General Anaesthesia Important Notes
1. General Anaesthesia Classification
- Inhalation general anaesthesia
- Liquids – chloroform, diethyl ether, halothane
- Gases – cyclopropane, nitrous oxide
- Intravenous anaesthesia
- Ultra short-acting barbiturates – thiopentone sodium, methohexital
- Non barbiturates – ketamine, benzodiazepines
2. General Anaesthesia Stages
- Stage 1 – stage of analgesia
- Stage 2 – stage of delirium
- Stage 3 – stage of surgical anaesthesia
- Stage 4 – stage of respiratory paralysis
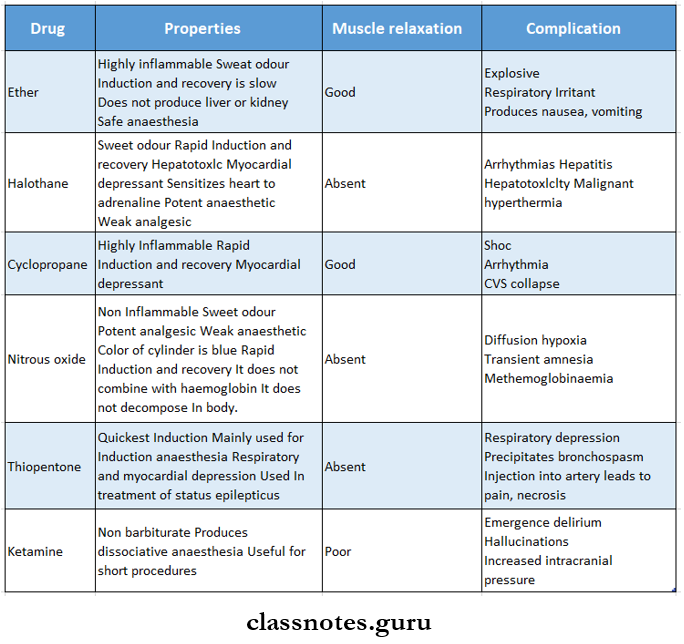
3. General Anaesthesia Drugs used
4. General Anaesthesia Neuroleptoanalgesia
- Consists of a combination of a major tranquiliser and a potent opioid analgesic
- Droperidol + fentanyl
- The patient remains conscious but assumes a trance-like state in which he is immobile apparently free from pain
- The addition of 65% N2O + 35% O2 converts neuroleptanalgesia to neurolept anaesthesia
General Anaesthesia Long Essays
Question 1. Classify general anaesthetics and describe pharmacological actions, merits and demerits of nitrous oxide.
(or)
Describe stages of general anaesthesia. Discuss nitrous oxide.
Answer:
Stages of Anaesthesia:
• Guedel describes four stages of ether anaesthesia.
Read And Learn More: Pharmacology Question and Answers
1. General anaesthesia Stage of analgesia.
- It is a stage from the beginning of anaesthetic inhalation to loss of consciousness.
- Some minor procedures can be performed during it
2. General anaesthesia Stage of delirium.
- It is the stage from loss of consciousness to the beginning of regular respiration.
- It is associated with excitement, struggling, shouting, crying, and sympathetic stimulation.
- No procedure can be carried out during this stage.
3. General anaesthesia Surgical anaesthesia.
- it is the stage from the onset of regular respiration to a cessation of spontaneous breathing.
- This has IV planes.
- There is a gradual loss of reflexes and relaxation of skeletal muscles.
- Most dental/surgical procedures are carried out in planes 1 or 2.
4. General anaesthesia Medullary paralysis.
- it is the stage from the cessation of breathing to failure of circulation and death.
- it is seen only with overdose
- it is never attempted.
General anaesthesia Classification:
General anaesthetics are classified into.
1. General anaesthesia Inhalation:
- Gas- Nitrous oxide, cyclopropane.
- Liquids.
- Ether, halothane, isoflurane, desflurane.
2. General anaesthesia Intravenous.
- Inducing agents.
- Thiopentone sodium
- Methohexitone sodium
- Propofol
- Slower-acting drugs.
- Benzodiazepines.
- Diazepam, lorazepam, midazolam.
- Dissociative anaesthesia.
