Plaque Control Important Notes
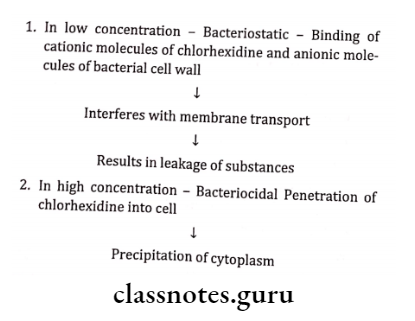
1. Chlorhexidine
- Chemically it is biguanidohexane with antiseptic properties
- Daily rinses with 10 ml of 0.2% aqueous solution effectively inhibit the development of plaque, calculus, and gingivitis
- The minimum concentration of chlorhexidine needed to inhibit plaque is 0.12%
- Chlorhexidine inhibits gram +ve, gram -ve organisms, and yeasts
- It is bacteriostatic at low concentrations and bacteriocidal at high concentrations
- Chlorhexidine causes local reversible side effects
- Side effects:
- Yellow-brown staining of teeth
- Mucosal soreness
- Desquamation
- Altered taste sensation
Read And Learn More: Periodontics Question and Answers
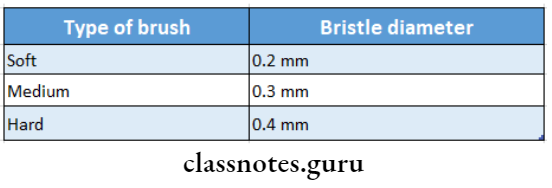
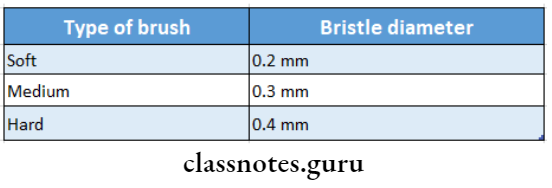
2. Types Of Brush
3. ADA’s specification of toothbrush
- Tooth head should be
- 1-1/4 inch in length
- 5/16-3/8 inches in width
- 2-4 rows of bristles
- 5-12 tufts per row
- 80-86 bristles per tuft
Plaque Removal Techniques
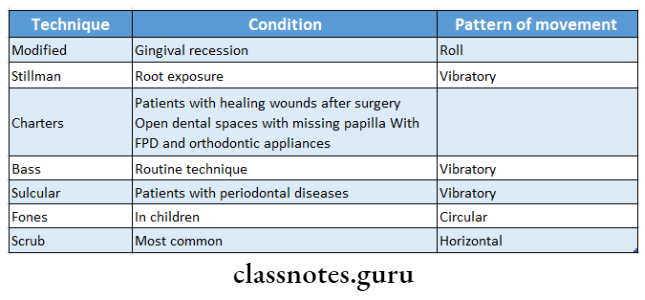
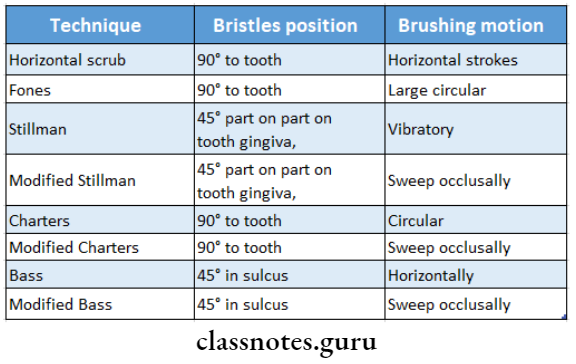
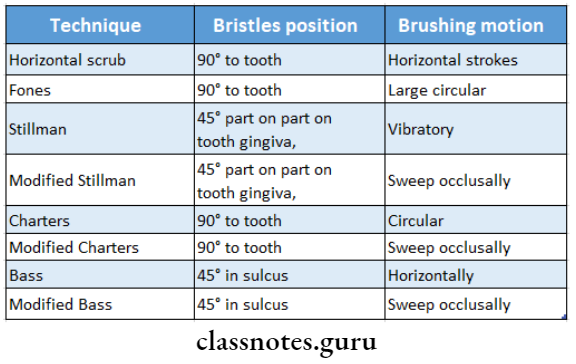
4. Brushing Techniques
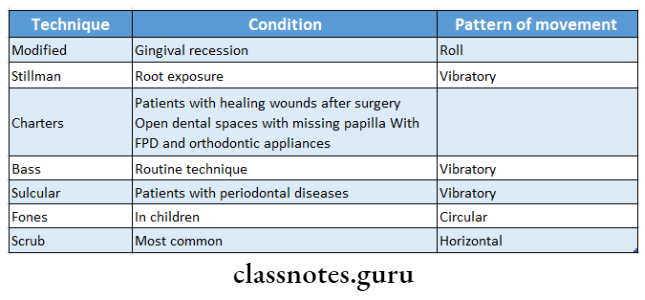
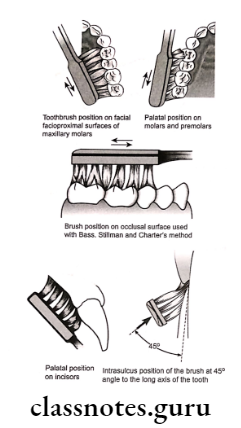
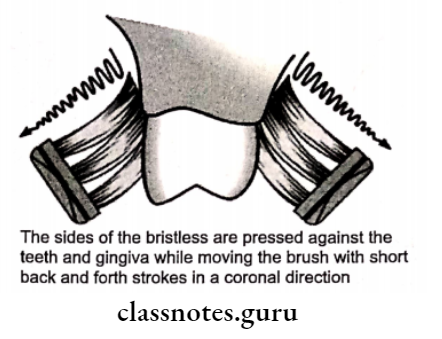
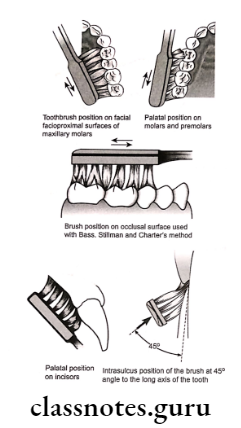
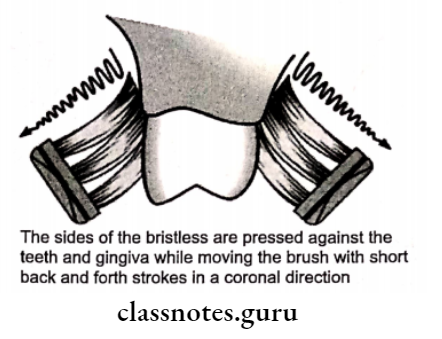
4. BassTechnique
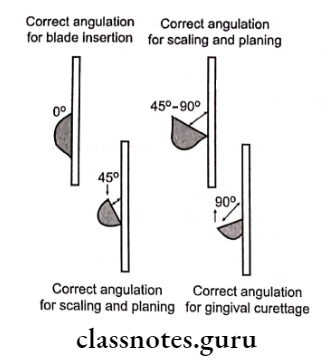
- In it, the bristles are placed at the gingival margin at an angle of 45° to the long axis of the tooth
- This forces the bristle ends into the gingival sulci and interproximal embrasures
- Produces blanching of the gingiva
- Helps in the cleaning of the cervical third of the tooth, gingival sulci, and interproximal areas.
