Oral Medicine Blood Disorders Important Notes
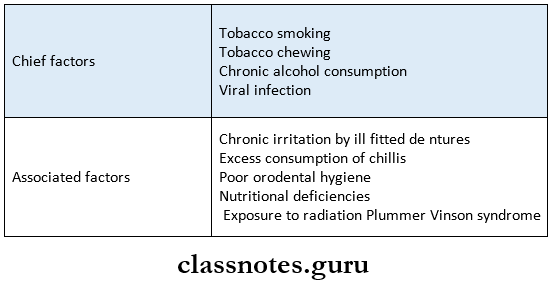
1. Plummer Vinson Syndrome
- Iron deficiency anemia
- Carcinoma of hypopharynx
- Koilonychias
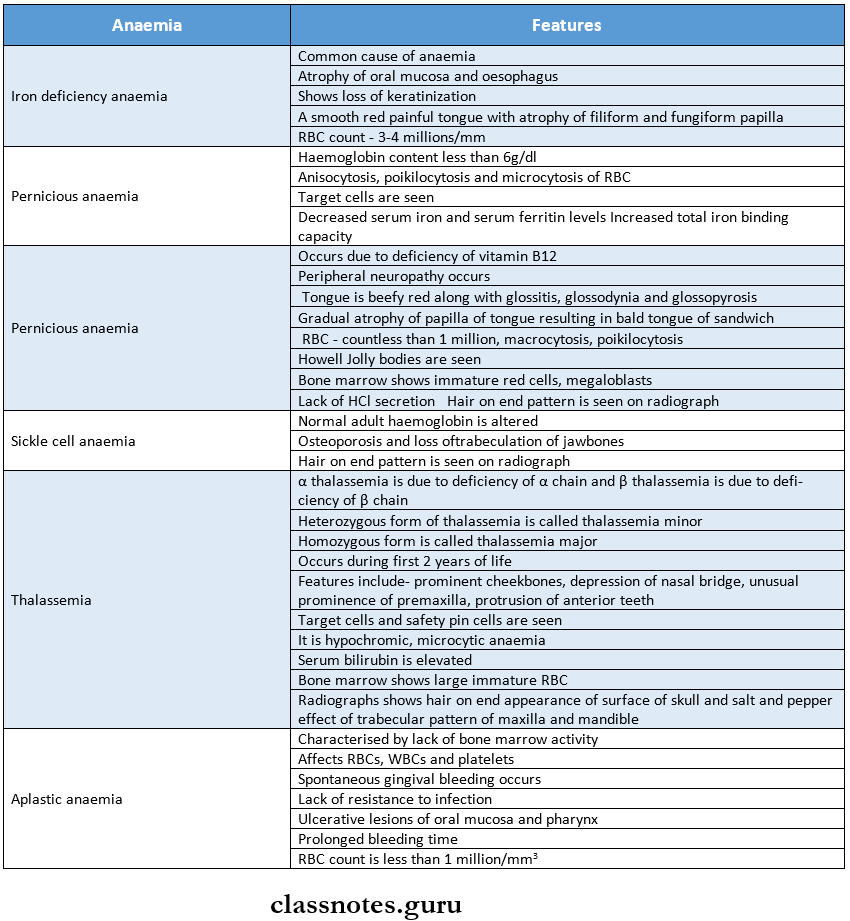
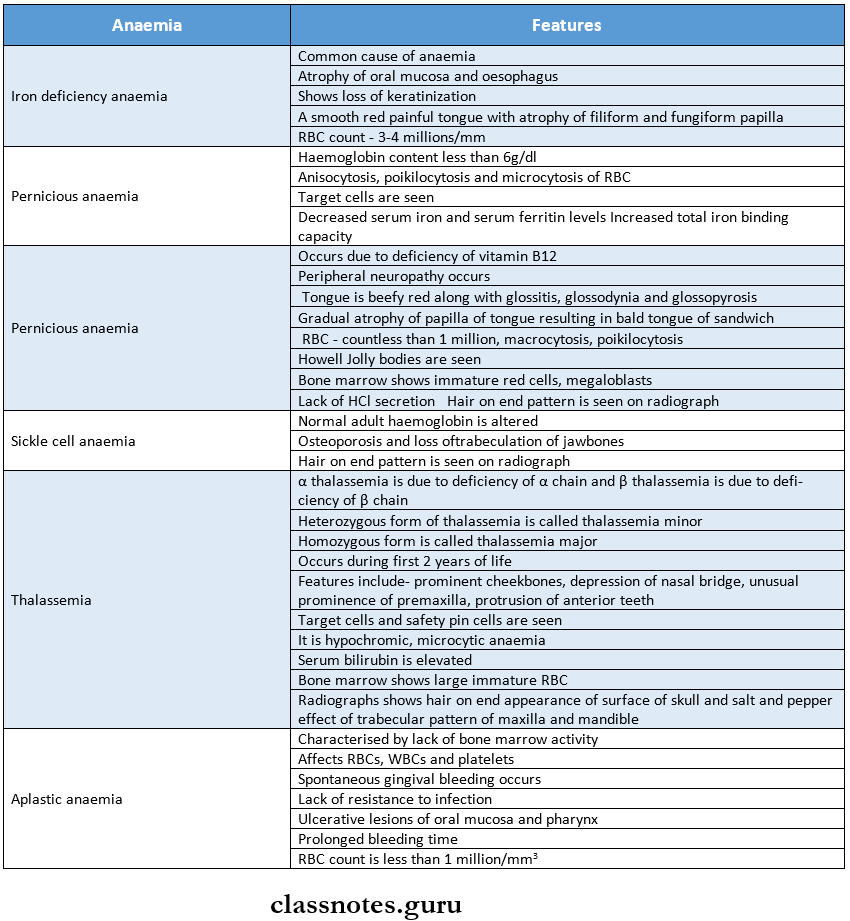
2. Types Of Anemia
3. Hair On-End Appearance Is Seen In
- Thalassemia
- Sickle cell anemia
4. Anitschow Cells
- They are modified epithelial cells with
- Elongated nuclei
- Linear bar of chromatin
- Seen in
- Sickle cell anemia
- Iron deficiency anemia
- Aphthous ulcer
Read And Learn More: Oral Medicine Question and Answers
Oral Medicine Blood Disorders Short Essays
Question 1. Define anemia. Write oral manifestations of iron deficiency anemia
(or)
Iron Deficiency Anaemia.
Answer:
- Anaemia:
- Anemia is defined as hemoglobin concentration in blood below the lower limit of the normal range for the age and sex of the individual.
- Iron Deficiency Anaemia
- It is a chronic, microcytic, hypochromic type of anemia, which occurs either due to inadequate absorption or excessive loss of iron from the body.
Iron Deficiency Anaemia Causes:
- Inadequate intake of iron in the diet
- Malabsorption of iron due to diarrhea
- The increased requirement for growing children and pregnancy
- Increased loss of iron due to injury, epistaxis, and peptic ulcer
- Gastrotomy
Iron Deficiency Anaemia Clinical Manifestations:
- Age and Sex – Women in the 4th and 5th decade
- Tiredness, headache, paresthesia, and lack of concentration
- Koilonychia – nails become brittle, flattened and spoon-shaped
- Lemon-tinted paler skin
- Dizziness and sensitivity to cold
- The liver and spleen may be palpable
- Tingling sensation in extremities
- Knuckle pigmentation is seen on the dorsum of the hand at the metacarpophalangeal joint
Iron Deficiency Anaemia Oral Manifestations:
- The pallor of the oral mucosa and gingival with atrophy and loss of keratinization
- Tongue – Glossitis, loss of papillae, and glossodynia
- The tongue appears bald and red with a glazed appearance
- Mucosa – Recurrent aphthous ulcer
- Candidiasis
- Abnormal bleeding
- Faulty wound healing
- Angular cheilitis
- Associated syndrome – Plummer-Vinson syndrome
Iron Deficiency Anaemia Laboratory Diagnosis:
- Hemoglobin level – decreased
- Total RBC count – < 3 million per mm3
- MCV, MCH, MCHC – reduced
- Serum iron level – decreased to 10 mg
- Hemosiderin – absent
Iron Deficiency Anaemia Management:
- Iron supplement
- Ferrous sulfate 300 mg 3-4 times/day for 6 months orally
- Iron sorbitol 1.5 mg/kg body weight given parenterally.
Question 2. Thalassemia Major.
Answer:
Thalassemia Major
- Thalassemia Major occurs when the patient is homozygous
- Thalassemia Major is also called Cooley’s anemia
- Thalassemia Major is an autosomal recessive disease
Thalassemia Major Clinical Manifestations:
- Age – occurs in the first two years of life
- The patient often suffers from jaundice
- Fever, chills, marked anemia, malaise, generalized weakness, and lethargy.
- Splenomegaly, leg ulcers
- Most of the patients have a mongoloid facies with a prominent forehead, depressed nasal bridge, and slant-ing eyes
- It leads to organ failure
Thalassemia Major Oral Manifestations:
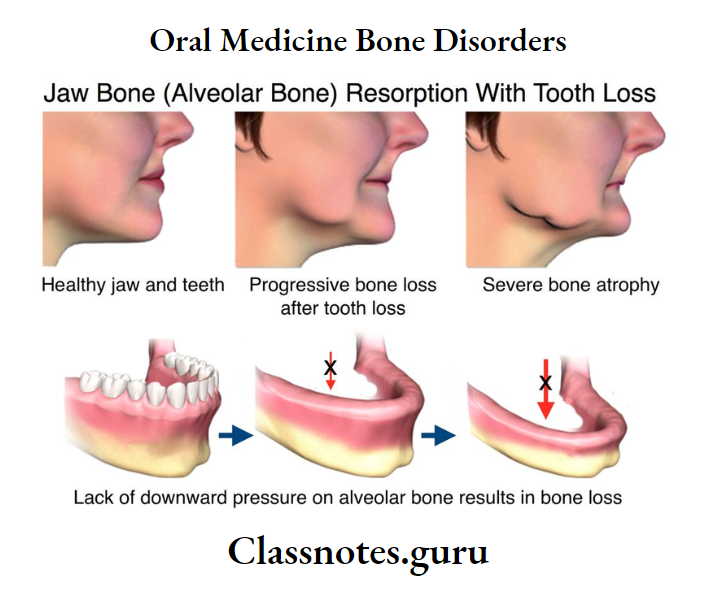
- Jaw bone – Excessive growth of the maxilla
- Mucosa-Yellow tinted palor mucosa
- Alveolar process – Hyperplastic
- Teeth – Bimaxillary protrusion
- Spacing and flaring of maxillary anterior
- Open bite
- Discoloration of teeth
- Chipmunk facies – Characterized by saddle nose, prominent malar bone, and pneumatization of maxil¬lary sinus
- Poor healing after dental treatment
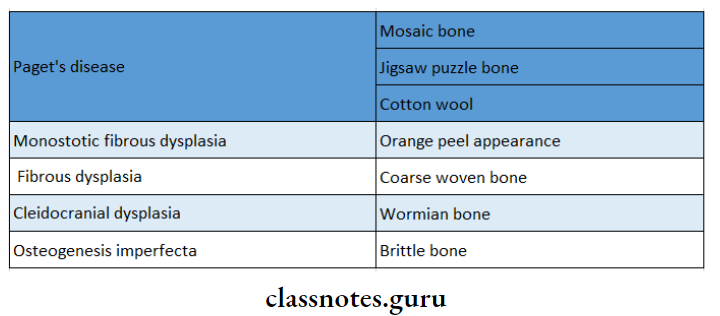
Thalassemia Major Radiographic Appearance:
- The skull bones exhibit a typical “hair-on-end” appearance on the radiograph
- Generalized rarefaction of the alveolar bone, thinning of the cortex, and enlarged marrow spaces are found
- It shows the “salt-and-pepper effect” by coarsening of some bony trabeculae and blurring of others
- Spike-shaped and short roots of teeth
- Antrum is reduced in size
Thalassemia Major Diagnosis:
- RBC – microcytic, hypochromic
- Bone marrow – shows increased erythropoietic activity
- Reticulocyte count-increased
- Serum bilirubin and urobilinogen – elevated
- Fetal hemoglobin – elevated
Thalassemia Major Management:
- Repeated blood transfusions are necessary
- Allogenic bone marrow transplantation can be done
- Splenectomy is indicated
- Supplementary folic acid is required
- Surgical correction in patients with abnormal facial appearance
Question 3. Agranulocytosis.
Answer:
Agranulocytosis
- Agranulocytosis is a serious acute disease characterized by a significant decrease in the number of granular leukocytes.
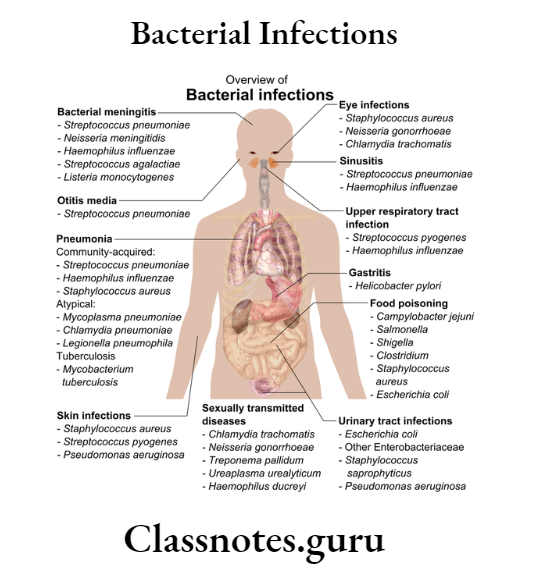
Etiology:
- Toxic effects of some drugs like sulfonamides
- Due to the hypersensitivity to drugs
- Long-term administration of analgesics
- Ionizing radiation, tuberculosis, typhoid, malaria
Agranulocytosis Clinical Features:
- Initially high fever, chills, and sore throat
- Skin appears pale and anemic
- Persistent infections with regional lymphadenitis
- Severe dysphagia
- Weak and rapid pulse
- Urinary tract infections
- Vaginal and rectal ulceration
- Patient dies within 3-5 days due to toxemia and septicemia
Agranulocytosis Oral Manifestations:
- Mucosa-necrotizingulceration
- They are covered by a yellow/grey membrane
- Gingival bleeding spontaneously
- Excessive salivation
- Halitosis
- Fungal infections
- The lesion appears as ragged and necrotic
- It is covered with grey black membrane
- Destroys supporting structures along with teeth loss.
Agranulocytosis Diagnosis:
- WBC count – reduced – 500 to 3000/mm³
- Bone marrow – the absence of granulocytes
- Granulocyte count < 100 cells/mm³
Agranulocytosis Treatment:
- Removal of the offending agent
- Transfusion of red cell constituent when hemoglobin is < 10 gm/dl.
- Antibiotics – To control septicemia
- A combination of drugs is given
- Granulocyte-macrophage colony-stimulating factors
- Dental management – for ulcers, 5% dyclonine and 5% Benadryl mixed with magnesium hydroxide or Kaolin with pectin is useful.
Question 4. Cyclic Neutropenia.
Answer:
Cyclic Neutropenia
Cyclic Neutropenia is an idiopathic disease characterized by episodic defects in neutrophil maturation in the bone marrow, resulting in periodic falls in circulating neutrophils
Cyclic Neutropenia Clinical Features:
- Recurrent upper respiratory tract infections
- Short-term fevers, sore throat
- Headache, arthritis, conjunctivitis
- Amyloidosis
- Regional lymphadenopathy, Gingivitis, ragged painful ulcers
Cyclic Neutropenia Diagnosis:
- WBC count – decreases to 3000 cells/cu mm
- Absence of infiltrating neutrophils
Cyclic Neutropenia Treatment:
- Antibiotics to control infection
- Oral hygiene maintenance
- Cytokine granulocyte colony-stimulating factor
- Splenectomy and nutritional supplement
Question 5. Hemophilia.
Answer:
Hemophilia
Hemophilia is a potentially fatal inherited bleeding disorder characterized by profound hemorrhage due to the deficiency of clotting factors
Etiology:
- Hereditary
- Sex-linked recessive trait
- Spontaneous mutations
Hemophilia Types:
- Hemophilia A – Due to factor 8 deficiency
- Hemophilia B – Due to factor 9 deficiency
- Hemophilia C – Due to factor 11 deficiency
- Von Willebrand’s disease
Hemophilia Clinical Features:
- Initially diagnosed in infancy
- Characterized by
- Easy bruising
- Prolonged bleeding after trauma
- Bleeding into the subcutaneous tissue
- Hematoma formation
- Nose-fatal epistaxis
- GIT – Gastric hemorrhage
- Joints – Recurrent hemarthrosis
- Osteoporosis
- Brain – Intracranial hemorrhage
- Urinary tract – hematuria
Hemophilia Oral Manifestations:
- Gingiva-Severe hemorrhage
- Soft tissue – Hematoma formation
- Jaw – Recurrent subperiosteal hematoma
- Tumor-like malformations
- Teeth – High caries index
- Severe periodontal disease
- Oropharyngeal bleeding
- Severe bleeding at the injection site
Hemophilia Treatment:
- Replacement therapy by the use of fresh frozen plasma
- Administration of Factor 8
- Prevention of complications by the use of a synthetic analog of anti-diuretic l-diamino-8-d-arginine vaso¬pressin
- Genetic counseling – To prevent inheritance of the condition
Question 6. Lab Investigations for anemia.
Answer:
1. Haemoglobin Estimation:
- If the hemoglobin value is below the lower limit of the normal range for a particular age and sex, the patient is said to be anemic
- Several methods are available but the most reliable and accurate is the cyanmethaemoglobin method utilizing Drab Kin’s solution and spectrophotometer
- Normal values
- Males – 13-18 g/dl
- Females – 11.5 – 16.5 g/dl
2. Peripheral Blood Film Examination:
The blood smear is evaluated in an area where there is neither rouleaux formation nor so thin as to cause red cell distortion
- Variation In Size:
- Normally, red cell diameter varies from 6.7 to 7.7 pm
- Macrocytes (larger than normal) are found in megaloblastic anemia, aplastic anemia
- Microcytes (smaller than normal) are found in iron deficiency anemia, thalassemia
- Variation In Shape (Poikilocytosis):
- It is produced in megaloblastic anemia, iron deficiency anemia, hemolytic anemia
- Inadequate Hemoglobin Formation:
- Lower hemoglobin content develops in iron deficiency anemia
- Increased hemoglobin content develops in megaloblastic anemia
3. Red Cell Indices:
- In iron deficiency anemia, MCV, MCH, and MCHC are reduced
- In megaloblastic anemia, MCV is raised
4. Erythrocyte Sedimentation Rate:
- Anaemia causes a rise in the ESR
5. Reticulocyte Count:
- To assess the marrow erythropoietic activity
Question 7. Diagnostic Test of Pernicious Anaemia.
Answer:
Diagnostic Test of Pernicious Anaemia
- Hypergastrinaemia:
- Pentagastrinaemia:
- Haematologic findings:
- Haemoglobin – below the normal range
- Red cells – Macrocytes
- Reticulocyte count – lower than normal
- Red cell indices – MCV – elevated
- MCH – elevated
- MCHC – Normal or reduced
- Leukocytes – Reduced
- Platelets – moderately reduced
- Biochemical Alterations:
- Serum bilirubin, LDH, haptoglobin, ferritin, and iron – increased
- Red cell folate – reduced
- Schilling Test: Abnormal due to intrinsic factor deficiency
Question 8. Diagnostic Test for Bleeding Disorders.
Answer:
1. Investigations Of Disordered Vascular Hemostasis
- Bleeding Time:
- It is based on the principle of formation of a hemostatic plug following a standard incision on the volar surface of the forearm and the time the incision takes to stop bleeding is measured
- Normal – 3-8 minutes
- Hess Capillary Resistance Test:
- This test is done by typing the sphygmo-manometer cuff to the upper arm and raising the pressure in it between diastolic and systolic for 5 minutes.
- After deflation, the number of petechiae appearing in the next 5 minutes in a 3cm² area over the cubital fossa is counted
- The presence of more than 20 petechiae is considered a positive test
2. Investigation Of Blood Coagulation:
- Screening Tests
- Whole Blood Coagulation Time:
- The estimation of whole blood coagulation time done by various capillary and tube methods
- Normal value – 4-9 minutes
- Activated Partial Thromboplastin Time (PTTK):
- This test is used to measure the intrinsic system factors as well as factors common to both intrinsic and extrinsic systems
- One-stage prothrombin time (PT) – It measures the extrinsic system factor VII as well as factors in the common pathway.
- Special Tests:
- Coagulation Factor Assays: These are based on the results of PTTK or PT tests.
- Quantitative Assays: The coagulation factors can be quantitatively assayed by immunological and other chemical methods
Question 9. Oral manifestations of Anaemia.
Answer:
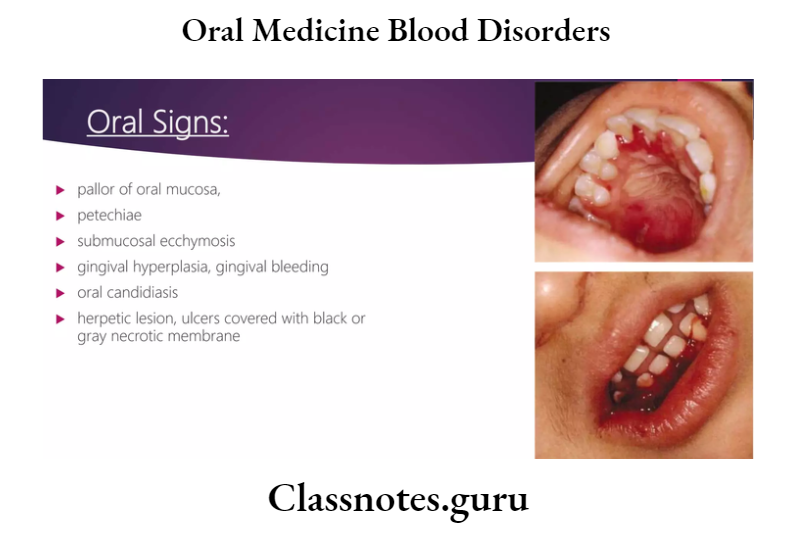
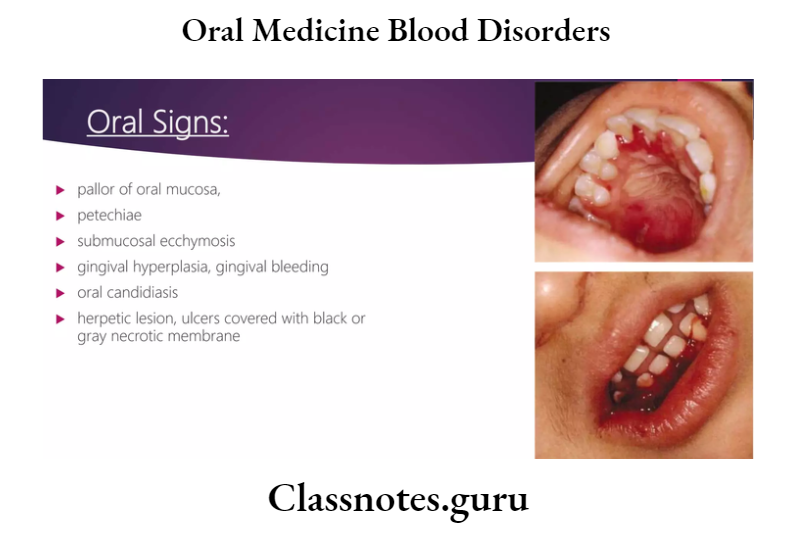
Oral Manifestations of Anaemia
- Mucosa – There is pallor of oral mucosa
- Generalized atrophy of mucosa occurs
- Tongue – Redness, soreness, or burning of tongue, Assuring of tongue
- Atrophy of papillae of the tongue
- Gingiva – Gingival enlargement
- Lip – Vermilion borders of the lip are very thin
- There is cracking and Assuring at the corner of the mouth
- Ulcers – Recurrent aphthous ulceration and candidiasis occur
- The width of the mouth is narrowed
- Throat – spasm in the throat
- Food sticking in the throat occurs
- Teeth – There may be delayed eruption
- Deposition of blood pigment in enamel and dentin
- Enamel hypoplasia
- Jaws – The patient is more prone to develop osteomyelitis due to hypervascularity of the bone marrow
- Nerves – Patient may present with paresthesia of men¬tal nerve
- Hypersensitivity and paresthesia
- Dysphagia
- Xerostomia – dryness of mouth
Question 10. Oral Manifestation of Leukemia.
Answer:
Acute Leukemia:
- Lymph nodes – submental, cervical, and pre and post-auricular lymph nodes may be enlarged and tender
- Lower lip – Paresthesia and crusting of the lower lip
- Chin – Paresthesia of chin
- Mucosa – The oral mucosa shows pallor, ulceration with necrosis, petechiae, ecchymosis, and bleeding ten¬dency
- There may be massive necrosis of lingual mucosa with sloughing
- Gingiva – It shows hypertrophy and cyanotic discolora-tion
- The gingiva appears boggy, edematous, and deep red bleeds easily due to ulceration of the sulcus epithelium and necrosis of underlying tissue
- Teeth – mobility of permanent teeth
- Infection – Candidial, viral, and bacterial infections occur frequently
Chronic Leukemia:
- Gingiva-Hypertrophy of gingiva
- There may be ulceration with necrosis and gangre¬nous degeneration
- Dark brown exudates and foul fetor oris are pre¬sent
- Tongue – It is frequently swollen and dark
- Lymph nodes – Regional lymphadenopathy
- Teeth – Rapid loosening of teeth
- Necrosis of periodontal ligament
- Destruction of alveolar bone
Question 11. ESR (Erythrocyte Sedimentation Rate).
Answer:
ESR (Erythrocyte Sedimentation Rate)
- ESR is a measure of the rate at which RBCs sediment in a tube of plasma
- ESR helps follow the progress of some chronic infections as well as diseases characterized by altered globulins such as collagen diseases, nephritis, rheumatic fever, and dysproteinemias
Erythrocyte Sedimentation Rate Technique:
- Mechanism
- The rate is accelerated when there are changes in the physicochemical properties of plasma or the red cell surface or when the changes in plasma protein cause the RBCs to aggregate
- Westergren Method:
- A graduated sedimentation tube is filled with oxalate blood and placed in a vertical position
- Results:
- The erythrocyte level is read at 10-minute intervals and the end of an hour.
Question 12. Lazy-leucocyte syndrome.
Answer:
Lazy-leucocyte Syndrome
- Lazy-leucocyte Syndrome is a result of the loss of chemotactic function of the neutrophils
Lazy-leucocyte syndrome Clinical Features:
- Age – Apparent at the age of 1-2 years
Lazy-leucocyte Syndrome Symptoms:
- Stomatitis
- Otitis media
- Bronchitis
- Recurrent infection
- Periodontitis
Lazy-leucocyte syndrome Diagnosis:
- Total WBC count – low
- Neutrophil count – 100-200 cells/mm3
- Bone marrow – Normal number of mature neutrophils
Lazy-leucocyte syndrome Management:
- Antibiotics – to control infections
Question 13. Plummer-Vinson Syndrome/Paterson-Brown- Kelly syndrome.
Answer:
Plummer-Vinson Syndrome
- Plummer-Vinson Syndrome is characterized by dysphagia, iron deficiency anemia, dystrophy of nails, and glossitis
Plummer-Vinson Syndrome Clinical Features:
- Age – It is found in middle age women
Plummer-Vinson Syndrome Symptoms:
- Dysphagia
- Angular cheilitis
- The patient may complain of spasms in the throat
- Sore mouth
- A smooth, red, and enlarged tongue
- Oral mucosa is pale and painful
- Dry mouth
- Spoon shaped nails
Plummer-Vinson Syndrome Diagnosis:
- Biopsy – It shows
- Atrophic epithelium
- Atrophy of lamina propria and muscles
Plummer-Vinson Syndrome Management:
- Correction of anemia
- Esophageal dilation
Question 14. Control of Bleeding.
Answer:
Control of Bleeding
- Bleeding in the surgical site around 48 hours after the surgical procedure is known as reactionary hemorrhage
- This is usually due to a local rise in blood pressure
- Bleeding seen after a week of the procedure is known as secondary hemorrhage
Bleeding Management:
- Pressure pack:
- A moist gauze with saline may be used to apply firm finger pressure on the area
- Local anesthetic pack:
- Local anesthesia with adrenaline can be used to temporarily control bleeding
- A gauze piece soaked in epinephrine may be placed
- Sutures:
- Bleeding from soft tissues may be controlled by placing sutures
- This helps to compress the mucosa against the bone and reduce bleeding
- Cautery:
- Bleeding from bone may be controlled by cauterization
- The exact bleeding spot is located first
- The area is dried as much as possible and a hot ball burnisher may be used to cauterize
- Electrocautery may also be used
- Ligation:
- If a major artery has been severed, it may need to be ligated.
- Gelfoam:
- This is a gelatin-based sponge that acts by disrupting platelets and establishing a framework with fibrin strands to create a clot
- It gets absorbed within 4-6 weeks
- Oxidized cellulose:
- It releases cellulosic acid
- This has a marked affinity for hemoglobin leading to the formation of an artificial clot
- These substances may be placed in the socket to enhance clot formation and control bleeding
- Bone wax:
- This is a mechanical agent to block the bleeding vessel
- Bleeding from bone may be occluded by placing a small piece of bone wax firmly on the spot of the bleeding
- The patient should be made to wait for half an hour in the dental clinic to confirm the absence of bleeding.
Question 15. Dental management of Haemophilia B.
Answer:
Dental Management Of Haemophilia B
- Anesthesia
- Local anesthesia is contraindicated in severe hae- -mesophilic patients
- If required, it should be given intramurally, in-parliamentary, and papillary
- Sedation with diazepam of nitrous oxide can be given
- Endodontic Treatment
- Common endodontic procedures can be provided
- Hemorrhage into the canal can be controlled with 1:1000 aqueous epinephrines
- Restorative
- Restorative procedures can be carried out
- Avoid the use of rubber dams to prevent trauma to the gingiva and other soft tissue
- The epinephrine-impregnated hemostatic cord can be used for gingival retraction
- Prosthodontics Treatment
- Complete dentures and partial dentures are well tolerated in hemophilic patients
- Periodontal Therapy
- Conservative therapy is acceptable
- Surgery requires replacement therapy
- Oral Surgical Procedure
- Local hemostatic agents and techniques are used
- After packing, the tooth socket must be protected by a mechanical splint to prevent disturbances to the clot
- The anti-fibrinolytic agent is used postoperatively
- Drugs Precaution
- Aspirin and other NSAIDs are avoided due to their antiplatelet function
- Intramuscular injection should be avoided owing to the risk of hematoma formation
- Electrosurgery
- Avoided as it causes tissue necrosis and haemor¬rhage
Oral Medicine Blood Disorders Short Answers
Question 1. Cyclic neutropenia
Answer:
Cyclic Neutropenia
Cyclic Neutropenia is an idiopathic disease characterized by episodic defects in neutrophil maturation in the bone marrow, resulting in periodic falls in circulating neutrophils
Cyclic Neutropenia Clinical Features:
- Recurrent upper respiratory tract infections
- Short-term fevers, sore throat
- Headache, arthritis, conjunctivitis
- Amyloidosis
- Regional lymphadenopathy, Gingivitis, ragged painful ulcers
Question 2. Four oral manifestations of aplastic anemia.
Answer:
Four Oral Manifestations Of Aplastic Anemia
- Petechiae and frank hematoma formation in the oral cavity
- Gingiva – Spontaneous bleeding
- Mucosa – Multiple ulcerations
- Persistent oral infections
- May lead to bacteremia and septicemia
Question 3. Oral manifestation of oral leukemia.
Answer:
Oral Manifestation Of Oral Leukemia
- Gingiva:
- Hypertrophy of gingiva
- Ulceration with necrosis and gangrenous degenera¬tion
- Dark brown exudates
- Foul fetor oris
- Tongue – Swollen and dark
- Lymph nodes – Regional lymphadenopathy
- Teeth-Loosening of teeth
- Necrosis of periodontal ligament
- Destruction of alveolar bone
Oral Medicine Blood Disorders Viva Voce
- Purplish discoloration of oral mucosa is found in primary polycythemia
- Delayed eruption and hypoplasia of dentition are found in sickle cell anemia
- The color of skin in thalassemia patients is ashen gray
- The bimaxillary protrusion is seen in Cooley’s anemia
- The beefy red tongue is found in pernicious anemia
- Spontaneous hemorrhage from the gingiva is a feature of aplastic anemia
- Spasm in the throat occurs in Plummer Vinson syn-drome
- Platelet count is used to evaluate primary hemostasis
- Haemophilia A is caused by a deficiency of Factor 8
- Microvascular infarcts are found in thrombotic thrombocytopenic purpura
- The labial frenum exhibits the most frequent bleeding in hemophilia
- DIC is treated by intravenous heparin
- The bald tongue of the sandwich is a feature of pernicious anemia
- Howell Jolly bodies are seen in pernicious anemia
- Safety pin cells are seen in thalassemia