- Ketamine
- Opioid analgesia – Fentanyl.
- Benzodiazepines.
Nitrous oxide:
- Nitrous oxide is a colourless, odourless, heavier-than-air, noninflammable gas.
Nitrous oxide Actions:
- A moderate increase in pain threshold.
- Slight amnesia effect.
- Euphoria is frequent.
- Decreased sense of smell.
- improved hearing.
- Slight myocardial depression.
- Minimal effect on respiration.
- Reduces minimal alveolar concentration.
Nitrous oxide Advantages:
- Non-inflammable, non-irritating.
- Rapid and smooth induction.
- Strong analgesic.
- Rapid recovery.
- No postoperative nausea.
- Has little effect on respiration and cardiovascular function.
- it is non-toxic to the liver, kidneys and brain.
Nitrous oxide Disadvantages:
- Less potent
- Poor muscle relaxant
- Enters the air-filled cavities faster.
- Repeated use causes bone marrow depression.
- Long-term exposure to low doses impairs DNA synthesis.
General Anaesthesia Short Essays
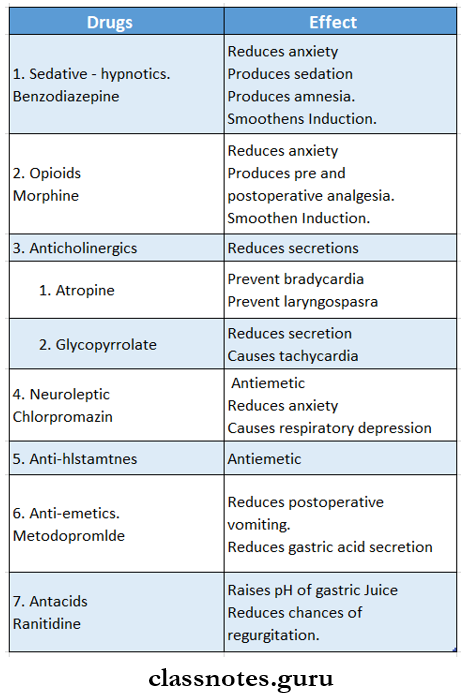
Question 1. Pre-anaesthetic medication.
Answer:
Pre-anaesthetic medication is the use of drugs before anaesthesia to make it more pleasant and safe.
Pre-anaesthetic medication AIMS:
- Relief of anxiety and apprehension preoperatively.
- Facilitate smooth muscle induction.
- Produce amnesia.
- Reduces secretion.
- Decreases vagal stimulation,
- Reduces postoperat4e nausea and vomiting.
- Decreases acidity and volume of gastric juice.
- Enhances hypnotic effects of drugs.
Pre-anaesthetic medication Drugs used for it:
- Sedative – hypnotic.
- Opioids.
- Anticholinergic.
- Neuroleptic.
- Antihistamine.
- Antiemetics.
- Antacids.
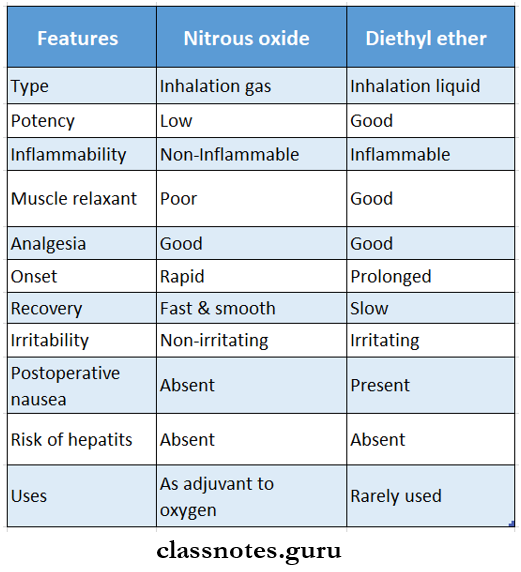
Question 2. Compart nitrous oxide and diethyl ether.
