Spleen Pancreas And Liver Question And Answers
Question 1. Describe about the functions, external features, and relations of spleen.
Answer:
Spleen:
- The largest lymphatic organ in the body
- It filters the blood, helps to provide immunity, and also synthesis RBC in fetal life
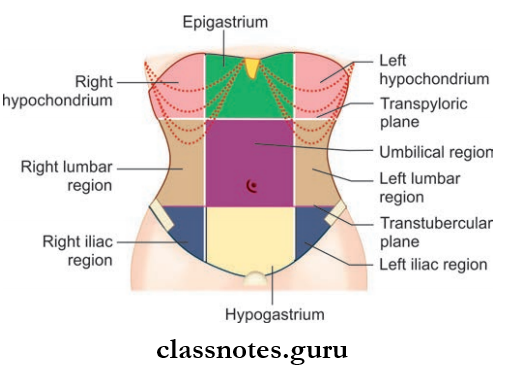
- Location: (Mainly) Left hypochondrium between the fundus of stomach and diaphragm, (partly) epigastrium, and behind 9th–11th ribs in the midaxillary line
Read And Learn More: Abdomen And Pelvis
Spleen Shape
- Wedge-shaped (44%)
- Tetrahedral (42%)
- Triangular (14%)
- Harris dictum – 1 3 5 7 9 11
- 1-inch thickness
- 3-inch breadth
- 5-inch length
- 7-ounce weight
- Lies behind 9th–11th ribs
Spleen Color: Purple color
Spleen Consistency: Soft
Spleen Size:
- Thickness: 2.5 cm (1 inches)
- Breadth: 7.5 cm (3 inches)
- Length: 12.5 cm (5 inches)
- Weight: 7 ounce
Spleen Pancreas And Liver Questions And Answers
Spleen Position
- The long axis of the spleen lies parallel to the long axis of the 10th rib
- Spleen is directed forwards, downwards, and laterally.
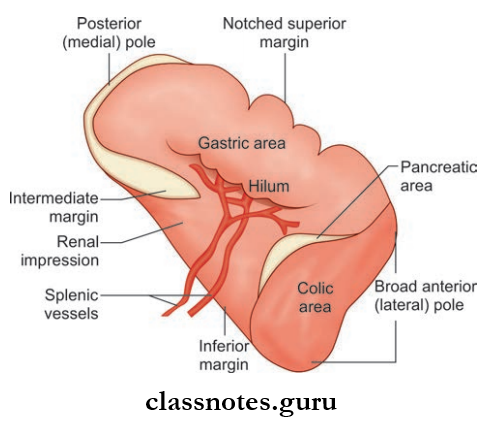
Spleen External Features Spleen has
- Two ends (anterior and posterior)
- Three borders (superior, inferior, and intermediate)
- Two surfaces (diaphragmatic and visceral).
Spleen Two Ends
- Anterior end
- It is the lateral end of the spleen
- This end is broad and is very much like a border
- Directed downwards, forwards, and to the left and reaches the midaxillary line.
- Posterior end
- It is the medial end of the spleen
- The blunt and rounded end
- This end rests on the upper pole of the kidney
- Directed upwards, backward, and medially.
Spleen Three Borders
- Superior Border
- Thin and convex
- It is characteristically notched near the anterior end
- This border separates the visceral surface from the diaphragmatic surface.
- Inferior Border
- Rounded border
- It also separates the visceral surface from the diaphragmatic surface.
- Intermediate Border
- Rounded border
- It is directed toward the right
- The hilum of the spleen lies in the intermediate border.
Liver Pancreas Spleen Anatomy MCQs
Spleen Two Surfaces
- Diaphragmatic Surface
- Convex and smooth
- Directed upwards backward and to the left
- Visceral Surface
- Concave and irregular
It Bears 4 Impressions Of The Viscera, They Are:
- Gastric Impression
- Largest impression on spleen
- Impression for the fundus of stomach
- Lies between the superior border and intermediate border
- Renal Impression
- Impression for left kidney
- Lies between the inferior border and intermediate border
- Colic Impression
- Impression for splenic flexure of colon
- Consists of a triangular area adjoining the lateral (anterior) end of the spleen
- Pancreatic Impression
- Impression for tail of pancreas
- Lies between the hilum of the spleen and the colic impression.
