Diseases Of The Nervous System Important Notes
- Nerve Injuries
- Neuropraxia
- It is a temporary physiological paralysis of nerve conduction
- Recovery is complete
- There is no reaction of degeneration
- Axonotmesis
- It is the division of nerve fibers or axons with intact nerve sheath
- There is the reaction of degeneration distal with near-complete recovery
- Features – sensory loss. Paralysis of muscles or causalgia
- Neurotmesis
- Complete division of nerve fibers with sheath occurs
- Degeneration occurs proximal up to the first node of Ranvier
- Recovery is incomplete
- Neuropraxia
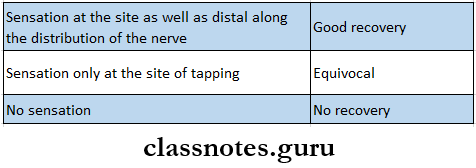
- Tinel’s Sign
- Used to assess the level of regeneration
- Done by tapping over the course of the nerve from the distal to the proximal end to elicit a sensation
- Result
- Commonly Used Tendon Grafts Are
- Palmaris tendon in the forearm
- Plantaris tendon in leg
- Trigeminal Neuralgia
- It is a sudden, severe, brief, stabbing, recurrent pain along the distribution of the trigeminal nerve
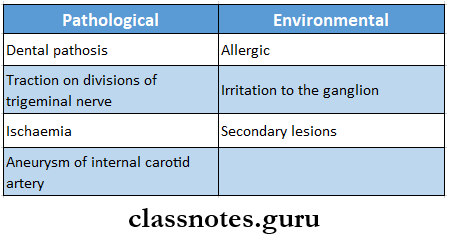
- Trigeminal Neuralgia Etiology:
- Pathological
- Dental pathosis
- Traction on division of trigeminal nerve
- Ischaemia
- Aneurysm of internal carotid artery
- Trigeminal Neuralgia Environmental
- Allergic
- Irritation to the ganglion
- Secondary lesions
Diseases of the nervous system questions and answers
Read And Learn More: General Surgery Question and Answers
- Trigeminal Neuralgia Trigger zones
- Vermillion border of the lip
- Around eyes
- Ala of nose
- Trigeminal Neuralgia Management
- Medical
- Carbamazepine – 100 mg twice daily
- Dilantin – 300-400 mg
- Gabapentin – 11200 -3600 mg/day
- Baclofen – 10 mg T1D
- Surgical
- Injection of alcohol in gasserian ganglion
- Nerve avulsion
- Electrocoagulation of gasserian ganglion
- Medical
- Trigeminal Neuralgia Trigger zones
Diseases Of The Nervous System Short Essays
Question 1. Bell’s Palsy
Answer:
Bell’s Palsy
Idiopathic paralysis of the facial nerve of sudden onset
Bell’s Palsy Etiology:
- 5 Hypothesis:
- Rheumatic
- Cold
- Ischaemia
- Immunological
- Viral
Bell’s Palsy Clinical Features:
- Pain in post auricular region
- Sudden onset
- Unilateral loss of function
- Loss of facial expression
- Absence of wrinkling
- Inability to close the eve
- Watering of eve
- Inability to blow the cheek
- Obliteration of nasolabial fold
- Loss of taste sensation
- Hyperacusis
- Slurring of speech
Bell’s Palsy Management:
- Physiotherapy:
- Facial exercises
- Massaging
- Electrical stimulation
- Protection to eye
- Covering of eye with bandage
- Medical management
- Prednisolone – 60-80 mg per day
- 3 tablets for 1st 4 days
- 2 tablets for 2nd 4 days
- 1 tablet for 3rd 4 days
- Surgical treatment
- Nerve decompression
- Nerve grafting
- Prednisolone – 60-80 mg per day
Neurological diseases questions and answers
Question 2. Trigeminal Neuralgia
Answer:
Trigeminal Neuralgia Definition: It is a sudden, severe, brief, stabbing, recurrent pain along the distribution of the trigeminal nerve
Trigeminal Neuralgia Etiology
Trigeminal Neuralgia Clinical Features:
- Age: Around 35 years
- Sex: Common in female
- Site: Right lower portion of the face, usually unilateral
- Duration: a few seconds to a few minutes
- As time passes duration between the cycles decreases
- Nature: stabbing or lancinating
- Aggravating factors: activation of Trigger Zones
- These are the vermillion border of the lip, around the eyes, and the nose
- Interference with other activities:
- The patient avoids shaving, washing face, chewing, and brushing, as these may aggravate pain
- These lead to a poor lifestyle
- Extreme cases: leads to “Frozen Or Mask Like Face”
Trigeminal Neuralgia Management:
- Medical:
- Carbamazepine: initial dose: 100mg twice daily until relief is achieved
- Dilantin: 300-400mg in single or divided doses
- Gabapentin: 11200-3600 mg/day TID/QID
- Baclofen: 10 mg TID
- Amitryptaline: 25-75 mg/ day QID
