Dental Auxiliaries Definition
Dental Auxiliary
A dental auxiliary is a person who is given responsibility by a dentist so that he or she can help the dentist render dental care but who is not himself/ herself qualified with a dental degree
Denturist
Denturist is a term applied to those dental laboratory technicians who are permitted to fabricate dentures directly for patients without a dentist’s prescription
Expanded Function Dental Auxiliary
An expanded function dental auxiliary is a dental assistant or a dental hygienist in some cases who has received further training in duties related to the direct treatment of patients though still working under the direct supervision of a dentist.
Dental Auxiliaries Important Notes
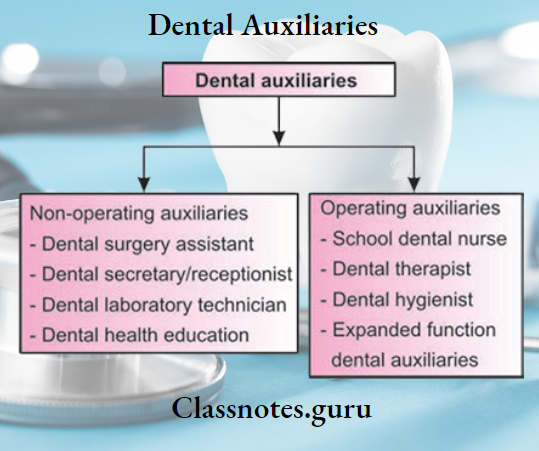
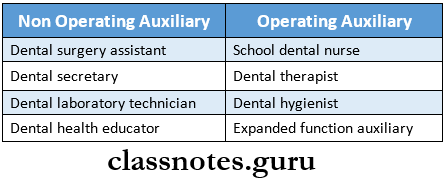
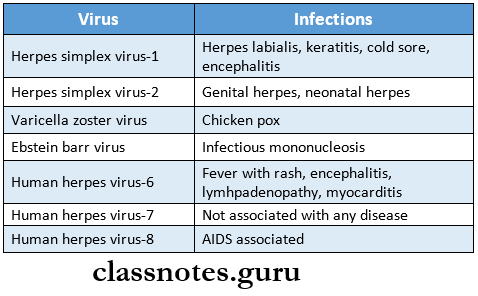
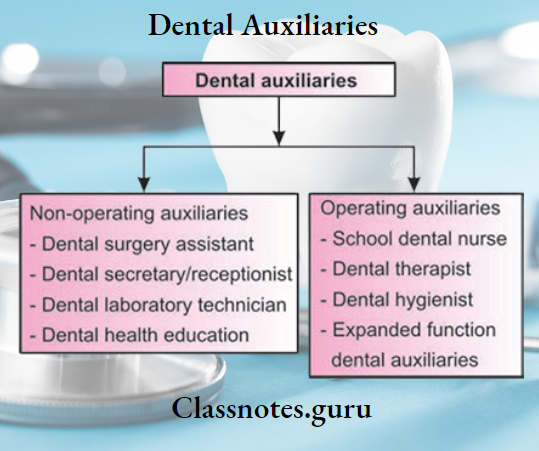
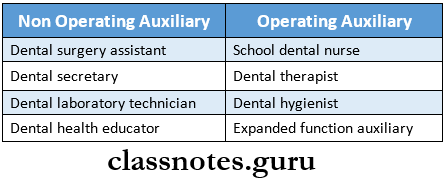
1. Classification Of Dental Auxiliaries
- Non operating
- Dental assistant
- Receptionist
- Dental laboratory technician or denturist
- Dental health educator
- Operating
- Dental nurse
- Dental Therapist
- Dental hygienist
2. Duties Of School Dental Nurse
- Oral examination and oral prophylaxis
- Topical fluoride application and administration of dietary fluoride supplements
- Administration of LA and extraction of teeth
- Dental health education
- Pulp capping and placement of amalgam filling
- Individual patient instruction in tooth brushing
- Patient referral
Read And Learn More: Percentive Communitive Dentistry Question And Answers
3. Four-Handed Dentistry
Four-handed dentistry is the term given to the art of seating both the dentist and the dental assistant in such a way that both are within easy reach of the patient’s mouth
Four-Handed Dentistry Process:
- The patient is in a fully supine position
- The assistant will hand the dentist the particular instrument he wants
- Assistant can also perform functions like retraction or aspiration
Dental Auxiliaries Questions And Answers
Dental Auxiliaries Long Essays
Question 1. Define dental auxiliary. Give classification and functions of dental auxiliaries.