5. Interdental cleansing aids
6. Composition of gentrifies
- Abrasives – CaCO3, Calcium phosphate
- Humectants – Maintains moisture
- Glycerine, sorbitol
- Preservatives – Benzoic acid
- Thickening agents – methylcellulose
- Foaming agents – Sodium lauryl sulfate
- Flavoring agents – Mint
- Sweetening agents – Mannitol, Saccharine
- Desensitizing agents – Sodium fluoride
- Anticalculus agent – Pyrophosphates
7. Anti-plaque mouth rinses
- Chlorhexidine
- Cetyl pyridine
- Essential oils
- Sanguinarine
- Sodium benzoate
8. Oral irrigating devices
- They disrupt and detoxify the bacterial plaque
- They effectively clean the nonadherent bacteria and debris in periodontal pockets
- Water and dilute chlorhexidine can be used as irrigating agents
9. Disclosing agents
- Disclosing agents stain bacterial deposits on teeth, tongue, and gingiva
- They help in the education and motivation of the patients
- It is a simple way to instruct the patients in the dental office
- Some disclosing agents are:
- Erythrosin
- Bismark brown
- Two-tone solution
- Mercurochrome
- Malachite green
10. Chemical plaque control
- It is adjuvant to mechanical plaque control
- It is used
- After periodontal surgery
- In poorly motivated patients
- Medically compromised patients
- Prophylactic rinse during scaling
- In gingival enlargements
- In patients with fixed appliances
- Mentally and physically handicapped patients
11. Local drug delivery system
Agents used for it are
- Activity tetracycline containing fibers
- Atridox-10% doxycycline
- Periocline- 2% minocycline
- Periochip – a small chip containing 2.5 mg of chlorhexidine
Plaque Removal Techniques
Plaque Control Long Essays
Question 1. What is plaque control? Describe various measures of plaque control.
