Developmental Disturbances Of Oral And Paraoral Structures Important Notes
- Types Of Cheilitis Glandular
- Simple
- Superficial suppurative
- Deep suppurative
- Laband Syndrome – Features
- Splenomegaly
- Enlarged nasal and external car soft tissue
- Shorter terminal phalanges
- Hypermobility of joints
- Hypoplasia of nails
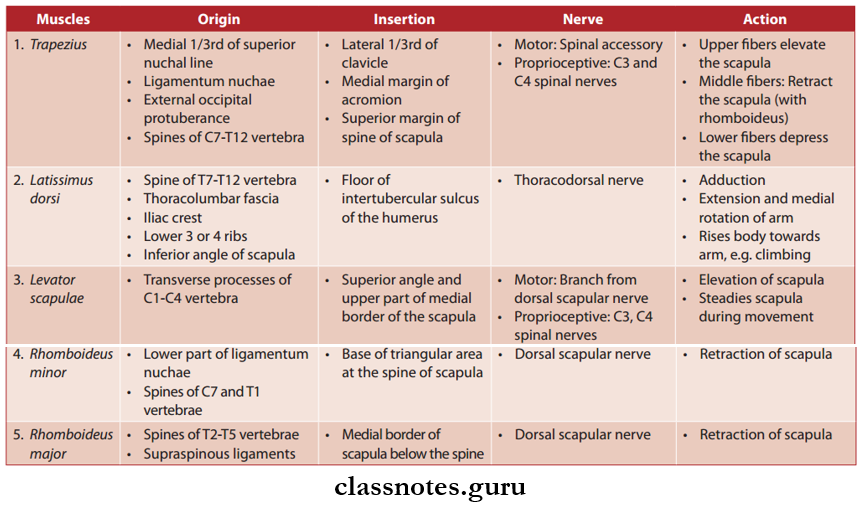
- Synonyms Of Different Terms
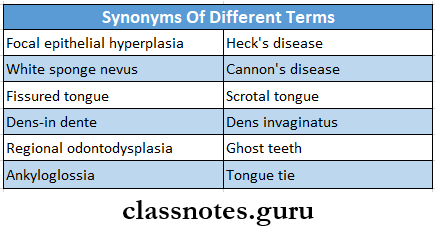
- Natal And Neonntnl Tooth
- Developmental Disorders
- Development Conditions Of The Tongue
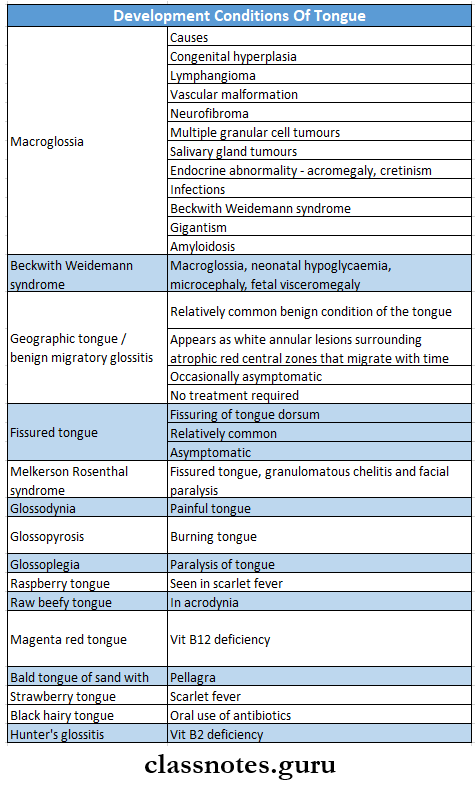
- Parillae Involved In Different Conditions
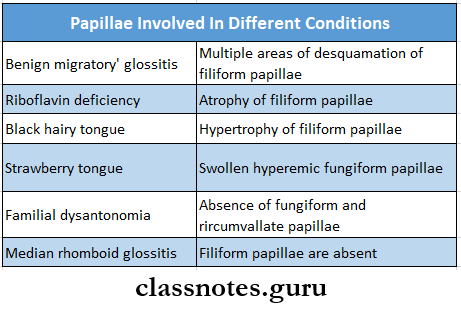
- Enamel Hypoplasia
- Enamel Hypoplasia Causes
- Hereditary
- Environmental
- Nutritional deficiencies
- Exanthematous diseases
- Congenital syphilis
- Hypocalcemia
- Local infection or trauma
- Fluorosis
- Enamel Hypoplasia Types:
- Enamel Hypoplasia Causes
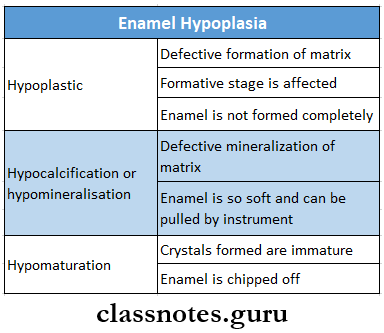
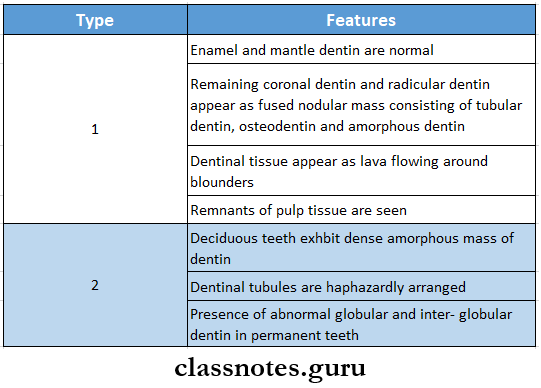
- Dentin Dysplasia
- Characterized by normal enamel but atypical dentin formation with abnormal pulpal morphology
- Dentin Dysplasia Types:
- Delayed Eruption Is Seen In
- Rickets
- Down syndrome
- Hypopituitarism
- Cleidocranial dysplasia
- Achondroplasia
- Cretinism
- Fibromatosis gingiva
- Cherubism
- Heck’s Disease Or Focal Epithelial Dysplasia
- Occurs predominantly in children
- Presents as multiple nodular lesions occurring mostly over the lower lip
- Lesions contain virus particles
- Gives a cobblestone or fissured appearance
