Protozoans Important Notes
1. Entamoeba Histolytica
- Occurs in three forms
- Trophozoites
- Pre cystic stage
- Cyst
- It passes its life cycle only in man
- Diseases caused by it
- Intestinal amoebiasis
- Extra intestinal amoebiasis
- Other Entamoeba are
- Entamoeba coli
- Entamoeba gingivalis
Read And Learn More: Microbiology Question and Answers
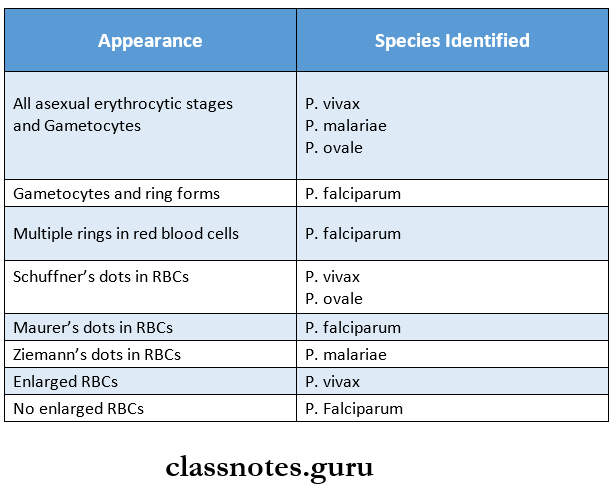
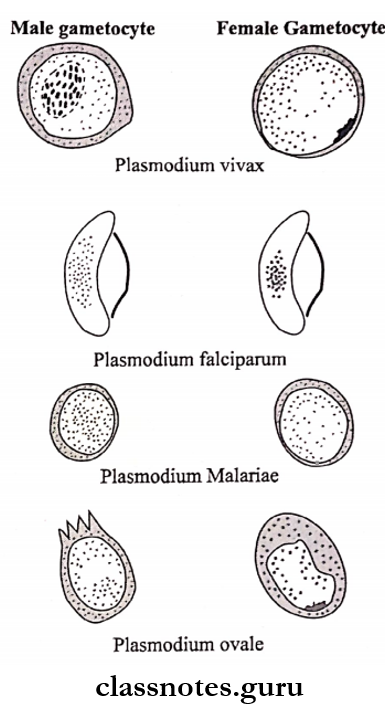
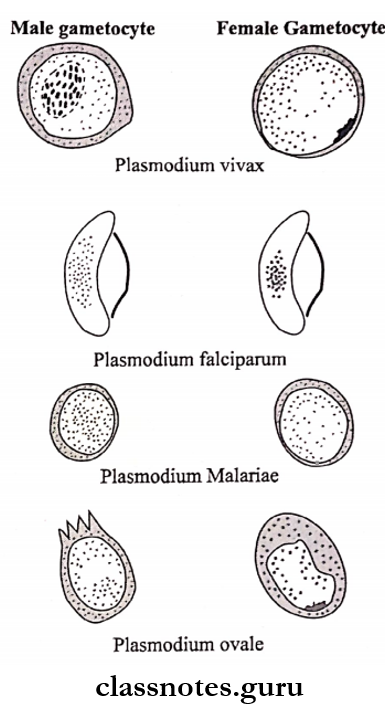
2. Species Of Plasmodium
- Pvivax
- P falciparum
- P malariae
- P ovale
3. Stages Of The Life Cycle Of Plasmodium
- Pre-erythrocytic schizogony
- Erythrocytic schizogony
- Gametogony
- Exo-erythrocytic schizogony
Protozoans and Virology Short Essay Questions with Answers
4. Malarial Pigment
- Yellowish brown – P. vivax
- Dark brown – P.falciparum, P.malariae
- Dark yellowish brown- P. ovale
5. Malaria