- Combination therapy: dilantin + carbamazepine
- Surgical
- Injection of alcohol in gasserian ganglion
- Nerve avulsion: performed on lingual, buccal, or mental
- nerve
- Part of the nerve is sectioned
- Electrocoagulation of gasserian ganglion: diathermy is done
Question 3. Electrocoagulation of Trigeminal ganglion
Answer:
Electrocoagulation Of Trigeminal Ganglion
- Electrocoagulation of the Trigeminal ganglion refers to percutaneous heat ablation of the Gasserian ganglion at the base of the skull
- It is performed by placing a needle into the ganglion through which an electrical current passes, heating the probe and producing a thermal lesion in the ganglion
Electrocoagulation Of Trigeminal Ganglion Side Effects:
- Facial numbness- mild to severe
- It may be temporary
Electrocoagulation Of Trigeminal Ganglion Complications:
- Unintended nerve damage
- Failure to access the Trigeminal nerve or Gasserian ganglion
- Bleeding from the puncture site
- Apnoea
Central nervous system diseases MCQs with answers
Question 4. Nerve grafting
Answer:
Nerve Grafting
Nerve grafting is defined as the replacement of a damaged nerve with a section of a healthy nerve that has been removed from another part of the body
Nerve Grafting Indication: When nerve suturing is impossible or undesirable
Nerve Grafting Ideal Requirements:
- Should be immunologically acceptable
- Should undergo Wallerian degeneration
- Should contain active nerve cells
- Should become vascularised after being placed in a favorable nourished bed
Nerve Grafting Donor Sites:
- The saphenous nerve of the thigh
- The sural nerve of the leg
- The medial cutaneous nerve of the forearm
Question 5. Neuropraxia
Answer:
Neuropraxia
Neuropraxia is the mildest type of peripheral nerve injury
Neuropraxia Features
- No organic damage
- Endoneurium, perineurium, and epineurium are intact a Temporary physiological paralysis of conduction through the intact nerve fibers
- No Wallerian degeneration
- There may be sensory loss or weakness of muscle groups
- Recovery is complete and requires hours to a few weeks
- EMG shows a lack of fibrillation
Question 6. Neurotmesis
Answer:
Neurotmesis
- In Neurotmesis there is partial or complete division of the nerve fibers as well as their sheaths
- Partial lesion produces lateral neuroma while complete division produces terminal neuroma.
Neurotmesis Clinical Features:
- In the proximal segment of the divided nerve:
- Retrograde degeneration up to the first node of Ranvier
- Distal ends of the axons move downwards
- The gap between the divided nerve ends gets replaced by organic clots and fibrous tissue
- In the distal segment of the divided nerve:
- Wallerian degeneration of axons occurs
- Schwan cells proliferate to form small bulb-like projection
Neurotmesis Treatment:
- Primary nerve repair
- Done in clean incised wounds when presented within 6 hours of injury
- It is immediate suturing of the nerve
- Secondary nerve repair
- Done in untidy contaminated wounds presented after 6 hours of injury
- In it, suturing is delayed for 3-4 hours
Nervous system pathology questions and answers
Question 7. Axonotmesis
Answer:
Axonotmesis
In axonotmesis, there is a rupture of nerve fibers or axons within intact sheaths
Axonotmesis Features:
- Wallerian degeneration occurs in the distal portion of the broken axons
- Loss of sensation, tone, and power of the muscles
- There is no nerve conduction distal to the site of injury
- EMG shows fibrillation potential and positive sharp waves
- Area of anesthesia and paralysis of muscles will be restricted to those structures which are supplied by the damaged nerve
- Secondary effects
- Impaired circulation due to disuse
- The affected portion is cold and blue
- Trophic changes occur
- Affected muscles no longer respond to stimulation
Axonotmesis Treatment:
- Maintain good nutrition
- Exercise of the paralyzed muscles
- Encouragement of the patients
- Axonal regeneration occurs without any surgical treatment.
