Diseases Of Cardiovascular System Short Answers
Question 1. Coronary vasodilators
Answer:
Coronary Vasodilators
They reduce the mortality in patients with cardiac failure
They are:
- Arteriolar dilators – hydralazine, minoxidil
- They relax arterial smooth muscles thus reducing peripheral vascular resistance and afterload
- Venodilators – nitrates
- They reduce the venous return to the heart
- This reduces the stretching of the ventricular walls and myocardial oxygen requirements
- Arteriolar and venular dilators – sodium nitro- pride, ACE inhibitors, prazosin, calcium channel blockers
- They reduce both preload and afterload
Question 2. Four causes of acute left ventricular failure
Answer:
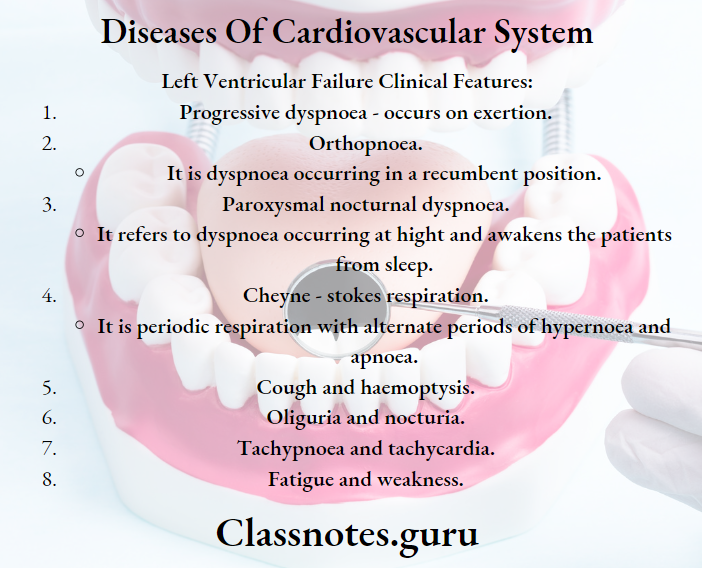
Four Causes Of Acute Left Ventricular Failure
- Left ventricular outflow obstruction
- Systemic hypertension
- Coarctation of aorta
- Aortic valvular stenosis
- Left ventricular inflow obstruction
- Left ventricular volume overload
- Mitral valve prolapsed
- Mitral regurgitation
- Aortic regurgitation
- Ventricular septal defect
- Reduced left ventricular contractility
- Cardiomyopathy
- Anterior wall myocardial infarction
Read And Learn More: General Medicine Question and Answers
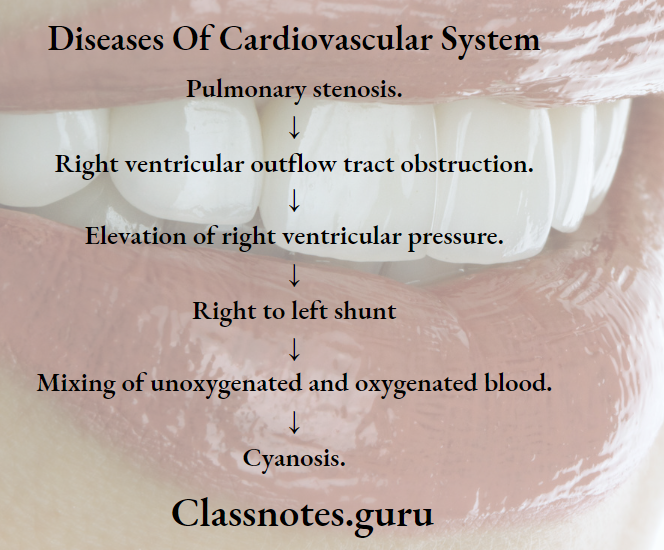
Question 3. Cyanosis.
Answer: Cyanosis
Definition: Bluish discoloration of skin and mucous membrane is called cyanosis.
Cyanosis Sites Involved:
- Lips a Nail beds
- Fingertips
- Ear lobule.
- The undersurface of the tongue.
- Malar eminence
- Creases of palms.
Cyanosis Types:
- Peripheral cyanosis.
- Central cyanosis.
Cardiovascular diseases short answers
Question 4. Causes of central cyanosis.