- Malaria Clinical Features
- Febrile paroxysm
- Anaemia
- Splenomegaly
- Malaria Complications
- Pernicious malaria
- Blackwater fever
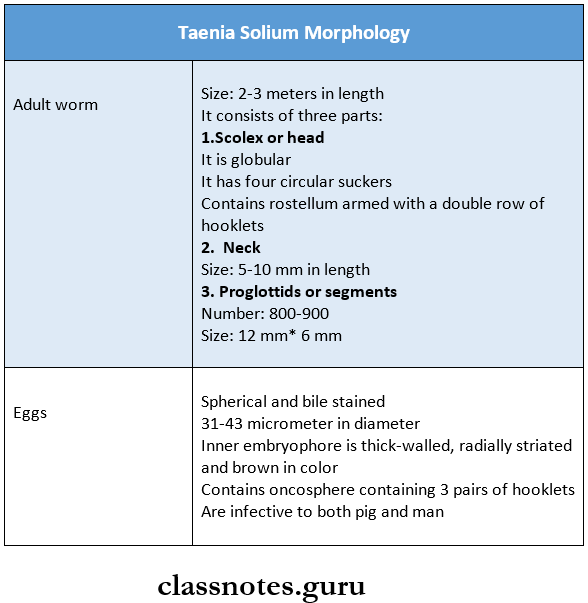
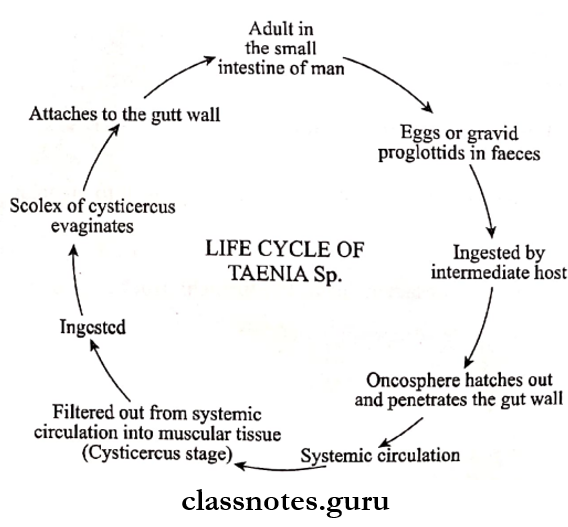
6. Cestodes
- Taenia saginata
- Taenia solium
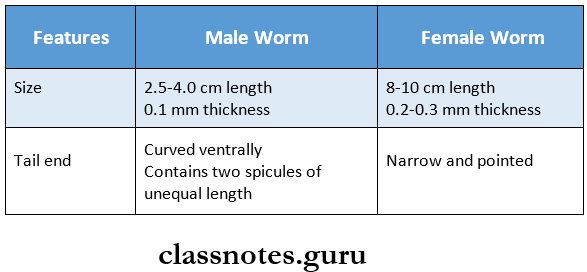
7. Nematodes
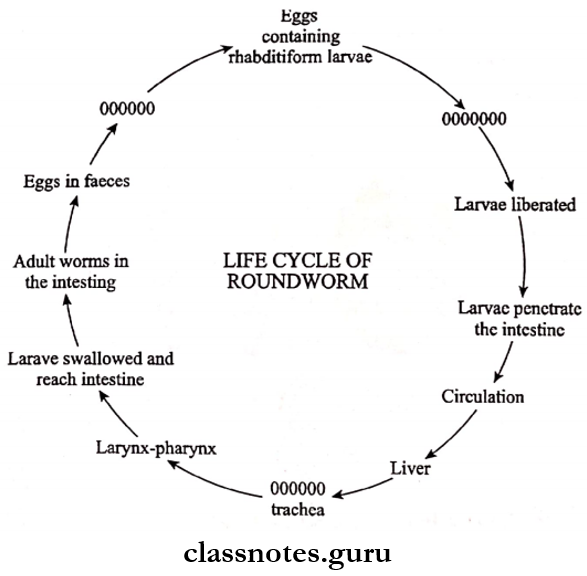
- Ascaris lumbricoides or round worm
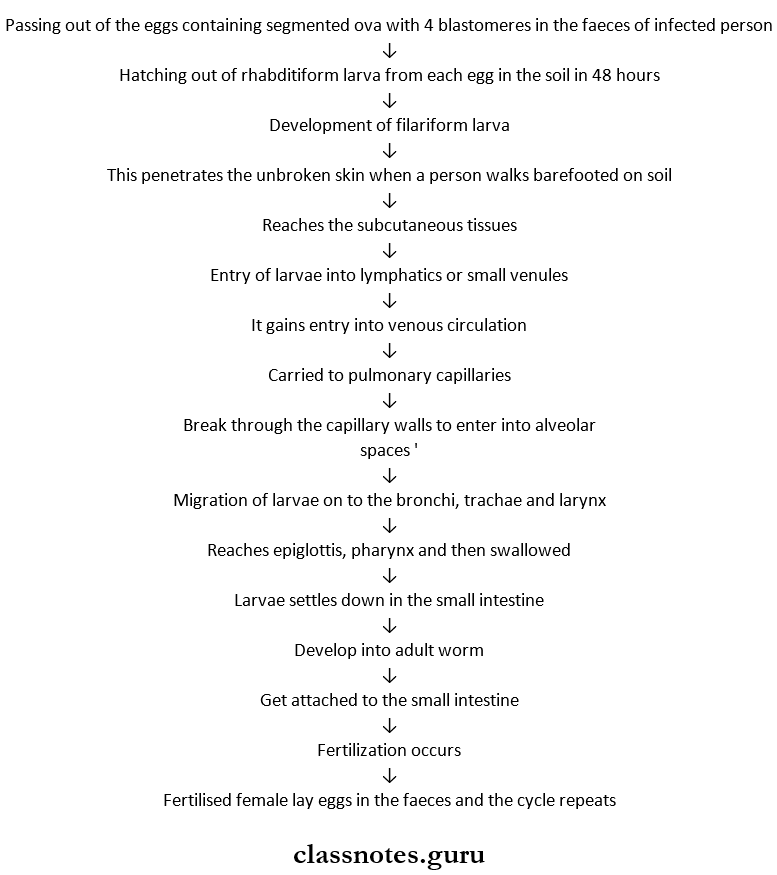
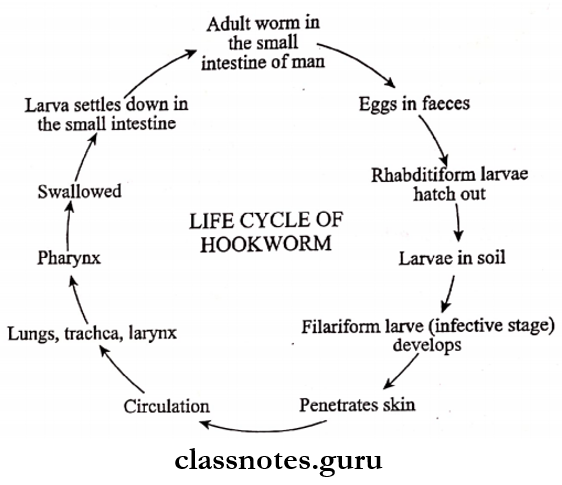
- Hookworm
- Ankylostoma duodenale
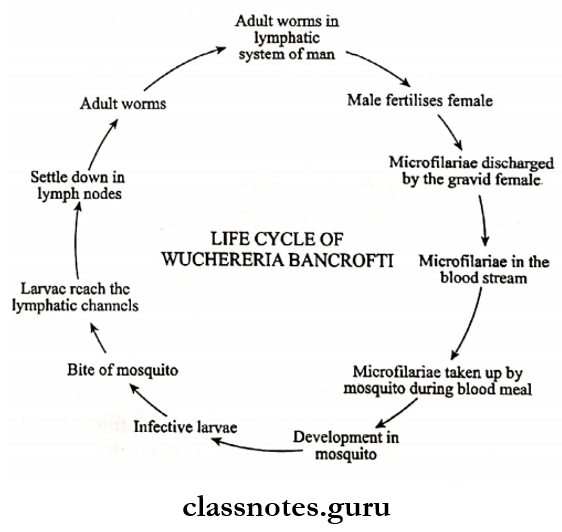
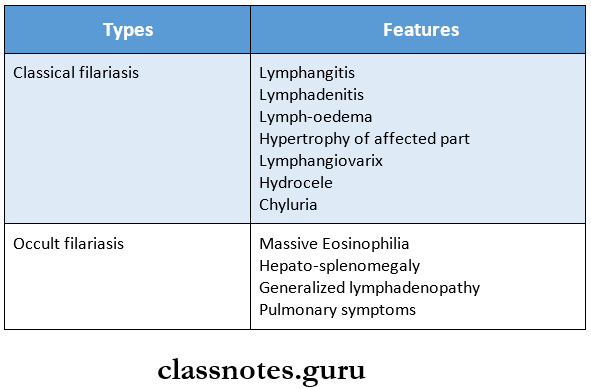
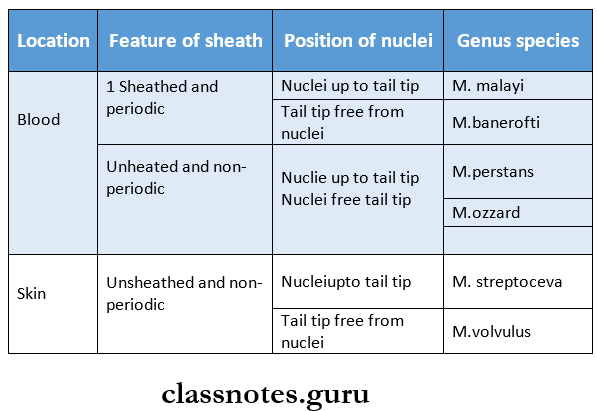
- Wuchereria bancrofti
Protozoans Long Essays
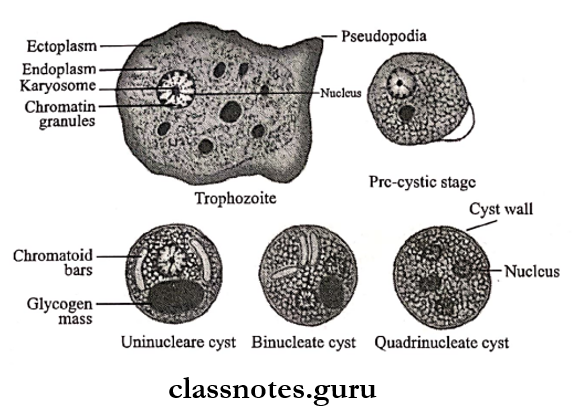
Question 1. Describe the morphology, pathogenesis, and life cycle of Entamoeba histolytica. Write about the laboratory diagnosis of intestinal amoebiasis.