Answer:
Dental Auxiliary Definition:
A dental auxiliary is a person who is given responsibility by a dentist so that he or she can help the dentist render dental care but who is not himself/ herself qualified with a dental degree
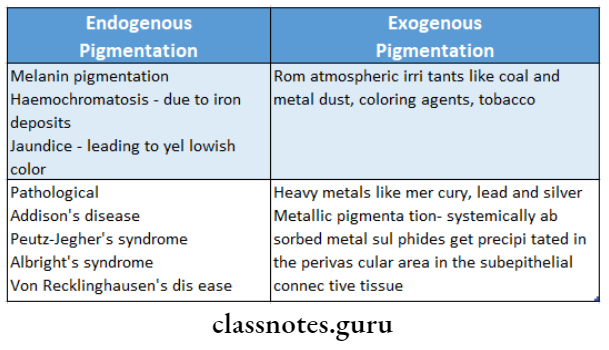
Classification Of Dental Auxiliary:
Dental Auxiliary Non-operating:
- Clinical
- Assists the dentist in his clinical work
- Doesn’t carry out any procedures independently
- Laboratory
- Assists dentist to carry out certain technical laboratory procedures
- Operating auxiliary
- Permit to carry out treatment procedures in the mouth under the direction and supervision of a dentist
Revised Classification:
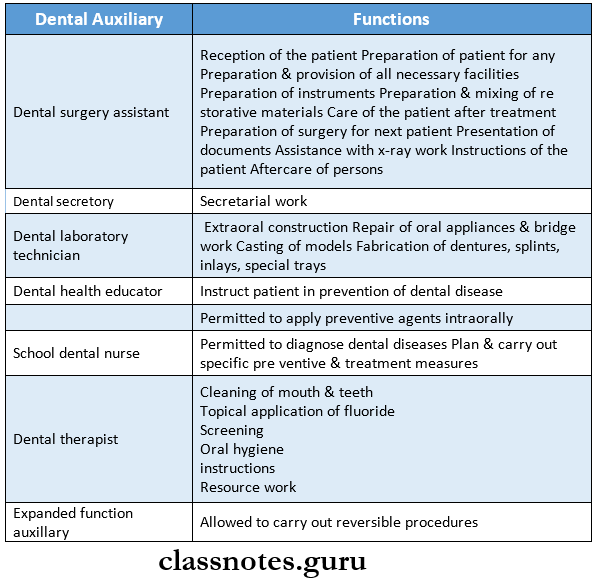
Functions Of Dental Auxillary:
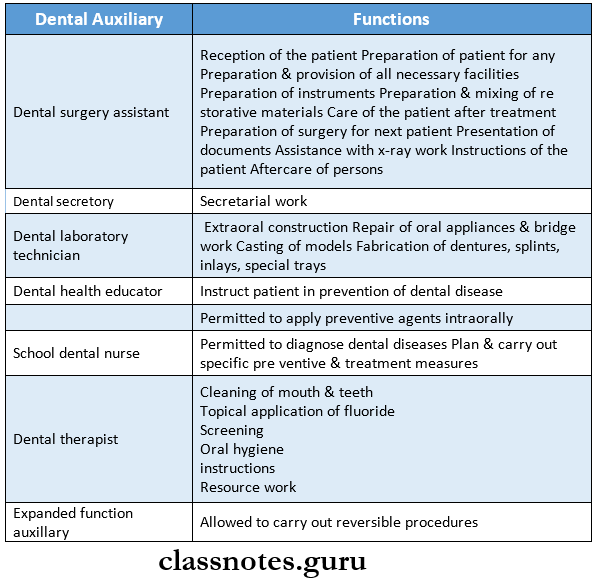
Question 2. Write about the functions of a school dental nurse.
Answer:
School Dental Nurse:
- This is an operating auxiliary who is allowed to diagnose and carry out certain treatment procedures usually in school children
Read And Learn More: Percentive Communitive Dentistry Question And Answers
- She is employed by the government to provide regular dental care to between 450-700 children at nearly 6 monthly intervals
- She is accepted as a member of the school
School Dental Nurse Functions:
- Permitted to diagnose dental diseases
- Plan and carry out specific preventive and treatment measures
School Dental Nurse Duties:
- Oral examination
- Prophylaxis
- Topical fluoride application
- Advice on dietary fluoride supplements
- Administration of local anesthesia
- Cavity preparation and placement of amalgam filling
- Pulp capping
- Extraction of primary teeth
- Oral hygiene instruction
- Health education
- Referral of patients for complex services
Types Of Dental Auxiliaries
Question 3. Explain the New Zealand school dental nurse.
Answer:
New Zealand Dental Nurse:
- The dental nurse scheme was established in Wellington, New Zealand in 1921 due to extensive dental disease
- The man who influenced its formation was T.A.Hunter, a pioneer in the establishment of a dental school in New Zealand
Dental Auxiliaries Short Essays
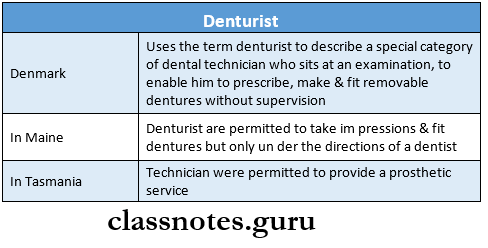
Question 1. Denturist.