Answer:
Plaque Control:
- Plaque Control is the removal of dental plaque on a regular basis and the prevention of its accumulation on teeth and adjacent gingival surfaces.
Plaque Control Mechanical:
Types based on the diameter of bristles:
- Soft-0.007-0.009 inches
- Medium -0.010 -0.012 inches
- Hard-0.013-0.014 inches
- Extra hard-0.015 inches
Based on use:
- Manual
- Automatic/Powered
- Frequency of brushing – every 12 hours
- Frequency of change of brush every 3 months
- Length of brushing time
- Initially 10-20 minutes
- Later 3-5 minutes
2. Dentrifices:
- Used in the form of powders, pastes, and gels
- Composition
- Abrasives – CaCO3, Calcium phosphate
- Humectants – Maintains moisture
- Periodontics
- Glycerine, sorbitol
- Preservatives – Benzoic acid
- Thickening agents – methylcellulose
- Foaming agents – Sodium lauryl sulfate
- Flavoring agents – Mint
- Sweetening agents – Mannitol, Saccharine
- Desensitizing agents – Sodium fluoride
- Anticalculus agent – Pyrophosphates
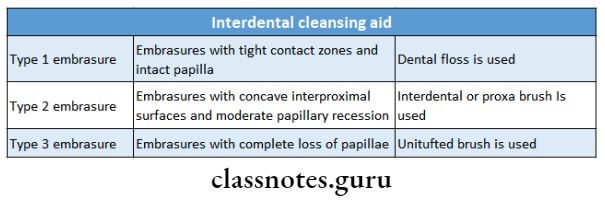
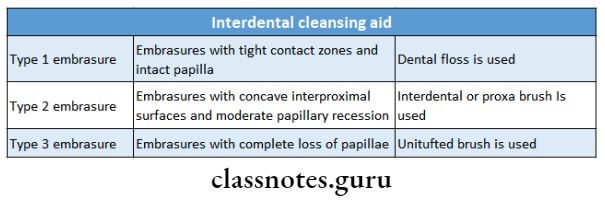
3. Interdental Cleaning aids:
Use: In periodontally involved patients, open embrasures
- Various aids:
- Dental floss
- Interdental brushes
- Wooden tips
- Yarns, gauze strips
4. Gingival massage:
- Devices used
- Toothbrush
- Rubber tip stimulator
- Interdental cleaning devices
Gingival massage Effects:
- Epithelial thickening
- Increased Keratinization
- Increased mitotic activity
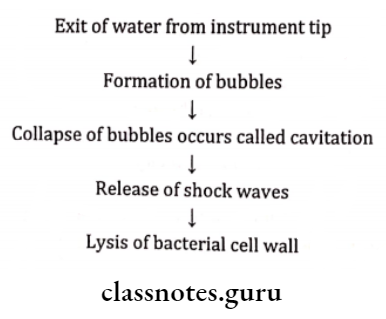
5. Oral irrigation:
- Clean non-adherent bacteria and debris
- Disrupt and detoxify subgingival plaque
- Delivers antimicrobial agents into periodontal pockets
- Irrigator tips: Cannula type, soft rubber tip
Chemical Plaque Control.
