B Pharmacy Important Questions Sedative And Hypnotics Important Notes
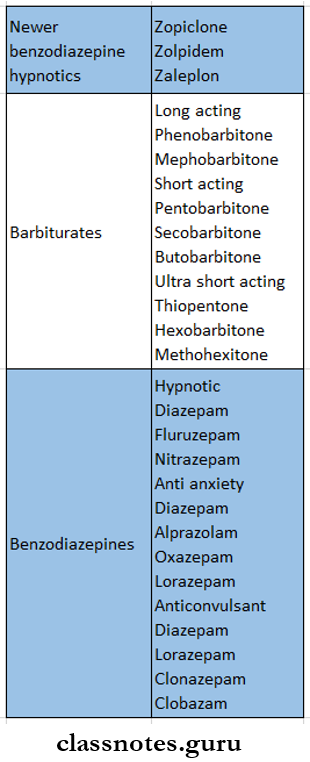
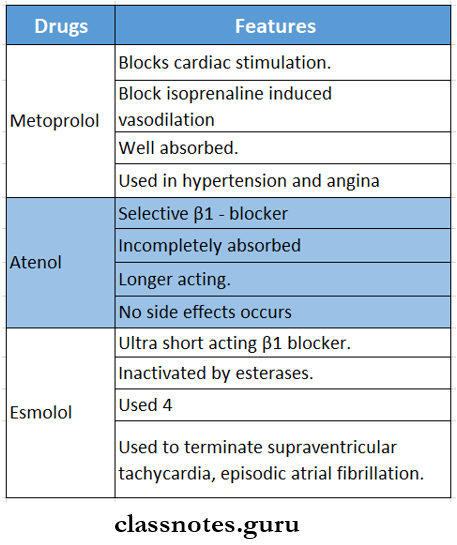
1. Sedative And Hypnotics Classification of barbiturates
- Long-acting
- Phenobarbitone
- Mephobarbitone
- Short-acting
- Pentobarbitone
- Secobarbitone
- Butobarbitone
- Ultra short-acting
- Thiopentone
- Hexobarbitone
- Methohexitone
Sedatives and hypnotics questions and answers
Read And Learn More: Pharmacology Question and Answers
2. Classification of sedatives and hypnotics Newer benzodiazepine hypnotics
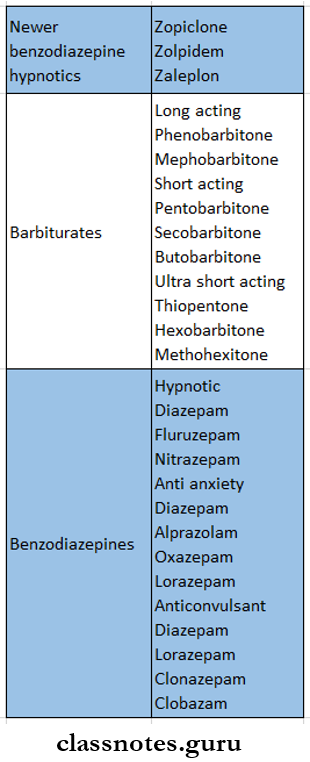
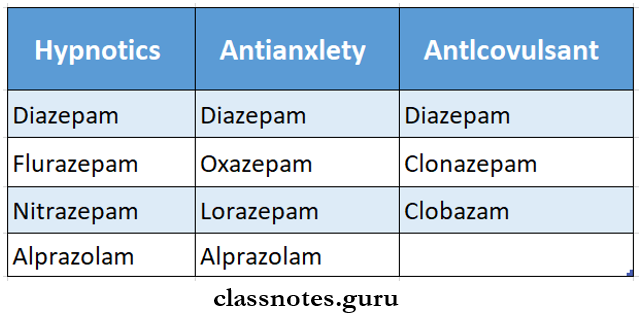
3. Sedative And Hypnotics Benzodiazepines
- They have a high therapeutic index
- Causes less distortion of sleep
- Do not alter the disposition of other drugs
- Lowers abuse liability
- Withdrawal symptoms are less marked
- Do not affect respiration or cardiovascular functions
4. Sedative And Hypnotics Thiopentone sodium
- It is ultra short-acting
- When injected 4 as 2.5% solution, it produces unconsciousness in 15-20 sec
- Its undissociated form has high lipid solubility and enters the brain almost instantly
B Pharmacy Important Questions Sedative And Hypnotics Long Essays
Question 1. Classify hypnotics. Mention the mechanism, actions, and management of barbiturates.
Answer:
Hypnotics Classification:
1. Hypnotics Barbiturates.
- Long-acting – Phenobarbitone
- Short-acting – Pentobarbitone.
- Ultrashort acting – Thiopentone sodium.
