Diseases Of Pulp Important Notes
- Diseases Of Pulp Formation Of Chloesterol Crystals
- Crystals are formed from chloesterol released by
- Disintegrating erthrocytes of stagnant blood vessels within the lesion
- Lymphocytes, plasma cells and macrophages
- The circulating plasma lipids
- Diseases Of Pulp Phoenix Abscess
- It is an acute inflammatory reaction superimposed on an existing chronic lesion such as cyst or granuloma
- The exaceberation of a chronic lesion is most commonly associated with the initiation of root canal therapy in a completely asymptomatic tooth
- Radiograph shows well-defined periradicular lesion
- Features Of Hyperalgesia
- Spontaneous pain
- Allodynia
- Increased response to painful stimuli
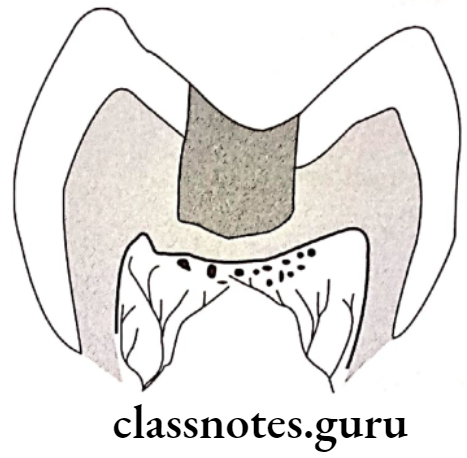
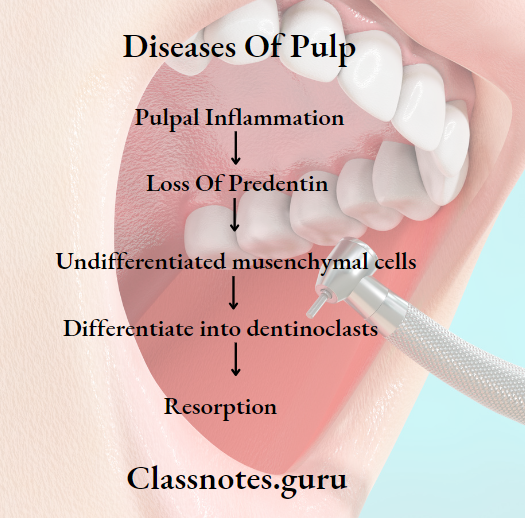
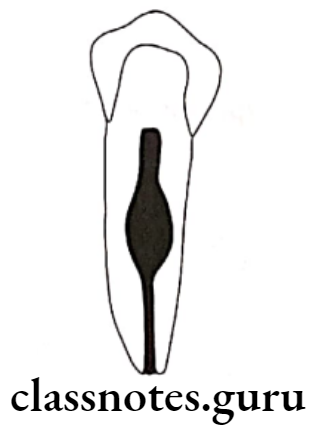
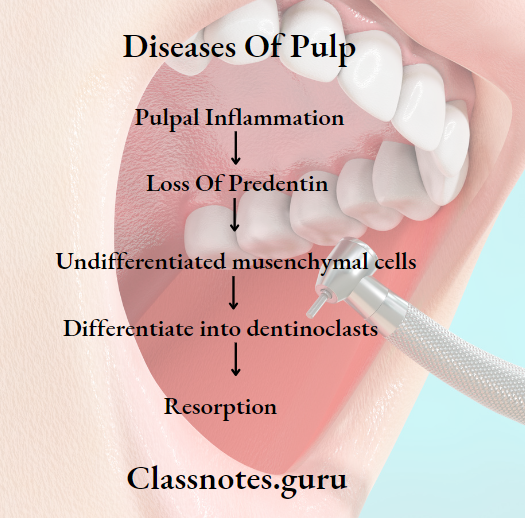
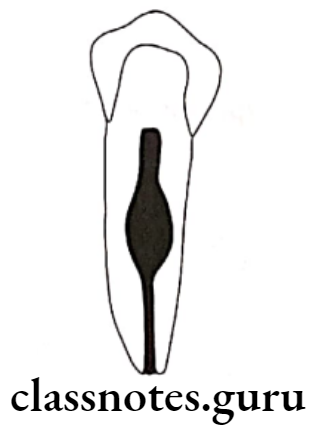
- Hyperalgesia Internal Resorption
- The cause is not known
- Clinical Features:
- Mostly asymptomatic
- Pink spot if lesion occur in crown
- Radiographically there is alteration or enlargement in the appearance of the pulp chamber or the wall of the root canal due to clastic activity
- Hyperalgesia Treatment:
- Extirpation by pulp stops resorption
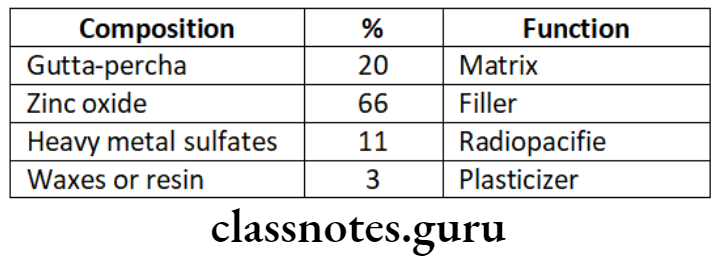
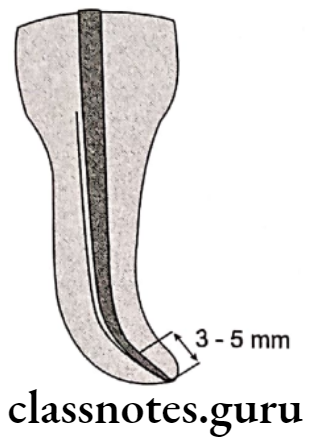
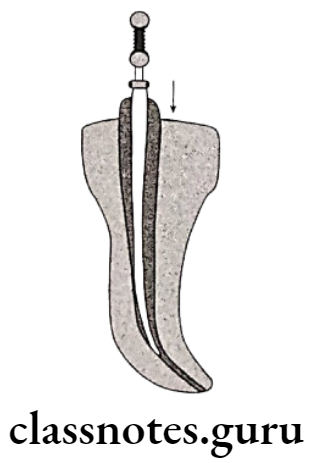
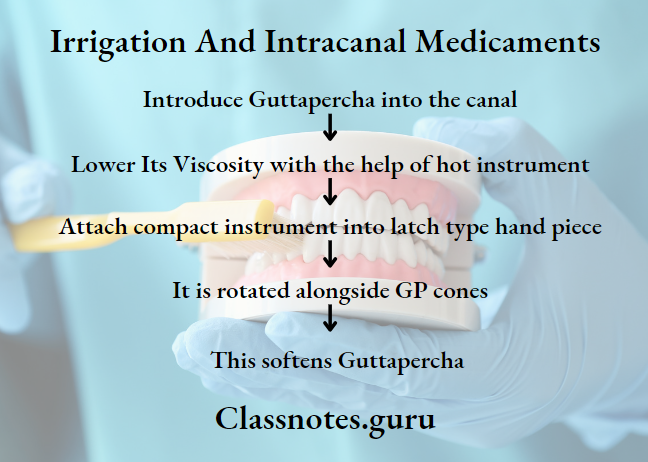
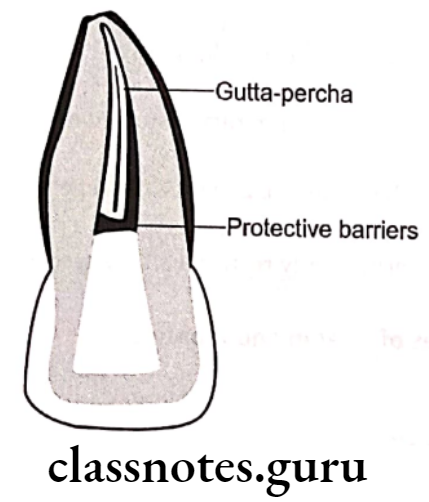
- Obturation of the defect requires effort and plasticized gutta percha
- It root is perforated, the MTA should be used to repait the defect surgically
- When repair has been completed the canal with its defect is obturated with plasticized gutta percha
- Inflammation induces
- Vasodilation
- Increased capillary pressure
- Increased vascular permeability
- Chronic apical abscess
- Asymptomatic or only slightly symptomatic if the sinus tract is obstructed
- Sinus tract allows continuous drainage of pus forming in the periapical lesion through the oral mucosa
- Most commonly associated with apical radiolucency
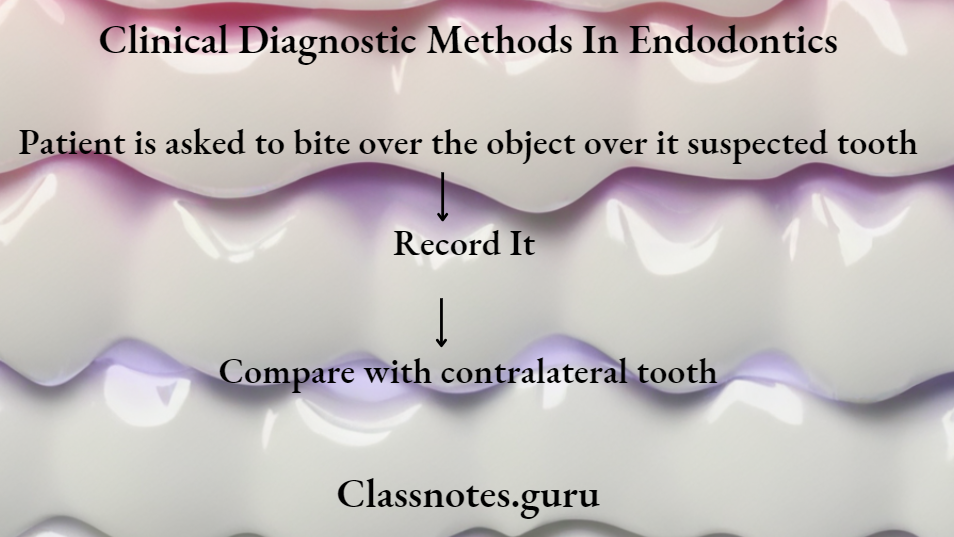
- Cracked Tooth Syndrome
- Diagnostic tests for cracked tooth syndrome:
- Visual examination aide by use of transillumination
- Use of methylene blue dye
- Biting test with the use of rubber wheels, cotton tip applicator, moist cotton rolls and tooth sloth
- Cold test and EPT
- Radiographs
- Ultrasound
- Cracked Tooth Syndrome Treatment:
- Stabilize the tooth with orthodontic band and wait for 2 weeks
- If symptoms subsides, proceed for full coverage crown
- If symptoms persiste, procedd for RCT and then crown
- Extraction if tooth has poor prognosis
