Have good activity against gram-negative organisms
- Less active against Gram-positive and anaerobes
- Rarely used in dentistry
- Given orally.
- Dose: 200-400 mg BD
- Plasma half-life – 3 hours
Cefixime Uses:
- Respiratory infections
- Biliary infections
- Urinary infections
- Adverse effects
- Stool changes
- Diarrhea