2. Hypnotics Benzodiazepine.
3. Hypnotics Newer hypnotics.
- Zopiclone, Zolpidem, Zaleplon.
Newer hypnotics Barbiturates:
- Barbiturates are drugs derived from barbituric acid. They are non-selective CNS depressants
Barbiturates Mechanism of Action:
Barbiturate
↓
Bind of GABAa receptor Cl- Channel complex.
↓
Potentiate GABAergic inhibition.
↓
Duration of Cl- channel kept open increases
↓
Increased chloride conductance.
↓
Membrane hyperpolarization.
↓
CNS depression.
Barbiturates Actions:
1. Barbiturates CNS.
- In hypnotic doses, barbiturates induce sleep and prolong the duration of sleep.
- Sedative doses given during the daytime can produce drowsiness, reduction in anxiety, and excitability.
- Barbiturates have anticonvulsant property.
- At higher doses, it produces general anesthesia.
2. Barbiturates Respiration.
3. Barbiturates CVS.
- Produces a slight decrease in BP and heart rate.
Sedatives and hypnotics pharmacology Questions & Answers
4. Barbiturates Skeletal muscles.
- Depress the excitability of the neuromuscular junction.
5. Barbiturates Kidney.
- The tone and motility of the bowel are decreased.
- Reduces urine flow
Barbiturate poisoning:
- The dosage of barbiturates above 6 -10 g causes acute barbiturate poisoning.
Barbiturate poisoning Management:
- Maintain airway, BP, adequate ventilation, and oxygen administration.
- Maintain blood volume by fluid infusion.
- Use of vasopressor.
- Gastric lavage.
- Hemodialysis is done in severe cases.
- Forced alkaline diuresis with mannitol, frusemide, or sodium bicarbonate is done.
Question 2. Describe the Barbiturate’s uses and adverse effects.
Answer:
Barbiturates:
Barbiturates Uses:
- As pre-anesthetic medication.
- As sedative and hypnotic.
- Thiopentone is used for induction of general anesthesia.
- Phenobarbitone is used in epilepsy.
- Used in the treatment of congenital non-hemolytic jaundice.
- Occasionally employed as an adjuvant in psychosomatic disorders.
Barbiturates Adverse Effects:
1. CNS effects.
- Hangover, mental confusion, impaired performed traffic accidents, distortions of mood.
2. Respiratory.
- Respiratory depression occurs.
3. Hypersensitivity.
- Skin rashes and swelling of the eyelids and lips occur.
4. Tolerance and dependence develop.
5. Withdrawal symptoms.
- Anxiety, restlessness, abdominal cramps, hallucinations, delirium, and convulsions occur.
6. Idiosyncrasy.
7. Megaloblastic anemia – due to prolong used of phenobarbitone.
Sedative hypnotic drugs MCQs with answers
Question 3. Classify barbiturates. Discuss thiopentone sodium.
Answer:
Barbiturates Classification:
1. Long-acting:
- Phenobarbitone, mephobarbitone.
2. Short-acting.
- Pentobarbitone, butobarbitone.
3. Ultra-short acting.
- Thiopentone, Hexobarbltone, Methohexltone.
Thiopentone sodium:
- Thiopentone sodium is ultra short-acting thiobarblturate
Thiopentone sodium Onset of Action:
Thiopentone sodium Duration of Action:
Thiopentone sodium Properties:
- Highly soluble in water.
- Produces unconsciousness in 15 – 20 s.
- Produces CNS depression.
- Poor analgesic.
- Weak muscle relaxant.
- Causes respiratory depression.
- Highly lipid soluble.
- Prepared freshly before use.
- Extravasation of solution causes Intense pain, necrosis, and gangrene.
Thiopentone sodium Uses:
- Common inducing agent
- Used for short non-painful operations.
- Used to control convulsions.
- Adverse effects:
- Laryngospasm.
- Shivering.
- Deliriums
Thiopentone sodium Dose:
- Injected IV dosage – 3 – 5 mg/kg as 2 – 5% solution.
Question 4. Discuss the mechanism, actions, uses, and adverse effects of benzodiazepines.
Answer:
Benzodiazepines:
- Benzodiazepines are a group of drugs used for sedatives and hypnotics.
Benzodiazepines Mechanism of Action:
Benzodiazepines bind to the specific site on GABAa – BZD
receptors Cl- Channel complex.
↓
This potentiates the inhibitory effect of GABA.
↓
Leads to an increase in the frequency of opening of Cl Channels.
↓
Increased Cl- conductance.
↓
Membrane hyperpolarization.
↓
CNS depression.
Benzodiazepines Actions:
1. CNS actions.
- Hypnosis – increases the duration of sleep.
- Anxiolytic – reduces anxiety.
- Causes CNS depression.
- Anticonvulsant – increases the seizure threshold.
- Amnesia – produces loss of memory for the events happening after drug administration.
