Maxillofacial Trauma Important Notes
1. Classification of fracture
- Classification of Fractures of Maxilla:
- Lefort classification
- Lefort 1
- Lefort 2
- Lefort 3
- Erich’s classification Horizontal fracture
- Pyramidal fracture
- Transverse fracture
- Depending to the zygomatic bone
- Sub zygomatic
- Supra zygomatic
- Depending on level
- Low level
- Mid-level
- High level
- Lefort classification
- Classification of Mandibular Fractures:
- General classification
- Simple/closed
- Doesn’t communicate with the exterior
- Compound
- It communicates with exterior
- Comminuted
- Bone is crushed into pieces
- Complex
- Involvement of vital structures
- Impacted
- One fragment driven into other
- Greenstick
- Fracture of one fragment & bending of other
- Pathological
- Superimposition of disease
- Simple/closed
- Completeness
- Complete fracture
- Incomplete fracture
- According to the favourability & direction
- Horizontal favourable fracture
- Horizontal unfavourable fracture
- Vertical favourable fracture
- Vertical unfavourable fracture
- General classification
Read And Learn More: Oral and Maxillofacial Surgery Question and Answers
-
- Kazanjian classification:
- Class 1: When teeth present on both sides of the fracture line
- Class 2: When teeth are present only on one side of the fracture line
- Class 3: When either side of the fracture line is edentulous
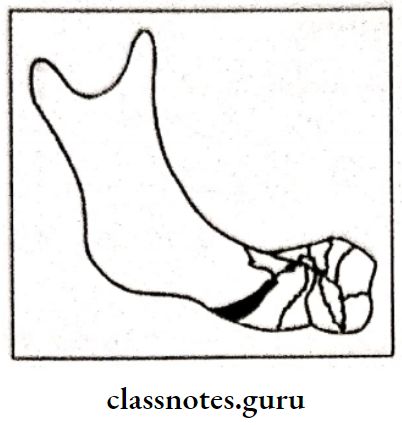
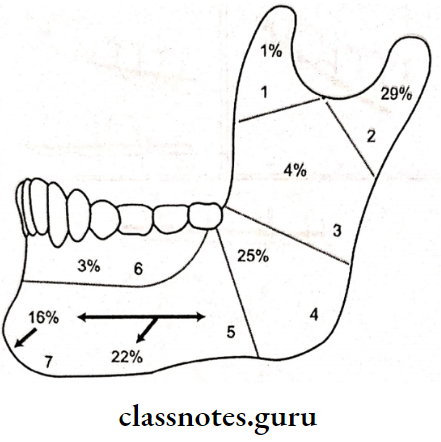
- Anatomical classification:
- Symphysis fracture
- Canine region fracture
- Body fracture
- Fracture of angle
- Fracture of ramus
- Coronoid fracture
- Condylar fracture
- Fracture of dentoalveolar region
- Kazanjian classification:
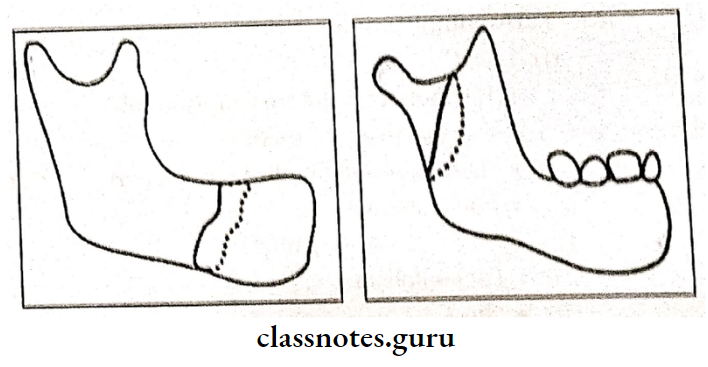
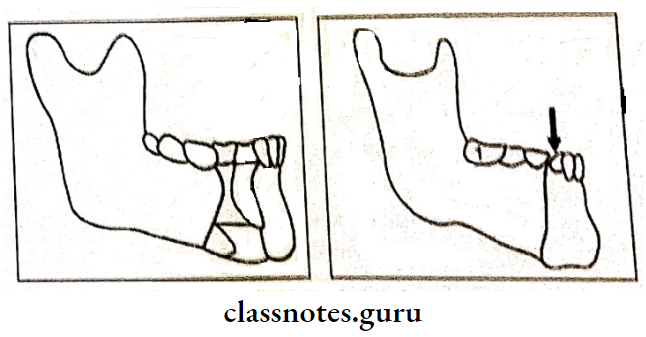
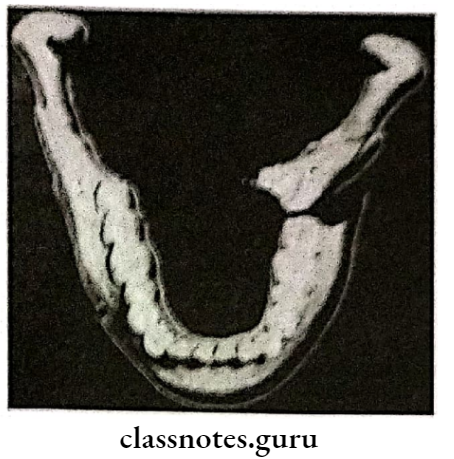
2. Favourable and unfavorable fractures:
- Horizontally favorable fracture: When viewed from side, the fracture line runs from the lower border of the mandible extending upward and backward to meet the upper border
- Horizontally unfavorable fracture: The fracture line extends from the lower border in an upward and forward direction to meet the upper border
- Vertically favorable fracture: When viewed from above the fracture line that runs from buccal plate obliquely backward towards the lingual plate, it will resist medial displacement of the posterior segment
- Vertically unfavorable fracture: If the vertical direction of the fracture line favors the unopposed action of the medial pterygoid muscle, the posterior fragment will be pulled lingually
3. Management of mandibular fractures
- Wiring:
- Essig’s wiring
- Gilmer’s wiring
