Diseases Of The Kidneys And Genitourinary System Important Notes
- Rennin
- Rennin is an enzyme released from the chief cells of fundic glands of the stomach
- Rennin is milk milk-curdling enzyme
- Rennin is absent in man
- Polyuria is seen in
- Hypercalcemia
- Glycosuria
- Hypokalemia
- Acute nephritic syndrome
- Acute nephritic is characterized by sudden onset of renal failure and oliguria
- Renal blood flow and glomerular filtration rate falls
- Nephritic syndrome
- Nephritic is characterized by protein loss in the urine of more than 3.5 g proteinuria/day, fluid retention or edema, hypercoagulability, hypercholesterolemia, and infections
- Clinical features
- Splenomegaly
- Ascites
- Varices and collateral vessel formation
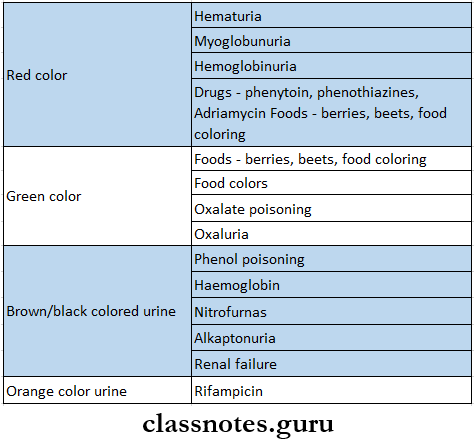
- Urine examination
Kidney diseases long answer questions
Diseases Of The Kidneys And Genitourinary System Long Essays
Question 1. Write about pathogenesis and treatment of acute glomerulonephritis.
(or)
Mention etiology, clinical features, complications, diagnosis, and management of acute glomerulonephritis.
(or)
A young person develops sudden facial puffiness. How do you investigate a case of acute glomerulonephritis, outline complications and treatment?
(or)
What are the causes and management of glomerulonephritis?
(or)
Describe the etiology, clinical features, complications, investigations, and management of acute nephritis.
(or)
Define acute nephritic syndrome. Discuss the clinical features and treatment of post-streptococcal acute glomerulonephritis.
Answer:
Glomerulonephritis/Acute Nephritis:
- It is an inflammation of the glomeruli and to a lesser extent the tubules of the kidney
Acute Nephritis Causes:
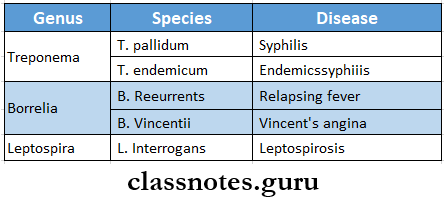
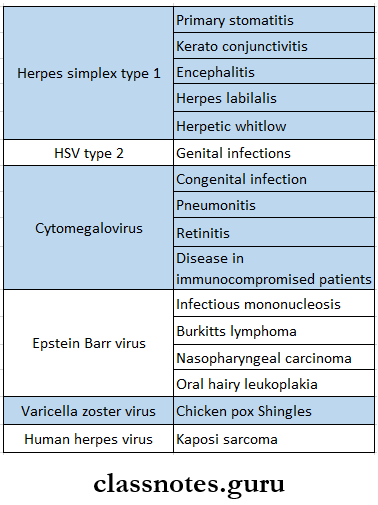
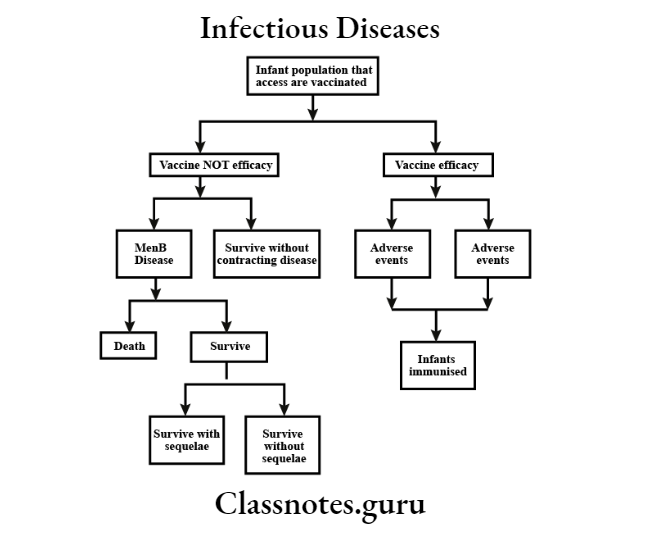
- Infectious diseases
- Post-streptococcal glomerulonephritis
- Non-streptococcal glomerulonephritis
- Bacterial
- Infective endocarditis
- Staphylococcal and pneumococcal infections
- Viral
- Hepatitis B
- Infectious mononucleosis
- Parasitic
- Systemic disorders
- Systemic lupus erythematosus
- Vasculitis
- Primary glomerular diseases
- Mesangiocapillary glomerulonephritis
- Miscellaneous
- Serum sickness
- IgA nephropathy
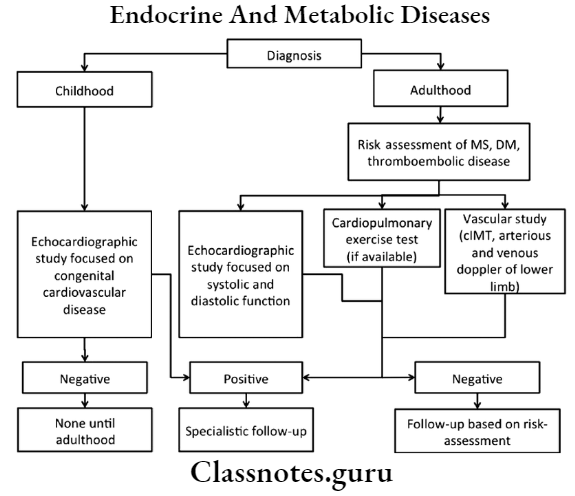
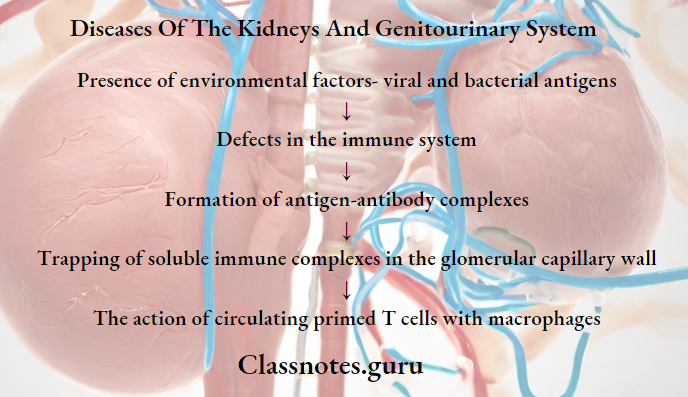
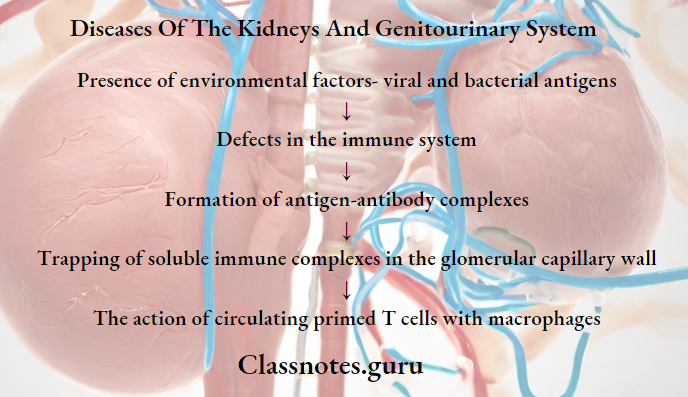
Pathogenesis:
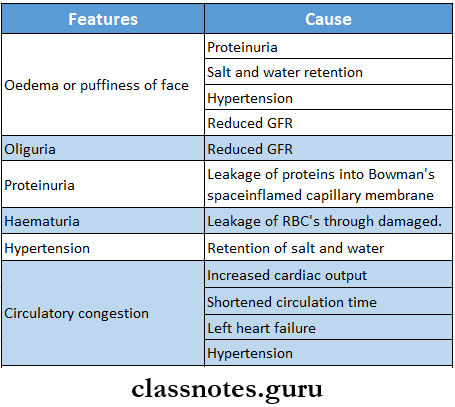
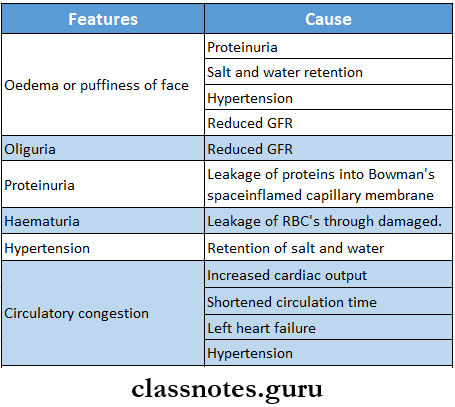
Acute Nephritis Clinical Features:
Acute Nephritis Complications:
- Hypertensive encephalopathy
- Pulmonary edema
- Uraemiaete
Long essay on renal and urinary tract diseases
Read And Learn More: General Medicine Question and Answers
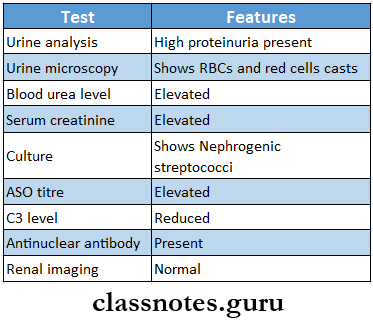
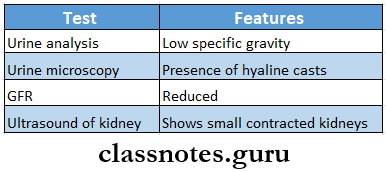
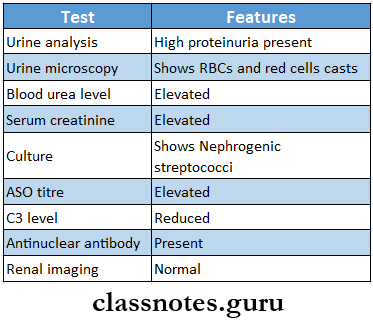
Acute Nephritis Diagnosis:
Acute Nephritis Management:
- Bed rest
- To improve acute symptoms
- Diet
- Restriction on dietary protein, sodium, and potassium intake
- Restriction on fluid intake
- Treatment of infection
- Procaine penicillin IM for 6 days is used to treat streptococcal infections
- Treatment of hypertension
- Diuretics are used
- Enalapril 2.5-10 mg daily is used
- Dialysis
- Required if there is presence of fluid overload
Acute Nephritic Syndrome or Acute Glomerulonephritis:
- It is an inflammation of the lomeruli and to la esser extent the tubules of the kidney
Post Streptococcal Acute Glomerulonephritis:
- It follows an acute streptococcal infection of the throat or skin
Question 2. Describe clinical features, diagnosis, and management of nephrotic syndrome.
(or)
Definenephroticc syndrome. Describe clinical features, investigations, and treatment of nephrotic syndrome.
(or)
Describe ethe tiology, clinical features, investigations, and management of the nephrotic syndrome.
(or)
Mention the causes of nephrotic syndrome. Describe clinical features, diagnosis, and treatment.
Answer:
Nephrotic Syndrome:
Nephrotic Syndrome Definition:
- It refers to massive proteinuria of ore than 3.5 g/day mainly of albumin, reduced albumin concentration, edema, hhyperlipidemia lipiduria, and hypercoagulability
Nephrotic Syndrome Causes:
- Primary renal disorders
- Minimal lesion
- Membranous glomerulonephritis
- Mesangioproliferative glomerulonephritis
- Focal glomerulosclerosis
- Secondary nephrotic syndrome
- Infections- malaria
- Following hepatitis B infection
- Complication of infective endocarditis
- Syphilis
- Following collagen disease
- Metabolic diseases- diabetes mellitus
- Hereditary
- Drugs- Gold, mercury, penicillamine, captopril, antitoxins
Nephrotic Syndrome Clinical Features:
- Edema-puffiness of eyelids or periorbital edema
- Generalised anasarca
- Ascites
- Bilateral pleural effusion
- Pulmonary edema
- Fever due to infection
- Arterial and venous thrombosis
- Pulmonary embolism
- Renal vein thrombosis
- Hypertension
- Hematuria
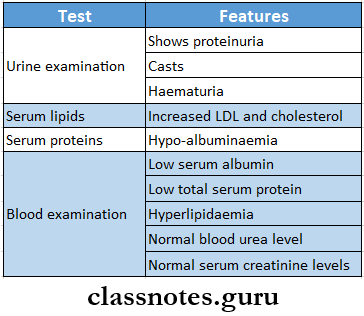
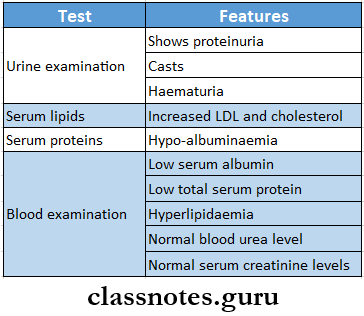
Nephrotic Syndrome Diagnosis:
Nephrotic Syndrome Management:
- Relief of edema
- Restriction of salt
- Use of diuretics
- Frusemide-80-120 mg/ daily
- In severe cases ,salt-free albumin- 20 g in 100 ml in 1 hour or plasma albumin intravenous infusion is used
- Control of proteinuria
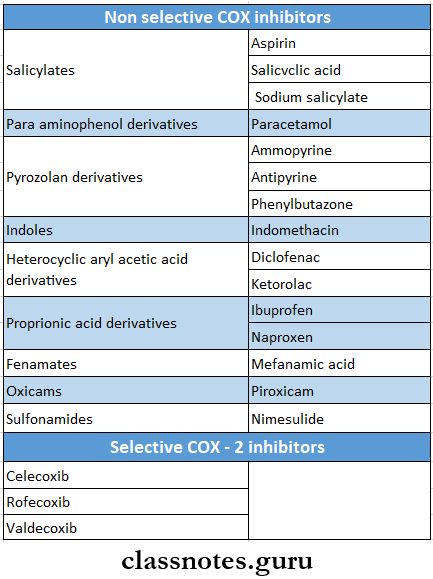
- ACE inhibitors, angiotensin receptor blockers, and NSAIDs are used
- Treatment of hyperlipidemia
- Lipid-lowering agent, atorvastatin 20 mg is used
- Immunosuppressive therapy
- Corticosteroids are given for 6-8 weeks at the dose of 1 mg/ kg daily
- Control of infection
- Antibiotics like cephalexin iareused
- Anti-coagulants
Genitourinary system disorders long essays
Diseases Of The Kidneys And Genitourinary System Short Essays
Question 1. Uraemia
Answer:
Uraemia
- Uremia is a clinical state in which the blood urea nitrogen level, an indicator of nitrogen waste products, is elevated.
Uraemia Clinical Features:
- Confusion,
- Loss of consciousness,
- Low urine production,
- Dry mouth,
- Fatigue,
- Weakness,
- Pale skin or pallor,
- Bleeding problems,
- Rapid heart rate (tachycardia),
- Edema (swelling), and
- Excessive thirst.
- Uremia may also be painful.
Uraemia Treatment:
- Immediate treatment for uremia (within the first 24 hours after diagnosis) is needed to stabilize the patient and address the cause of uremia. Immediate treatment for uremia may include:
- Blood products
- Blood transfusions
- Fluid therapy
- Hemodialysis (Filtering blood outside the body)
- Hospitalization
- Intravenous fluid
- Medication to increase blood pressure and cardiac output such as dopamine
- Ongoinguremia treatment
- Long-term treatment for uremia may include:
- Dialysis
- Dietary modification
- Medication
Uraemia Complications:
- Complications of uremia include:
- Anemia
- Bleeding disorders (delayed blood clotting, platelet dysfunction)
- Cardiac arrest
- Fragile bones
- Kidney failure
- Malnutrition
- Respiratory failure
- Sexual dysfunction
Question 2. Proteinuria
Answer:
Proteinuria
- Urine containing more than 150 mg of proteins is called proteinuria
Proteinuria Tests:
- Heat coagulation method
- Electrophoresis of proteins
- Dipstick test
- Immunoelectrophoresis
- Radioimmunoassay
Etiopathogenesis:
- Tubular proteinuria
- Produces damage more to tubules than to glomeruli
- Urine contains more than 1-3 g/day of proteins
- Glomerular proteinuria
- Glomerular injury occurs
- Albuminuria occurs
- Asymptomatic proteinuria
- Common in younger individuals
- It is postural or exercise-induced
- There is presence of hypertension, haematuria, and impaired renal function
- Orthostatic proteinuria
- Persons passa an amount of proteins in the urine during the day assuming an upright posture
- Microalbuminuria
- Contains 30-300 mg/ day albumin in urine
- Bence-Jones proteinuria
- Contains Bences Jonces proteins in urine
- Identified by immunoelectrophoresis of urine
Question 3. Diuretics
Answer:
Diuretics
- Drugs that increase urine and solute excretion causing loss of sodium and water from the body are called diuretics.
Diuretics Classification:
- High efficacy or loop diuretics Furosemide, Bumetanide, Torasemide
- Medium efficacy diuretics
- Benzothiadiazine or thiazides Hydrochlorothiazide, Benzthiazide
- Thiazides like drugs Chlorthalidone, Metolazone
- Low efficacy or weak diuretics
- Carbonic anhydrase inhibitors Acetazolamide
- Potassium-sparing diuretics Aldosterone antagonist- spironolactone Inhibitors of renal epithelial sodium channel- Triamterene, amiloride
- Osmotic diuretics Mannitol, isosorbide, Glycerol
Chronic kidney disease (CKD) long essay
Question 4. Management of renal colic
Answer:
Management Of Renal Colic
- Treatment for renal colic and kidney stones involves reducing pain and breaking up the stones.
- In some cases, kidney stones may pass on their own, allowing symptoms of renal colic to resolve.
- However, it is common for kidney stones to recur.
- Drinking plenty of fluids may help the stone to pass and may lessen the pain of renal colic.
Renal Colic Medications Used Are:
- Allopurinol (for uric acid kidney stones)
- Alpha-blocker medications to help stones pass
- Antibiotics to clear infections
- Cystine control medications to reduce cystine levels in urine
- Diuretics
- Pain medications
- Potassium citrate or sodium bicarbonate regulates urine pH and ppreventsstone formation
- Sodium cellulose phosphate to bind calcium in the intestine
- Other treatments for renal colic
- Heat therapy (For pain)
- Lithotripsy (Use of ultrasonic vibration to break down kidney stones)
- Surgery to remove large stones
- Ureteral stent placement, to keep the urine tubes from the kidneys to the bladder (Ureters) open
- Ureteroscopy (Minimally invasive surgery)
Diseases Of The Kidneys And Genitourinary System Short Answers
Question 1. Frusemlde
Answer:
Frusemlde
- It is high efficacy’- diuretics
Frusemlde Uses:
- Edema
- Hypertension
- Forced diuresis
- Hypercalcaemia
- Renal stones
- During blood transfusions
Frusemlde Adverse Effects:
- Acute salt depletion
- Hepatic coma
- Photosensitivity
- Headache
- Giddiness
- Nausea, vomiting
- Paresthesia, impotence
Urinary tract infection (UTI) long essay
Question 2. Renal colic
Answer:
Renal Colic Clinical Features
- Pain, especially in the back, side, or groin;
- Blood in the urine; abnormally colored urine;
- Fever;
- chills; and
- Nausea with or without vomiting.
Renal Colic Causes:
- Bowel disease
- Surgery
- Genetics
- Certain dietary’ factors, or
- Diseases, such as ccystinuria
Question 3. Haematuria
Answer:
Haematuria Causes:
- Renal disorders
- Trauma
- Glomerular disease
- Carcinoma
- Extrarenal disorders
- Trauma
- Injections
- Urethritis
- Prostatitis
- Systemic disorders
- Vasculitis
- Bleeding diseases
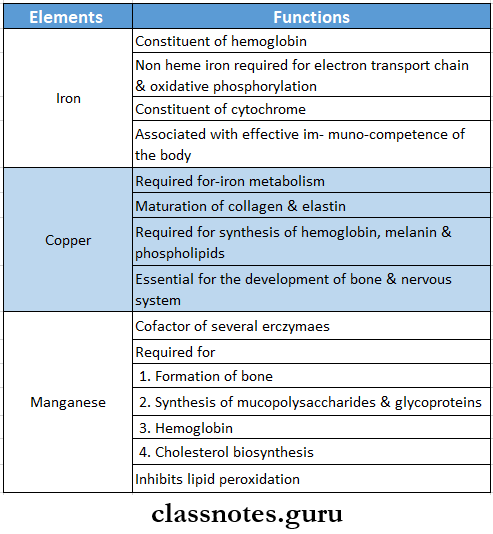
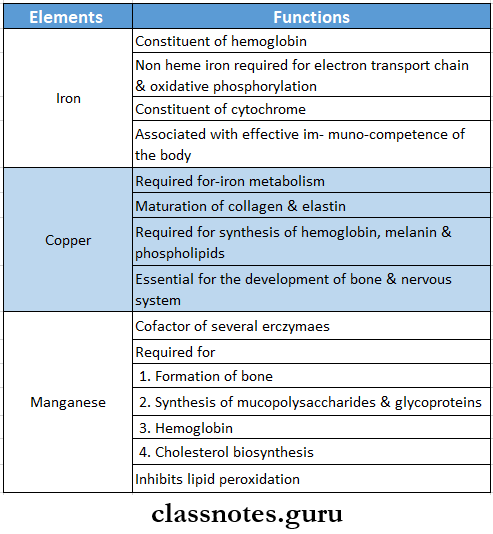
Question 4. Trace elements
Answer:
Trace elements
Glomerulonephritis long answer question
Question 5. Nephrotic syndrome
Answer:
Nephrotic Syndrome Definition:
- Nephrotic Syndrome refers to massive proteinuria mof ore than 3.5 g/ day mainly of albumin, reduced albumin concentration, oedema hyperlipidemia, lipiduria, and hypercoagulability
Nephrotic Syndrome Clinical Features:
- Edema-puffiness of eyelids or periorbital edema
- Generalised anasarca
- Ascites
- Bilateral pleural effusion n Pulmonary edema
- Fever due to infection
- Arterial and venous thrombosis
- Pulmonary embolism
- Renal vein thrombosis
- Hypertension
- Hematuria
Question 6. Uraemia
Answer:
Uraemia
- Uremia is a clinical state in which the blood urea nitrogen level, an indicator of nitrogen waste products, is elevated.
Uraemia Clinical Features:
- Confusion
- Loss of consciousness
- Low urine production
- Dry mouth
- Fatigue
- Weakness
- Pale skin or pallor
- Bleeding problems
- Rapid heart rate (tachycardia)
- Edema (swelling), and
- Excessive thirst
- Uremia may also be painful.
Question 7. Complications of acute nephritis
Answer:
Complications Of Acute Nephritis
- Hypertensive encephalopathy
- Pulmonary edema
- Uraemiaete
Question 8. Acute renal failure
Answer:
Acute Renal Failure Definition
- Acute Renal Failure is defined as sudden and usually reversible deterioration of renal function developing ooverdays or weeks with rapid rise in blood urea
Acute Renal Failure Causes:
- Pre renal causes
- Hemorrhage
- Severe burns
- Crushing injuries
- Shock
- Hypovolaemia
- Septicaemia
- Cardiac failure
- Intra renal causes
- Vasculitis
- Renovascular obstruction
- Acute tubular necrosis
- Urinary tract obstruction
Acute Renal Failure Clinical Features:
- Oliguria
- Anuria
- Reduced GFR
- Septicaemia
- Acute ischemia
Question 9. Chronic renal failure- three laboratory abnormalities
Answer:
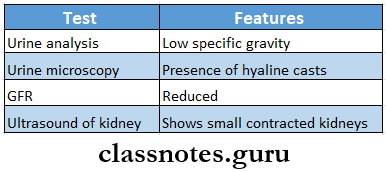
Nephrotic syndrome long essay for exams
Question 10. Treatment of chronic renal failure
Answer:
Treatment Of Chronic Renal Failure
- Treatment of hypertension
- Salt restriction
- Use of diuretics and ACE inhibitors or angiotensin receptor blockers
- Diet
- Protein restriction
- Salt restriction
- Fluid restriction
- Treatment of anemia
- Blood transfusion when hemoglobin level falls below 5 g/dl
- Treatment of metabolic acidosis
- Use of intravenous sodium bicarbonate 1 g/8 hourly
- Treatment of infections
- Treatment of renal osteodystrophy
- Administration of 1 alpha-hydroxycholecalciferol or 1,25 di- hydroxycholecalciferol- 0.25-1 microgram/day
- Dialysis and renal transplantation
Question 11. Diabetic nephropathy
Answer:
Diabetic Nephropathy
- It is a evere complication of diabetes mellitus
- Occurs in both types
Diabetic Nephropathy Features:
- Asymptomatic proteinuria
- Nephrotic syndrome
- Progressive Renal failure
- Hypertension
Question 12. Acute tubular necrosis
Answer:
Acute Tubular Necrosis
- There are clinically three distinct stages of acute tubular necrosis
- They are:
- Oliguric phase
- Patient passes less than 500 ml of urine per day
- Urine contains proteins, casts, and cells
- SThe specificgravity of urine is about 1.010 or more
- Phase persists for 10-14 days
- Diuretic phase
- Patient passes large amount of solute-free urine 3-5 litres/day for 3-5days
- Recovery phase
- It occurs after 7-20 days
- Urine volume becomes normal
Question 13. Define- nephrotic syndrome
Answer:
Nephrotic syndrome
- It refers to massive proteinuria mof ore than 3.5 g/day mainly of albumin, reduced albumin concentration, oedema hyperlipidemia, lipiduria, and hypercoagulability
Question 14. Importance of urine analysis
Answer:
Importance Of Urine Analysis
- Urine analysis is saimple procedure used for diagnosing, screening, and treating infections
- For it, urine is collected in
Urine Analysis Uses:
- For urinary tract infections
- For kidney disorders
- in chrome disorders like diabetes mellitus
- In infections like polyuria
- In combination owithother tests
Urine Analysis Importance:
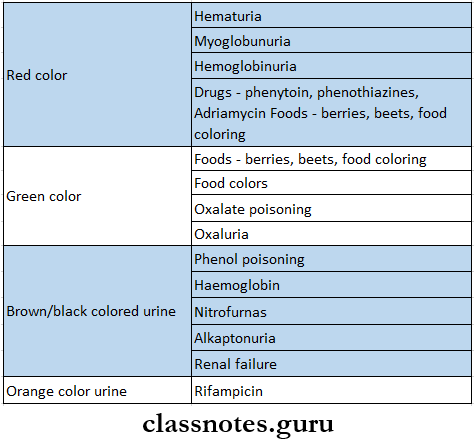
- Gross examination of urine- color ami consistency
- Microscopic examination- casts, cells present in urine
- prof urine
- The specific gravity of urine
- Presence of proteins
- Presence of glucose
Renal failure pathophysiology long essay
Question 15. Drugs causing kidney damage
Answer:
Drugs Causing Kidney Damage
- Drugs causing damage to kidneys are:
- Cyclosporine
- Aminoglycosides antibiotics
- Cisplatin
- Amphotericin B
- Beta lactam antibiotics
- Indomethacin
VIVA VOCE
- The presence of albumin m urine is a sign of glomerular abnormally
- Glomerular filtration «eases when systolic blood pressure falls below 70 mm of Hg