Answer:
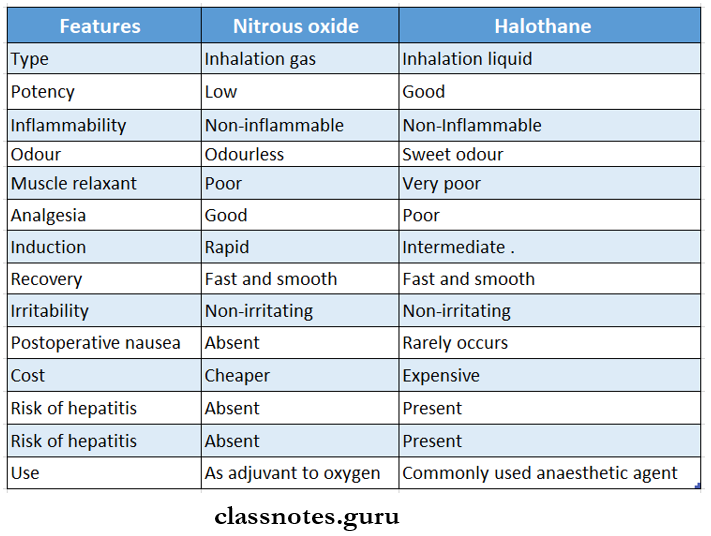
Question 3. Compare nitrous oxide and halothane.
Answer:
Question 4. Ether.
Answer:
Ether is a highly volatile, colourless, inflammable liquid.
- Vapours produced by it are irritating.
Ether Actions:
- Stimulates the sympathetic system.
- increases heart rate
- Depresses vagus nerve;
- Decreases BP.
- Stimulates salvation.
- it is irritating to the respiratory tract.
- increases CSF pressure and blood glucose level.
- Potent analgesic, anaesthetic.
- Marked muscle relaxant.
Ether Advantages:
- Potent and reliable anaesthetic.
- Good analgesia.
- Provide full muscle relaxation.
- Bronchodilator.
- Easy to administer.
- Cheaper.
- No significant effect on cardiovascular and respiratory function.
- Does not sensitize the heart to adrenaline.
Ether Disadvantages:
- inflammable.
- Highly soluble in blood.
- Slow and unpleasant induction.
- Produce irritating vapours.
- Slow recovery.
- Postoperative nausea and vomiting are frequent.
- Enhances salivation and respiratory secretion.
- Due to this atropine is given for pre-medication.
Ether Status in Anaesthesia:
- Due to the above disadvantages, ether is not preferred.
- But due to easy administration and low cost, it is used in peripheral areas.
Question 5. Benzodiazepine.
Answer:
Benzodiazepines are one of the drugs used for premedication.
- it includes drugs like diazepam, midazolam. Oxazepam, lorazepam.
Benzodiazepine Actions:
- Mild decrease in BP.
- Minimal changes in respiration.
- Antiemetic.
- Produces amnesia.
- Relieves anxiety.
- Produces emotional responses in adolescent, females.
Benzodiazepine Uses:
- Induce, maintain and supplement anaesthesia.
- For conscious sedation.
- Slow-acting general anaesthetic.
- Used for endoscopy, cardiac catheterization, angiographic, mandibular fractures, etc.
Benzodiazepine Advantages:
- No significant respiratory depression.
- No postoperative nausea and vomiting.
- Absence of stimulation of involuntary movements.
- Also used as.
- Sedatives hypnotics.
- Antianxiety drugs.
- Centrally acting skeletal muscle relaxant
- Combined with analgesic and used for rheumatoid disorders.
- Antiepileptic.
Question 6. Halothane.
Answer:
Halothane is a colourless, volatile liquid.
Halothane Advantages:
- Sweet odour.
- Non-irritant and non-inflammable.
- intermediate solubility in blood.
- Potent anaesthetic.
- Quick and pleasant induction.
- Rapid recovery
- Less chances of postoperative nausea and vomiting.
Halothane Disadvantages:
- Poor analgesic.
- Poor muscle relaxation.
- Causes direct depression of myocardial contractility.
- Reduce cardiac output, BP, and heart rate.
- Causes respiratory depression.
- Causes malignant hyperthermia.
- Severe hepatitis.
- Reduces renal blood flow and GFR.
- Expensive.
- Status in Anaesthesia:
- Halothane is a routinely used anaesthetic.
- Analgesic and muscle relaxant are used as adjuvant.