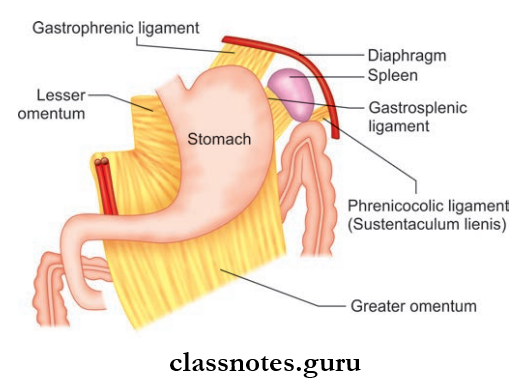
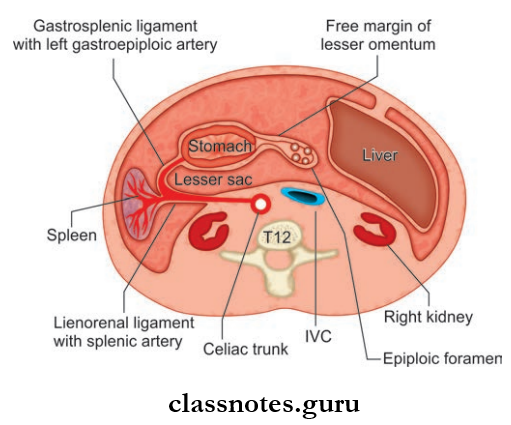
Spleen Relations
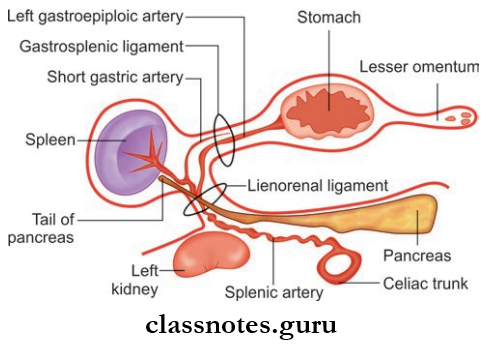
- Peritoneal Relations
- Spleen is surrounded by the peritoneum, except at its hilum
- From the hilum, two peritoneal folds/ligaments extend into the stomach and left kidney respectively and they are:
- Gastrosplenic Ligament:
- Extent: From the hilum of the spleen to greater curvature of the stomach
- Contents: Short gastric nerves, vessels, and lymphatics
- Lienorenal Ligament:
- Extent: From hilum of the spleen to anterior surface of left kidney
- Contents:
- Tail of pancreas
- Splenic vessels
- Pancreaticosplenic lymph nodes
- Visceral Relations
- Visceral Surface
- Fundus of stomach
- Anterior surface of left kidney
- Splenic flexure of the colon
- Tail of pancreas
- Diaphragmatic Surface
- Diaphragm
- Visceral Surface
Liver Pancreas And Spleen Function Questions
Question 2. Write a note on the blood supply, lymphatic drainage, and nerve supply of the spleen. Mention the vascular segments of the spleen.
Answer:
Spleen Arterial Supply: Supplied by splenic artery (the largest branch of the celiac trunk)
Spleen Course:
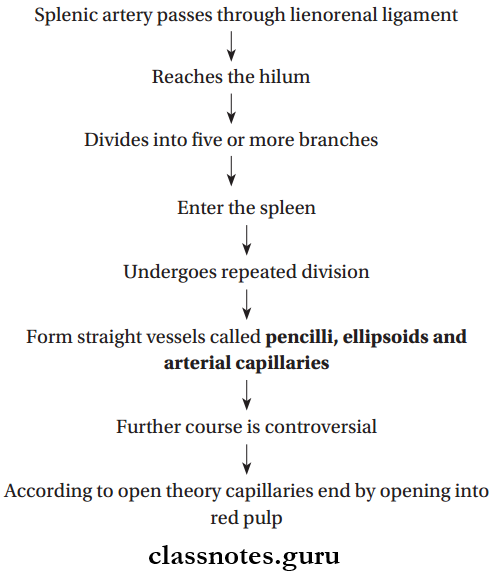
Vascular Segments of Spleen
- Splenic Srtery Gives Of Two Branches: Superior and inferior
- Superior and inferior branches supply superior and inferior parts of the spleen respectively
- Since there is no anastomoses with these branches, there exists an avascular plane between the superior and inferior portions
- This avascular plane passes perpendicular to the long axis of the spleen
- Thus spleen is said to have two vascular segments: Superior and inferior
- Knowledge about vascular segments are important for surgical practices.
Spleen Venous Drainage
- By splenic vein formed at the hilum by union of 5 or more tributaries arising from the splenic substance
- The splenic vein joins with the superior mesenteric vein and forms the portal vein.
Spleen Lymphatic Drainage
- It has no proper lymphatics
- Few lymphatics are seen in the connective tissue of capsule and trabecula
- Drain into pancreaticosplenic lymph nodes.
Spleen Nerve Supply
- Only sympathetic supply
- Derived from celiac plexus.
Human Digestive System – Liver Pancreas Spleen
Question 3. Describe about the external features of the pancreas and its relations.