Answer:
Entamoeba histolytica causes intestinal amoebiasis and hepatic amoebiasis
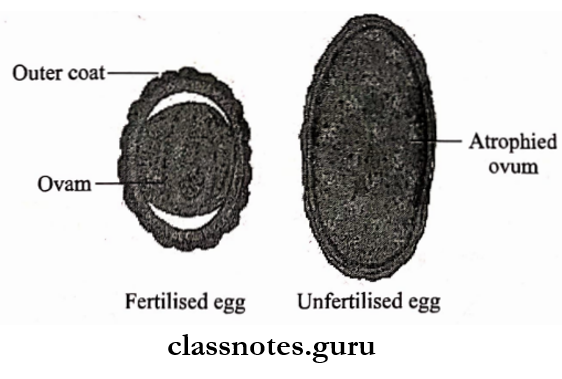
Entamoeba Histolytica Morphology:
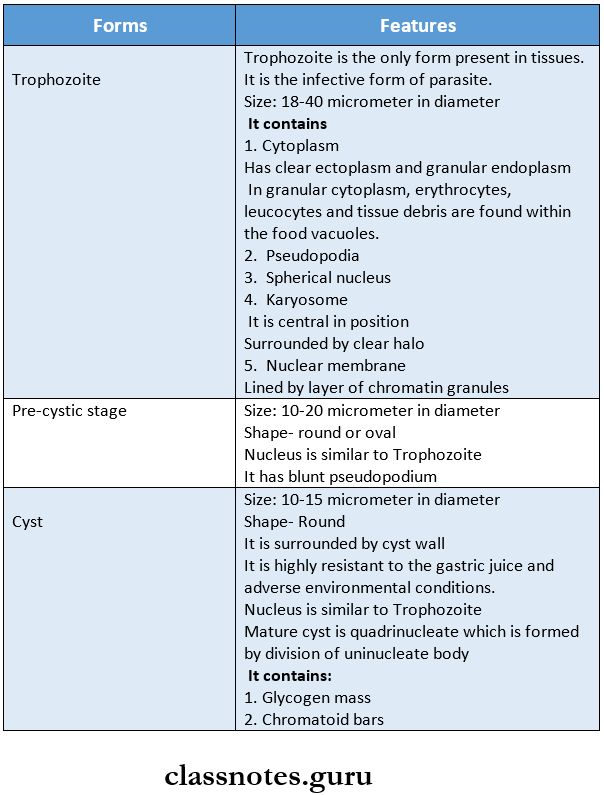
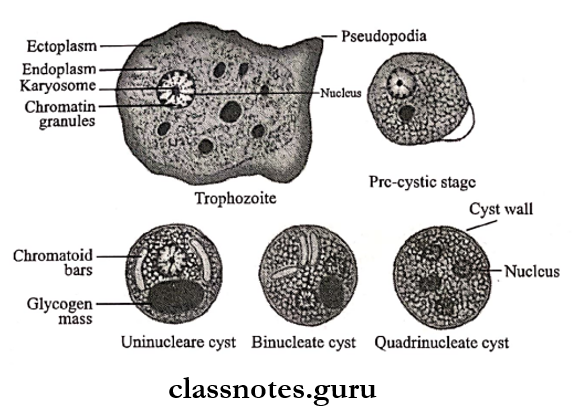
The parasite exists in 3 forms
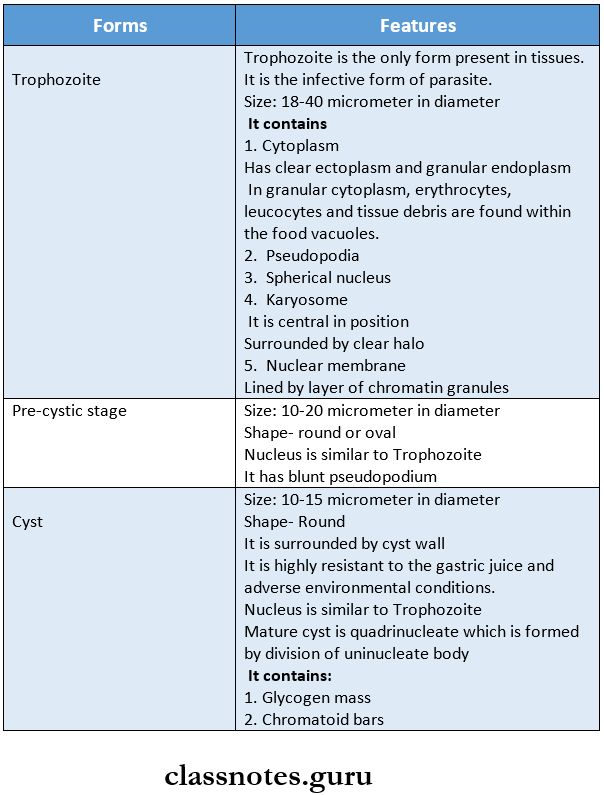
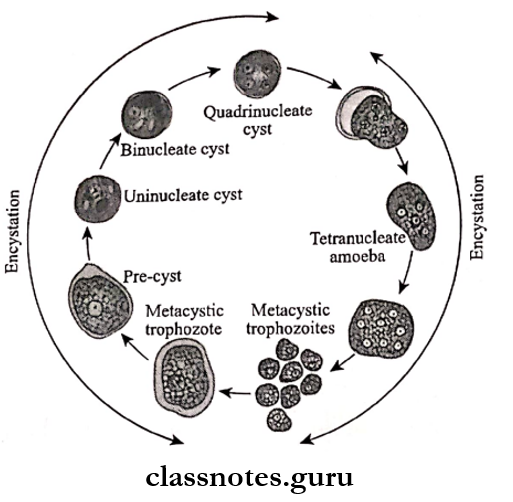
Entamoeba Histolytica Life Cycle:
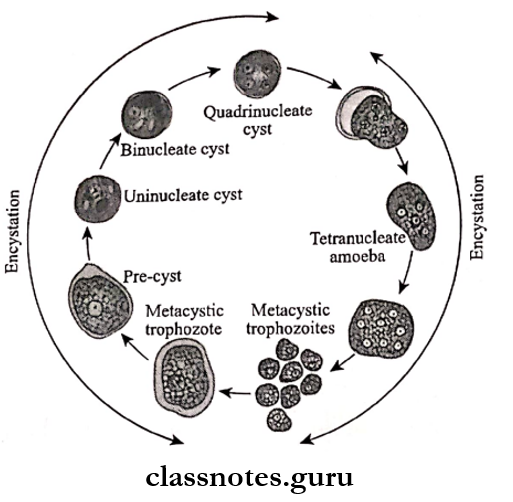
- E. histolytica passes its life cycle in only one host, the human.
- The mature quadranucleate cysts are infective forms.
- These cysts enter men through the ingestion of water and food containing it
- These reach the caecum or the lower part of the ileum called the excystation
- Each mature cyst liberates a tetranuclear amoeba
- Forms eight metacystic Trophozoites by binary fission
- It gets lodged in the submucous tissue of the large intestine
- E. histolytica secretes a proteolytic enzyme
- Causes destruction and necrosis of tissues
- Results in the formation of flask-shaped ulcers
- Next, these Trophozoites are
- Excreted along with blood and mucus in feces
- Results in amoebic dysentery
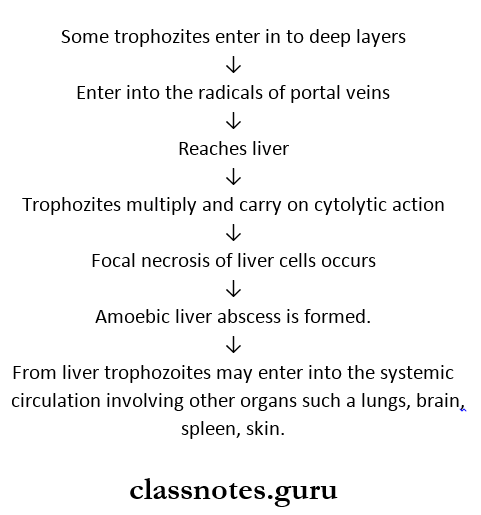
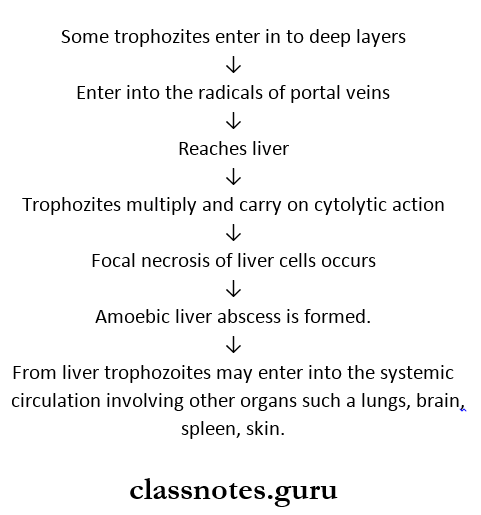
- Enter into deeper layers
- Enter the portal vein
- Reaches liver
- Causes amoebic hepatitis and amoebic liver abscess
- The effect of the parasite on the host decreases
- This increases host tolerance, and healing starts
- Encystation occurs, which is the transformation of Trophozoites into cysts and cysts.