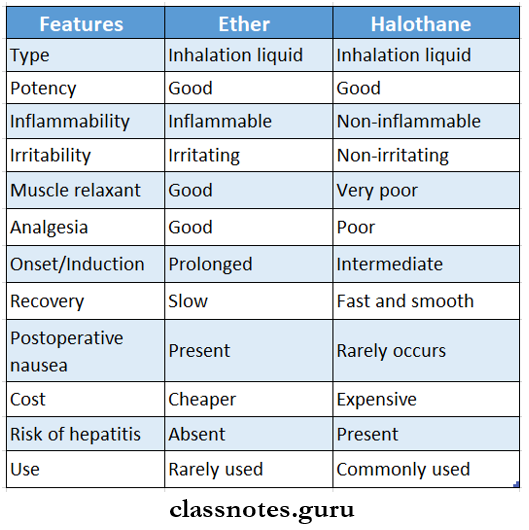
Question 7. Compare ether and halothane.
Answer:
Question 8. Diazepam.
Answer:
Diazepam belongs to benzodiazepine.
Diazepam Dose:
- 0.2 – 0.5 mg/kg.
General Anaesthesia Short Answers
Question 1. Actions of nitrous oxide.
Answer:
Nitrous oxide is a colourless, odourless, non-inflammable gas.
Nitrous oxide Actions:
- A moderate increase in pain threshold.
- Slight amnesia effect
- Euphoria is frequent
- Decreased sense of Smell.
- improved hearing.
- Slight myocardial depression.
- Minimal effect on respiration.
Question 2. Diazepam. its uses.
Answer:
- To induce conscious sedation in small repeated doses or by slow infusion.
- Sedative hypnotic.
- Anxiety.
- Centrally acting skeletal muscle relaxant
- Combined with analgesic for the treatment of rheumatic disorders.
- Antiepileptic drugs.
Question 3. Ketamine.
Answer:
Ketamine induces dissociative anaesthesia characterized by profound analgesia, immobility, amnesia, light sleep and a feeling of dissociation from one’s own body and surrounding.
Ketamine Site of action:
- Cortex and subcortical areas.
Ketamine Dose:
- 1-2 mg/kg slow IV or
- 10 mg/kg IM
- The onset of action -1 – 3 min.
- Recovery – After 10-15 min.
Ketamine Indications:
- Surgery of head and neck.
- Children.
- Asthmatic patients.
- For short operations.
- in patients who do not want to lose consciousness.
Ketamine Contra-indications:
- Hypertensives.
- ischaemic heart disease.
- Pregnancy.
- increased intracranial tension.
- Psychiatric disorders.
Question 4. Methohexitone.
Answer:
Methohexitone is a more potent and shorter-acting thiopentone congener.
- It is more rapidly metabolized.
- It has quick and brief actions.
- Induction – in 15 – 30 sec.
- Recovery – within 2 – 3 min.
Methohexitone Actions:
- Less hypotensive
- Slight increase in heart rate
- Moderate hypoventilation.
Methohexitone Contra/Indication:
- Epileptic patients.
Question 5. Thiopentone sodium.
Answer:
Thiopentone sodium is ultra short-acting thiobarbiturate.
Thiopentone sodium The onset of action:
- 15-20 sec when given intravenously.
Thiopentone sodium Duration of action:
- 4 – 7 min.
Thiopentone sodium Properties:
- Highly soluble in water.
- Prepared freshly before injection.
- Highly lipid soluble.
- Poor analgesic.
- Weak muscle relaxant
- Extravasation of solution causes intense pain, necrosis and gangrene.
Thiopentone sodium Adverse effects:
- Laryngospasm.
- Shivering and delirium.
Question 6. Propofol.
Answer:
it is an oily liquid employed as a 1% emulsion
Propofol Pharmacokinetics:
- Unconsciousness occurs in 15-45 sec and lasts approximately 10 minutes
- Distributes rapidly
- Plasma half-life – 2-4 min
Propofol Advantages:
- Faster onset
- Quick recovery
- Antiemetic
- Safer in pregnancy
Propofol Uses:
- IV induction
- Shorter duration procedures like endoscopies, bums dressings
Propofol Adverse Effects:
- Pain at the injection site
- Fall in BP
- CVS and respiratory depression