Plaque Removal Techniques
Oral irrigation Use: As an adjunct
- Prevents recurrence of disease
Oral irrigation Classification:
1. First generation:
- Reduces plaque score by 20-50%
Example: Antibiotics
2. Second generation:
- Reduces plaque score by 70-90%
Example: bisbiguanides
3. Third generation:
- Effective against specific organisms
Chemicals:
- Antibiotics Penicillin
- Enzymes – Lipase
- Quarternary Ammonium Compounds – Benzalkonium chloride
- Bisbiguanides – Chlorhexidine
- Metallic salts – Copper, Zinc
- Herbal extracts
- Phenols
- Hydrogen peroxide
- Fluorides
- Others Triclosan
Question 2. Define oral hygiene and gingival physiotherapy. Describe various aids available for plaque control
Answer:
Oral Hygiene:
- The cleanliness of the oral cavity is appraised in terms of the extent of accumulated food debris, plaque, mate- ria alba, and tooth surface stains
Gingival Physiotherapy:
- Mechanical stimulation of the gingiva either by toothbrush- ing or interdental cleansing with various aids or simple finger massage leads to
- Increased keratinization
- Increased blood flow
- The increased flow of GCF within the gingival sulcus
Measures Of Plaque Control:
Mechanical measures
1. Toothbrush:
- The frequency of brushing should be once every 12 hours
- Frequency of change of brush- every three months
- Length of brushing time
- Initially-10-20 minutes
- Later-3-5 minutes
2. Dentrifices:
- Used in the form of powders, pastes, and gels
Dentrifices Composition:
- Abrasives- calcium carbonate, calcium phosphate
- Mechanically clean the teeth
- Removes stained pellicles from the tooth surface
- Restores natural lustre
- Aids in eliminating plaque from the tooth surface
- Humectants
- Maintains moisture
- Glycerine, sorbitol
- Preservative- benzoic acid
- Prevents microbial growth
- Thickening agent-methyl cellulose
- Binds the solids to form a homogenous paste and ease dispersion of paste in the mouth
- Controls stability and consistency of tooth-paste
- Foaming agents- sodium lauryl sulfate
- Produces foam which aids in the removal of food debris
- Antimicrobial property
- Flavoring agents-Mint
- Render the product pleasant to use
- Sweetening agents- mannitol, saccharine
- Imparts sweetness and makes it pleasant
- Desensitizing agents- sodium fluoride
- Anticalculus agent-pyrophosphates
3. Interdental cleaning aids:
Interdental cleaning aids Use:
- In periodontally involved patients
- Open embrasures
Interdental cleaning aids Various Aids:
- Dental floss
- Interdental brushes
- Wooden tips
- Yarns, gauze strips
4. Gingiva massage:
Gingiva massage Devices Used:
- Toothbrush
- Rubber tip stimulator
- Interdental cleaning devices
Gingiva massage Effects:
- Epithelial thickening
- Increased keratinization
- Increased mitotic activity
5. Oral irrigation:
- Clean non-adherent bacteria and debris
- Disrupt and detoxify subgingival plaque
- Delivers antimicrobial agents into periodontal pockets
Oral irrigation Irrigation Tips:
- Cannula type
- Soft rubber tip
Chemical plaque control
Oral irrigation Uses:
- As adjunct
- Prevents recurrence of disease
Oral irrigation Classification:
1. First generation:
- Reduces plaque score by 20-50%
- Example: antibiotics
2. Second generation:
- Reduces plaque score by 70-90%
- Example: bisbiguanides
3. Third generation:
- Effective against specific organisms
Chemicals Used:
- Antibiotics- Penicillin, Erythromycin
- Enzymes- Lipase, Amylase
- Quaternary ammonium compounds- Benzalkonium chloride
- Bisbiguanides- Chlorhexidine
- Metallic salts- Copper, zinc
- Herbal extracts
- Phenols
- Hydrogen peroxide
- Fluorides
- Others- Triclosan
Question 3. What is oral physiotherapy? Describe the indications, contraindications, advantages, and disadvantages of modifying Stillman’s method.
Answer:
Oral Physiotherapy
- It is mechanical stimulation of the gingiva either by toothbrushing or interdental cleansing with various aids or simple finger massage leads to
- Increased keratinization
- Increased blood flow
- The increased flow of GCF within the gingival sulcus
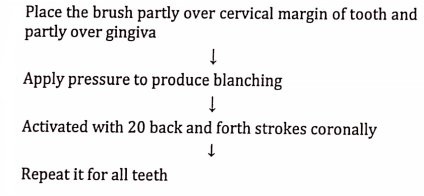
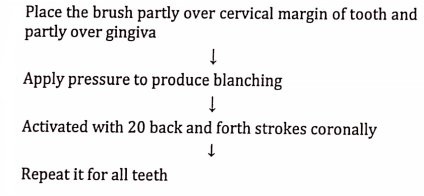
Modified Stillman’s Technique:
Modified Stillman’s Technique Indications:
- In gingival recession
- Dental plaque removal from cervical areas below the height of the contour of the enamel
- Gingival massage
Modified Stillman’s Technique:
Modified Stillman’s Technique Advantages:
- Prevents abrasive tissue destruction
Modified Stillman’s Technique Disadvantages:
- Time-consuming
- Improper brushing can damage the epithelial attachment
Question 4. Define plaque. Describe the formation and maturation of plaque. Add a note on the chemical method of plaque control.