Medically Important Protozoans Long Essay Questions
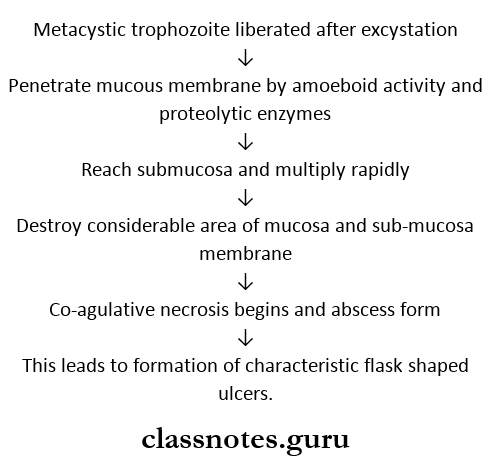
Entamoeba Histolytica Pathogenesis:
E. Histolytica can cause two types of pathological lesions as follows
1. Primary (or) Intestinal Amoebiasis:
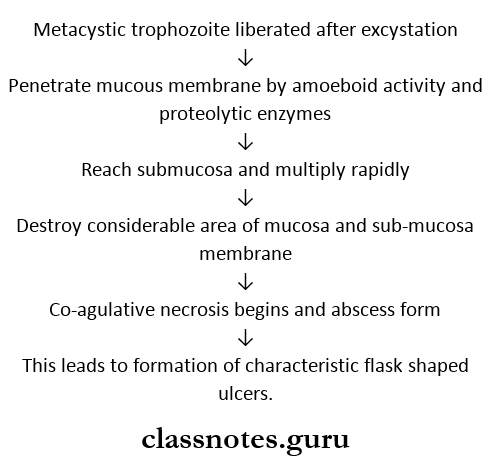
- This condition is called amoebic dysentery.
- This ulcer may be generalized or) may be localized to the ileocaecal (or sigmoidorectal region.
- Occasionally ulcers may involve deeper tissues and may cause perforation (or) peritonitis.
- Erosion of blood vessels may lead to hemorrhage.
- The superficial lesions generally heal without scarring.
- Deep ulcers form scars leading to strictures, partial obstruction, and thickening of the gut wall
Virology and Protozoology Question Bank for NEET PG
2. Extra-Intestinal Amoebiasis (or) Secondary (or) Metastatic Lesions.
Laboratory Diagnosis of Intestinal Amoebiasis:
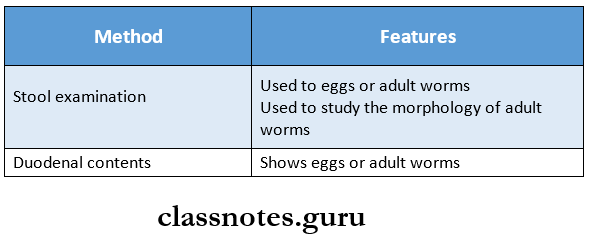
1. Stool Examination:
- The stool is collected directly into a wide-mouthed con¬tainer and examined without delay.
- Macroscopic Examination
- The stool is an offensive odor
- Dark brown and semifluid
- Acid in reaction
- Mixed with blood and mucous
- Microscopic Examination
- The cellular exudates is scanty, and consist of nuclear masses of a few pus cells, macrophages, and epithelial cells
- RBCs are seen in clumps
- Charcot- Leyden crystals are also seen
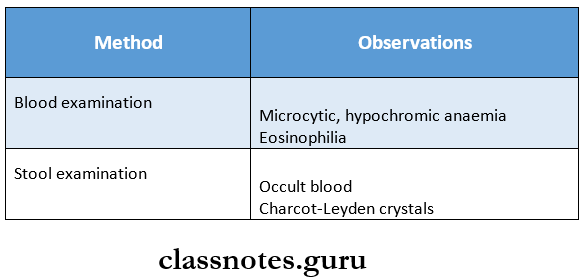
2. Blood Examination
- In early cases, it is always negative
- The antibody can be detected in later stages of invasive intestinal amoebiasis
- The test used is ELISA haemagglutination assay (HIA).
3. DNA Probes:
- DNA probes have been used to detect E. histolytica in stool specimens.
Question 2. Describe the life cycle of malarial parasites in man. Give a brief description of pathological lesions produced in man.
Answer:
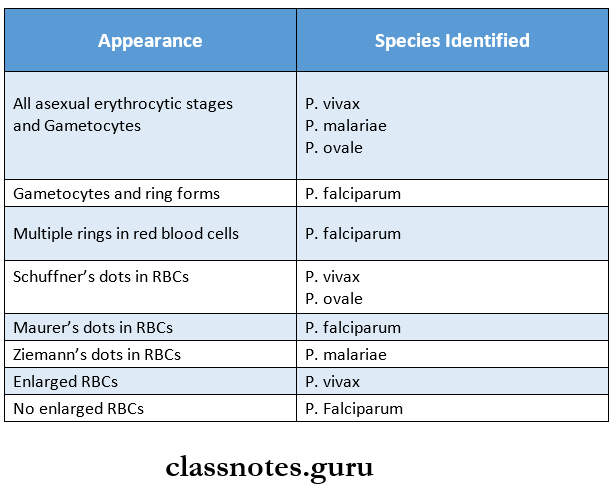
Malaria is a disease caused by four plasmodium species which are as follows:
- P. vivax
- P. Falciparum
- P. Malaria
- P. Ovale.
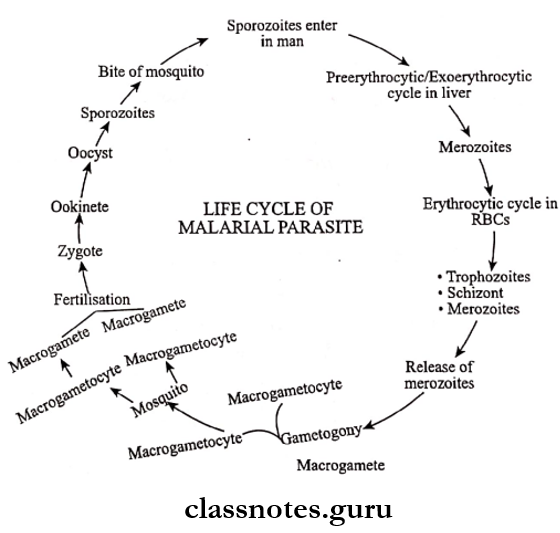
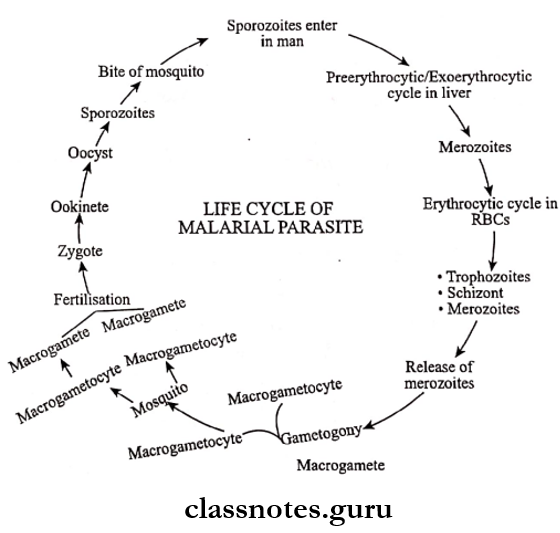
Malarial Life Cycle: The malarial parasites pass their life cycle in two. hosts.
- Man intermediate host [a sexual development]
- Female anopheles mosquito – definitive host [sexual development].
Human Cycle, Or Schizogony, Or A Sexual Cycle:
- The sporozoite is the infective form of a malarial parasite.
- A man gets infected by the bite of an infected female Anopheles mosquito
- This mosquito contains sporozoites in the salivary gland, which enter directly into the blood circulation of man
- By this human cycle starts, which comprises of following stages.