2. Skeletal muscle.
3. CVS action.
- At high doses, it decreases BP and heart rate.
4. GIT.
- Decreases gastric acid secretion.
5. Respiration.
- At high doses, causes respiratory depression.
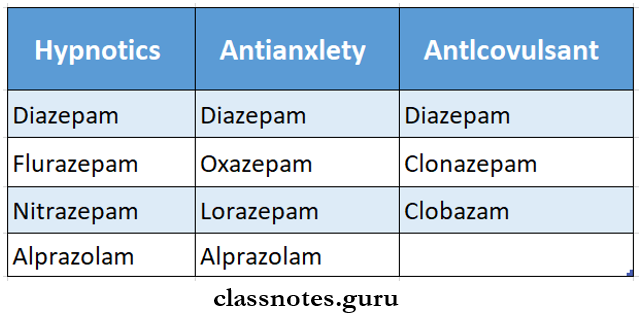
Benzodiazepines Uses:
- As hypnotic – to treat insomnia.
- As anxiolytic – to reduce anxiety.
- As anticonvulsant – 4 diazepam is used.
- As a centrally-acting muscle relaxant
- As pre-anesthetic medication.
- IV midazolam or diazepam is used as an intravenous anesthetic.
- For minor procedures.
- For initial control of mania.
- During alcohol withdrawal.
- Along with analgesics, NSAIDs, spasmolytics, antiulcer, and many other drugs.
Benzodiazepines Adverse effects:
- Benzodiazepines are well-tolerated drugs.
- Common side effects are.
- Drowsiness, dizziness, vertigo, ataxia, amnesia.
- The blurring of vision.
- Dry mouth, sweating.
- Headache, daytime sedation.
- Tolerance and dependence.
- Drug given during labor causes hypotonia and respiratory depression in new-born.
Question 5. Define sedative hypnotics classify. What are the advantages of benzodiazepines over barbiturates as sedative-hypnotics?
Answer:
Definition:
Sedative:
A sedative is a drug that reduces excitement and calms the subject without inducing sleep.
Hypnotics:
Hypnotic is a drug that induces and/or maintains sleep similar to normal sleep.
Advantages of Benzodiazepine over barbiturates:
- Benzodiazepine has a high therapeutic index.
- It induces sleep similar to natural sleep.
- Hypnotic doses do not affect respiration or cardiovascular functions.
- BZDs have practically no action on another body system.
- Causes less distortion of sleep architecture.
- Do not cause microsomal enzyme induction.
- Do not alter the blood level of other drugs.
- Have low abuse liability.
- Tolerance is mild.
- Psychological and physical dependence is less marked.
- Specific BZD antagonist flumazenil is present to use in the cause of poisoning.
- The rebound phenomenon is less marked.
Classification of sedatives and hypnotics Questions & Answers
Sedative And Hypnotics Short Essays
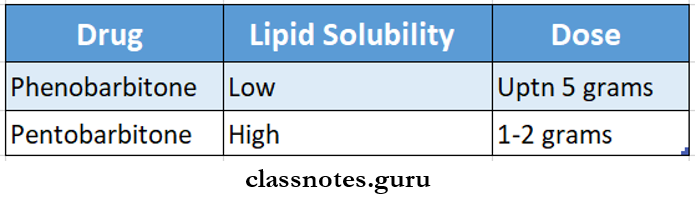
Question 1. Classify barbiturates. Write it dose.
Answer:
Barbiturates:
- Barbiturates are non-selective CNS depressants.
Barbiturates Classification:
1. Long-acting.
- Phenobarbitone, mephobarbitone.
2. Short acting.
- Pentobarbitone, secobarbitone, Butobarbitone.
3. Ultra-short acting.
- Thiopentone, methohexitone, and hexobarbitone.
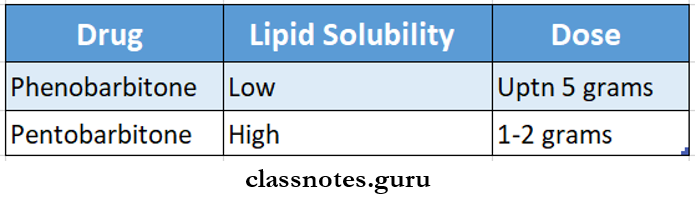
Barbiturates Dose:
- The dose depends on lipid solubility.
- Higher lipid solubility indicates a lower dose.
Barbituratesv Examples:
Question 2. Uses of benzodiazepines (BZDs).
Answer:
Benzodiazepines Uses:
1. As hypnotics
- BZDs are used to treat insomnia.
- They shorten sleep latency and reduce nocturnal awakening.
- In dentistry, it is used to ensure sleep the night before the dental procedure in an apprehensive patient.