Answer:
Denturist
Denturist is a term applied to those dental laboratory technicians who are permitted to fabricate dentures directly for patients without a dentist’s prescription
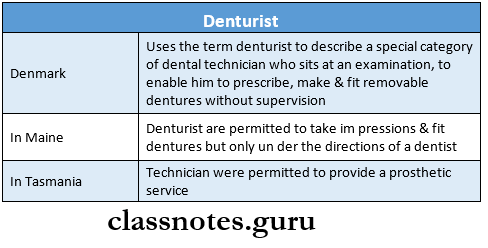
The desire for autonomy among dental laboratory technicians led to the formation of denturists
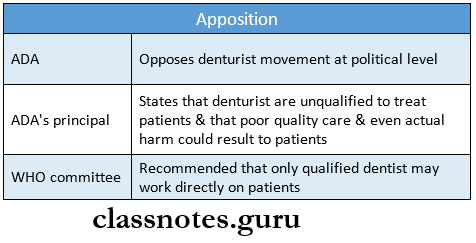
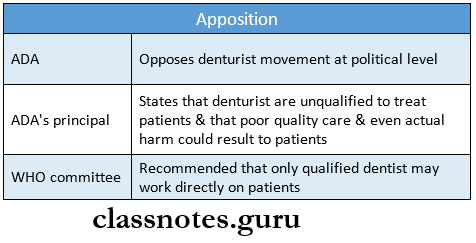
Denturist Opposition:
Question 2. Expanded dental auxiliary.
Answer:
Expanded Dental Auxiliary
- Expanded function dental auxiliary is a dental assistant or a dental hygienist in some cases who has received further training in duties related to the direct treatment of patients though still working under the direct supervision of a dentist
- They are allowed to carry out reversible procedures
- They do not prepare cavities
Expanded Dental Auxiliary Duties:
- Placing and removing rubber dams
- Placing and removing temporary restoration
- Placing and removing matrix bands
- Condensing and carving amalgam restoration
- Placing of acrylic restoration
- Applying the final finish and polish
Expanded Dental Auxiliary Procedure:
- The auxiliary seats a patient
- Performs initial inspection
- Carry out x-ray
- Examines the patient
- Diagnose and carry out a treatment plan
- Gives local anesthesia
- Prepare cavity and insert pulp protective agents
Expanded Dental Auxiliary Functions:
Allowed to carry out reversible procedures
Classification Of Dental Auxiliaries
Question 3. Needs and development of dental personnel.
Answer:
Needs And Development Of Dental Personnel
- With increasing health consciousness the demand for dental care increases among the public
- There was a necessity to make it affordable and available to all
- In order to provide cost-effective services and satisfy demand utilization of some of the paraprofessionals in this field become inevitable
- This personnel receive less training of a shorter duration
- They provide certain limited preventive treatment
- The types of dental personnel in a society are a part of the structure
- It encompasses the various providers of dental care who have different rules, functions, and periods of training and who combine to treat patients
- They assist the dentist in treating the patients
Dental Auxiliaries Short Question And Answers
Question 1. Dental hygienist.
Answer:
Dental Hygienist
- He is a person, not a dentist or a medical practitioner, who does oral prophylaxis, gives instructions in oral hygiene and preventive dentistry, assists the dental surgeon in chairside work, and manages the office
- He shall work under the supervision of the dental surgeon
- The duration of his training is 1-2 years
Dental Hygienist Functions:
- Cleaning of mouth and teeth
- Topical application of fluoride
- Screening
- Oral hygiene instructions
- Resource work
Dental Assistants vs. Dental Hygienists
Question 2. Dental surgery assistant.
Answer:
Dental Surgery Assistant
A dental surgery assistant is a non-operating auxiliary who assists the dentist/ dental hygienist in treating patients but who is not legally permitted to treat patients independently
Dental Surgery Assistant Functions:
- Reception of the patient
- Preparation of the patient for any treatment
- Preparation and provision of all necessary facilities
- Preparation of instruments
- Preparation and mixing of restorative materials
- Care of the patient after treatment
- Preparation of surgery for the next patient
- Presentation of documents
- Assistance with x-ray work
- Instructions of the patient
- Aftercare of persons
Question 3. Expanded dental auxiliary.
Answer:
Expanded Dental Auxiliary
- Expanded function dental auxiliary is a dental assistant or a dental hygienist in some cases who has received further training in duties related to the direct treatment of patients though still working under the direct supervision of a dentist
- They are allowed to carry out reversible procedures
- They do not prepare cavities
Expanded Dental Auxiliary Duties:
- Placing and removing rubber dams
- Placing and removing temporary restoration
- Placing and removing matrix bands
- Condensing and carving amalgam restoration
- Placing of acrylic restoration
- Applying the final finish and polish
Dental Hygienist Responsibilities
Dental Auxiliaries Viva Voce
- The dental laboratory technician is a nonoperating auxiliary
- Dr. Edmund Kells hired the first dental surgery assistant
- The formal training period for dental laboratory technicians is 1 year
- A certified dental assistant gets trained for a period of 8 months
- Mrs. Irene Newman was the first dental hygienist
- The expanded function dental auxiliary in Philadelphia was called technotherapists