Medical Microbiology Notes on Protozoans and Viruses
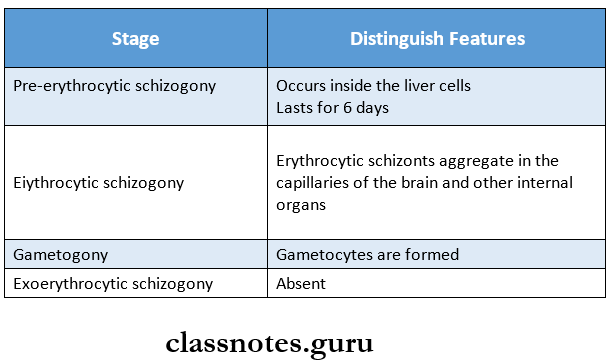
1. Pre-erythrocytic Schizogony
- It is a developmental phase of sporozoites inside the liver cells
- The shape of sporozoites is round
- Size-Varies
- They undergo nuclear division to develop schizonts
- Each schizont contains 20,000-50,000 merozoites
- Duration of this stage
- P. vivax – 8 days
- P. falciparum – 6 days .
- P. malariae – 13-16 days
- P. ovale – 9 days
- After this period, the liver cells rupture
- As a result, merozoites are released into the bloodstream
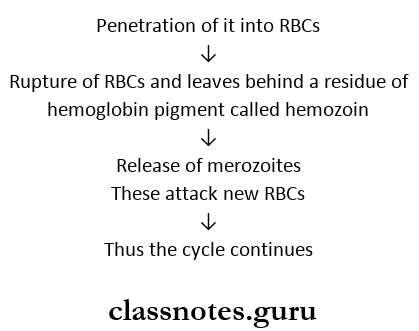
2. Erythrocytic Schizogony:
- Release of merozoites into the blood
- Penetration of it into RBCs
- Rupture of RBCs, which leaves behind a residue of hemoglobin pigment called hemozoin
- Release of merozoites
- These attack new RBCs
- Thu,s the cycle continues
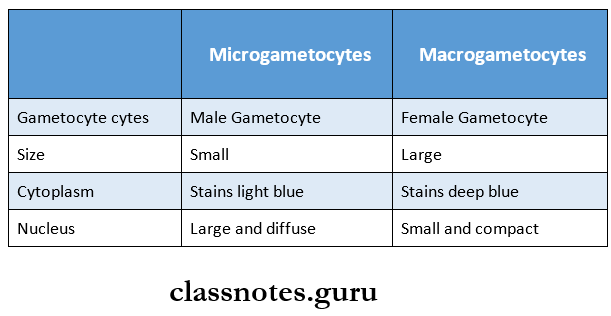
3. Gametogony:
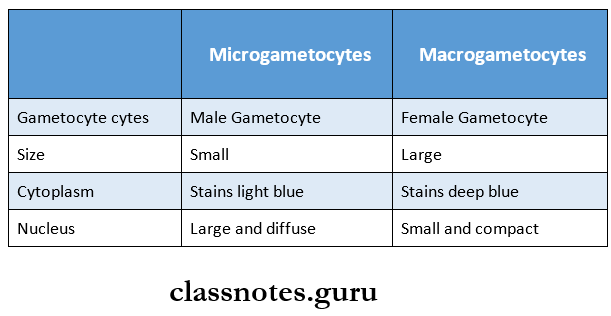
- Some merozoites develop sexual forms known as microgametocytes and macrogametocytes
4. Exo-erythrocytic Schizogony:
- Some sporozoites enter liver cells but don’t multiply
- Enter in the resting phase and are known as Hypnozoite
- These hypnozoites get reactivated
- Forms schizonts
- Releases merozoites called phanerozoic
- Attack RBCs
- Causes relapse of malaria
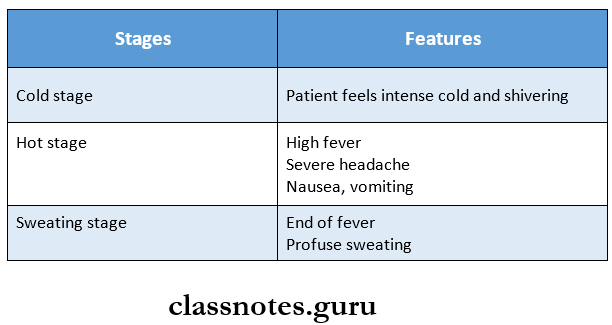
Malaria Clinical Features:
- Intermittent fever, which is named as malaria, is caused by plasmodium
- It consists of
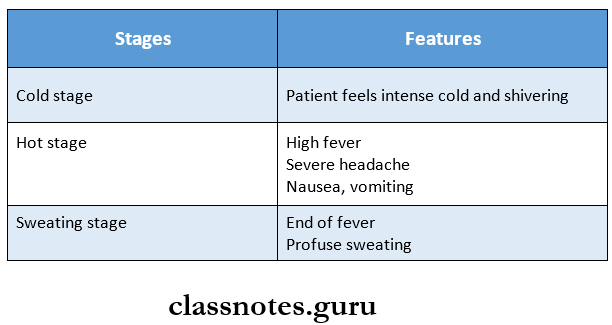
1. Febrile Paroxysm
- It comprises three stages
2. Anaemia
- Microcytic or normocytic hypochromic anemia develops
3. Splenomegaly.
- The spleen becomes enlarged and palpable
- Blackwater fever and pernicious malaria are the most commonly seen complications in falciparum malaria.
Parasitology and Virology Essay Questions PDF Download
Protozoans Short Essays
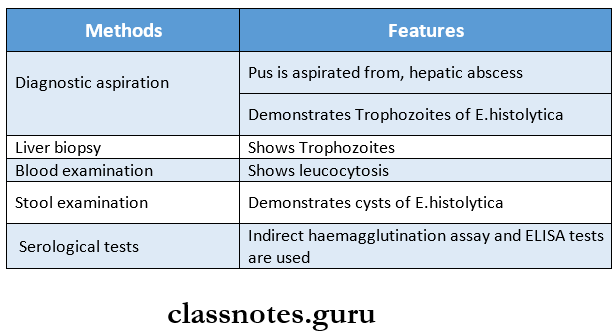
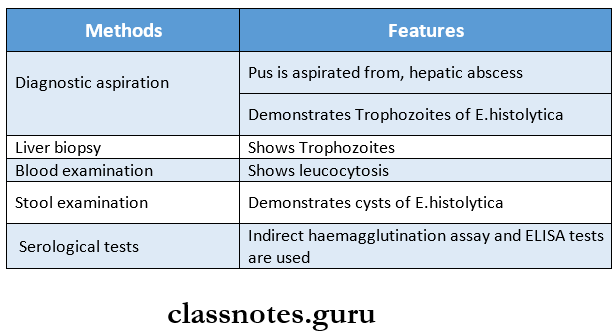
Question 1. Laboratory diagnosis of extraintestinal amoe¬biasis
Answer:
Diagnostic methods for extraintestinal amoebiasis are as follows
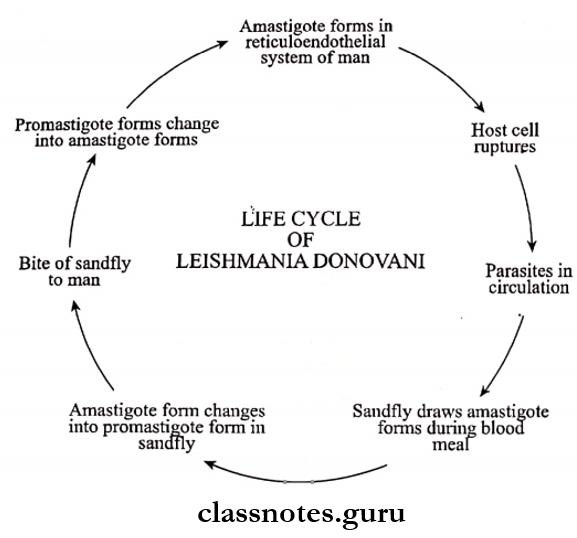
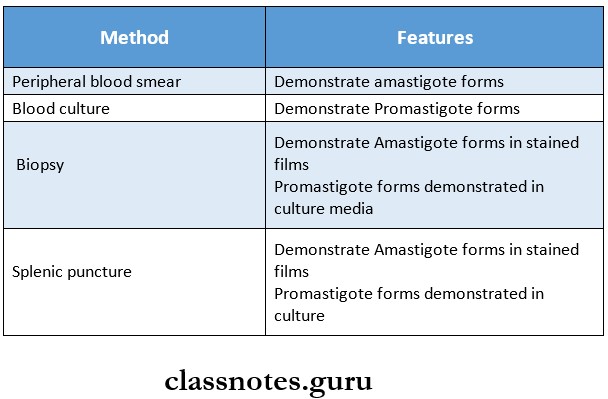
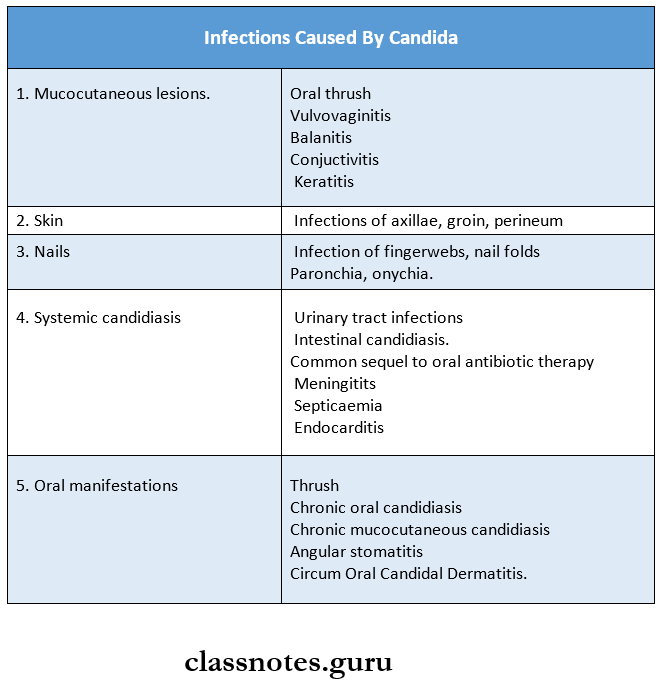
Question 2. Leishmania donovani
Answer:
It causes visceral leishmaniasis or kala-azar
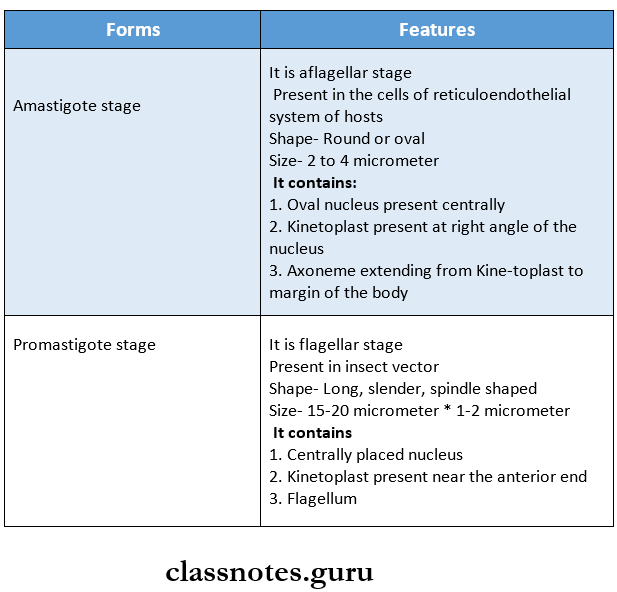
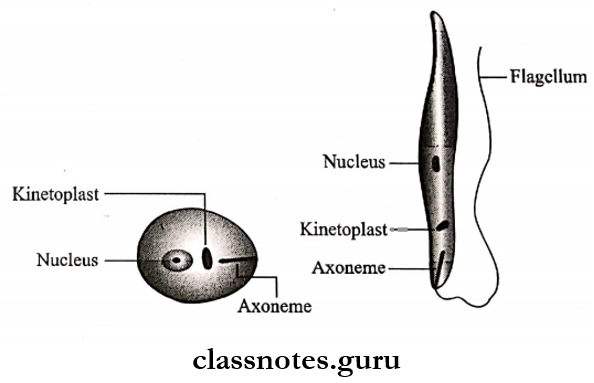
Leishmania Donovani Morphology: It occurs in two forms:
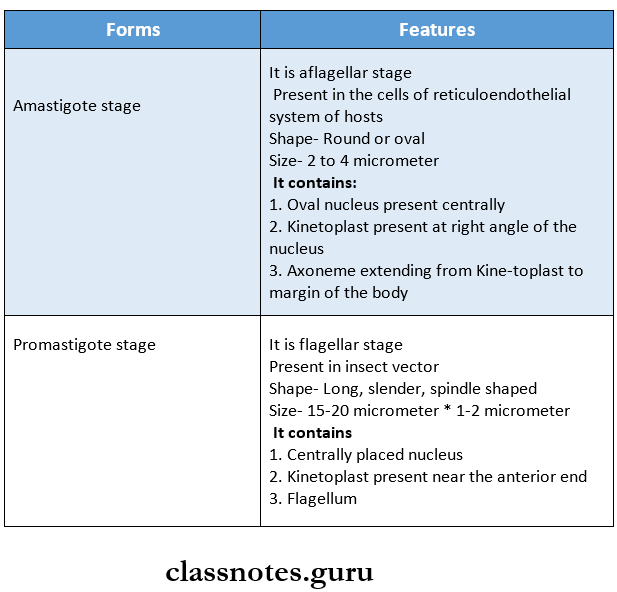
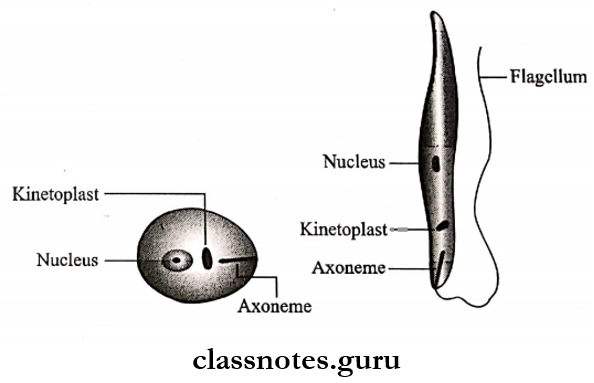
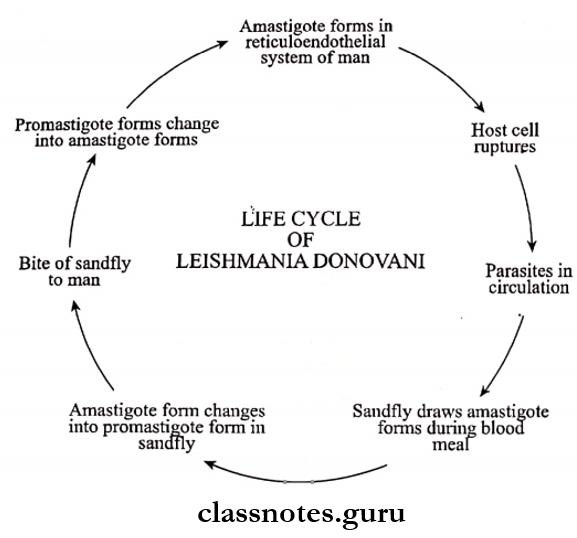
Leishmania Donovani Life Cycle:
- The parasite has two stages in its life cycle
- Amastigote form
- Promastigote form
- Initially, the multiplication of the amastigote form occurs in the reticuloendothelial cells in the host
- Enlargement of host cells occurs
- These cells rupture to release parasites into circulation
- Blood-sucking insect obtains it by sucking
- Development of the Promastigote form from the Amastigote form
Leishmania donovani Clinical Features:
- Pyrexia
- Splenomegaly
- Hepatomegaly
- Lymphadenopathy
- Anaemia
Question 3. The life cycle of the plasmodium in the mosquito
Answer:
- The sexual development of the plasmodium occurs in the mosquito
- It starts in the human host with the formation of Gametocytes
- The cycle includes the following steps
- Bite of a female anopheles from the patient
- Mature sexual forms develop in the mosquito
- In the midgut
- 1 microgametocyte- develops 4-8 microgametes
- 1 macrogametocyte- Develops 1 macrogamete
- Fertilization of the acrogamete occurs
- Formation of a zygote
- Lengthening and maturation of the zygote to form the ookinete
- Formation of oocyst from ookinete
- Maturation of oocyst
- Increase in size and number of sporozoites
- Rupture of the oocyst to release sporozoites in the body of the mosquito
- Distribution of sporozoites into various organs and tissues, especially in salivary glands
Question 4. Laboratory diagnosis of malaria
Answer:
The demonstration of the parasite in the blood is the most important method for the diagnosis of malaria.