Answer:
Causes Of Central Cyanosis
- Pulmonary causes
- High altitude
- Pneumonia
- Pneumothorax
- COPD
- Severe acute asthma
- Respiratory failure.
- Cardiovascular causes.
- Acute pulmonary edema.
- Cyanotic heart disease.
- Blood disorders.
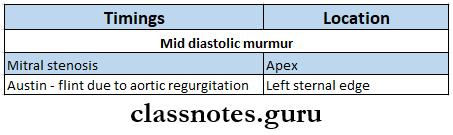
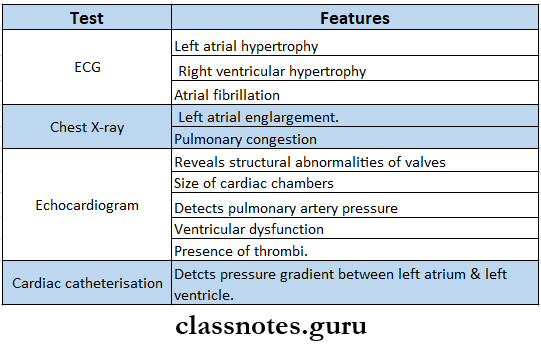
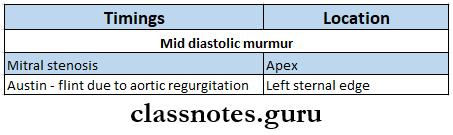
Question 5. Mid-diastolic murmur.
Answer:
Mid-Diastolic Murmur
Mid-diastolic murmur is a trembling murmur heard at the apex.
Mid-Diastolic Murmur Causes:
- Dilatation of left ventricle,
- Functional mitral regurgitation.
Question 6. Bradycardia – causes.
Answer:
Sinus Node Dysfunction:
- Myocardial infarction.
- Hypothermia.
- Hypothyroidism.
- Obstructive jaundice.
- Raised intracranial pressure
- Typhoid fever
- Drugs like digoxin, calcium channel blockers, and beta-blockers.
Question 7. Tachycardia.
Answer:
Tachycardia
A heart rate of more than 100 per minute due to any cause is called tachycardia.
Tachycardia Causes:
- Physiological
- Exercise
- Emotion
- Fear
- Smoking.
- Excessive consumption of tea, coffee, etc.
- Pathological.
- Anxiety.
- Fever
- Thyrotoxicosis.
- Anaemia.
- Heart failure
- Hypo or hypertension
- Pheochromocytoma.
- Drugs – bronchodilators.
Tachycardia Types:
- Supraventricular tachycardia.
- Ventricular tachycardia.
Heart diseases Q&A
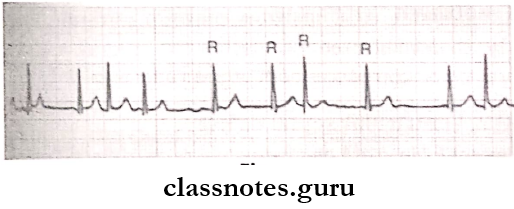
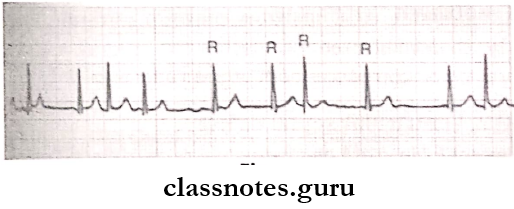
Question 8. Atrial fibrillation.
Answer:
Atrial Fibrillation
Atrial fibrillation is the most common cardiac arrhythmia.
- The atrial rate is more than 350 beats/min.
Atrial Fibrillation Causes:
- Coronary artery disease
- Rheumatic valvular disease
- Idiopathic
- Cardiomyopathy
- Thyro toxicosis.
- Alcoholism.
- Congenital heart disease.
- Pulmonary embolism.
Atrial Fibrillation Treatment:
- Treat the cause
- Anti-arrhythmic drugs,
- Anti-coagulant.
- Defibrillation.
Question 9. Cardiac arrest.
Answer:
Cardiac Arrest
Definition: It is defined as the sudden complete arrest of heart function.
Cardiac Arrest Causes:
- Ventricular fibrillation
- Ventricular asystole.
- Electromechanical dissociation.
Cardiac Arrest Clinical Features:
- Absence of pulses.
- Cold extremities.
- Loss of consciousness.
- Cessation of respiration.
- No heartbeat.
Cardiac Arrest Management:
- A – airway.
- Clear mouth and airway.
- Extend neck and raise chin.
- B-breathing.
- Direct mouth-to-mouth breathing.
- Indirect mouth-to-mouth breathing.
- C-circulation.
Common heart disorders short questions
Question 10. Heart failure.
Answer:
Heart Failure
Heart failure denotes a pathophysiologic state when the heart is not able to maintain its cardiac output to meet the demands of metabolizing tissues.
Heart Failure Types:
- Acute and chronic.
- Compensated and decompensated
- Right, left, and biventricular heart failure.
- Forward and backward heart failure.
- Systolic and diastolic heart failure.
- High and low output failure.
Question 11. Treatment of cardiac failure.
Answer:
Treatment Of Cardiac Failure
- General measures.
- Bed rest
- Regular isotonic exercises
- Low-calorie intake.
- Salt restriction.
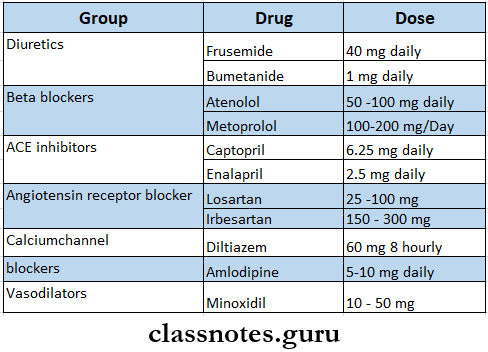
- Drug therapy.
- Digitalis – digoxin – 0.25 – 0.5 mg/ day
- Sympathomimetic amine – dopamine, dobutamine.
- Diuretics – thiazides, loop diuretcis, potassium sparing.
- Vasodilators – ACE inhibitors – captopril – 12.5 – 25 mg TID.
- Cardiac transplantation.
Question 12. Complications of heart failure.
Answer:
Complications Of Heart Failure
- Acute renal failure.
- Hypokalemia.
- Hyponatraemia.
- Jaundice.
- Deep vein thrombosis.
- Arrhythmias.
- Systemic embolism.
Question 13. Congenital heart disease.
Answer:
Congenital Heart Disease Clinical Features:
- Central cyanosis.
- Growth retardation.
- Syncope
- Stature
Etiology:
- Infections – rubella infection.
- Chromosomal defects – Down’s syndrome.
- Connective tissue disorders,
- Alcohol abuse.
Question 14. Classification of congenital heart disease.
Answer:
Classification Of Congenital Heart Disease
- Acyanotic.
- Acyanotic with left to right shunt.
- Atrial septal defect.
- Ventricular septal defect.
- Patent ductusarteriosus.
- Acyanotic without shunt.
- Pulmonary stenosis.
- Aortic stenosis.
- Coarctation of aorta.
- Cyanotic.
- Complete transposition of great vessels.
- Tetralogy of Fallot
- Persistent truncus arteriosus.
Coronary artery disease short question answer
Question 15. Atrial septal defect.
Answer:
Atrial Septal Defect
It is a cyanotic heart disease with a left to right shunt through a defect in the interatrial septum.
Atrial Septal Defect Types:
- Ostium secundum defect – Involves fossa ovalis.
- Ostium primum defect.
- Lies in the common atrioventricular canal.
Atrial Septal Defect Features:
- Asymptomatic.
- Good volume pulse
- Systolic murmur.
- Diastolic flow murmur.
- Wide and fixed splitting of the second heart.
- Chest X-ray – shows an enlargement of the heart.
- ECG – shows incomplete or complete right bundle branch block.
- Echocardiogram – shows right ventricular dilatation, hypertrophy.
- Color Doppler – measures flow velocities.
Atrial Septal Defect Treatment:
- Surgical closure of the defect.
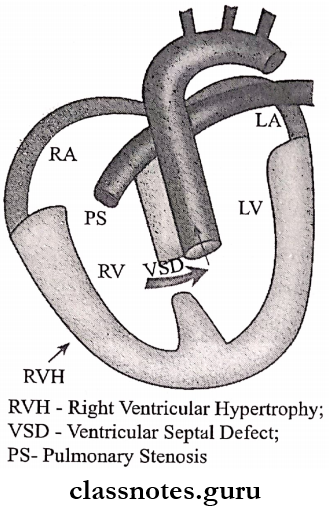
Question 16. Fallor tetralogy.
Answer:
Fallot Tetralogy Components:
- Pulmonary stenosis.
- Ventricular septal defect.
- Over-riding of the aorta.
- Right ventricular hypertrophy.
Fallot Tetralogy Clinical Features:
- Cyanosis – develops after 1 year of age.
- The child may become apnoeic and may fall unconscious.
- Growth retardation.
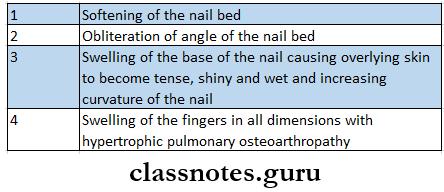
- Grade 4 clubbing.
- Polycythaemia.
- Ejection systolic murmur.
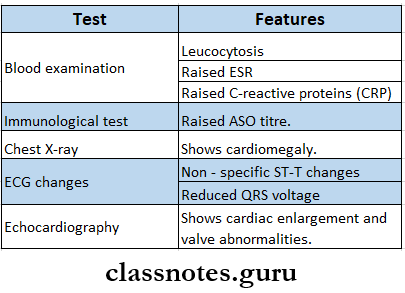
Question 17. Rheumatic fever/Jone’s criteria.
Answer:
Rheumatic Fever/Jone’s Criteria
Rheumatic Fever is an acute inflammatory disease that occurs as a complication of group A streptococcal infection.
Rheumatic Fever Clinical Features:
- Jone’s criteria.
- Major criteria.
- Carditis
- Polyarthritis
- Chorea
- Erythema marginatum
- Subcutaneous nodules.
- Minor criteria.
- Fever
- Arthralgia.
- Raised ESR
- Previous history of rheumatic fever.
- Positive CRP.
Hypertension short answer format
Question 18. Aortic regurgitation – signs.
Answer:
Collapsing Or Good Volume Pulse:
- Bounding peripheral pulses.
- Corrigan’s sign-dancing carotids.
- Quincke’s sign-capillary pulsation in nail beds.
- Duroziez’s sign.
- Pistol shots sound.
- De Musset’s sign – head nodding with a carotid pulse.
- Cyanosis.
- Pitting ankle oedema.
- Tender hepatomegaly.
Question 19. Infective endocarditis.
Answer:
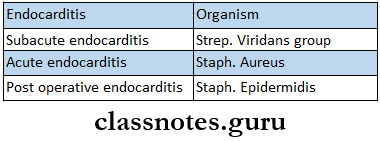
Infective Endocarditis
Infective Endocarditis is a microbial infection of the mural endocardium a heart valve or valves or lining of blood vessels.
Question 20. Complications of infective endocarditis.
Answer:
Complications Of Infective Endocarditis
If not treated, infective endocarditis may lead to.
- Stroke
- Organ damage
- Spread of infection to other body parts
- Heart failure.
- Septic embolization
- Mycotic aneurysm.
- Neurologic complications.
- Renal complications.
- Musculoskeletal complications.
Question 21. Complications of hypertension.
Answer:
Complications Of Hypertension
- Central nervous system.
- Cerebral atheroma
- Transient cerebral ischaemic attacks
- Stroke.
- Hypertensive encephalopathy
- Subarachnoid hemorrhage.
- Retinopathy.
- Heart
- Left ventricular hypertrophy.
- Cardiac failure.
- Kidney
Atherosclerosis question and answer
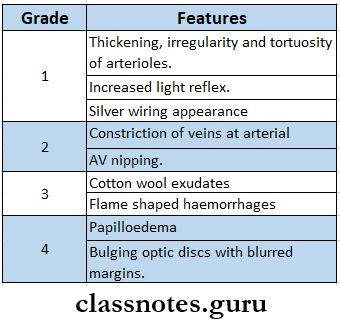
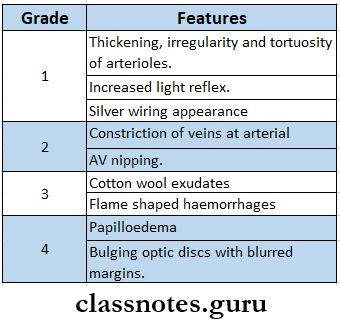
Question 22. Hypertensive retinopathy.
Answer:
Hypertensive Retinopathy
It is an ophthalmic complication of hypertension.
Grades:
- Cardiac causes
- Malignant arrhythmias.
- Ischaemic heart disease
- Heart blocks
- Valvular heart disease
- Infective endocarditis
- Myocarditis
- Cardiomyopathy.
- Thromboembolism.
- Idiopathic.
Question 23. Causes of sudden death in myocardial infarction.
Answer:
Causes Of Sudden Death In Myocardial Iinfarction
- Noncardiac causes
- Cerebral hemorrhage.
- Ruptured aortic aneurysm.
Question 24. Risk factors for coronary artery disease.
Answer:
Old Age:
- Sex – common in males
- Family history
- Smoking, alcohol.
- Hypertension.
- Mental stress Hypercholesterolemia.
- Diabetes mellitus.
- Sedentary habits
- Obesity
- Polyunsaturated fatty acid deficiencies
- Hyperfibrinogenaemia.
- Low levels of anti-oxidant vitamins
- Protein S and C deficiency.
Question 25. Aspirin.
Answer:
Aspirin
Aspirin is a non-selective COX inhibitor.
Aspirin Uses:
- As analgesic
- Fever
- Arthritis, fibromyositis
- Acute rheumatic fever
- Rheumatoid arthritis
- Osteoarthritis.
- Postmyocardial infarction.
- Inflammatory bowel disease.
Aspirin Adverse Effects:
- Nausea, vomiting, epigastric distress.
- Headache, dizziness, confusion.
- Allergic reactions – rashes, urticaria, photosensitivity.
- Hemolysis.
- Nephrotoxicity.
- Hepatotoxicity.
- Reye’s syndrome.
- Salicylism.
Heart failure short questions
Question 26. Oral anticoagulants.
Answer:
Oral Anticoagulants
Oral anticoagulants are drugs given orally to reduce the coagulability of blood.
Oral Anticoagulants Classification:
- Coumarin derivative.
- Bishydroxycoumarin, warfarin sodium, acenocoumarol.
- Indanedione derivative.
Oral Anticoagulants Uses:
- Venous thrombosis
- Pulmonary embolism.
- Post-operative, post-stroke patients.
- Rheumatic valvular disease.
- Unstable angina.
- Vascular surgery.
Question 27. Beta-blockers – uses.
Answer:
Hypertension:
- Angina pectoris.
- Cardiac arrest
- Myocardial infarction.
- Congestive cardiac failure.
- Obstructive cardiomyopathy.
- Pheochromocytoma.
- Thyrotoxicosis.
- Glaucoma.
- Prophylaxis of migraine.
- Anxiety.
Question 28. Nitrates.
Answer:
Nitrates.
Nitrates are vasodilators. They are
- Nitroglycerin
- Isosorbide dinitrate
- Isosorbide mononitrate
- Pentaerythritol tetranitrate.
Nitrates Uses:
- External angina
- Vasospastic angina
- Unstable angina
- Cardiac failure.
- Myocardial infarction.
- Cyanide poisoning.
- Relieves oesophageal spasm.
- Spasmolytic.
Question 29. Anti-anginal drugs.
Answer:
Anti-Anginal drugs
Anti-anginal drugs are used to improve the balance between oxygen supply and demand.
- Drugs used in the treatment of angina are as follows.
- Nitrates
- Nitroglycerin, isosorbide dinitrate, isosorbide mononitrate.
- Calcium channel blockers.
- Verapamil, diltiazem, amlodipine, nifedipine.
- Beta-blockers
- Potassium channel openers.
- Miscellaneous.
- Dipyridamole, aspirin, ivabradine.
Question 30. Calcium channel blockers (CCB).
Answer:
Calcium Channel Blockers (CCB) are.
- Dihydropyridines.
- Nifedipine.
- Nimodipine.
- Amlodipine.
- Nicardipine.
- Felodipine.
- Others.
Calcium Channel Blockers Use
- Angina pectoris
- Hypertension.
- Arrhythmia.
- Peripheral vascular disease.
- Hypertrophic cardiomyopathy.
- Migraine.
- Subarachnoid hemorrhage.
- Preterm labor.
Question 31. ESR, erythrocyte sedimentation rate.
Answer:
ESR, Erythrocyte Sedimentation Rate
It was first demonstrated by Edmund Beirnacki in 1897.
Erythrocyte Sedimentation Rate Definition:
The rate at which the erythrocytes settle down in a vertical tube is called ESR.
Erythrocyte Sedimentation Rate Normal values:
- According to Westergren’s method.
- Males -3-7 mm in 1 hour.
- Females – 5 – 9 mm in 1 hour.
- Infants – 0 – 2 mm in 1 hour.
Erythrocyte Sedimentation Rate Significance:
- Confirms diagnosis.
- Helps to assess the patient’s response to treatment for certain chronic inflammatory diseases.
Factors Affecting ESR:
- The specific gravity of RBC ais Rouleaux formation.
- Size of RBC
- Viscosity of blood.
- RBC count.
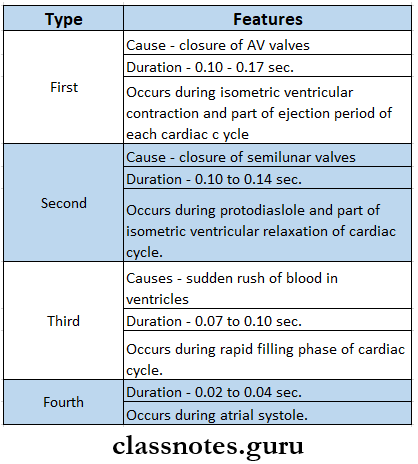
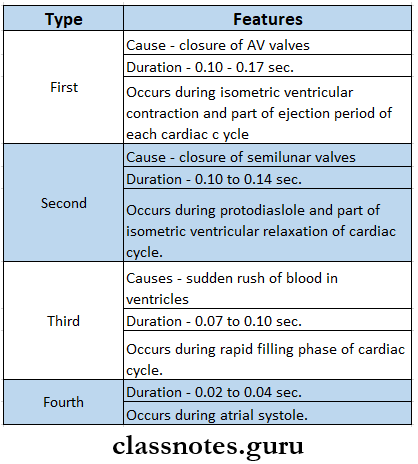
Question 32. Heart sounds.
Answer:
Heart Sounds
Mechanical activities of the heart during each cardiac cycle produce some sounds called heart sounds.
Heart sounds Types
Question 33. Pericarditis.
Answer:
Etiology:
- Infection.
- Immunological reaction.
- Trauma
- Neoplasm.
- Idiopathic.
Pericarditis Clinical Features:
- Retrosternal pain.
- Pain radiates to the shoulder and neck.
- Aggravated by deep breathing, movement, changes of position, exercise, and swallowing.
Pericarditis Management:
- Aspirin – 600 mg 4 hourly.
- Indomethacin – 25 mg 8 hourly.
- Paracentesis.
- Surgical drainage.
Cardiac diseases short question bank
Question 34. Collapsing pulse.
Answer:
Collapsing Pulse
It is a pulse characterized by a rapid upstroke, rapid downstroke, and a high volume.
Factors Effecting it:
- Increased stroke volume.
- Diastolic leak back into left ventricle
- Low systemic vascular resistance
Collapsing Pulse Significance:
- It occurs in.
- Aortic regurgitation
- Patent ductusarteriosus
- Ruptured sinus of Valsalva
- Large arteriovenous fistula
- Hyperkinetic circulatory states,
Question 35. Treatment of deep vein thrombosis.
Answer: ‘
Bed rest with legs elevated to 15 degrees
- Physiotherapy
- Graduated elastic stockings.
- Use of heparin.
- Thrombolysis with streptokinase.
- Thrombectomy.
Question 36. Corrigan’s sign.
Answer:
Corrigan’s Sign
Described by Sir Dominic John Corrigan.
- It is a sign of severe aortic valve regurgitation.
- It is a jerky carotid pulse characterized by full expansion followed by quick collapse.
- It appears in the advanced form of the disease.
- By this time, the patient is usually symptomatic.
Corrigan’s Sign Causes:
- Rheumatic fever.
- Infective endocarditis,
- Marfan’s syndrome.
- Ehlers – Danlos syndrome.
- Collagen vascular disease.
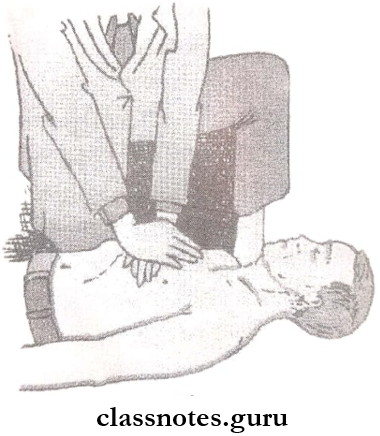
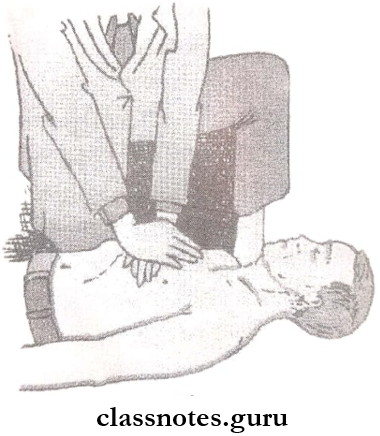
Question 37. Cardiopulmonary resuscitation.
Answer:
Cardiopulmonary Resuscitation
Position the patient on a firm surface such as the floor.
- The heel of the hand should be placed over the lower end of the sternum and with the other hand above it depress the sternum for 3-4 cm,
- It should be maintained at the rate of 60 per minute.
- It should be continued as long as cardiac resuscitation remains feasible and cerebral function is intact.
- It may take a few minutes or even a few hours.
Question 38. Intermittent claudication.
Answer:
Intermittent Claudication
It is a symptom occurring due to chronic arterial occlusion.
Intermittent Claudication Features:
- Pain occurs during exertion and gradually disappears within minutes upon cessation of activity.
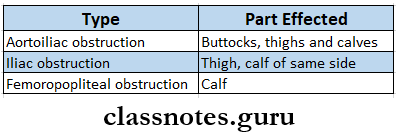
- The group of muscles which will be affected depends on the site of arterial occlusion.
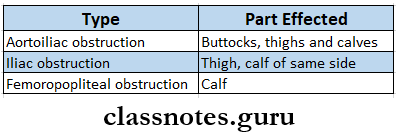
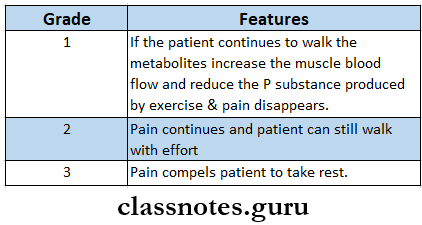
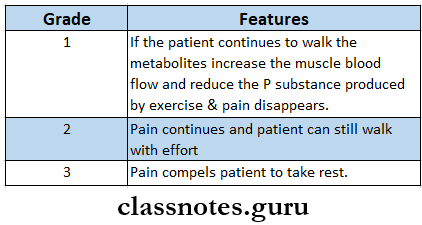
Boyd’s Classification:
VIVA VOCE
- The most common congenital heart disease is a ventricular septal defect
- The commonest cause of ventricular tachycardia is acute myocardial infarction
- The commonest cyanotic heart disease is tetralogy The commonestRheumatic fever mostly results in mitral regurgitation
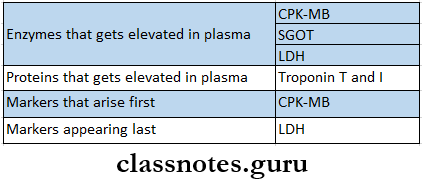
- Markers the commonesfirstst in myocardial infarction is CPK-MB
- The pacemaker of the heart is the SA node
- The first symptom of heart failure is dyspnoea
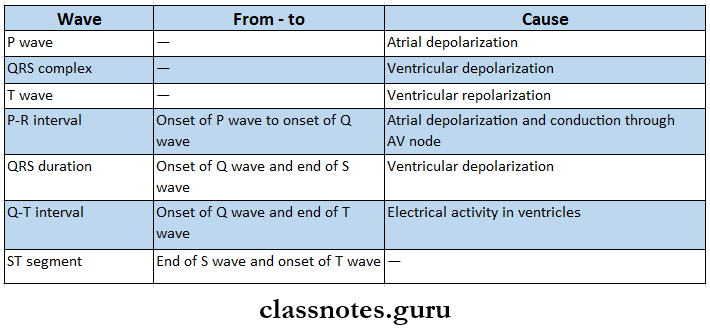
- In atrial flutter P wave of ECG sarees a saThe pacemaker appearance
- Preload is the first diastolic filling pressure of the ventricle just before,e contraction
- The force against which the ventricular contracts is termed as afterload
- Kussumaul’s sign is an increase of jugular venous pressure during inspiration.