- Risdon wiring
- Eyelet wiring
- Multiloop wiring
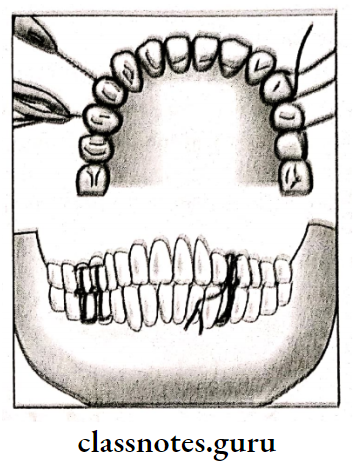
- Arch bar fixation
- Bone plating
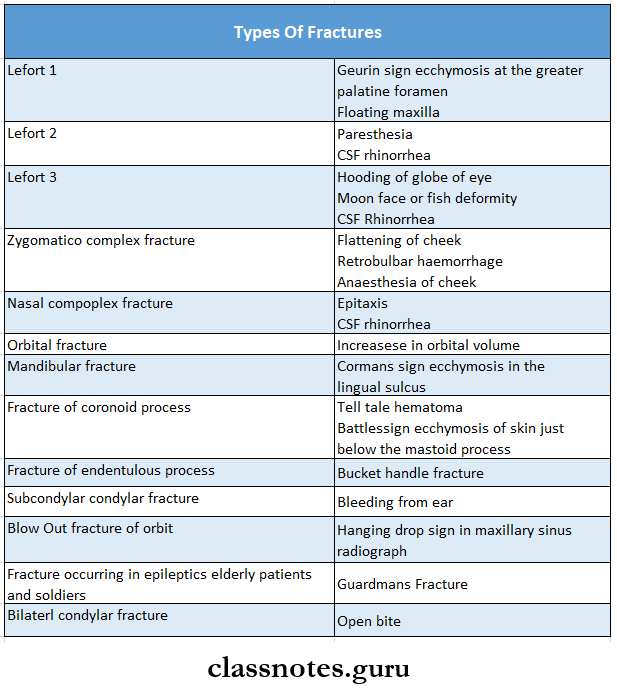
4. Important features of different types of fractures:
5. Methods of immobilization of mandibular fractures:
- Osteosynthesis without IMF
- Intermaxillary fixation
- IMF with osteosynthesis
6. Principles of fracture management:
- Reduction
- Fixation
- Immobilization
7. Line of fracture:
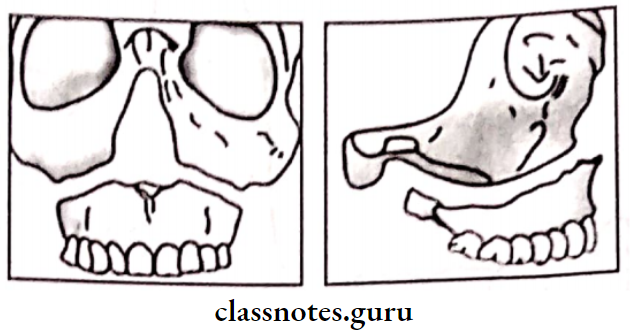
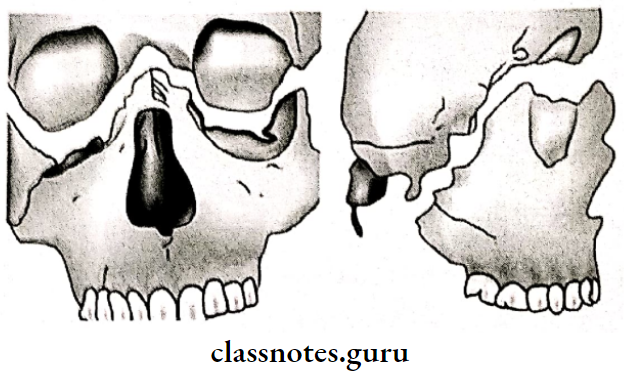
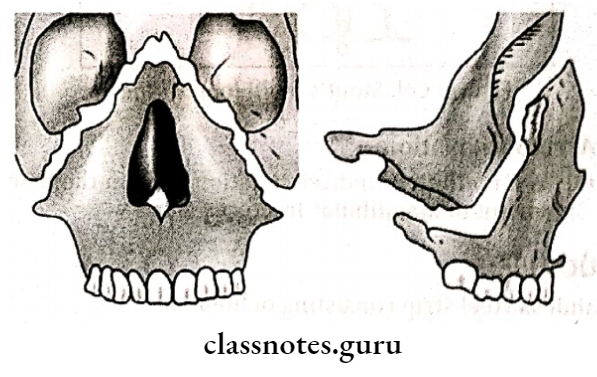
- Lefort 1: Fracture line extends from the nasal septum to the lateral pyriform rims, travels horizontally above the teeth apices runs below the zygomatic buttress and crosses the lower third of the pterygoid laminae
- Lefort 2: The fracture line runs from the middle area of the nasal bone down either side crossing the frontal process of the maxilla into the medial wall of each orbit Within each orbit the line crosses the lacrimal bone behind the lacrimal sac
- Lefort 3: The fracture line extends from the frontonasal suture transversely backward parallel with the base of the skull and involves full depth of the ethmoid bone including the cribriform plate
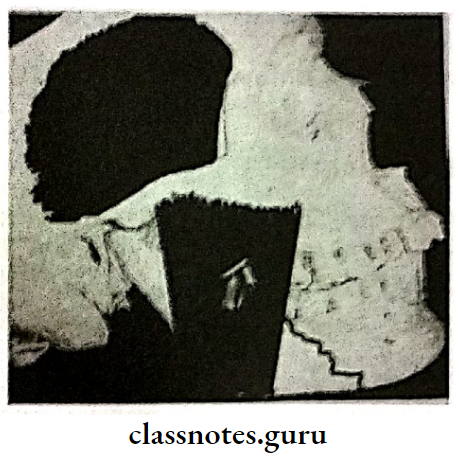
8. Classification of condylar fractures
- General classification:
- Simple fracture
- Compound fracture
- Comminuted fracture
- Lindhal classification:
- Fracture level
- Condylar head fracture
- Condylar neck fracture
- Subcondylar fracture
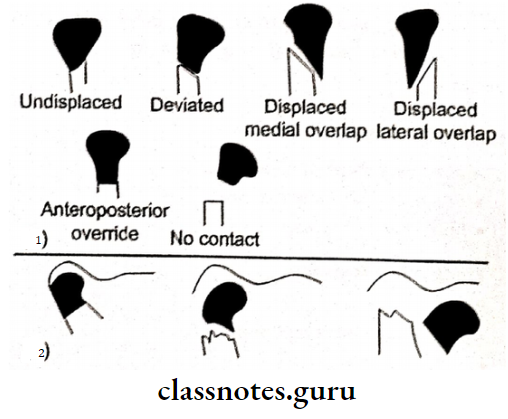
- Relationship of the condyle to ramus:
- Undisplaced
- Deviated
- Displaced with medial overlap
- Displaced with lateral overlap Anteroposterior overlap
- Relationship of condylar head to fossa:
- No displacement
- Displacement
- Injury to meniscus
- Fracture level
- Maclennan classification:
- No displacement
- Deviated
- Displacement
- Dislocation
9. Complications of fractures:
- Early complications:
- Local:
- Haemorrhage- Internal or external
- Damage to vital structures
- Damage to surrounding tissues, nerves or skin
- Haemarthrosis
- Systemic complications:
- Fat embolism
- Shock
- Thromboembolism
- Pneumonia
- Local:
- Late complications
- Local Complications:
- Delayed union
- Non-union
- Malunion
- Myositis ossificans
- Systemic complications:
- Gangrene, tetanus, septicaemia
- Osteoarthritis
- Local Complications:
Maxillofacial Trauma Long Essays
Question 1. Classify fractures of maxilla & mandible. Discuss the management of mandibular fractures. Management And types of Dental Wiring
Answer:
Classification Of Fractures Of Maxilla:
- Lefort classification:
- Lefort I