Answer:
Plaque Definition:
- Plaque is defined clinically as a structurally resilient, yellowish-grey substance consisting of bacterial agree- nations that adhere tenaciously to teeth and other in- intraoral hard surfaces such as restorations
Formation of Plaque:
- Formation of an organic pellicle
- A thin, saliva-derived layer called acquired pellicle covers the tooth surface and it consists of numerous components including glycoproteins, proline-rich proteins, phosphoproteins, and histidine-rich proteins. enzymes and other molecules that can function as adhesion sites for bacteria
- This involves the adsorption of positively charged salivary crevicular fluid and other environmental macromolecules to negatively charged hydroxyapa- tite surfaces of teeth
- Its formation on the teeth surfaces forms the sub- strate for colonization and subsequent proliferation of micro-organisms
- Initial adhesion and attachment of bacteria
- Formation of the organic pellicle aids in the adherence of certain bacteria to the tooth surface
- These are the initial colonizers
- Bacterial adherence occurs through specific at-attachments
- With the multiplication and growth of the primary colonizers, the extra-cellular matrix also increases through the accumulation of bacterial products
Dental Plaque Prevention
Plaque Maturation:
- Initial colonizers make use of available oxygen, leading to the reduced oxygen level
- This becomes favorable for anaerobic bacteria to grow
- These organisms then adhere to the cell surface receptors of the initial colonizers
- Hence the plaque matures
Chemical Plaque Control
Chemical Plaque Control Uses:
- As adjunct
- Prevents recurrence of disease
Chemical Plaque Control Classification:
- First generation
- Reduces plaque score by 20-50%
- Example: antibiotics
- Second generation
- Reduces plaque score by 70-90%
- Example: bisbiguanides
- Third generation
- Effective against specific organisms
Plaque Control Chemicals Used:
- Antibiotics- Penicillin, Erythromycin
- Enzymes- Lipase, Amylase
- Quaternary ammonium compounds- Benzalkonium chloride
- Bisbiguanides- Chlorhexidine
- Metallic salts-Copper, zinc
- Herbal extracts
- Phenols
- Hydrogen peroxide
- Fluorides
- Others- Triclosan
Dental Plaque Prevention
Plaque Control Short Essays
Question 1. Chlorhexidine.
Answer:
Chlorhexidine Indications:
- As an adjunct to the mechanical method
- Immediately after pack removal
- After oral surgical procedures
- In patients with fixed appliances
- For handicapped patients
- Drug-induced gingival enlargements
- Medically compromised patients
- Acute infections
- As prophylactic rinse
Chlorhexidine Adverse Effects:
- Staining of teeth
- Burning sensation
- Impaired taste sensation
- Rarely, parotid swelling
Chlorhexidine Mechanism:
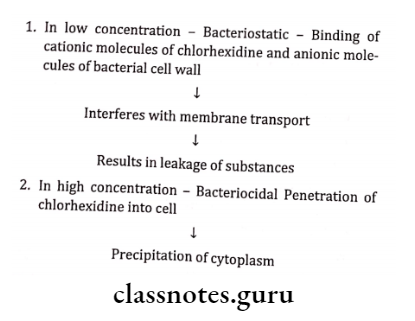
Chlorhexidine Efficient concentration
Question 2. Brushing Techniques.
Answer:
Dental Plaque Prevention
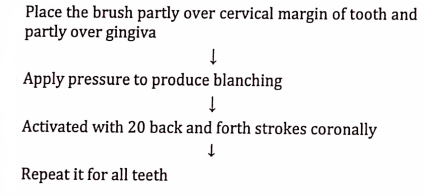
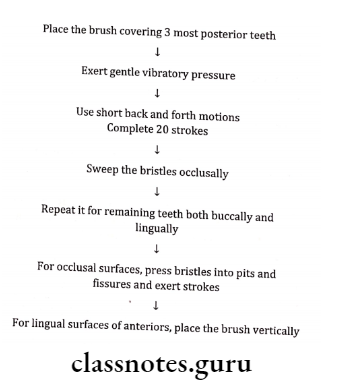
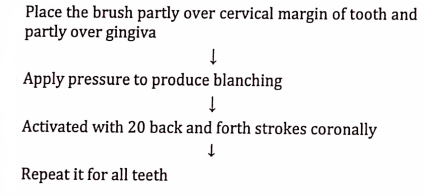
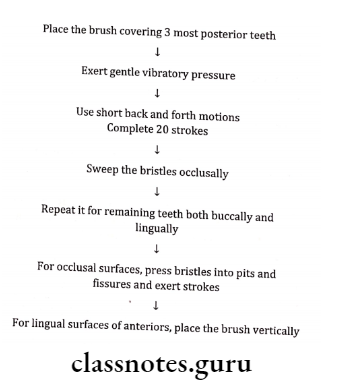
Question 3. Modified Bass Techniques.
Answer:
- Placement of head – 45° to the long axis of teeth
- Initial most posterior teeth
Modified Bass Techniques Method:
Question 4. Dentrifices
Answer:
- Used in the form of powders, pastes, and gels
Dentrifices Composition:
- Abrasives- calcium carbonate, calcium phosphate
- Mechanically clean the teeth
- Removes stained pellicles from the tooth surface
- Restores natural lustre
- Aids in eliminating plaque from the tooth surface
- Humectants
- Maintains moisture
- Glycerine, sorbitol
- Preservative- benzoic acid
- Prevents microbial growth
- Thickening agent-methyl cellulose
- Binds the solids to form a homogenous paste and ease dispersion of paste in the mouth
- Controls stability and consistency of toothpaste
- Foaming agents- sodium lauryl sulfate
- Produces foam which aids in the removal of food debris
- Antimicrobial property
- Flavoring agents- Mint
- Render the product pleasant to use
- Sweetening agents- mannitol, saccharine
- Imparts sweetness and makes it pleasant
- Desensitizing agents- sodium fluoride
- Anticalculus agent-pyrophosphates
Question 5. Merits and limitations of toothbrush (or) Uses and abuses of toothbrush
Answer:
Merits Or Uses Of Toothbrush:
- Cleans teeth and interdental spaces and prevents plaque formation
- It disturbs and removes plaque
- Stimulates and massages gingival tissues
- Increases patient motivation
- Increased accessibility in interproximal and lingual tooth surfaces
Limitations Or Abuses Of Toothbrush:
- Horizontal or vertical scrubbing toothbrushing method with pressure results in a scuffled epithelial surface with denuded underlying connective tissue
- Overuse of toothbrush results in punctuate lesions that appear as red pinpoint spots
- Penetration of gingiva by filament ends due to the use of a toothbrush with frayed broken bristles results in diffuse redness and denuded attached gingiva
- Gingival recession exhibits receded margin of the gingiva
- Gingival contour exhibits rolled out, bulbous, hard, firm marginal gingiva
Dental Plaque Prevention
Plaque Control Short Question And Answers
Question 1. Chemical Plaque Control.
Answer:
Chemical Plaque Control Uses:
- As adjunct
- Prevents recurrence of disease
Chemical Plaque Control Classification:
1. First generation:
- Reduces plaque score by 20-50%
Example: Antibiotics
2. Second generation:
- Reduces plaque score by 70-90%
Example: bisbiguanides
3. Third generation:
- Effective against specific organisms
Chemical Plaque Control Chemicals:
- Antibiotics Penicillin
- Enzymes – Lipase
- Quarternary Ammonium Compounds – Benzalkonium chloride
- Bisbiguanides – Chlorhexidine
- Metallic salts – Copper, Zinc
- Herbal extracts
- Phenols
- Hydrogen peroxide
- Fluorides
- Others Triclosan
Plaque Reduction
Question 2. Modified Stillman method.
Answer:
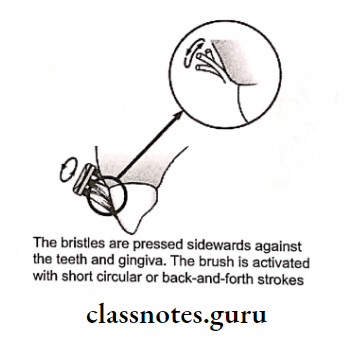
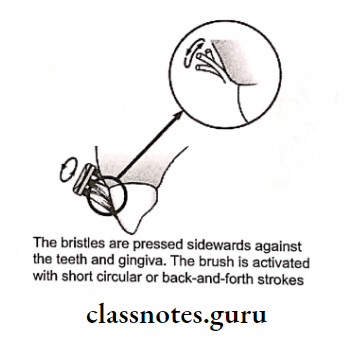
Question 3. Charter’s method.
Answer:
Charter’s method Indication: After surgery
Question 4. Powered Toothbrush.