2. As anxiolytics and for daytime sedation.
- Reduces anxiety.
- Produces calming effects.
3. As an anticonvulsant
- Increases seizure threshold.
- Used especially in emergency control of status epileptic- cities, febrile convulsions, tetanus, etc
4. Muscle relaxant
- BZDs reduce muscle tone by centrally acting.
- Reduces muscle tone and aches associated with anxiety.
5. As IV anesthesia.
- BZDs induce, maintain and supplement anesthetic
6. As pre-anesthetic medication.
- Used due to its sedative and anxiolytic effects.
7. During alcohol withdrawal
- Reduces the intensity of withdrawal symptoms.
- an In minor procedures like endoscopies, fracture reduction, and cardiac catheterization.
9. In psychiatry.
- For initial control of mania.
Hypnotic drugs short notes with answers
Question 3. Barbiturate poisoning.
Answer:
Barbiturate poisoning:
- The dosage of barbiturates above 6 – 10 g causes acute barbiturate poisoning.
Barbiturate poisoning Manifestations:
- Excessive CNS depression.
- Respiration depression with slow and shallow breathing.
- Hypotension.
- Bullous eruptions.
- Cardiovascular collapse.
- Renal shutdown.
- Pulmonary complications.
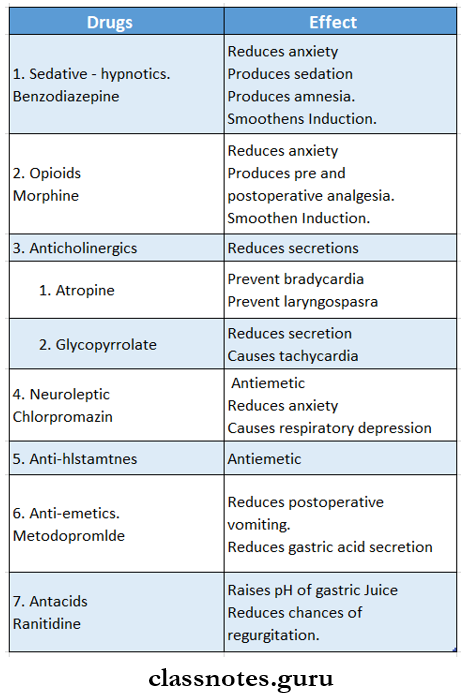
Question 4. Benzodiazepine as pre-anesthetic medication.
Answer:
Benzodiazepine is used for pre-anesthetic medication because it
- Reduces anxiety.
- Produces sedation.
- Produces amnesia.
- Relieves post-operative pain.
- Make anesthesia safer.
- Sraoothens induction with little respiratory depression.
- Reduces side effects of anesthesia like gastric acidity.
- Diazepam 5 -10 mg is given orally.
Sedative And Hypnotics Short Answers
Question 1. Flumazenil.
Answer:
Flumazenil is benzodiazepine antagonist
- It rarely is a benzodiazepine antagonist
- It rarely induces seizures.
- Its action starts seconds after IV administration and lasts for 1 – 2 hours.
Flumazenil Mechanism:
- It competes with BZD agonists and reverses depressant effects.
- Competes with inverse agonists for BZD receptor and reverses stimulant effects.
- It abolishes the hypnogenic, psychomotor, cognitive, and EEC effects of BZD.
Flumazenil Uses:
- To reverse actions of BZD.
- In benzodiazepine overdosage or poisoning.
Question 2. Define sedatives, hypnotics, and tranquilizers.
Answer:
Sedative:
A sedative is a drug that reduces excitement and calms the subject without inducing sleep.
Hypnotics:
Hypnotic is a drug that induces and/or maintains sleep similar to normal sleep.
Tranquilizer:
- It is an old term.
- It means a drug that reduces mental tension and produces calmness without inducing sleep or depressing mental faculties.
Mechanism of action of sedatives and hypnotics
Question 3. Urine should be alkalized in acute barbiturate poisoning? Why?
Answer:
The dosage of barbiturates above 6 -10 g causes acute barbiturate poisoning.
- There is no specific antidote for it, only an alkaline diet- sis is the main treatment for it.
- It is done with mannitol, sodium bicarbonate, and frusemide.
- Barbiturates are weakly acidic drugs.
- But in alkaline urine, they exist in ionized form.
- Thus, they are not reabsorbed while passing through renal tubules.
- As a result, they are rapidly excreted in the urine.
Sedatives and hypnotics important exam questions
Question 4. Midazolam
Answer:
- It is an ultra-short-acting benzodiazepine
- Duration of action is < 6 hours
- Dose: 7.5-10 mg
- It is used as IV anesthesia because
- It is faster
- Short-acting
- More potent
- Does not cause respiratory and CVS depression
- Does not cause pain or irritation at the injection site
- Used as an adjuvant to general anesthesia