Answer:
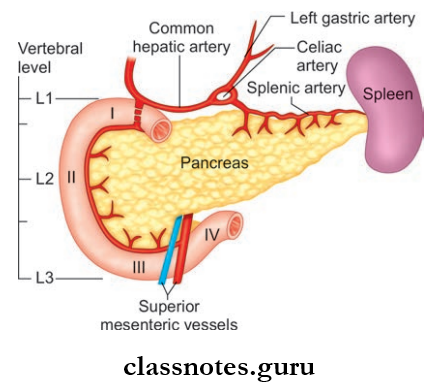
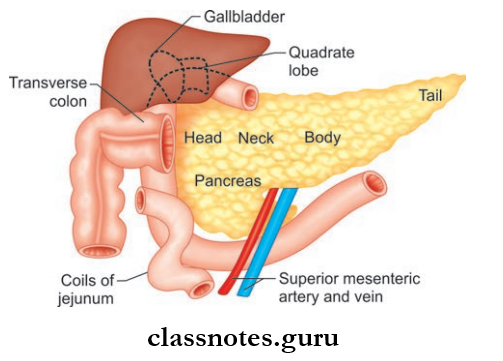
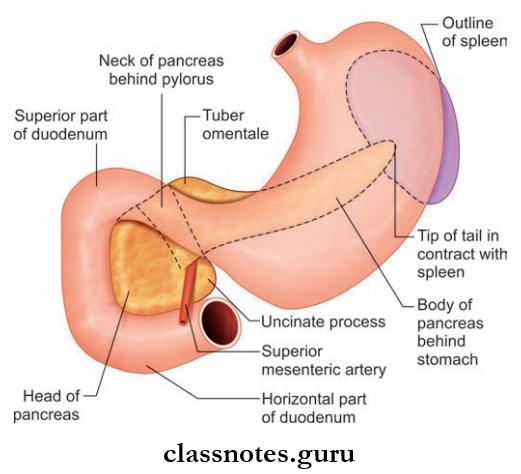
Pancreas
- Fleshy in appearance
- Soft and fully lobulated
- Pancreas Location:
- Vertebral Level: L1 and L2
- Region: Epigastrium and left hypochondrium
- Position: Lies more or less horizontally on the posterior abdominal wall
Pancreas Shape: Jshaped
Pancreas Size:
- Length: 15–20 cm
- Breadth: 2.5–4 cm
- Thickness: 1.2–1.8 cm
- Weight: 90 g
- Subdivisions of pancreas
Pancreas Can Be Divided Into 4 Parts, Namely:
- Head with uncinate process
- Neck
- Body
- Tail
1. Hand Of Pancreas:
- Enlarged and flattened right end of the pancreas
- Lies within the Cshaped concavity of duodenum in front of L2 vertebrae
- There is a projection from the lower part of head of the pancreas called the uncinate process
- Head Of The Pancreas Has:
- Three borders (superior, inferior, and right lateral border)
- Two surfaces (anterior and posterior)
Hand Of Pancreas Relations of:
- Superior Border
- The first part of the duodenum
- Superior pancreaticoduodenal artery
- Inferior Border
- The third part of the duodenum
- Inferior pancreaticoduodenal artery
- Right Lateral Border
- The second part of the duodenum
- Terminal part of the bile duct
- Anterior and posterior
- pancreaticoduodenal
- arterial anastomoses
- Anterior Surface
- The first part of the duodenum
- Transverse colon
- Root of transverse mesocolon
- Jejunum
- Posterior Surface
- Inferior vena cava
- Left renal vein
- Bile duct (sometimes gets embedded in pancreatic tissue)
- Uncinate Process
- Anteriorly: Superior mesenteric vessels
- Posteriorly: Aorta
Hand Of Pancreas Applied Anatomy
Since the bile duct and head of the pancreas have a close relationship, pancreatitis or carcinoma head of the pancreas can obstruct the bile duct leading to biliary retention resulting in jaundice.
Liver, Pancreas, Spleen Anatomy And Physiology
2. Neck Of Pancreas:
- Slightly constricted part between head and body of pancreas
- Length: 2.5 cm
- Directed forwards upwards and to the left
- Neck Of Pancreas Has:
- Two surfaces (anterior and posterior)
- Two borders (upper and lower)
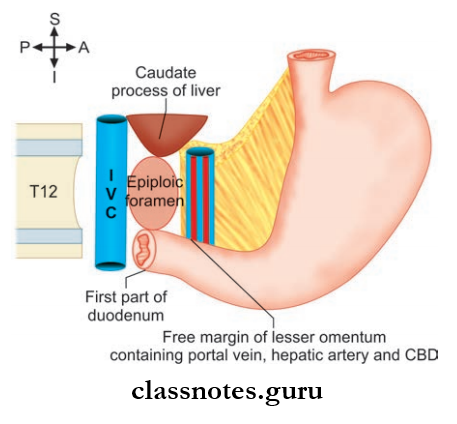
Neck Of Pancreas Relations:
- Anterior Surface
- Pylorus
- The peritoneum covering the posterior wall of the lesser sac
- Posterior Surface
- Commencement of portal vein
- Termination of superior mesenteric vein
- Upper Border
- First part of duodenum
- Lower Border
- Root of the transverse mesocolon
3. Body Of Pancreas:
- Elongated part present between neck and tail
- Directed towards the left side with a slight upward and backward inclination
- Lies just below the transpyloric plane
- Body Of Pancreas Has:
- Three borders (anterior, superior, and inferior)
- Three surfaces (anterior, posterior, and inferior)
- One process: Tuber omental (it is the part of the body of pancreas projecting upwards beyond the lesser curvature of the stomach and comes in contact with lesser omentum).
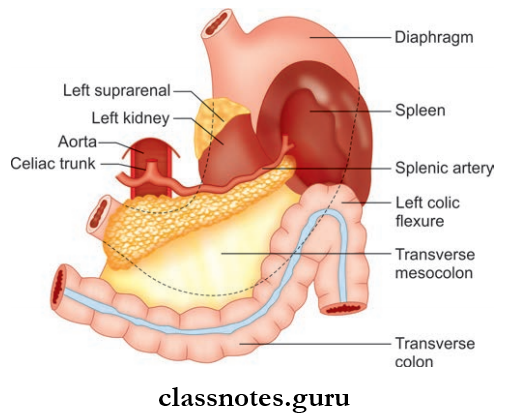
Body Of Pancreas Relations:
- Anterior Border: Provides attachment for the root of the transverse mesocolon
- Superior Border
- Celiac artery
- Hepatic artery
- Splenic artery
- Inferior Border: Superior mesenteric vessels
- Anterior Surface
- Lesser sac
- Stomach
- Posterior Surface
- Left crus of the diaphragm
- Left kidney and suprarenal gland
- Aorta and origin of superior mesenteric artery
- Left renal vessels
- Splenic vein
- Inferior Surface
- Duodenojejunal flxure
- Coils of jejunum
- Left colic flexure
4. Tail Of Pancreas (Mobile Part)
- Narrow left end of the pancreas
- Tail Of Pancreas passes between the layers of lienorenal ligament
- Tail Of Pancreas is related to visceral surface of spleen.
Important Questions On Spleen Pancreas And Liver
Question 4. Classify ducts of the pancreas and give a brief description about their course.
Answer:
Ducts Of The Pancreas
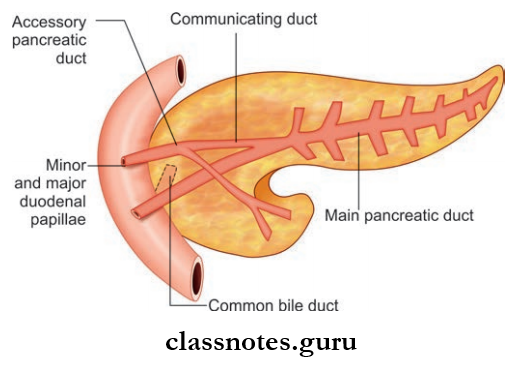
Pancreas Has Two Ducts:
- Main pancreatic duct
- Accessory pancreatic duct.
1. Main Pancreatic Duct (Duct of Wirsung)
- White in color
- Lies near to the posterior surface of the pancreas
Main Pancreatic Duct (Duct of Wirsung) Course:
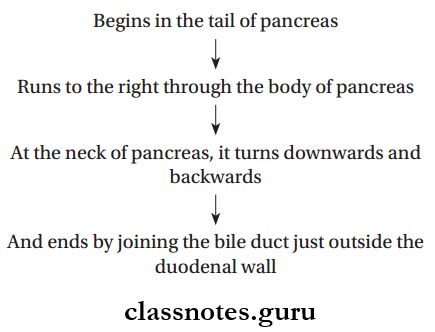
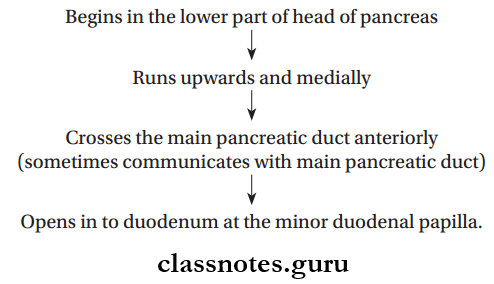
Accessory Pancreatic Duct (Pancreatic Duct of Santorini) Course:
Question 5. Write a note blood supply, lymphatic drainage, and nerve supply of the pancreas.
Answer:
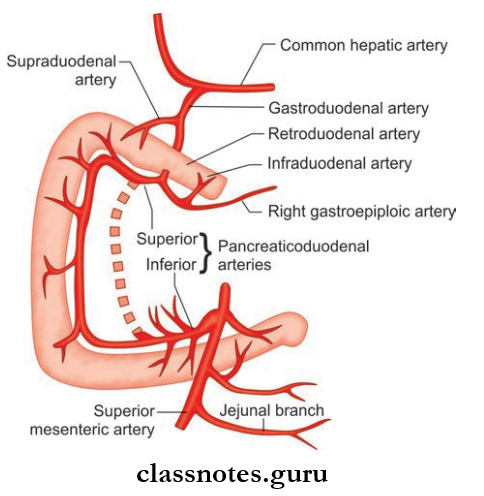
Pancreas Arterial Supply
- Gastroduodenal artery—branch of common hepatic artery
- Anterior superior pancreaticoduodenal artery
- Posterior superior pancreaticoduodenal artery
- Branches Of Splenic Artery:
- Dorsal pancreatic artery
- Greater pancreatic artery
- Great pancreatic artery.
Pancreas Venous Drainage
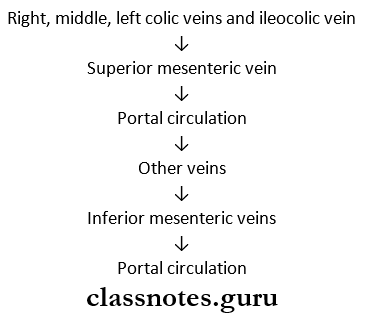
- Veins Drain Into:
- Portal vein
- Superior mesenteric vein
- Splenic vein.
Pancreas Nerve Supply
- Sympathetic and parasympathetic fiers are derived from celiac and superior mesenteric plexus
- Sympathetic Supply: Vasomotor in function
- Parasympathetic Supply: Controls pancreatic secretion.
Liver Pancreas Spleen Viva Questions
Question 6. Write a note on development of pancreas.
Answer:
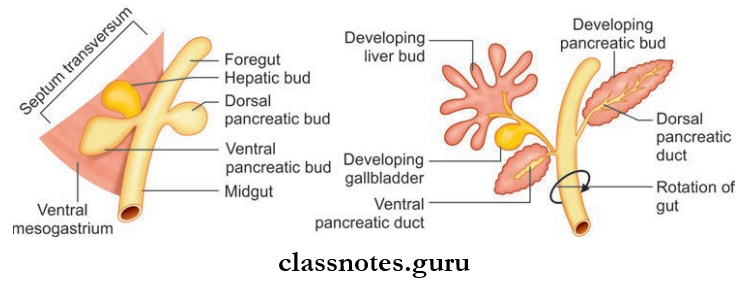
Development Of Pancreas
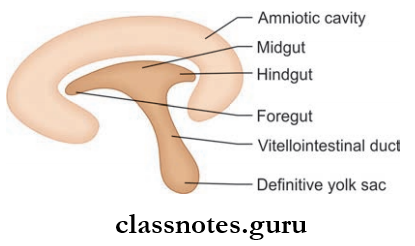
- Pancreas is developed from two endodermal buds (ventral and dorsal buds), formed at the junction of foregut and midgut
- Dorsal bud lies at dorsal aspect of gut
- Ventral bud lies below hepatic bud
- Large part of the pancreas develops from the dorsal bud Ventral bud gives rise to inferior part of head of the pancreas and the uncinate process
- The dorsal bud gives rise to upper part of head of the pancreas, body, and tail of pancreas
- Dorsal and ventral buds give rise to primitive ducts Proximal part of the duct of dorsal bud form the accessory pancreatic duct
- The distal part of the duct of dorsal bud and duct of ventral bud together forms main pancreatic duct
- Anomalies: Annular pancreas—pancreatic tissue surrounds the duodenum and obstructs it.
Question 7. Describe in detail about the external features, and anatomical and physiological division of the liver. What is Riedel’s lobe?
Answer:
Liver
- Largest visceral organ of the body
- Occupy most of the right upper part of abdomen
- Location: Right hypochondrium, upper part of epigastric region, and medial part of left hypochondrium
- Shape: Wedge-shaped
- Color: Red-brown
- Weight:
- Male: 1.6 kg
- Female: 1.3 kg
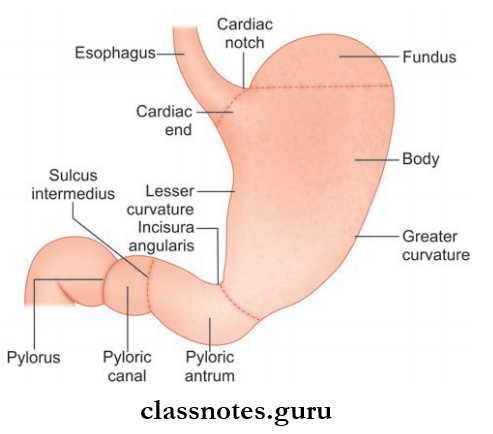
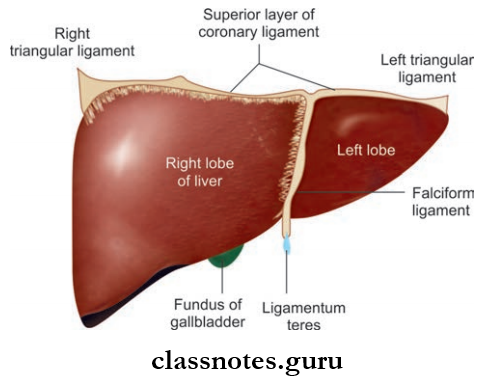
Liver External Features It has
- Five Surfaces:
- Anterior, posterior, superior, inferior, and right
- Anterior, posterior, superior, and right surfaces do not have any clear-cut border, so they are collectively called diaphragmatic surface
- The inferior surface is well-demarcated by the inferior border
- One Border: Inferior Border
- It is sharp anteriorly (marked by notch for ligamentum teres and cystic notch), but is rounded laterally
- Anteriorly it separates the anterior surface from the inferior surface
- Laterally it separates the right surface from the inferior surface.
- Two Lobes:
- Anatomically on the diaphragmatic surface, liver is divided into right and left lobes by:
- Falciform ligament—anteriorly and superiorly
- Fissure for ligamentum teres—inferiorly
- Fissure for ligamentum venosum—posteriorly
- Right lobe is about 5–6 times larger than the left
- It presents with parts of all 5 surfaces
- In addition, two more lobes (caudate and quadrate lobes) arise from the right lobe of the liver.
- Anatomically on the diaphragmatic surface, liver is divided into right and left lobes by:
Pancreas And Liver Short Questions And Answers
Riedel’s Quadrate Lobe
- Rectangular in shape
- Situated on the anterior aspect of the inferior surface of liver
Riedel’s Quadrate Lobe Boundaries:
- Right: Fossa of gallbladder
- Left: Fissure for ligamentum teres
- Anteriorly: Inferior border
- Superiorly: Porta hepatis.
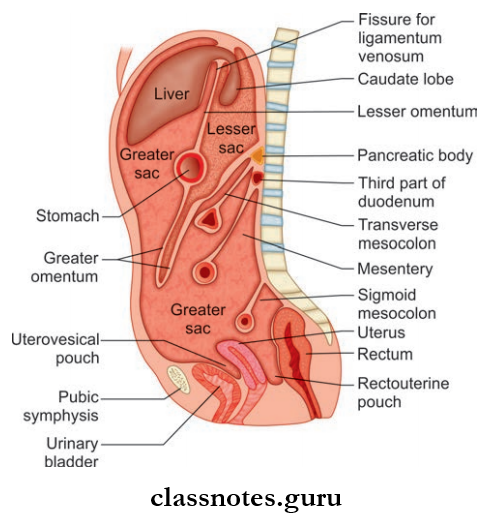
Riedel’s Quadrate Lobe Caudate Lobe: Situated on the posterior part of the inferior surface of the liver
Riedel’s Quadrate Lobe Boundaries:
- Right: Groove for inferior vena cava
- Left: Fissure for ligamentum venosum
- Superiorly: Continuous with the superior surface of the liver
- Inferiorly: Porta hepatis
- Just posterior to porta hepatis, the caudate lobe is connected to the right lobe of liver by a process known as caudate process
- Although both caudate and quadrate lobes arise from right lobe, both are functionally distinct
- But the quadrate lobe is functionally related to the left lobe.
Riedel’s Quadrate Lobe Physiological Division of Liver
- The liver is also divided into right and left physiological lobes
- It is based on the intrahepatic distribution of branches of the bile duct, hepatic artery, and portal vein
- Grossly The Division Is Done By An Imaginary Line Passing Through:
- Fossa of the gallbladder to the groove for inferior vena cava in the posteroinferior surface
- From the groove for the inferior vena cava to the cystic notch in the anterosuperior surface
- Both the physiological lobes are almost equal in size
- Each Lobe Has Its Own:
- Hepatic duct
- Portal vein
- Primary branch of the hepatic artery.
Question 8. Describe briefly about hepatic segments of Chouinard.
Answer:
Hepatic Segments Of Chouinard
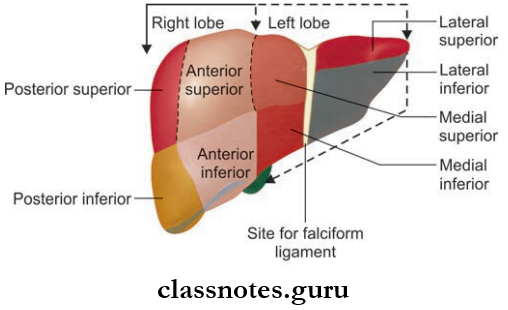
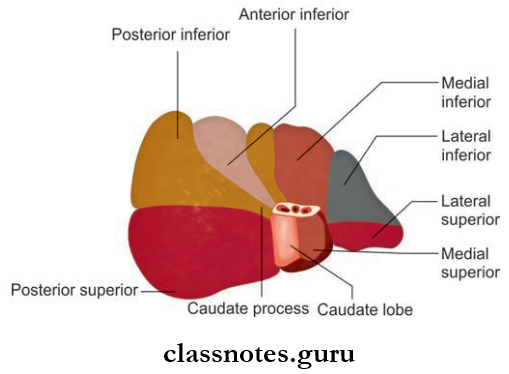
- Functional segments of liver on the anterior surface
- Visceral surface
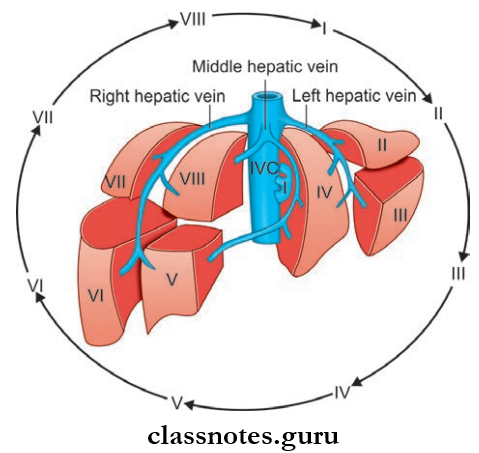
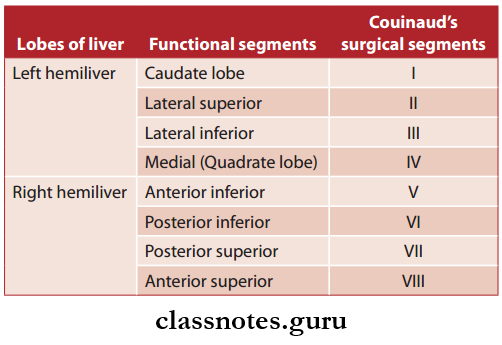
- Couinaud classification of liver anatomy divides the liver into eight functionally independent segments
- The right lobe is subdivided into anterior and posterior segments (no identifiable demarcation present)
- The left lobe is subdivided into medial and lateral segments (divided by fissure for ligamentum teres and ligamentum venosum)
- They can further be divided into superior and inferior, giving a total of 8 hepatic segments
Couinaud Lobes
- Right Lobe
- Right anterior superior
- Right anterior inferior
- Right posterior superior
- Right posterior inferior
- Left Lobe
- Left lateral superior
- Left lateral inferior
- Left medial superior
- Left medial inferior
Equivalent terms for functional and surgical hepatic segments
- Each segment has its own vascular inflow, outflow, and biliary drainage
- In the center of each segment, there is a branch of the portal vein, hepatic artery, and bile duct
- These segments have great surgical importance, each segment is surgically resectable
- Hepatic veins draining the segments are intersegmental and so drain more than one segment.
Liver And Pancreas Important Points For Exams
Question 9. Write in detail about the blood supply of the liver. Classify hepatic veins and also mention the lymphatic drainage and nerve supply of the liver.’
Answer:
Arterial Supply Of Liver
- The liver receives blood supply from:
- Hepatic Artery: 20% of blood
- Portal vein: 80% of blood
Supply Of Liver Course
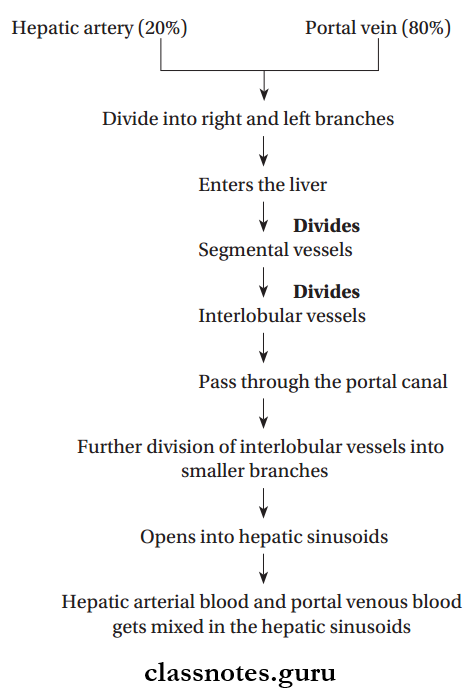
Supply Of Liver Venous Drainage
- Hepatic sinusoids Interlobular veins Sublobular veins Hepatic veins
- Hepatic veins drain into the inferior vena cava
- Hepatic Veins Are Divided Into Two Groups: Upper group and lower group
- Upper Group:
- Consists of 3 veins, namely the right hepatic vein, left hepatic vein, and middle hepatic vein
- Right and left hepatic veins drain from the right lobe only
- Middle hepatic vein drains from both right and left lobes
- Lower Group:
- Consists of numerous small veins from the right lobe and caudate lobe.
- Upper Group:
Lymphatic Drainage Of The Liver
- Superficial Lymphatics drain into hepatic nodes in the porta hepatis
- From there to retro pyloric nodes and then to celiac nodes
- Deep Lymphatics drains through two trunks:
- Ascending Trunk: Drains to lymph nodes around inferior vena cava
- Descending Trunk: Drains to hepatic lymph nodes in the porta hepatis.
Nerve Supply Of Liver
- Sympathetic Supply: Derived from celiac plexus
- Parasympathetic Supply: Derived from a hepatic branch of the anterior vagal trunk.
Question 10. Briefly mention the peritoneal and visceral relations of liver.
Answer:
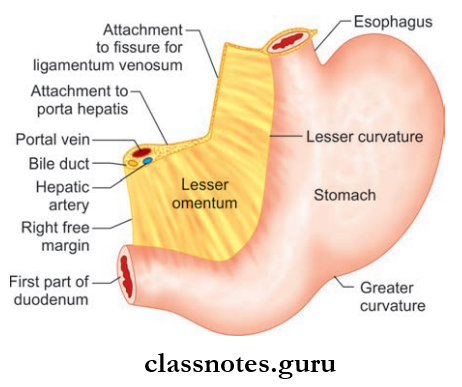
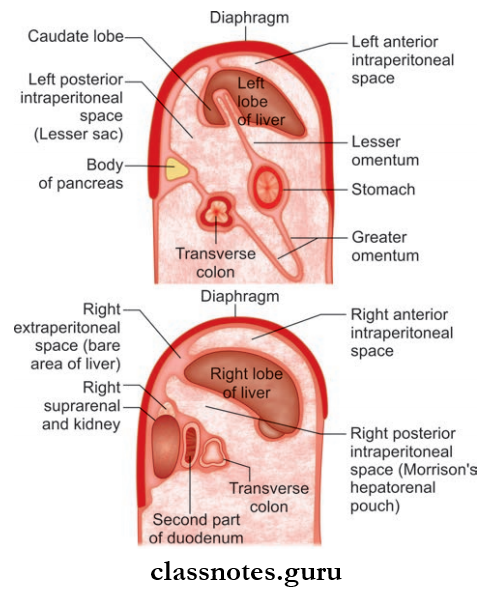
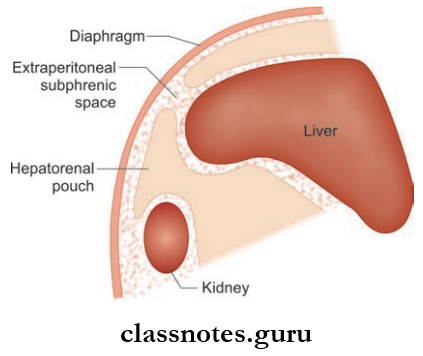
The Peritoneal And Visceral Relations Of Liver
Peritoneal Relations Of Liver
- Most areas of the liver are covered by the peritoneum, areas free from the peritoneum are:
- Bare Area Of Liver: Triangular area on the posterior aspect of the right lobe
- Fossa for gallbladder
- Groove for inferior vena cava
- Coronary ligament
- Lesser omentum.
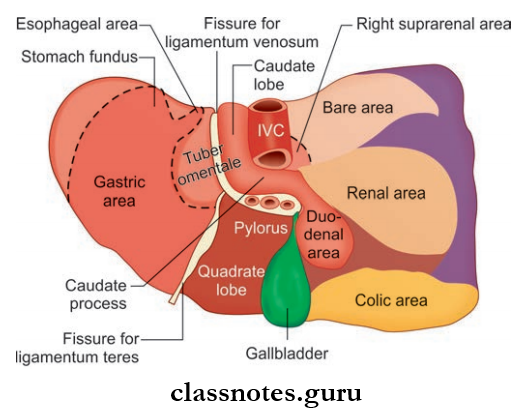
- Visceral Surface Is Related To:
- The right side of the stomach—gastric and pyloric areas
- The superior part of the duodenum—duodenal area
- Lesser omentum
- Gallbladder
- Right colic flexure
- Right kidney and suprarenal gland; renal area.
Question 11. Write a note on the development of liver and gallbladder.
Answer:
The Development Of The Liver And Gallbladder
- The liver is derived from an endodermal bud known as hepatic bud
- Hepatic bud is formed at the junction between the foregut and midgut
- It grows into the septum transversum via ventral mesogastrium
- The Bud Enlarges And Divides Into:
- The large cranial part called pars hepatica
- Small caudal part called pars cystic
- Pars hepatica divides into two parts, which later form the parenchyma of right and left lobes, Kupffr’s cells and blood cells are formed from the mesoderm of septum transversum
- Pars cystic forms the gallbladder and cystic duct.
Spleen Anatomy And Function Question Answers
Spleen Pancreas And Liver Multiple Choice Questions And Answers
Question 1. What are the structures related to the hilum of liver from before backward?
- Hepatic duct
- Hepatic artery
- Portal vein
- All of the above
Answer: 4. All of the above
Question 2. Coinaud’s hepatic segment corresponds to:
- Left lobe to the left of the falciform ligament
- Fossa for gallbladder
- Caudate lobe
- Quadrate lobe
Answer: 1. Left lobe to the left of falciform ligament
Question 3. The right lobe of liver consists of which of the following hepatic segments?
- 4, 5, 6, 7, 8
- 3, 4, 5, 6, 7
- 5, 6, 7, 8
- 3, 4, 5, 6
Answer: 3. 5, 6, 7, 8
Question 4. The blood supply of the spleen is:
- Segmental in origin
- Nonsegmental in origin
- Both
- None
Answer: 1. Segmental in origin
Question 5. The neck of pancreas on its posterior surface is related to:
- Bile duct
- Inferior vena cava
- Superior mesenteric vein
- Gastroduodenal artery
Answer: 3. Superior mesenteric vein
Question 6. Which is intraperitoneal?
- Kidney
- Abdominal aorta
- IVC
- Ureters
- Liver
Answer: 5. Liver
Question 7. During removal of the spleen, a surgeon must be careful not to cut which branch of the splenic artery.
- Superior mesenteric
- Left gastric
- Left gastroepiploic
- Superior pancreaticoduodenal
Answer: 3. Left gastroepiploic