Answer:
Powered Toothbrush Indications:
- Patient lacking motor skills
- Handicap
- Hospitalized patients
- Patient with the orthodontic appliance
Powered Toothbrush Types Of Motion:
- Reciprocating – back-and-forth movement
- Arcuate Up and down movement
- Elliptical – Combination
Question 5. Dentrifices.
Answer:
- Used in the form of powders, pastes, and gels
Dentrifices Composition:
- Abrasives- calcium carbonate, calcium phosphate
- Humectants
- Maintains moisture
- Glycerine, sorbitol
- Preservative- benzoic acid
- Thickening agent-methyl cellulose
- Foaming agents- sodium lauryl sulfate
- Flavoring agents-Mint
- Sweetening agents- mannitol, saccharine
- Desensitizing agents- sodium fluoride
- Anticalculus agent-pyrophosphates
Question 6. Interdental cleaning aids
Answer:
Interdental cleaning aids Use:
- In periodontally involved patients
- Open embrasures
Interdental cleaning aids Various Aids:
- Dental floss
- Interdental brushes
- Wooden tips
- Yarns, gauze strips
Question 7. Adverse effects of chlorhexidine.
Answer:
- Staining of teeth
- Burning sensation
- Impaired taste sensation
- Rarely, parotid swelling
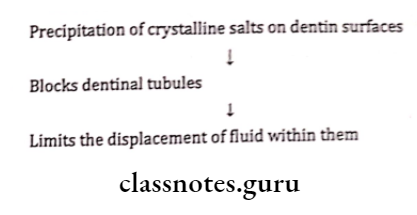
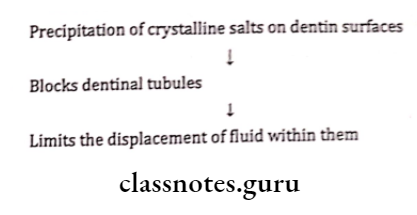
Question 8. Desensitizing agents
Answer:
Agents Used:
- Dentrifices
- Varnishes
- Fluoride compounds
Desensitizing Agents Mode Of Action:
Question 9. List three chemical plaque control agents.
Answer:
- Antibiotics- Penicillin, Erythromycin
- Enzymes- Lipase, Amylase
- Quaternary ammonium compounds- Benzalkonium chloride
- Bisbiguanides- Chlorhexidine
- Metallic salts- Copper, zinc
- Herbal extracts
- Phenols
- Hydrogen peroxide
- Fluorides
- Others- Triclosan
Question 10. Interdental brushes
Answer:
- Made of bristles mounted on a handle
- Suitable for cleaning large, irregular, or concave tooth surfaces
- Inserted interproximal and are activated with short back-and-forth strokes
- The diameter of the brush should be slightly larger than the gingival embrasures
- Single-tufted brushes are highly effective on the lingual surfaces of mandibular molars and premolars
Plaque Reduction
Question 11. Oral irrigation devices.
Answer:
Direct high-pressure, steady, or pulsating stream of water through a nozzle to the tooth surfaces is applied
Oral irrigation devices Uses:
- Clean nonadherent bacteria and debris
- Removes non-structured debris from inaccessible areas
- Used as adjuncts to tooth brushing
Oral irrigation devices Advantages:
- Retards accumulation of plaque and calculus
- Reduces gingival inflammation
Oral irrigation devices Types:
1. Home use irrigator tip:
- Soft rubber tip
- The plastic nozzle is bent at 90 degrees at the tip
- Attached to a pump
2. Subgingival irrigator:
- Cannula type- office use
- Soft rubber tip- home use
- Effective penetration of irrigant up to 70%
Question 12. Perio-aid
Answer:
- Wooden toothpicks on a handle are known as period-aid They can be used on facial or lingual surfaces throughout the oral cavity
- Deposits are removed by using either the side or the end of the tip.
- The device is particularly efficient for cleaning along the gingival margin and into periodontal pockets
Question 13. Functions of gentrifies
Answer:
- Removal of food debris, and stains and minimizing the build-up of plaque
- Anticaries action
- Mouth freshener
- The use of triclosan with copolymer Gantrez in toothpaste reduces plaque and gingivitis
- It reduces periodontitis
- Aid in cleaning and polishing tooth surfaces
Question 14. Indications of chlorhexidine
Answer:
- As an adjunct to mechanical methods
- Immediately after pack removal
- After oral surgical procedures
- In patients with fixed appliances
- For handicapped patients
- Drug-induced gingival enlargements
- Medically compromised patients
- Acute infections
- As prophylactic rinses
Question 15. Abuses of toothbrush
Answer:
- Horizontal or vertical scrubbing toothbrushing method with pressure results in a scuffled epithelial surface with denuded underlying connective tissue
- Overuse of toothbrush results in punctuate lesions that appear as red pinpoint spots Penetration of gingiva by filament ends due to use of a toothbrush with frayed broken bristles results in diffuse redness and denuded attached gingiva
- Gingival recession exhibits receded margin of the gingiva
- Gingival contour exhibits rolled out, bulbous, hard, firm marginal gingiva
Plaque Reduction
Question 16. Ideal toothbrush
Answer:
- It should fulfill an individual patient’s requirements in size, shape, and texture
- Should be easy and efficiently manipulated
- Should be readily cleaned and aerated
- Should be durable and inexpensive
- Should be designed for utility, efficiency, and cleanliness
Question 17. Gingival massage
Answer:
- It is mechanical stimulation of the gingiva either by toothbrushing or interdental cleansing with various aids or simple finger massage leads to
- Increased keratinization
- Increased blood flow
- The increased flow of GCF within the gingival sulcus
Question 18. Proxabrush
Answer:
- Proxy brushes are small interdental brushes used in type 2 embrasures
- In type 2 embrasures, dental floss is less effective in these cases because interproximal gingival recession usually leads to the exposure of concave root depressions
Question 19. Objectives of brushing teeth
Answer:
- To clean teeth, tongue, and interdental spaces of food
- remnants, debris, stains, etc
- To prevent plaque formation
- To disturb and removes plaque
- To stimulate and massage gingival tissue
Question 20. Dental Floss.
Answer:
Dental Floss Types:
- Twisted or non-twisted
- Bonded or non-bonded
- Waxed or un-waxed
- Thick or thin
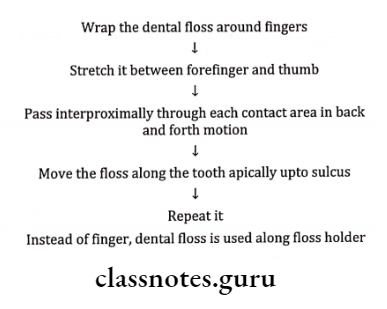
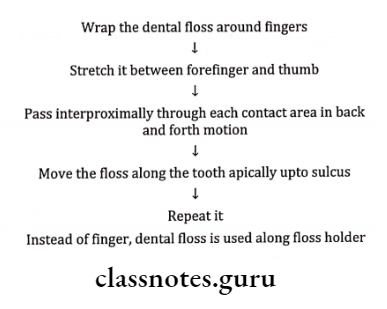
Dental Floss Technique:
Question 21. Disclosing agents.
Answer:
- They are prepared in liquid, tablet, or lozenge form that contains a dye or other coloring agent.
- It is used to identify bacterial plaque deposited for in-construction, evaluation, and research
Disclosing agents Purpose:
- Patient’s education
- Evaluate the effectiveness of the treatment
- Evaluate plaque indices
- Self-evaluation
Disclosing agents Requirements:
- Color should contrast normal color of the oral cavity
- It should not rinse off immediately
- It should not have bad taste
- It should not cause any irritation
- It should be thin enough
Disclosing agents Agents:
- Iodine containing preparations
- Bismarck brown
- Merbromin
- Erythrosin
- Fast green
- Two-tone
Question 22. Atridox
Answer:
- Atridox is 10% Doxycycline
- Atridox is biodegradable
- Used as a mixture in syringes
Atridox Advantages:
- Used in periodontal chemotherapy
- Used as a local drug delivery system
- Used as an adjuvant to mechanotherapy
Plaque Reduction
Question 23. Anticalculus agents.
Answer:
- Calculus control kinds of toothpaste also known as tartar control toothpaste.
- Dentrifices that are widely used as an aid in oral hygiene containing either soluble pyrophosphate or zinc compounds have demonstrated a 10 – 50% reduction in calculus.
- Pyrophosphatase and zinc compounds are thought to produce their anti-calculus effects by absorbing small hydroxy apatite crystals, thus inhibiting growth as larger and more organized crystals.
- The inhibitory effects reduce the deposition of new supragingival calculus but will not affect existing calculus deposits.
- Before starting the use of anti-calculus agents, patients’ teeth must be cleaned & completely free of supragingival calculus to achieve the greatest effect from the toothpaste.