Developmental Disturbances Of Oral And Paraoral Structures Long Essays
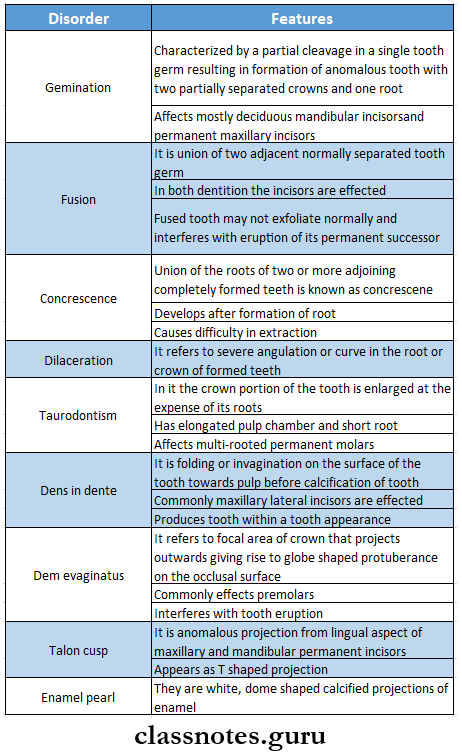
Question 1. Enumerate and describe developmental disturbances affecting the shape of teeth.
(or)
Discuss developmental disturbances affecting the morphology of the tooth
Answer:
Developmental Disturbances Affecting The Shape Of Teeth:
Read And Learn More: Oral Pathology Questions and Answers
Question 2. Enumerate various causes of enamel hypoplasia and describe hypoplasia of teeth associated with fluorosis.
(or)
Classify enamel hypoplasia. Describe Ethiopia- to genesis and clinical features of mottled enamel.
Answer:
Enamel Hypoplasia: It is defined as an incomplete or defective formation of the organic enamel matrix of teeth
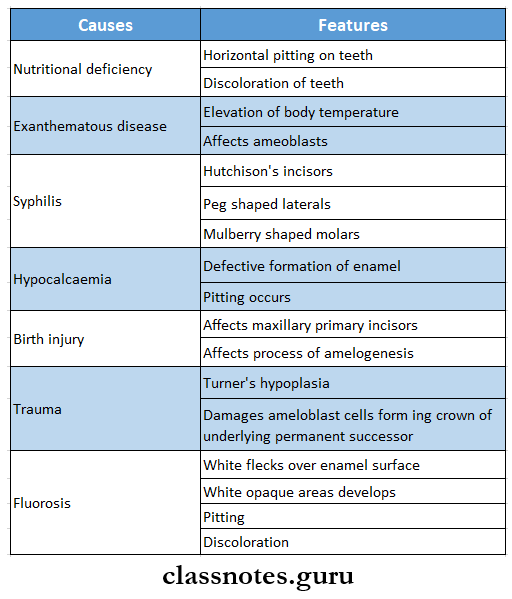
Enamel Hypoplasia Types And Causes:
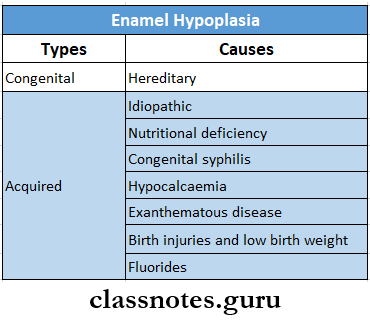
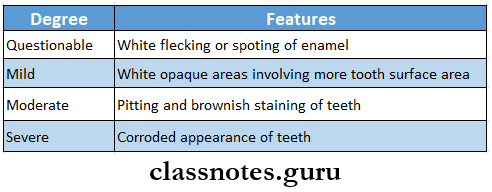
Enamel Hypoplasia Due to Fluorides: Mottled enamel results due to fluoride
Enamel Hypoplasia Etiology: Ingestion of fluoride-containing drinking water during tooth formation
Enamel Hypoplasia Pathogenesis:
- Higher levels of fluoride during the formative phase of tooth development
- Interference in tooth calcification
- Defective enamel matrix formation
Enamel Hypoplasia Clinical Features:
Depending upon the level of fluoride there is a wide range of severity in the appearance of mottled enamel
Enamel Hypoplasia Treatment:
Bleaching of affected teeth for cosmetic purposes
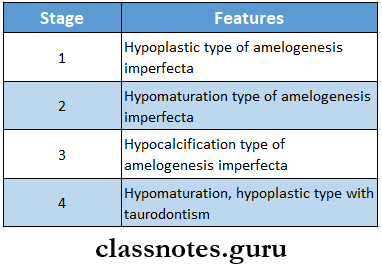
Question 3. Write in detail on amelogenesis imperfecta enamel hypoplasia.