- Lefort II
- Lefort III
- Erich’s classification:
- Horizontal fracture
- Pyramidal fracture
- Transverse fracture
- Depending to the zygomatic bone:
- Sub zygomatic
- Supra zygomatic
- Depending on level:
- Low level
- Mid level
- High level
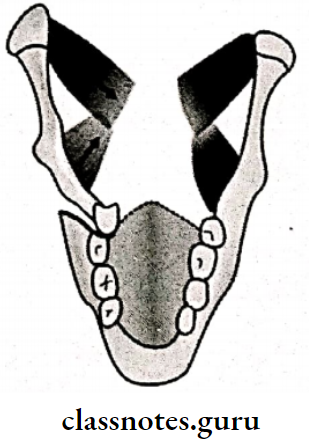
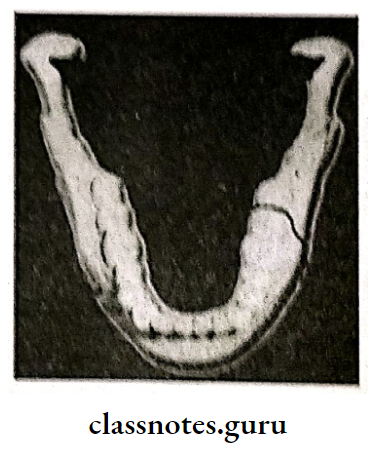
Classification of Mandibular Fractures:
1. General classification:
- Simple/closed: Doesn’t communicate with exterior
- Compound: It communicate with exterior
- Comminuted: Bone is crushed into pieces
- Complex: Involvement of vital structure
- Impacted: One fragment driven into other
- Greenstick: Fracture of omne fragment and bending o other
- Pathological: Superimposition of disease
2. Completeness:
- Complete fracture
- Incomplete fracture
3. According to the favourability & direction:
- Horizontal favorable fracture
- Horizontal unfavorable fracture
- Vertical favorable fracture
- Vertical unfavorable fracture
4. Kazanjian classification:
- Class 1: When teeth present on both sides of the fracture line
- Class 2: When teeth are present only on one side of fracture line
- Class 3: When either side of the fracture line is edentulous
5. Anatomical classification
- Symphysis fracture
- Canine region fracture
- Body fracture
- Fracture of angle
- Fracture of ramus
- Coronoid fracture
- Condylar fracture
- Fracture of dentoalveolar region
Clinical Features Of Fractures Of Maxilla:
- Change in the contour of the face
- Lacerations
- Ecchymosis of the floor of mouth Occlusal disturbances
- Step deformity of the mandible
- Pain & tenderness
- Trismus
- Deviated mouth opening
- Anaesthesia & paraesthesia of the lower lip & chin
Management and types of Dental Wiring:
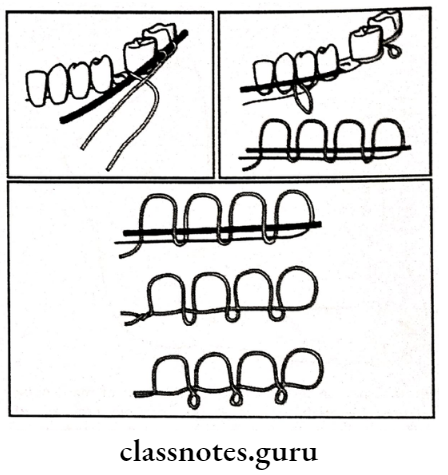
1. Essig’s wiring:
- Used to stabilize dentoalveolar structures
- Steps:
- Move the luxated teeth back to the position
- Adapt wire to the teeth
- Pass the wirws one end buccly and other lingually
- Join both the ends
- Pass small wires Interdentally and fix it
- Twist it cut it and adjust in
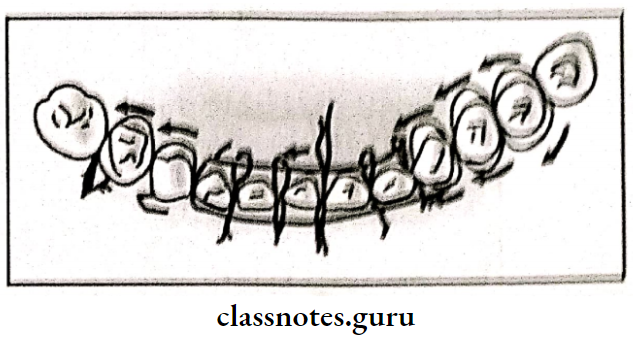
2. Gilmers wiring:
- Pre stretched wire is passed around the individual tooth
- Both ends are brought together & twisted Repeat for each tooth
- Repeat for both the arches
- Final twisting mandibular & maxillary wires
- Twist cut it & adapt interdentally
3. Risdon’s wiring:
- Pass the wire around both the 2nd molar
- Both the ends are twisted together
- Repeat for each tooth
- Both the base wires are brought to the midline
- Twisted together
- Cut it
- Adapt it to the neck of the teeth
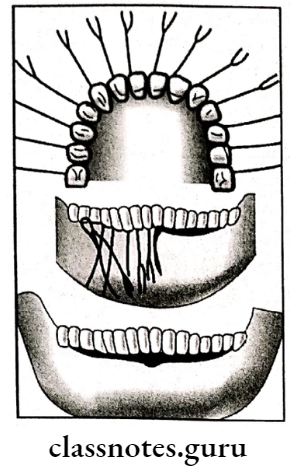
4. Eyelet wiring:
- Prepare loops in the center of wire
- Two tails of the wire are passed interdentally
- One end is passed around distal tooth from lin gually to buccally
- Other end is passed around mesial tooth lingually to buccally
- Twist both the ends
- Cut it short
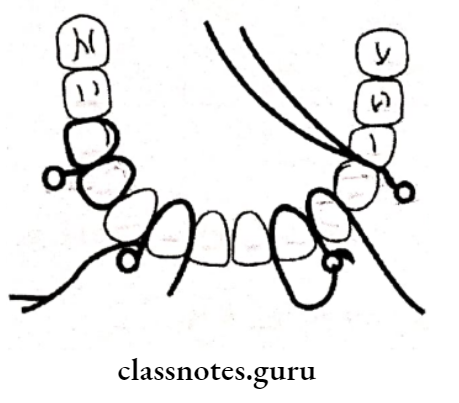
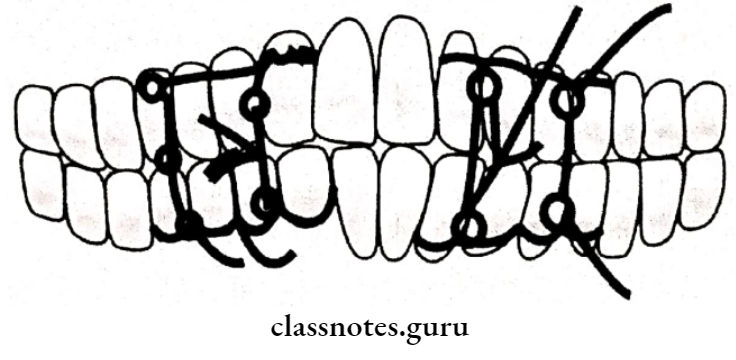
5. Multiloop wiring:
- Adapt solder wire around the buccal surface of the tooth
- Adapt wire buccally from last molar to midline
- Pass the other end distal to the 2nd molar over lingual side
- Pass interdentally bring it to the buccal side by passing under the wire
- Now pass it from buccal to lingual
- Round it around the tooth
- Repeat the same procedure
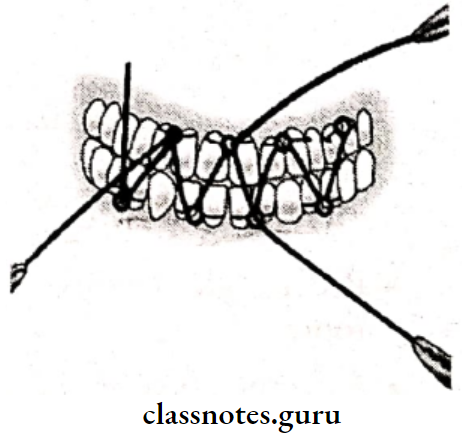
6. Arch Bar Fixation:
It is a method of indirect fixation used in the management of mandibular fractures.
Structure of Arch Bar Fixation:
- Stainless steel strip consisting of hooks
- In upper jaw hooks are located in upward direction
- In lower jaw it is located in downward direction
- It is adapted to the buccal surface
- It is fixed to each tooth with the help of stainless steel wires
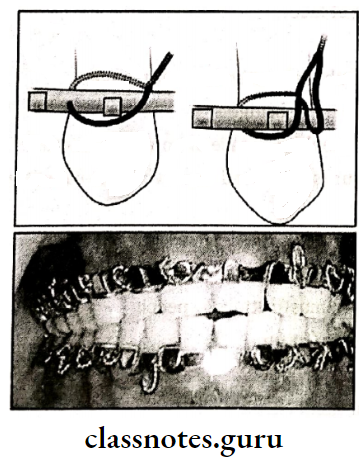
Advantages of Arch Bar Fixation:
- Less traumatic
- Stable appliance
Question 2. Describe clinical features & management of Lefort 1.
Or
Classify fractures of the middle third of the facial skeleton. How would you manage Leforte Fractures?
Or
Lefort 1 fracture And Geurin fracture
Answer:
Lefort 1:
- Clinical Features of Lefort 1:
- Oedema of lower part of face
- Ecchymosis in buccal vestibule
- Bilateral epitaxis
- Mobility of upper teeth
- Disturbed occlusion
- Pain
- Upward displacement of fragment telescopic fracture
- ‘Cracked cup’ sound on percussion of upper teeth
- Guerin sign’ecchymosis in the greater palatine region
Management of Lefort 1:
- Principles:
- Reduction
- Fixation
- Immobilization
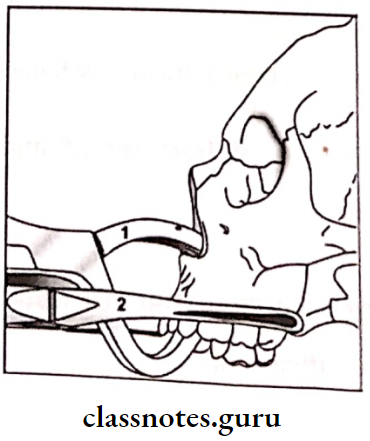
Principles are of Lefort 1:
1. Reduction:
- Reduction of impacted fragment with the help of disimpaction forceps ( Rowe’s & William’s forceps)
- Placement of Rowe’s forcep:
- The straight blade is placed into the nostrils
- A curved blade is placed over the palate
- Placement of William’s forceps: placed over the buccal accept
- Displaces maxilla in mesiodistal direction
2. Fixation:
- Zygomatic suspension fixation is done
- Holes are drilled over the zygomatic arch
- Pass the wire through it
- Bring it up to the arches
- Twisted over are arch bars
3. Inter Maxillary Fixation:
Question 3. Classify zygomatic fractures. Describe about its clinical features & its management.
Or
How to the management of zygomatic fracture and Gillies Temporal Approach.
Answer:
Classification of zygomatic fractures:
- Based on the extent of involvement:
- Fractures involving orbit
- Fractures not involving the orbit
- Zingg classification:
- Type 1:
- Isolated to one component
- Zygomatic arch
- lateral orbital wall
- Inferior orbital rim
- Type 2:
- Involving all four buttresses
- Type 3:
- Complex fractures
- Type 1:
- Based on direction:
- Displacement around a horizontal axis
- Displacement around vertical axis
Clinical Features of zygomatic fractures:
- Flattening of cheek
- Unilateral epistaxis
- Tearing of sinus mucosa causes blood to collect into the sinus cavity
- As the maxillary sinus drains into the middle meatus, unilateral epistaxis occurs
- Circumorbital ecchymosis
- Subconjunctival hemorrhage
- Due to the ability of oxygen to diffuse through conjunctiva to the collected blood under the conjunctiva
- Limitation of ocular movements
- Enophthalmus
- Due to herniation of orbital contents through the fractured walls
- Blurring of vision
- Anesthesia of cheek
- Edema of cheek
- Step deformity
- Limitation of mandibular movements Trismus
- Due to spasm of temporalis by impingement of zygomatic arch fragments on muscle
Management of zygomatic fractures:
- Stable fractures: open reduction
- Unstable fractures open reduction & trans osseous wiring
Operative Technique:
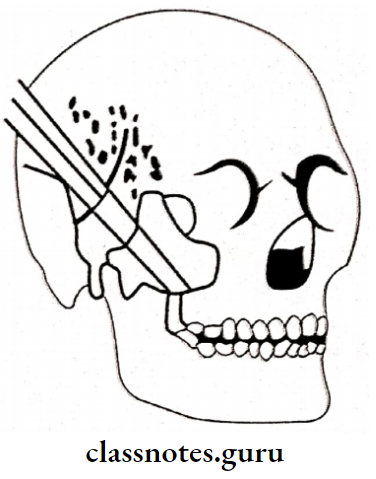
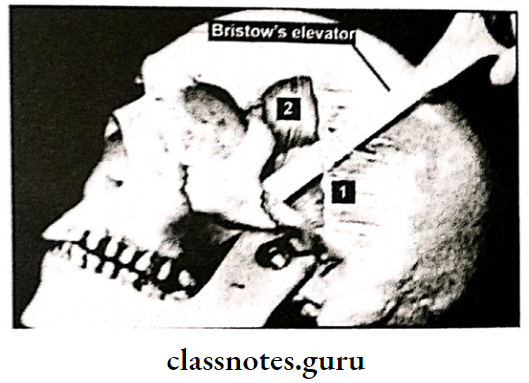
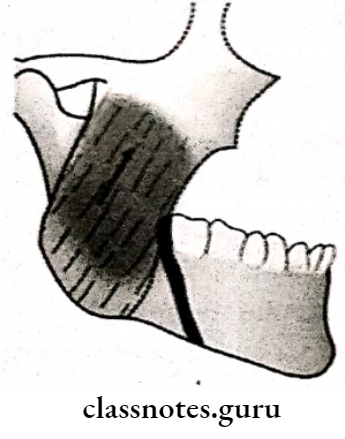
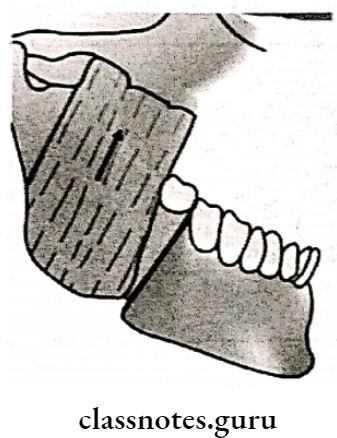
- Gillies Temporal Approach:
- Plugged external auditory meatus with cotton
- Incision given over zygomatic arch as well as temporal area
- Expose temporal fascia
- Insert Bristow’s periosteal elevator above the temporal muscle
- Manipulate it upward, forward & outward
- Reduction is done
- Closure of wound
Question 4. Classify condylar fractures. Describe its clinical features, & its management.
Or
Clinical features & management of condylar
Answer:
Classification of condylar fracture:
1. General classification:
- Simple fracture
- Compound fracture
- Comminuted fracture
2. Lindhal classification:
- Fracture level:
- Condylar head fracture
- Condylar neck fracture
- Subcondylar fracture
- Relationship of the condyle to ramus:
- Undisplaced
- Deviated
- Displaced with medial overlap
- Displaced with lateral overlap
- Anteroposterior overlap
- Relationship of condylar head to fossa:
- No displacement
- Displacement
- Injury to meniscus:
Lindhal’s classification of condylar fracture:
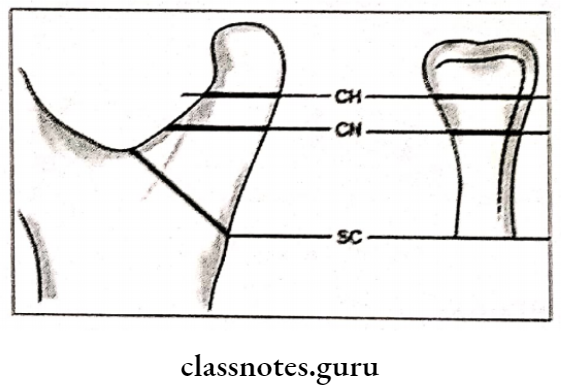
- CH – Condylar head intracapsular fracture
- CN- Condylar neck fracture,
- SC – Subcdylar fracture
3. Maclennan classification:
- No displacement
- Deviated
- Displacement
- Dislocation
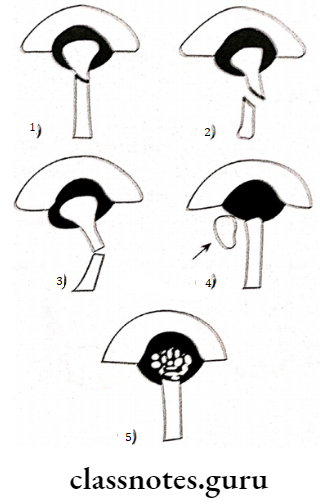
- No displacement
- Displacement
- Deviation
- Dislocation
- Comminution (Multiple fragmentation)
Relation ship of the condylar fragment:
- 1 – To the Mandibular ramus stump
- 2- To the Glenoid fossa
Clinical Features of condylar fracture:
- Abrasion over the fractured area
- Difficulty in mastication
- Laceration over chin
- Facial nerve injury
- Limitation in mouth opening
- Deviation of chin
- Bleeding of external auditory meatus
- Pain
- Lack of condylar movement
- CSF leak
Intraorally of condylar fracture:
-
- Premature contact of molars
- Posterior open bite
- Crossbite
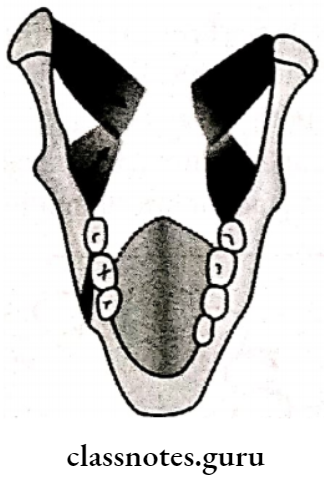
- In bilateral cases: Anterior open bite with posterior gagging” Guardman’s Fracture”
Management of condylar fracture:
- Non-Surgical treatment:
- Restrict the movements
- Restrict the diet to semisolid
- Application of class II elastic traction
- Correction of malocclusion
- IMF for 2-3 weeks
- Surgical treatment:
- Absolute indications:
- Dislocation in middle cranial fossa
- Anterior dislocation
- Bilateral condylar fracture
- Relative indications:
- subcondylar fracture with anterior openbite
- Anterior & medial displacement of the fragment
- Malunited fracture
- Loss of posterior teeth
- Interference with the functions
- Absolute indications:
Question 5. Write diagnosing & management of fracture of angle of the mandible in 40 years old edentulous patient.
Answer:
Diagnosis of fracture :
- Making of impression of upper & lower arches
- Fabrication of cast models
- Study of occlusion through it
- Model surgery is carried out through it
Management of fracture :
- Use of denture for fixation & immobilization of fragment
- The denture can be used as a splint
- Splinting of the denture by circum mandibular wiring
- If dentures are not present
- Impression is taken of upper & lower arches Processing of acrylic baseplates
- Used as denture called
- Gunning Splint
- Processing of archbars into dentures
- Wiring of denture
- Prosthetic incisors are removed to create a hole for feeding purposes

Question 6. Write clinical features & management of Lefort 3
Answer:
Clinical Features of Lefort 3:
- Balloning of face
- Panda facies
- Racoon eyes
- bilateral subconjunctival hemorrhage
- lengthening of face
- Separation of sutures
- ‘Dish face’ deformity
- Enophthalmus
- Diplopia
- Deviation of nasal bridge
- Epitaxis
- CSF rhinorrhoea
Management of lefort 3:
Question 7. Describe the management of unfavorable fractures.
Answer:
Management of unfavorable fractures:
Question 8. Write in short principles of fracture management. Add a note on different modalities for fracture mandible involving teeth in the line of fracture.
Or
Fracture of the body of the mandible in children.
Answer:
Principles Of Fracture Management:
- Reduction:
- Restoration of fractured fragments to their original position
- Brought by
- Closed reduction
- Open reduction
- Fixation:
- Fractured fragments are fixed
- This prevent displacement of the fragments
- Consists of:
- Direct fixation
- Indirect fixation
- Consists of:
- Immobilization:
- Fixation device is retained in position till bony union is obtained
- It depends on type of fracture & bone involve
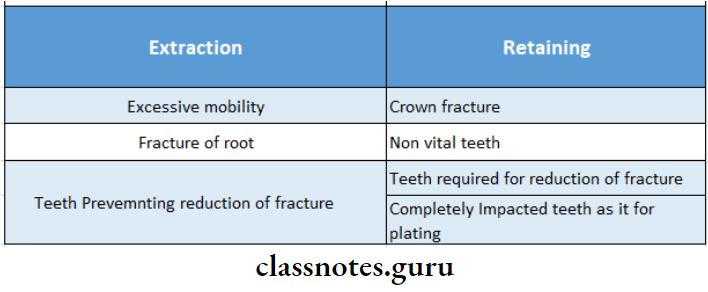
Management Of Fracture Of Mandible Involv- Ing Teeth In The Line Of Fracture:
- Teeth can be extracted or retained
- Indications for them
Maxillofacial Trauma Short Essays
Question 1. Diplopia.
Answer:
Diplopia
- It is a blurred, double vision experienced by the patient
- It can be temporary or permanent
Types of Diplopia:
- Monocular Diplopia:
- Double vision through one eye
- Indicates detached lens or traumatic injury
- Binocular diplopia:
- Blurred through both the eyes
Causes of Diplopia:
- Physical interference:
- Fibrous adhesions Haematoma
- Herniation of periorbital fat
- Functional interference:
- Disturbance to the inferior rectus & inferior oblique muscle
- Neurological causes:
- Paralysis of nerve
- Supranuclear impairment
- Intraorbital damage
- Infranuclear injuries
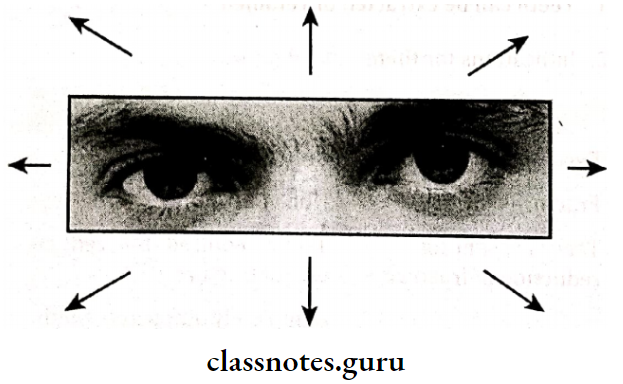
Diagnosis of Diplopia:
1. Testing motions of the eye:
- Hold a pencil at an arm distance from the patient
- Ask the patient in all the 9 direction
- Observe obstruction in any direction if present
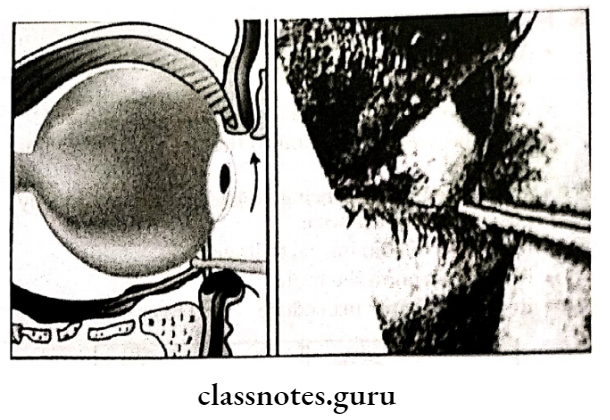
2. Forced duction test:
- Grasp the tendon of inferior rectus through forceps
- Ask the patient to look in all the direction
- Observe any obstruction
3. Hess test:
- Patient’s motions of the eye are recorded over a Hess chart
Question 2. Lefort II fracture/ Pyramidal fracture.
Answer:
Lefort II fracture/ Pyramidal fracture:
Clinical Feature sof Lefort II fracture:
- Gross edema of middle third of the face
- Ballooning of face
- Black eye
- Bilateral subconjunctival hemorrhage
- Depressed nasal bridge
- Anterior open bite in case of impacted fracture
- If the fragment is displaced downward, it causes lengthening of face
- Bilateral epistaxis
- Loss of occlusion
- Difficulty in mastication & speech
- Airway obstruction
- CSF leak
- Paraesthesia of cheek
- Step deformity
Question 3. Splints.
Answer:
Types of Splints:
- Custom made:
- Fabricated for the individual patient
- Indications:
- Failure of wiring Edentulous patient
- Pregnant patients Growing children
- Indications:
- Fabricated for the individual patient
- Acrylic:
- Types: Lateral compression splint
- Steps:
- Make impression
- Fabricate cast
- Mark & cut the fracture line
- Check for occlusion
- Adapt wire to it
- Fabricate the acrylic splint with the help of self cure acrylic
- Gunning splints:
- Modification of dentures in case of edentulous patient
- Fixation:
- In mandibular circumferential wiringalges to athl
- In maxilla pre alveolar wiring
- Fixation:
- Modification of dentures in case of edentulous patient
Question 4. Miniplate osteosynthesis.
Answer:
Miniplate osteosynthesis
Developed by Michelet in 1973
- AIM:
- To attain fracture adaptation
- Application of the plate to the traction side of the bone
- Principle:
- Fixation by stability
- Factors:
- Location of dense cortical bone
- Displacing forces acting on the mandible
Question 5. Favorable & unfavorable fractures.
Answer:
Favourable Fractures:
- It is one in which the fracture lines run in such a way that the forces of the muscles bring the fracture frag ments closer instead of displacing them
- It can be horizontal or vertical depending in the direction they are viewed
- If it is viewed from lateral surface of the mandible, it is horizontal
- If it is viewed from the occlusal surface, it is vertical
Unfavorable Fractures:
- It is one in which the fracture line runs in such a way that the muscle forces tend to displace the fragments away from each other
- It can also be horizontal or vertical depending in the direction they are viewed
- If it is viewed from the lateral surface of the mandible, it is horizontal
- If it is viewed from the occlusal surface, it is vertical
Question 6. Pathological fractures.
Answer:
Pathological fractures
Occurring due to underlying disease
- Tumors:
- Giant cell tumor
- Bone cysts
- Infections:
- Acute osteomyelitis
- Metabolic bone diseases:
- Hyperparathyroidism
- Osteoporosis
- Paget’s disease
Question 7. Wire osteosynthesis.
Answer:
Wire osteosynthesis
It is nonrigid method of fixation
Technique of Wire osteosynthesis:
- Drilling of holes on either side of the fracture line
- Passing wire through each hole
- Prevent damage to nerves
- Bring both ends of the wires to the buccal surface
- Twist them together
- Cut & tuck them
- Irrigate the wound
- Retain the wires permanently
- IMF done
Question 8. Nonunion.
Answer:
Nonunion
Lack of bony fusion of fractured ends
- Etiology of Nonunion:
- Inadequate fixation
- Infection of the fracture
- Lack of adequate blood supply
- Excessive periosteal stripping
- Pathological fractures
- Features of Nonunion:
- Pain
- Difficulty in occlusion
- Difficulty in mastication
- Abnormality mobility of fractured fragments
- Radiological Feature:
- The gap between the fragments
- Management of Nonunion:
- Expose the site
- Graft the space
- Stabilize the fractured ends
- Fixation
- Immobilization
Question 9. Complications of fracture.
Answer:
1. Early complications:
- Local:
- Hemorrhage- Internal or external
- Damage to vital structures
- Damage to surrounding tissues, nerves or skin
- Haemarthrosis
- Systemic complications:
- Fat embolism:
- Features
- Sudden onset dyspnoea
- Hypoxia
- Fever
- Confusion, coma, convulsions
- Translent red-brown petechial rash affecting
- Shock
- Thromboembolism
- Pneumonia
- Fat embolism:
2. Late complications:
- Local complications:
- Delayed union
- Non-union
- When no signs of healing occur after 3-6 months it is called non-union
- Features:
- Pain at the fracture site
- Non-use of extremity
- Tenderness and swelling
- Joint stiffness
- Malunion:
- Myositis ossificans:
- Calcifications and bony masses develop within the muscle
- Presents as pain, tenderness, focal swelling, and joint/muscle contractions
- Systemic complications:
- Gangrene, tetanus, septicaemia
- Osteoarthritis
Maxillofacial Trauma Short Question And Answers
Question 1. Cap splint.
Answer:
Uses of Cap Splint:
- Fixation of fractures
- Fracture of the mandible in children
- Fracture of the edentulous mandible
Technique of :
- Impression of upper & lower arches
- Fabrication of cast & splint
- Reduction of fragments
- The casting of the splint
- Cementation of splint over occlusal surfaces of teeth
Question 2. Battle’s sign.
Answer:
Battle’s sign
- Location: Mastoid region
- Cause: Condylar fracture
- Feature: Ecchymosis in the pre-auricular region
Question 3. Bone plate.
Answer:
Bone plate
- The semirigid type of fixation
- Depending on the fracture bone plates are fixed
The technique of Bone plate:
- Incision
- Exposure of fracture site
- Reduction of fracture
- Adaptation of bone plates
- Fixation with the help of screws
Question 4. Subconjunctival ecchymosis.
Answer:
Subconjunctival ecchymosis
- Fracture of orbital walls
- Subperiosteal hemorrhage
- Destruction of the periosteum of orbit
- Leads to subconjunctival hemorrhage
- Appears bright red in color due to the diffusion of oxygen
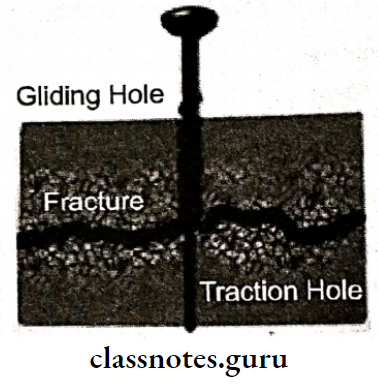
Question 5. Lag screw.
Answer:
Lag screw
- Introduced by Brons & Boring in 1970
- It is a long screw driven into both sides of the fractured bone
Mechanism of Lag screw:
- As the screw is tightened, fractured ends are brought together
- Thus closes the space between them
The technique of Lag screw:
- Drilling of gliding hole in the proximal fragment
- Drilling of traction hole in distal fragment
- Engaging screw
- Tightening it
- Results in pulling of distal fragment through threads & proximal fragment by screw head
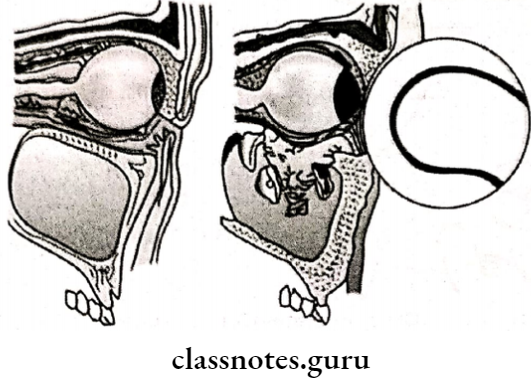
Question 6. Blow-out fracture.
Answer:
Blow-out fracture
Occurs when the object of diameter greater than the diameter of the object strikes
Pathogenesis of Blow – out fracture:
- Fracture of the floor of the orbit
- Herniation of fat into antral cavity Increase in orbital volume
- Enophthalmos
Features of Blow – out fracture:
- Enophthalmos
- Entrapment of muscles of orbit
- Restricted movement of orbit
- Diplopia
- Subconjunctival hemorrhage
- Paraesthesia
- Circumorbital edema
- Ecchymosis
Question 7. Dento alveolar fractures.
Answer :
Features of Dento alveolar:
- Mobility of dentoalveolar segment
- Subluxation on avulsion of teeth
- Splitting of teeth
- Occlusal derangement
- Laceration of gingiva
Management of Dento alveolar:
- Reduction of segment Occlusion correction
- Stabilizing with wiring
- Soft diet for 3 weeks
Question 8. Enophthalmos.
Answer:
Enophthalmos
It is inward sinking of the eye
Causes of Enophthalmos:
- Decrease in the orbital volume due to herniation of orbital fat
- Increase in bony orbit due to fracture of its walls
- Loss of ligament
- Post traumatic fibrosis
- Combination of above
Clinical Features of Enophthalmos:
- Hooding of upper eyelid
- Anterior projection of globe
Treatment of Enophthalmos:
- Surgical intervention
- Placing materials behind the globe
Question 9. Gunshot injuries.
Answer:
Gunshot injuries
These are penetrating wounds
Classification of Gunshot injuries:
- Penetrating wounds: missile is retained in wound
- Perforating wounds: Missile exits from another wound
- Avulsive wound: Large amount of structure is destroyed
Etiology of Gunshot injuries:
- High velocity bullets
- Low velocity projectiles
Question 10. Geurin’s sign.
Answer:
Geurin’s sign
- Location: In the region of greater palatine foramen
- Cause: Lefort 1 fracture
- Feature: Ecchymosis in the greater palatine foramen
Question 11. Coleman’s sign.
Answer:
Coleman’s sign
- Location: Floor of the mouth
- Cause:
- Blow in the chin
- Base of skull fracture
- Mandibular fracture
- Feature: Ecchymosis in the floor of the mouth
Question 12. Black eye.
Answer:
Black eye
Feature of Lefort II fracture
- Appearance of Black eye:
- Presence of bilateral circumorbital edema
- Presense of bilateral circumorbital ecchymosis
- Diagnosis of Black eye: Difficult due to rapid development of swelling of eyelids
Question 13. Gunning splints.
Answer:
Gunning splints
Gunning splints are retained in position by circumfer ential wiring or by peralveolar wiring,
- Indication of Gunning splints:
- Fracture of edentulous mandible
- Contraindications of Gunning splints:
- Unfavourable fracture lying outside the denture bear- ing area
- Severe fracture displacement
- Construction of Gunning splints:
- Upper and lower impressions are made
- Casts are poured
- Upper and lower base plates are adapted
- Bite blocks are prepared only in posterior resgion
- Hooks are incorporated over buccal side of the blocks Grooves are made over canine region to prevent the peralveolar and circumferential wires from slipping along the surface of the splint
Question 14. Epistaxis.
Answer:
Epistaxis
It is defined as bleeding from the nose
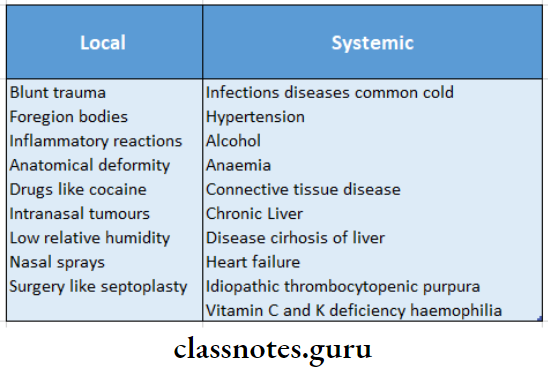
Causes of Epitaxis:
Maxillofacial Trauma Viva Voce
- The most common site of fracture of the mandible is the angle
- The Lefort I fracture is a transverse fracture of the maxilla
- Dish face deformity is commonly seen with a fracture of the middle third of face
- Fractures of the coronoid process can occur due to reflex muscular contraction
- The optimum length of the screw for fixation of the plate in the mandible is 4 mm
- The contraindication to miniplate along the line of osteosynthesis would be a fracture in a 10 years old
- Glasgow coma scale is used to ascertain level of consciousness
- The best radiographic view for examination of fracture of the middle face is Water’s view
- Geurin sign is the presence of ecchymosis at the greater palatine foramen area
- The golden hour of trauma refers to the period of time exactly one hour after the trauma is sustained
- Corman’s sign is ecchymosis in the lingual sulcus
- Verill’s sign includes eyelid ptosis, blurring of vision, and slurring of speech
- The inferior dental nerve is frequently damaged in fractures of the body and the angle of the mandible
- Lefort I fractures mainly involves the tooth-bearing area of the maxilla
- Lefort II involves maxilla, nasal and lacrimal bones
- Lefort III involves maxilla, lacrimal, nasal and ethamoidal bones
- The maxillary incisor region is a common site of dental fractures
- Cracked pot sound on percussion is seen in alveolar fractures
- Lag screws are used to immobilize oblique fractures
- The use of acrylic cap splints with circumferential wiring is best method to treat mandibular fractures in children.