1. Microscopic Examination Of Blood Film:
- Thick and thin smears of blood are prepared on the same slide or) two different slides.
- Blood is collected before antimalarial therapy
2. Fluorescent Microscopy:
- A blood smear is prepared on a slide and is stained with acridine orange
- The slide is observed under a fluorescent microscope.
- The nuclear DNA of the malarial parasite is stained green, and the cytoplasmic RNA is stained red.
3. Blood Counts:
- Blood shows moderate leukopenia and monocytosis.
4. Serological Tests:
- The serological tests used are
- ELISA
- Indirect haemagglutination assay
- Indirect immunofluorescence test.
5. DNA Probes:
- These are sensitive and specific diagnostic methods for the diagnosis of malaria
- It can detect even a low parasitemia, i.e., <10 parasites/dl
6. Polymerase Chain Reaction (PCR):
7. Rapid Diagnostic Tests:
- These are based on the detection of antigens using immune chromatographic methods.
- In these tests, a dipstick containing monoclonal antibodies is directed against the parasitic antigens.
- This test takes about 15 minutes.
- Several commercial kits are available.
- Kits available to detect histidine-rich protein (HRP-II) of P. falciparum.
- The test is commercially available as the parasite ‘F’ test.
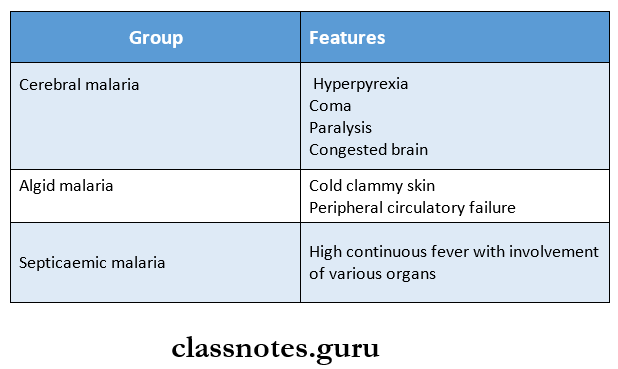
Question 5. Complications of plasmodium falciparum infection?
Answer:
Complications of P.Falciparum Are:
- Pernicious malaria
- Blackwater fever.
1. Pernicious Malaria:
- It is a life-threatening condition
Pernicious Malaria Cause:
- It is due to heavy parasitization.
Pernicious Malaria Clinical Features:
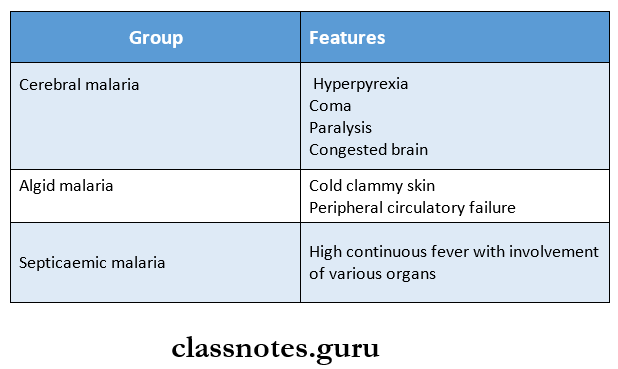
- It is grouped into the following:
2. Blackwater fever:
This occurs in persons who are previously infected and have had inadequate doses of quinine
Black Water Fever Clinical Features:
- Intravascular hemolysis,
- Fever,
- Haemoglobinuria
- Vomiting and prostration with the passage of dark red (or blackish urine ,hence called backwater fever.
Black Water Fever Mechanism:
- An autoimmune mechanism may be involved in hemolysis
- Parasitized erythrocytes from previous infection act as an antigen
- Antibodies are formed against it
- Due to this antigen-antibody reaction, massive destruction of erythrocytes occurs
- There is excessive deposition of haemosiderin pigment in the liver, spleen, and kidneys.
- Sequels of black water fever include
- Circulatory failure
- Renal failure,
- Liver failure,
- Anaemia.
Protozoans: Short Questions and Answers
Question 1. Draw morphological forms of Entamoeba His¬tolytica
Answer:
Question 2. Amoebic dysentery
Answer:
- Amoebic dysentery is also known as intestinal amoebiasis
- It is a condition in which the infection is confined to the intestine and is characterized by the passage of blood and mucus in the stool
Amoebic Dysentery Types:
1. Acute Amoebic Dysentery
- Multiple ulcers occur
- These ulcers are deep and extensive
- Its complications are
- Pericaecal and pericolic abscess
- Amoebic appendicitis
- Perforation
- Generalized peritonitis
- Gangrene of the guts
- Fistula
2. Chronic Amoebic Dyssentery
- A single latent ulcer is present in the caecum, while multiple small superficial ulcers are scattered throughout the large intestine
- Stricture formation occurs
- Amoeboma in the caecum and large intestine develops
Question 3. E.gingivalis / Morphology of E.gingivalis
Answer:
E.gingivalis Morphology:
- It is a small amoeba measuring 10 – 20 (μm in diameter and is actively motile by multiple pseudopodia.
- It has the only trophozoite stage, and there is no cystic phase.
- It contains
- The cytoplasm is divided into clear ectoplasm and granular endoplasm.
- Cytoplasmic inclusions consisting of bacteria,a leucocytes but never RBCs
- The nucleus is spherical
- Central karyosome.
- Nuclear membrane is lined with closely packed chromatin granules.
E.gingivalis Pathogenesis:
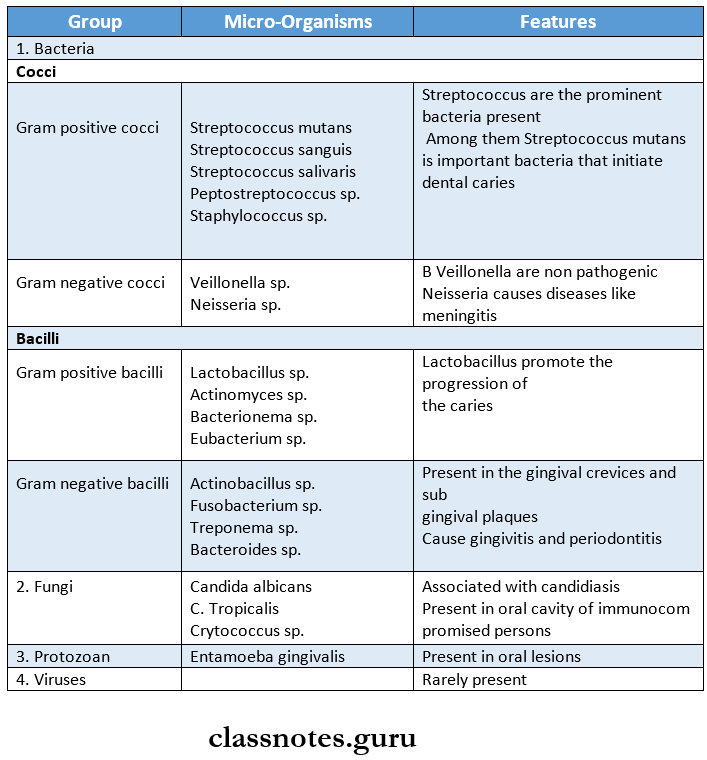
- E.gingivalis is a parasite of human mouth.