Question 8. Types of nerve injuries
Answer:
Seddon’s Classification:
- Neuropraxia:
- Results from mild insult to nerve
- No axon degeneration occurs
- Mild paraesthesia present
- Axonotmesis
- Severe injury
- Degeneration of afferent fibers
- Severe paraesthesia present
- Neurotmesis
- Most severe injury of the nerve
- Complete destruction of nerve structure
Sunderland’s Classification:
- First-degree injury
- Type 1
- Mild compression of the nerve trunk
- Results in ischemia and conduction block
- No axonal degeneration
- Recovery within a day
- Type 2
- Moderate compression
- Results in edema and conduction block
- Recovery within 1-2 days
- Type 3
- Severe compression
- Disruption of myelin sheath
- Sensory loss
- Recovery in 1-2 months
- Type 1
- Second-degree nerve injury
- Synonymous to Seddon’saxonotmesis
- Axonal damage occurs
- Epineurium, perineurium and endoneu- rium is intact
- Paraesthesia and anaesthesia present
- Spontaneous recovery
- Third-degree nerve injury
- Synonymous to Seddon’s axonotmesis
- Axonal damage
- Damage to epineurium
- Paraesthesia and anaesthesia present
- Regeneration of axon is blocked
- Incomplete sensory recovery
- Surgical repair needed
- Fourth-degree nerve injury
- Synonymous to Seddon’saxonotmesis
- Damage to epineurium, endoneurium and axons
- Intact epineurium
- Sensory impairment
- Poor recovery
- Surgical intervention needed
- Fifth-degree nerve injury
- No conduction of impulses
- Even epineurium is destroyed
- Poor prognosis
Question 9. Facial nerve palsy
Answer:
Facial Nerve Palsy Etiology:
- Congenital
- Traumatic
- Infections
- Inflammation
- Neoplastic
- Idiopathic
Facial Nerve Palsy Clinical Features:
- Unable to raise eyebrows
- Unable to blow cheeks
- Expressionless face
- Absence of wrinkling and Absence of function of the mandibular nerve
- Lack of movement of the upper lip
- Unable to close one eye
- Absence of nasolabial fold
- Absence of taste sensation
- Drooling of the lower lip on the affected side
Common nervous system disorders questions
Question 10. Frey’s syndrome
Answer:
Frey’s Syndrome
This is auriculotemporal nerve syndrom
Frey’s Syndrome Causes: Iatrogenic causes- followed by parotidectomy
Frey’s Syndrome Features:
- Pain in auriculotemporal nerve distribution
- Gustatory sweating
- Flushing on the affected side
Frey’s Syndrome Diagnosis: Positive starch iodine test
Frey’s Syndrome Treatment:
- Topical application of anticholinergic
- Radiation therapy
- Surgical procedures
- Skin excision
- Nerve section
- Tympanic neurectomy
Nervous system short and long questions
Question 11. Horner’s syndrome
Answer:
Horner’s Syndrome
Homer’s syndrome is a clinical syndrome caused by damage to the sympathetic nervous system
Horner’s Syndrome Clinical Features:
- The affected part of the face shows:
- Ptosis
- Anhydrosis
- Dilation lag
- Enophthalmos
- Loss of ciliospinal reflex
- Bloodshot conjunctiva
Horner’s Syndrome Diagnosis:
- Cocaine drop test
- Cocaine eyedrops block tire reuptake of noradrenaline resulting in the dilation of a normal pupil
- In Horner’s syndrome, the pupil fails to dilate
- Paredrine test
- Helps to localize the cause of miosis
- Dilation lag test
Question 12. Branches of the facial nerve
Answer:
Branches Of The Facial Nerve
- Within the Facial Canal
- Greater petrosal nerve
- Nerve to stapedius
- Chorda tympani nerve
- At Its Exit From Stylomastoid Foramen
- Posterior auricular
- Digastric
- Stylohyoid
- Terminal Branches
- Temporal
- Zygomatic
- Buccal
- Marginal mandibular
- Cervical
- Communicating Branches With Adjacent Cranial And Spinal Nerve
Diseases Of The Nervous System Viva Voce
- Tinel’s sign is used to assess the level of regeneration
- Cut the end of nerve forms neuroma proximally and glioma distally
- Causalgia is a burning sensation in the distribution of a peripheral nerve
- Carpel tunnel syndrome is the compression neuropathy of the median nerve in the carpus
- Tendon is the continuity of muscle