Answer:
Amelogenesis Imperfecta Definition:
Amelogenesis Imperfecta is a heterogeneous group of hereditary disorders of enamel formation affecting both deciduous and permanent dentition
Amelogenesis Imperfecta Stages:
Amelogenesis Imperfecta Clinical Features:
- Affects both dentitions
- Color- chalky white to yellow
- Prone to disintegration
- Open contact points due to loss of enamel
- Abraded occlusal surfaces and incisal edges
- Abrasion of dentin
- Cheesy consistency of enamel
- Alteration in the eruption process
- Anterior open bite
- Presence of grooves and wrinkles on enamel surfaces
- The presence of some white opaque flecks at incisal margins giving Snow-capped teeth appearance
Amelogenesis Imperfecta Radiographic Features:
- Enamel appears thin over cusp tips and on inter-proximal areas
- Hypoplastic type- radiodensity of enamel is greater than adjacent dentin
- In hypomaturation type- the radiodensity of enamel is equal to normal dentin
Amelogenesis Imperfecta Treatment:
Composite veneering for cosmetic reasons
Question 4. Describe the pathogenesis and clinical features of enamel hypoplasia due to congenital syphilis. Enumerate environmental causes for enamel hypoplasia. Write in detail about them
Answer:
Enamel Hypoplasia Due To Congenital Syphilis: Enamel hypoplasia can occur in congenital syphilis
Enamel Hypoplasia Due To Congenital Syphilis Pathogenesis:
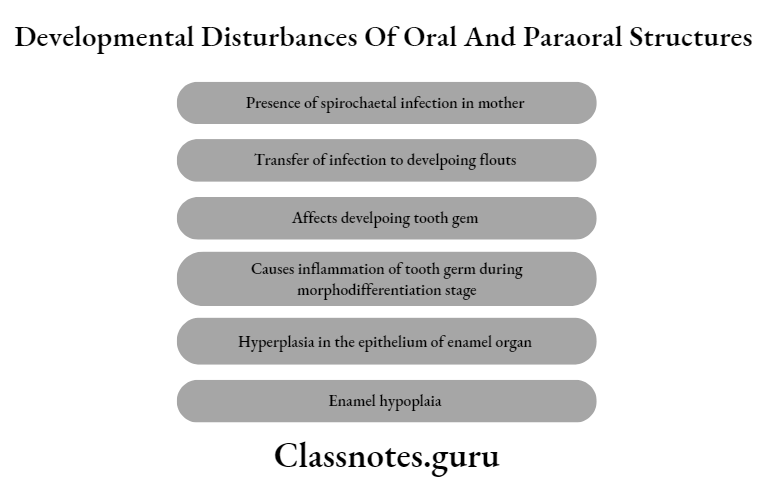
Enamel Hypoplasia Due To Congenital Syphilis Clinical Features:
- Commonly affects permanent incisors and molars
- Affected incisors exhibit tapering of mesial and distal surfaces towards incisal edges
- Results in screwdriver appearance of teeth
- Central notch develops at the incisal edge
- Such teeth are called Hutchison’s incisors
- Peg-shaped lateral incisors
- Discolored occlusal surfaces of molars
- Affected teeth are covered by a globular mass of enamel called Moon molars or Mulberry molars
Environmental Causes For Enamel Hypoplasia
Enamel Hypoplasia Due To Congenital Syphilis Treatment:
- Restoration
- Veneering- in severe hypoplasia
- Bleaching with 30% hydrogen peroxide
- Calcium sucrose phosphate gel
- Desensitizing paste
Question 5. Enumerate the developmental disturbances in the formation of dentin. Write in detail the clinical types, clinical features, radiographic
features and histopathological features of dentin dysplasia.
Answer:
Developmental Disturbances in Dentin Formation:
- Dentinogenesis imperfect
- Dentin dysplasia
- Regional odontodysplasia
- Dentin hypo calcification
Dentin Dysplasia:
- Dentin Dysplasia is an autosomal dominant inherited disorder characterized by defective dentin formation
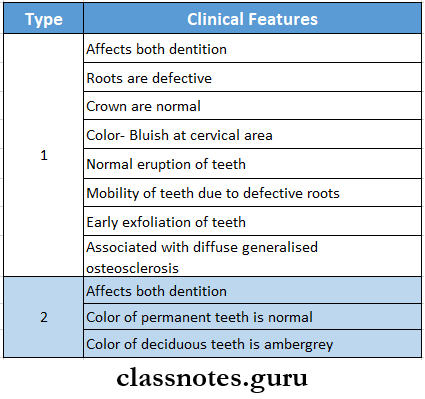
Dentin Clinical Types:
- Type 1- radicular dentin dysplasia affecting radicular dentin
- Type 2- coronal dentin dysplasia affecting coronal dentin
Dentin Clinical features
Dentin Radiographic Features
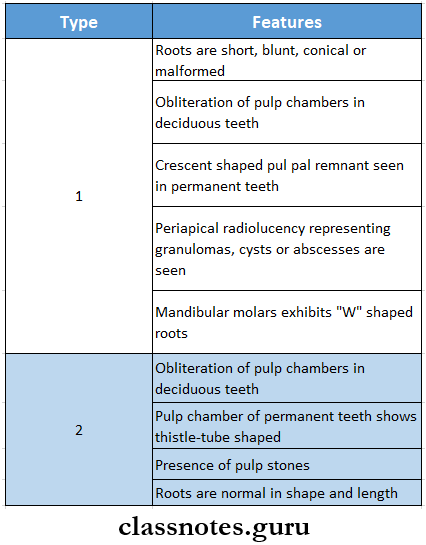
Dentin Histopathological Features
Question 6. Write in detail on dens invaginatus and dens evaginatus.
Answer:
Dens Invaginatus: It refers to folding or invagination on the surface of the tooth towards the pulp before calcification of the tooth
Dens invaginatus Types:
- Coronal Type
- In it, invagination occurs on the crown portion of the tooth
- Type 1- Invagination occurs within the crown of the tooth
- Type 2- Invagination extends below the cementoenamel junction
- Type 3- Invagination extends through root
- In it, invagination occurs on the crown portion of the tooth
- Radicular Dentin
- Invagination occurs in the root portion of teeth
Dens Invaginatus Clinical Forms:
- Mild Form
- The presence of deeply invaginated or accentuated lingual pit
- Intermediate Form
- Reveals small pear-shaped invagination of enamel and dentin into pulp chamber
- Results in tooth within a tooth appearance
- Extreme Form
- Invagination extends beyond the pulp chamber
- Also known as dilated odontomas
Dens Invaginatus Significance:
- Susceptible to
- Caries
- Pulpitis
- Pulp necrosis
- Periapical cysts
- Periapical abscesses
Dens Evaginatus: It refers to the focal area of the crown that projects outwards giving rise to a globe-shaped or nipple-shaped protuberance on the occlusal surface
Dens Evaginatus Clinical Features:
- Mainly affects premolars
- The affected tooth exhibits globe globe-shaped extra cusp on the occlusal surface between the buccal and lingual cusp
- Also affects molars, canines, and incisors
- Intel refers to tooth eruption
- Causes malocclusion
- Predisposes to pulpitis
Question 7. Describe in detail dentinogenesis imperfecta.
Answer:
Dentinogenesis Imperfecta: It is an inherited disorder of dentin formation characterized by excessive formation of defective dentin
Dentinogenesis Imperfecta Types:
- Type 1- Dentinogenesis imperfecta associated with osteogenesis imperfecta
- Type 2- Dentinogenesis imperfect without osteogenesis imperfecta
- Type 3- Bradywine type
Dentinogenesis Imperfecta Clinical Features:
- Affects both dentition
- On eruption- teeth have amber-like translucency
- A few days after appeared to normal
- Later color becomes yellowish-brown
- Teeth exhibit broad crown and narrow constricted cervical area giving a shape appearance
- Early loss of enamel
- Attrition of dentin
- Dentinal tubules are haphazardly arranged
- Dentin is soft and easily penetrable
- Brandywine type is associated with multiple pulp exposure
Dentinogenesis Imperfecta Radiographic Features:
- Type 1 and Type 2
- Bell Shaped Crowns With Constricted Cervical Area
- Roots are thin and spiked
- Obliteration of pulp chamber
- Type 3
- Extremely large pulp chambers with thin shells of enamel and dentin over it
- So known as shell teeth
- Presence of multiple pulp exposure with periapical pathology
Dentinogenesis Imperfecta Treatment:
- Metal and ceramic crowns
- Complete denture prosthesis in case of severe attrition
Developmental Disturbances Of Oral And Paraoral Structures Short Essays
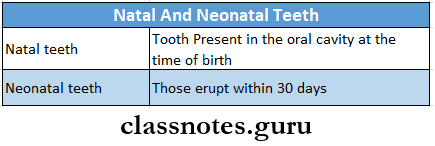
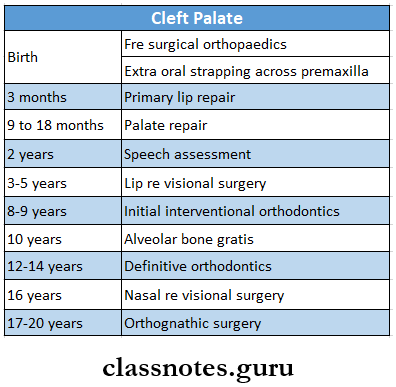
Question 1. Cleft palate
Answer:
Cleft Palate
A cleft palate is a developmental or maturation defect of the embryonic process
Cleft Palate Etiology:
- Genetic
- It is inherited as a dominant or recessive trait
- Environmental factor
- Teratogenic drugs
- Infections such as rubella
- Multifactorial
- Involves more than one factor
Predisposing Factors:
- Increased maternal age
- Race- mineraloids
- Reduced blood supply to nasomaxillary arch
Cleft Palate Clinical Features:
- Can be unilateral or bilateral
- Difficulty in eating and drinking
- Regurgitation of food and liquid through the nose
- Difficulty in speech
- Increases mental trauma
Cleft Palate Management
Question 2. Median rhomboid glossitis
Answer:
Median Rhomboid Glossitis Definition: It is an asymptomatic, elongated, erythematous patch of atrophic mucosa on the middorsal surface of the tongue
Median Rhomboid Glossitis Causes:
- Persistence of tubervulumimpar on the surface of the dorsum of the tongue
- Candidiasis
Median Rhomboid Glossitis Clinical Features:
- Initially, a narrow, mildly erythematous area develops along the median fissure on the dorsum of the tongue
- Later appears as a diamond or lozenge-shaped area
- Asymptomatic
- Size- less than 2 cm in diameter
- Color- pale pink to bright red
- Surface- smooth, flat or slightly raised, fissured or lobulated
- A similar lesion develops over the palate just opposite the tongue lesion
Histopathological Features:
- Epithelium
- Mild to severe parakeratosis
- Thinning of supra-papillary epithelium
- Neutrophilic infiltration
- The presence of numerous candidal hyphae
- Areas of irregular hyperplasia
- Rete Ridges
- Presence of acanthosis
- Elongation of rete pegs
- Connective tissue
- Very vascular
- Chronic cell infiltration
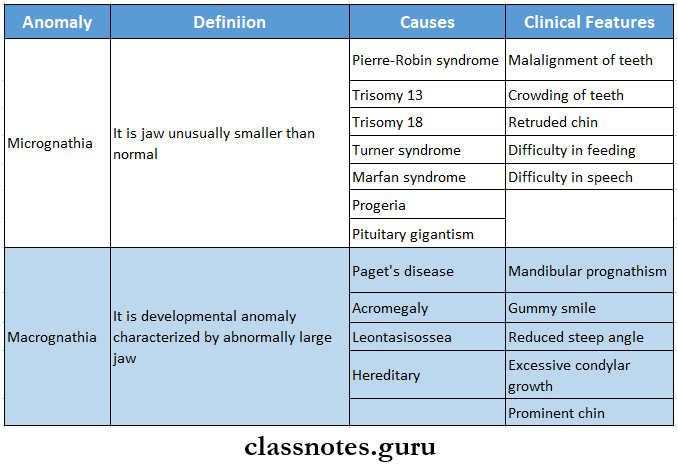
Question 3. Micrognathia and macrognathia
Answer:
Micrognathia And Macrognathia
Question 4. Fordyce’s granules
Answer:
Fordyce’s Granules
Fordyce’s granules are an ectopic collection of numerous sebaceous glands
Fordyce’s Granules Clinical Features:
- Mostly seen in adult life
- Occurs bilaterally
- The sites involved are:
- Upper lip
- Buccal mucosa
- Gingiva
- Anterior pillars of fauces
- Tongue
- Rarely over the lower lip
- The number of it increases during puberty
- Appears as multiple, small, discrete, milia-like yellowish-white bodies beneath the surface mucosa
- Size-1-2 mm in diameter
Histopathological Features:
- Glands are located superficially over surface epithelium
- Composed of 1-5 lobules
- Its duct directly opens onto the mucosal surface
- Peripheral cells are flat and darkly stained
- Inner cell are lipid-rich
Fordyce’s Granules Treatment: No treatment is required
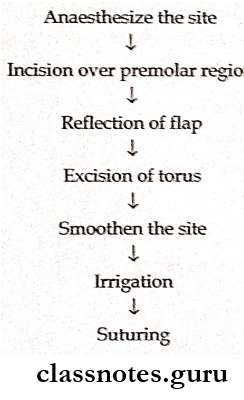
Question 5. Torus mandibular
Answer:
Torus Mandibular
Torus mandibular is an exostosis ox outgrowth of bone found on the lingual surface of the mandible
Torus Mandibularis Clinical Features:
- Seen in the first decade of life
- Occurs on the lingual surface of the mandible above the mylohyoid line opposite to the bicuspid teeth
- Torus Mandibularis may be unilateral or bilateral
- Varies in shape- flat, spindle-shaped, nodular, or lobular
- Overlying mucosa may be intact or blanched
- Torus Mandibularis may become ulcerated if traumatized
Torus Mandibularis Treatment
Question 6. Hunter’s glossitis
(or)
Moeller’s glossitis
Answer:
Hunter’s Glossitis
- Hunter’s Glossitis is an oral manifestation of pernicious anemia
- The tongue is generally inflamed
- Color- beefy red
- Patches axe present over the dorsum and lateral borders of the tongue
- Presence of aphthous ulcers
- Gradual atrophy of papilla of tongue
- Loss of taste sensation
- Inflammation -and burning sensation is present
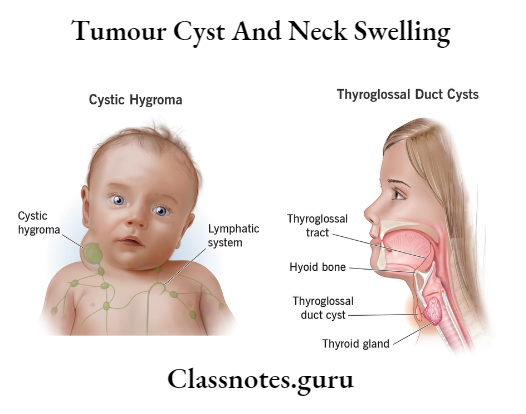
Question 7. Benign Lymphoepithelial Cyst
Answer:
Benign Lymphoepithelial Cyst
A benign Lymphoepithelial Cyst develops within a benign lymphoid aggregate or accessory tonsil of the oral or pharyngeal mucosa
Benign Lymphoepithelial Cyst Clinical Features:
- Presents as a movable, painless submucosal nodule
- Color- yellow-white
- Size- less than Ote cm in diameter
- Intraoral sites
- Floor of mouth
- Lateral and ventral surface of the tongue
- Soft palate
- CYst ruptures and produces foul-tasting cheesy discharge
Histopathological Features:
- Cyst is lined by atrophic and degenerated stratified squamous epithelium
- Absence of rete pegs.
- The cystic lumen is filled with dystrophic calcification
- Goblet cells are present within superficial layers of epithelium
- Consists of aggregates of mature lymphocytes
Benign Lymphoepithelial Cyst Treatment: Surgical excision of the cyst
Question 8. Fusion, gemination, and concrescence
Answer:
Fusion: It is defined as the union of two adjacent normally separated tooth germs at the level of dentin
Fusion Causes:
- Hereditary
- Trauma
- Physical force or pressure
Fusion Clinical Features:
- Affects both dentition
- Can occur between two normal teeth or between one normal and one supernumerary teeth
- Occurs bilaterally
- Can be complete or Incomplete
- Interferes with eruption of permanent teeth
- Leads to
- Spacing or diastema formation
- Crowding of teeth
- Esthetic problem
- Periodontal problem
- Esthetic problem
Gemination: It is a developmental anomaly characterized by partial cleavage in single tooth germ resulting in the formation of the anomalous tooth with two partially separated crowns and one root
Gemination Clinical Features:
- Affects both dentition
- Commonly affects deciduous mandibular incisors and permanent maxillary incisors
- The crown of affected teeth is extremely, widened
- Leads to
- Tooth malalignment
- Spacing of teeth
- Dental arch asymmetry
- Cosmetic problems
- Periodontal problem
- Increased caries susceptibility
- Disturbances in the eruption of teeth
Concrescence: It is the union of the roots of two or more adjoining teeth due to the deposition of cementum
Concrescence Etiology:
- Traumatic injury
- Crowding of teeth
- Hypercementosis
Concrescence Clinical Features:
- It is an acquired defect
- Occurs in both erupted or unerupted teeth
- Permanent maxillary molars are usually affected
- It can occur between a normal molar and a supernumerary molar
- Rarely involves deciduous dentition
- It is frequently seen in those areas of the dental arch where the roots of the neighboring teeth lie close to each other
Concrescence Significance: Complicates extraction
Question 9. Taurodontism
Answer:
Taurodontism
Taurodontism is a peculiar developmental condition in which the crown of the tooth is enlarged at the expense of its roots
Taurodontism Pathgenesis:
Taurodontism occurs due to failure of the Hertwig’s epithelial root sheath to invaginate at the proper horizontal level
Taurodontism Clinical Features:
- Taurodontism involves both the sex
- Taurodontism commonly affects multi-rooted permanent molar teeth and sometimes premolar
- Taurodontism rarely occurs in primary dentition
- Common in Neanderthal men
- The affected tooth exhibits an elongated pulp chamber with rudimentary roots
- Teeth are usually rectangular with minimum constriction at the cervical area
- The furcation area of the teeth is more apically placed
- Teeth often have a greater apical-occlusal height
Taurodontism Associated Syndrome:
- Down’s syndrome
- Klinefelter syndrome
- Poly X syndrome
Taurodontism Treatment: No treatment is required
Question 10. Anodontia
Answer:
Anodontia
Anodontia refers to the absence of one or more teeth
Anodontia Types:
- True- congenital absence of teeth
- False- It is due to the extraction of teeth
- Pseudo- It is due to multiple unerupted teeth in the jaw
Anodontia Causes:
- Genetic causes
- Radiation
Anodontia Clinical Features:
- Common in females
- Taurodontism may be unilateral or bilateral- Commonly missing teeth are
- 3rd molar
- Maxillary lateral incisor
- Maxillary or mandibular
- 2nd premolar
- Reduced alveolar development
- Increased freeway space
- When a deciduous tooth is missing then even its permanent successor will be missing
Anodontia Management:
- Orthodontic treatment- to correct malocclusion
- Prosthesis- traditional fixed prosthesis and resin-bonded bridges are used
Question 11. Supernumerary teeth
Answer:
Supernumerary Teeth
The presence of any extra tooth in the dental arch in addition to the normal series of teeth is called supernumerary teeth
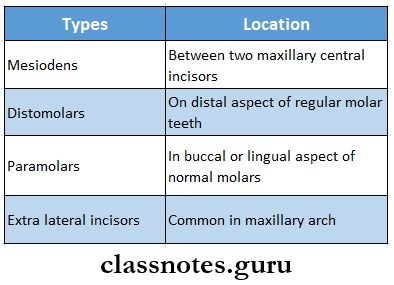
Supernumerary Teeth Mode Of Formation:
- Supernumerary Teeth may develop either from an accessory tooth bud in the dental lamina
- Supernumerary Teeth may develop due to splitting of a regular normal tooth bud during the initial phase of odontogenesis
Supernumerary Teeth Clinical Features:
- Supernumerary Teeth can occur in both sex
- Supernumerary Teeth may resemble the corresponding tooth
- Most of the teeth exhibit a conical shape
- They may be either erupted or impacted
Supernumerary Teeth Significance:
- Causes crowding or malocclusion
- Causes cosmetics problems
- Responsible for increased caries incidence and periodontal problems
- The dentigerous cyst may develop from an impacted supernumerary teeth
Supernumerary Teeth Treatment:
- Extraction
- Surgical removal of impacted teeth
Question 12. Regional odontodysplasia
Answer:
Regional Odontodysplasia
Regional Odontodysplasia is an uncommon but unique non-hereditary developmental disturbance of teeth characterized by defective formation of enamel and dentin in addition to abnormal pulp and follicle calcification
Regional Odontodysplasia Etiology:
Local ischaemic changes in the tissue during odontogenesis
Regional Odontodysplasia Clinical Features:
- Both dentitions are affected
- Maxilla is more effected than mandible
- Frequently occurs unilaterally
- Commonly affects central and lateral incisors
- Surface- soft leathery surface
- Color- yellowish-brown in color
- Affects several contiguous teeth in a single quan- grant
- Affected teeth show delayed eruption or complete failure of eruption
Regional Odontodysplasia Radiographic Features:
- Marked decreased radiodensity
- Enamel and dentin are very thin
- The ghostly appearance of involved teeth
- Pulp chambers are extremely large and open
- Pulp chambers often contain pulp stones
Regional Odontodysplasia Treatment:
- Extraction of involved teeth
- Fabrication of prosthesis
Question 13. Benign migratory glossitis and geographic tongue classification.