- It occurs as a commensal in gingival tissue around the teeth particularly in the unhealthy tissues such as in pyorrhoea alveolaris.
- It is also found in the crypts and histologic sections of diseased tonsils.
- It is transmitted by close contact, like kissing.
- Laboratory diagnosis depends on the demonstration of tro¬phozoites of E. gingivalis in the material removed from the gingival margin of the gum (or) from the denture.
Question 4. Erythrocytic schizogony
Answer:
- It is the second stage of the human cycle of the malaria parasite
- During this phase, the parasite resides inside the RBC and passes through stages of Trophozoites, schizonts, and merozoites.
- The following changes occur during this phase
- Release of merozoites into the blood
Question 6. Plasmodium falciparum
Answer:
Plasmodium falciparum is one of the malarial parasites
Stages of Human Cycle in P. Falciparum:
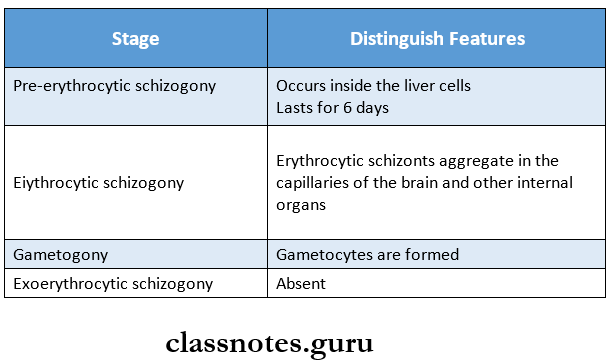
- P. falciparum is the most pathogenic among the plasmodium species infecting man
- No relapse occurs in P. falciparum infection
- It invades erythrocytes of all ages
- Its incubation period is 10-14 days
Plasmodium Falciparum Complications:
- Pernicious malaria
- Blackwater fever
Question. Blackwater fever
Answer:
This occurs in persons who are previously infected and have had inadequate doses of quinine
Black Water Fever Clinical Features:
- Intravascular hemolysis,
- Fever,
- Haemoglobinuria
- Vomiting and prostration with the passage of dark red (or blackish urine ,hence called backwater fever.
Question 9. Kala-azar
Answer:
Leishmania donovani produces the disease Kala Azar (or visceral leishmaniasis.
Kala-azar Clinical Features:
- Pyrexia,
- Splenomegaly,
- Hepatomegaly,
- Lymphadenopathy and
- Anaemia.
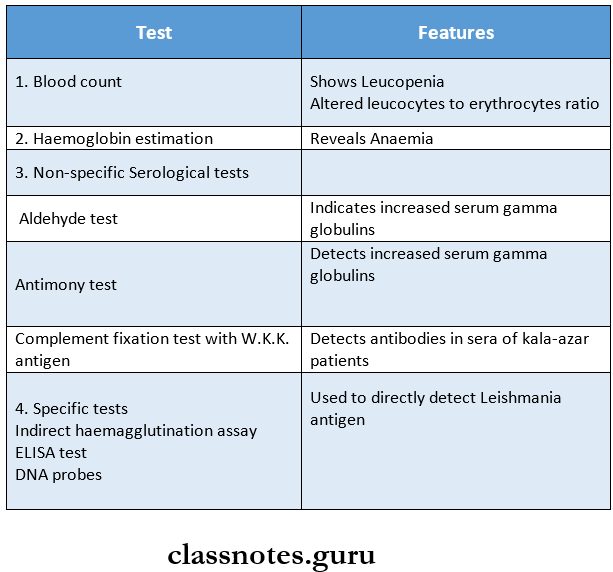
Kala-azar Laboratory Diagnosis:
1. Direct Evidence:
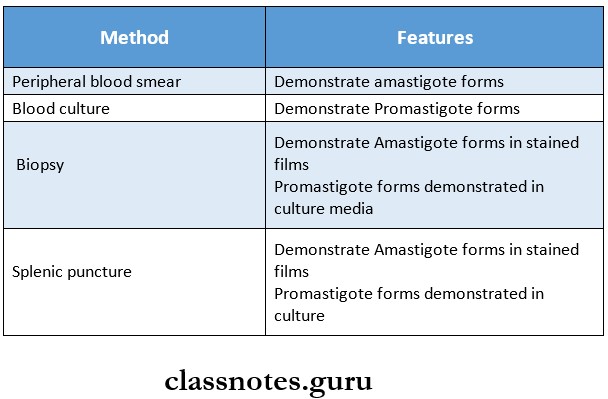
2. Indirect Evidence:
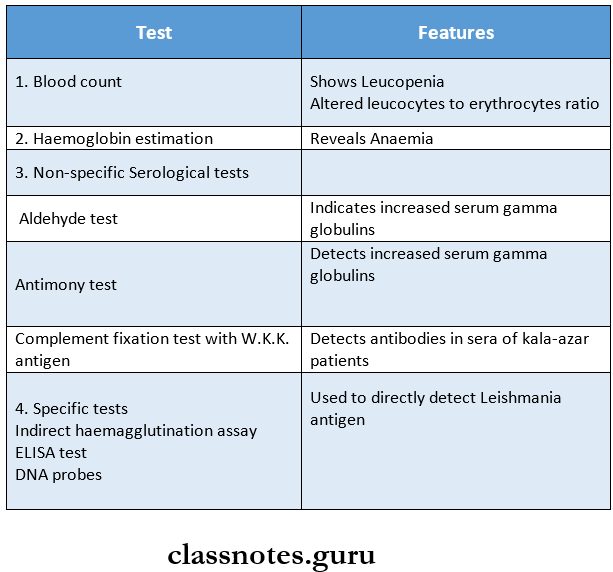
3. Rapid immune chromatographic strip test:
- It detects antibodies against the K39 antigen of L. donovani
- It indicates active kala-azar
Question 10. Benign tertian malaria
Answer:
- Benign tertian malaria is caused by Plasmodium vivax
- Initially, there may be continuous or remittent fever
- In later stages, typical intermittent periodic fever develops
- Initially, two broods of parasites undergo schizogony on alternate days but then one brood drops out.
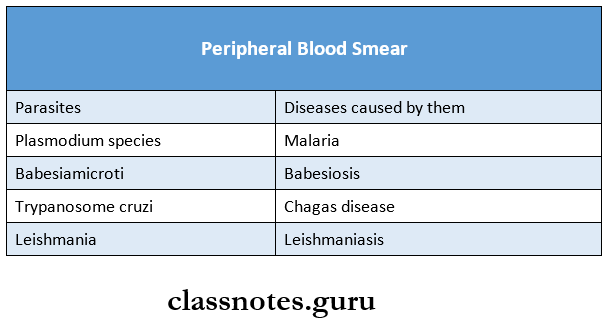
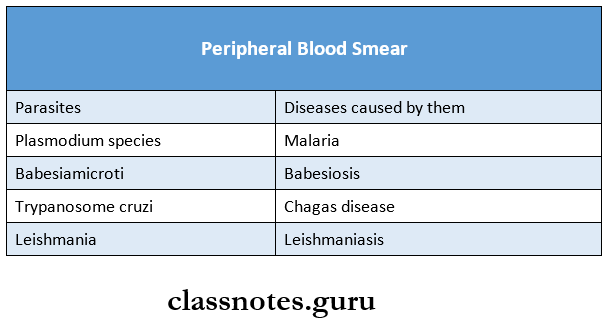
Question 11. Mention the parasites found in the peripheral blood smear.
Answer: