Immunological Factors In Disease Important Notes
- Hypersensitivity Reactions
- Anaphylactic Reaction
- Anaphylactic Reaction is a state of rapidly developing immune response to an antigen mediated by IgE antibodies
- Anaphylactic Reaction Clinical features:
- Systemic anaphylaxis
- Pruritus
- Wheel and flare lesions
- Bronchospasm
- Tightness of chest
- Wheezing
- Laryngeal edema
- Dyspnea
- Cyanosis
- Shock
- Diarrhea
- Pulmonary edema
- If not treated death occurs Local anaphylaxis
- Hay fever
- Bronchial asthma
- Food allergies
- Contact dermatitis
- Angioedema
Immunological factors in disease questions and answers
Read And Learn More: General Medicine Question and Answers
Immunological Factors In Disease Long Essays
Question 1. Classify allergic reactions. Describe clinical features and management of generalized anaphylaxis.
Answer:
Allergic Reactions
- Hyperscusillvity/allergy In defined as an exaggerated/inappropriate state of normal Immune response with the onset of adverse effects on the body.
- Lesions of hypersensitivity are a form of antigen-antibody reaction
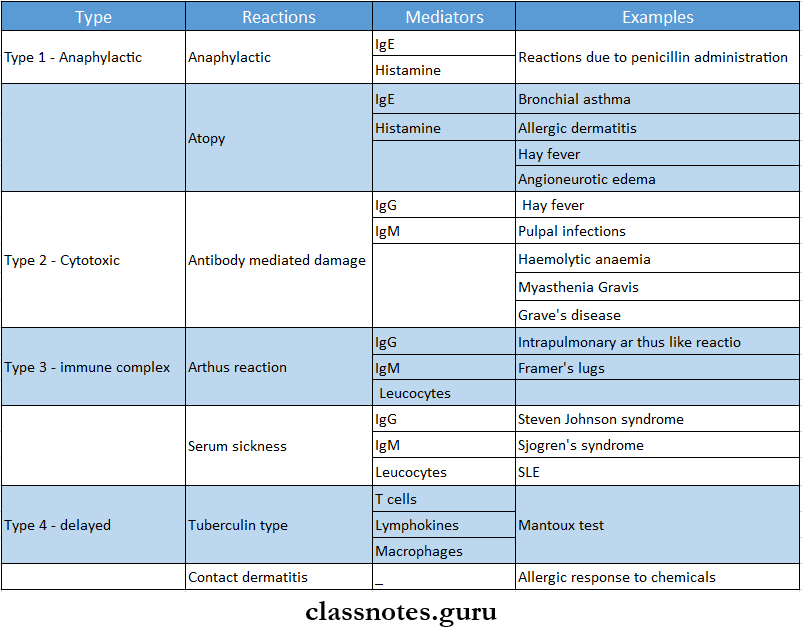
- Hypersensllivlly reactions are classified into 4 types,
- Type 1: Anaphylactic (atopic) reaction
- Type 2: Cyloxlc (cytolytic) reaction
- Type 3: Immune complex-mediated (arthus) reaction,
- Type 4: Delayed hypersensitivity (cell-mediated) reaction.
- Depending, upon the rapidity, duration, and type of immune response, they are classified into immediate type and delayed type.
- Immediate type: On administration of antigen, reaction occurs immediately, This includes types 1, 2, and 3.
- Delayed type: Reaction is slower in onset, develops within 24-48 hours and the effects is prolonged. Includes type 4 reaction.
Anaphylaxis:
- Anaphylaxis or type 1 hypersensitivity is defined as a state of rapidly developing immune responses to an antigen (i.e., allergen) to which the individual is previously sensitized.
- The reaction appears within 15 – 30 min of exposure to antigen.
Etiology:
- Type 1 reaction is mediated by humeral antibodies of IgE type or regain antibodies in response to antigen.
- The definite cause is not known, but the following may be responsible.
- Environmental pollutants
- Genetic basis
- Concomitant factors Allergic response may be linked to the occurrence of certain viral infections of upper respiratory tract.
Anaphylaxis Effects:
- Increased vascular permeability
- Smooth muscle contraction
- Vaaocontriction followed by vasodilation
- Shock
- Increased gastric secretion
- Increased nasal and lacrimal secretions
- Eosinophils and neutrophilia.
Anaphylaxis Examples:
- Reactions against mycobacterial infection.
- Tuberculin reaction, the granulomatous reaction in tuberculosis, leprosy.
- Reaction against virally infected cells
- Reaction against malignant cells in the body.
- Reaction against organ transplantation, for example, transplant rejection, graft versus host reaction.
Short essay on immunological factors in disease
Immunological Factors In Disease Short Essays
Question 1. Anaphylaxis
Answer:
Anaphylaxis
- Anaphylaxis or type 1 hypersensitivity is defined as a stale of rapidly developing immune response to an antigen (i.e., allergen) to which the individual is previously sensitised.
- The reaction appears within 15 – 30 min of exposure to antigen.
Etiology:
- Type 1 reaction is mediated by humoral antibodies of IgE type or regain antibodies in response to antigen.
- The definite cause is not known, but the following may be responsible.
- Environmental pollutants
- Genetic basis
- Concomitant factors – Allergic response may be linked to occurrence of certain viral infections of upper respiratory tract.
Anaphylaxis Effects:
- Increased vascular permeability
- Smooth muscle contraction
- Vasoconstriction followed by vasodilation
- Shock
- Increased gastric secretion
- Increased nasal and lacrimal secretions
- Eosinophia and neutrophilia.
Anaphylaxis Examples:
- Reactions against mycobacterial infection.
- Examples: Tuberculin reaction, granulomatous reaction in tuberculosis, leprosy.
- Reaction against virally infected cells
- Reaction against malignant cells in the body.
- Reaction against organ transplantation for example, transplant rejection, graft versus host reaction.
Question 2. Oedema- causes
Answer: Oedema
Oedema Causes:
- Congestive heart failure
- Nephrotic syndrome
- Severe malnutrition
- Hepatic cirrhosis
- Acute or chronic renal failure
- Hypothyroidism
Long essay on immunity and disease
Question 3. Diagnostic procedures for hypersensitive reactions
Answer:
Hypersensitive Reactions Diagnostic Tests:
- Precipitation test
- When a soluble antigen reacts with its antibody in the presence of electrolytes at optimal temperature and pH, the antigen-antibody complex forms an insoluble precipitate called precipitation
- Tests:
- Ring test
- Ring is formed at the junction of antigen and antibody
- Flocculation test
- When instead of sedimenting, the precipitate is suspended as floccules, the reaction is called flocculation
- Immunodiffusion test
- Gel is used in it
- Types
- Single diffusion in one dimension
- Double diffusion in one dimension
- Single diffusion in two dimension
- Double diffusion in two dimension
- Immunoelectrophoresis
- Electroimmunodiffusion
- Ring test
- Counter immune electrophoresis
- Rocket electrophoresis
- Agglutination:
- In it antigen combines with its antibody in presence of an electrolyte to form clumps of particles
- Types:
- Slide agglutination test
- Tube agglutination test
- Coombs test
- Heterophile agglutination test
- Weil Felix reaction
- Paul-Bunnel test
- Streptococcus MG agglutination test
- Passive agglutination test
- Latex agglutination test
- Haemagglutination test
- Coagglutination
- Complement fixation test:
- Antigen-antibody complex formed fixes complement
- Neutralisation test
- Bacterial exotoxins neutralises antibody
- Immunofluorescence:
- Antigen-antibody complexes produce fluorescence
Immunology essay questions with answers
Immunological Factors In Disease Short Answers
Question 1. T cells
Answer:
T cells
- T cells are lymphocytes
- They are thymus-dependent
T cells Types:
- Regulatory T cells
- T helper cells
- Facilitates B cell response to produce immunoglobulin
- The balance between T helper cells and T suppressor cells produces an optimum immune response
- Overactivity of helper cells leads to autoimmunity
- Decreased activity of helper cells causes an immunodeficiency state
- T suppressor cells
- They block the immune reaction
- Overactivity of suppressor cells leads to an immunodeficiency state
- Decreased activity of suppressor cells causes an autoimmunity state
- Effector cells
- Cytotoxic T cells
- It can lyse specific target cells
- Delayed-type hypersensitivity cells
- Responsible for delayed hypersensitivity reaction
- Cytotoxic T cells
- T helper cells
Question 2. Penicillin anaphylaxis
Answer:
Penicillin Anaphylaxis
- Penicillin allergy develops within minutes and is called an immediate hypersensitivity reaction
- Penicillin Anaphylaxis can induce both types of reactions
- Humoral-mediated immunity- causes
- Type 1- Anaphylaxis
- Type 2-Cytolytic reaction
- Type 3- Arthus reaction
- Cell-mediated immunity- causes
- Delayed hypersensitivity reaction
- Induces synthesis of IgE antibodies
- Formation of antigen-antibody complexes
- Degranulation of mast cells
- Release of inflammatory mediators
- Bronchospasm
- Laryngeal edema
- Hypotension
Immunopathology essay type questions
Question 3. Serum sickness
Answer:
Serum Sickness Causes:
- After the administration of foreign serum
- Tetanus antitoxin
- Rabies antiserum
Serum sickness Mechanism:
- Antibodies form immune complexes in blood vessels with administered antigens
- These complexes fix complement which attracts the leukocytes to the area causing direct tissue injury
Serum Sickness Features:
- Fever
- Swelling
- Lymphadenopathy
- Joint and muscle pain
- Rash
- Peripheral neuritis
- Kidney disease
- Myocardial ischemia
Question 4. Pemphigus Vulgaris
Answer:
Pemphigus Vulgaris
- Pemphigus Vulgaris is the most common type of pemphigus
Pemphigus Vulgaris Features:
- Age: 40-70 years
- Sex: Common in females
Pemphigus Vulgaris Presentation:
- Development of vesicles and bullae over skin and mucous membrane
- Rupture of vesicles or bullae
- Formation of painful ulcers that bleed profusely
- Oblique pressure on the unaffected aeas around the lesion causes the stripping of the normal skin or mucous membrane called “Nikolsky’s sign”
- Areas affected:
- Skin lesions- over scalp, trunk, and umbilical areas
- Orallesions- cheek, palate, and gingiva
- Leads to excessive pain, excessive salivation, difficulty in intake of food, halitosis
Immunological basis of disease short answers
Question 5. Allergy
Answer:
Allergy
- Allergy is a state of hypersensitivity induced by exposure to a particular antigen
- This antigenic substance capable of inducing type 1 IgE-mediated immune response
- The first dose of allergenic exposure sensitizes B lymphocytes
- The subsequent exposure results in harmful immunologic activation resulting in expression of an allergic reaction
Question 6. Urticaria
Answer:
Urticaria Types:
- IgE dependent urticaria
- Complement mediated urticaria
- Nonimmunologic urticaria
- Idiopathic urticaria
Urticaria Features:
- Formation of wheal and flare cutaneous lesions involving only superficial portions of the dermis
- This results in circumscribed wheals with erythematous raised borders with blanched centers
Question 7. Angioedema
Answer:
Etiology:
- Food or drug allergy
- Biochemical abnormality
- Absence of inhibitor of Cl esterase enzyme from serum
- Formation of kinin-like substances
Angioedema Clinical Features:
- Exhibits as smooth, diffused, edematous swelling involving face, lips, chin, eyes, tongue, and extremities
- Leads to edema of the glottis resulting in suffocation
Angioedema Treatment:
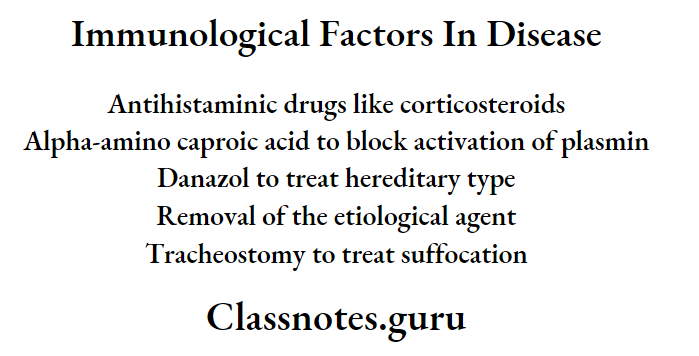
Autoimmune diseases essay questions
Question 8. Steven Johnson syndrome
Answer:
Steven Johnson Syndrome
- Steven Johnson is a severe form of erythema multiforme with widespread involvement, typically involving the skin, oral cavity, eyes, and genitalia
Steven Johnson syndrome Clinical Features:
- Symptoms:
- Fever
- Malaysia
- Photophobia
- Eruptions on oral mucosa, genital mucosa, and skin
- Skin Lesions:
- Flemorrhagic
- Vesicle and bullae are present
- Eye Lesions:
- Photophobia
- Conjunctivitis
- Corneal ulceration
- Keratoconjunctivitis
- Genital Lesions:
- Non-specific urethritis
- Balanitis
- Vaginal ulcers
- Complications:
- Trachea-bronchial ulceration
- Pneumonia
Mechanism of immune system in diseases
Steven Johnson syndrome Treatment:
- ACTH
- Cortisone
- Chlortetracycline
VIVA VOCE
- Adrenaline is the drug of choice in anaphylaxis