Answer:
Benign Migratory Glossitis
Geographic tongue is also termed benign migratory glossitis due to the constantly changing pattern of serpiginous white lines surrounding areas of smooth, depopulated mucosa
Benign Migratory Glossitis Clinical Features:
- Age- 5-84 years
- Sex- slight predilection to females
- Site- dorsal surface and lateral margins of the tongue
- Size- varies in diameter
- Presentation
- It is asymptomatic
- The patient may complain of a burning sensation on spicy foods or intake of citrus fruits
- It appears as an erythematous, non-indurated, atrophic lesion
- Bordered by slightly elevated distinct rim
- Multiple areas of desquamation of filiform papilla in an irregular fashion are seen
- The central portion appears inflamed
- Fungiform papilla persists as elevated red dots
Benign Migratory Glossitis Management:
- Topical application of anesthetic agents
- Balanced diet
- Elimination of irritants
- Psychological reassurance
- Topical corticosteroids
Benign Migratory Glossitis Geographic tongue
Benign Migratory Glossitis is defined as an irregularly shaped reddish area of depopulation and thinning of dorsal tongue epithelium which is surrounded by a narrow zone of regenerating papillae that are whiter than the surrounding tongue surface
Benign Migratory Glossitis Geographic Tongue Classification:
- Type 1- lesions are confined to the tongue
- Type 2- lesions axe also seen elsewhere in the mouth
- Type 3- lesions on the tongue that are not typical and that may be accompanied by lesions elsewhere in the mouth
- Type 4- no tongue lesions are present but geographic areas are present in the mouth
Developmental Disturbances Of Oral And Paraoral Structures Viva Voce
- Cheilitis glandular is a chronic, progressive enlargement of the labial salivary gland
- Hypertrichosis is the presence of thick and abundant hair
- Double lip appears as a cupid’s bow
- Peutz-Jeghers syndrome is characterized by intestinal polyposis and mucocutaneous pigmentation, precocious puberty
- Fordyee’s granules are an ectopic collection of numerous sebaceous glands
- Ascher’s syndrome is characterized by double lip, Blepharochalasis, and nontoxic thyroid enlargement
- Median rhomboid glossitis is due to the persistence of tuberculum impair
- A hairy tongue is characterized by hypertrophy of filiform papilla
- Teeth that erupt within 1st month of birth are neonatal
- Teeth that are present at the time of birth are natal
- Taste buds are predominantly located on the cerium-vallate papilla
- Taurodontism is associated with klinefilter syndrome.
- Mesiodens are courmoa supernumerary teeth.
- Bohri’s nodules are seen at the junction of the hard and soft palate.
- Epstein pearls are seen along the median raphe of the hard palate.
- Dental lamina cysts are newborn alveolar ridges.
- The most common ankylosed teeth are deciduous mandibular second molar.
- The most common missing deciduous teeth is maxillary and mandibular lateral incisors,
- The most common missing permanent is third molars
- The most commonly affected teeth are microdontia is maxillary lateral incisors.
- Blue sclera is seen in osteogenesis imperfecta.
- Regional adontodysplasia is also called ghost teeth due to smaller crowns and larger pulp chambers.
- Rootless teeth are characteristic of dentin dysplasia.
- Shell teeth are seen in dentinogenesis imperfect type 111
- Germination is the division of single tooth germ by invagination
- In germination patient has one tooth more than normal.
- Fusion is union of two normally separated tooth germ.
- In fusion, patients will have one tooth less than normal.
- Permanent molars are most commonly affected by taurodontism.
- The torus mandibularis is commonly seen on the lingual surface of the the mandible opposite of the premolar.

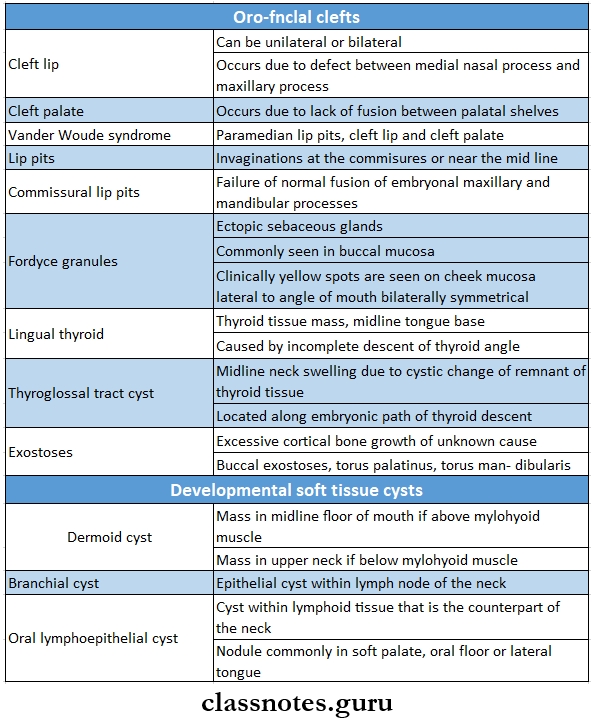
 Pectoral Muscles Anatomy Short Essay
Pectoral Muscles Anatomy Short Essay