- Limitations of direct pulp capping in primary teeth
- Internal resorption
- Calcification
- Chronic pulp infection
- Necrosis
- Interradicular involvement
Diseases Of Dental Pulp
Diseases Of Pulp Long Essays
Question 1. Describe about etiology, clinical features and treatment of acute apical abscess.
Answer.
Acute Apical Abscess:
Acute Apical Abscess can be defined as a localized acute or chronic suppurative infection in the periapical region of a tooth
Read And Learn More: Endodontics Question and Answers
Acute Apical Abscess Etiology:
- Extension of pulpal infection into periapical tissue
- Fracture of tooth with pulp exposure
- Accidental perforation of the apical foramen during root canal treatment
- Extension of periodontal infection into the periapical tissues
- Anachoretic infection of the periapical tissues
Acute Apical Abscess Clinical Features:
- Acute abscess produces severe pain in the affected tooth
- There will be localized swelling and an erythematous change in the overlying mucosa
- The pain aggrevates during percussion and when pressure is applied
- Acute Apical Abscess causes extrusion of the tooth from its socket
- The associated tooth in non-vital and sometimes it can be mobile also
- The affected area of the jaw may be tendered on palpation
- Application of heat intensifies pain
- Pus discharging sinus often develops
- Chronic periapical abscess often produces dull pain
Acute Apical Abscess Complications:
- Space infections
- Septicaemia
- Ludwig’s angina
- Cavernous sinus thrombosis
- Osteomyelitis
Acute Apical Abscess Radiographic Features:
- Widening of periodontal ligament space
- There is loss of lamina dura
- Area of diffuse periapical rarefaction is seen
- Margins vary from well defined to poor defined
- In advanced cases, the trabeculae are destroyed
- Radiolucency may involve adjacent tooth
- Osteitis can occur at the side of root
- Maxillary posterior teeth may lead to destruction of a portion of the antral floor
- Roots of the affected teeth may show resorption
Diseases Of Pulp And Periapical Tissues
Acute Apical Abscess Management:
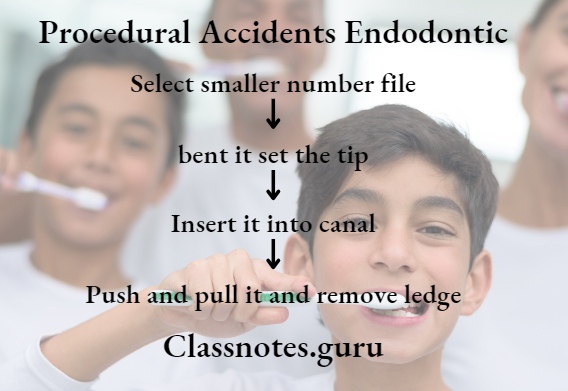
- Emergency opening of the pulp chamber through passing file into the preiapical region
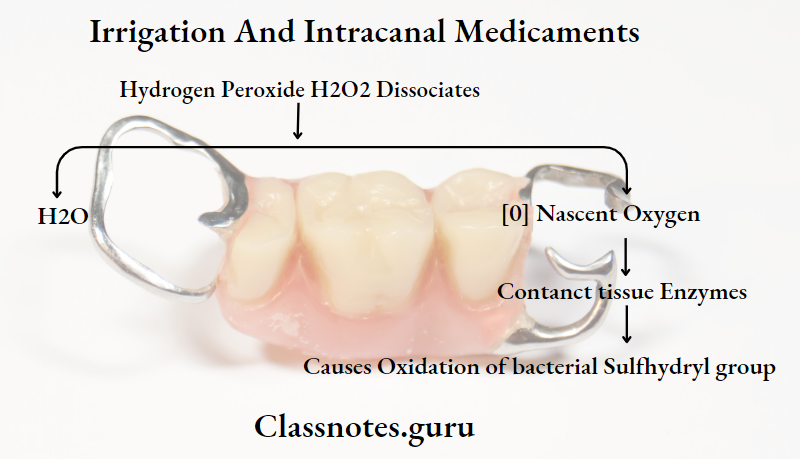
- Through and through drain is placed in the abscess and irrigated with 1:1 mix of 3% H2O2 and normal saline solution
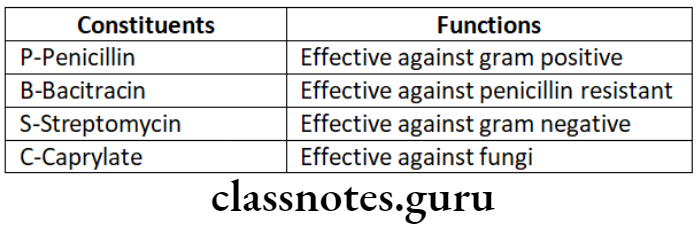
- Antibiotics
- Pencillin 500mg QID for 5 days
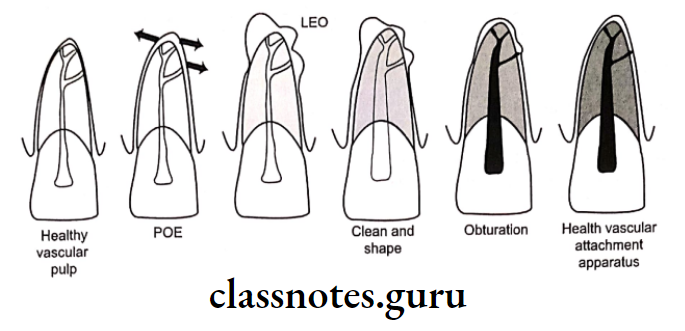
- Endodontic treatment
- Root canal treatment or extraction of offending tooth as required, is carried out in 24-48 hours.
- Warm saline mouth rinse
Pulp Diseases In Endodontics
Diseases Of Pulp Short Essays
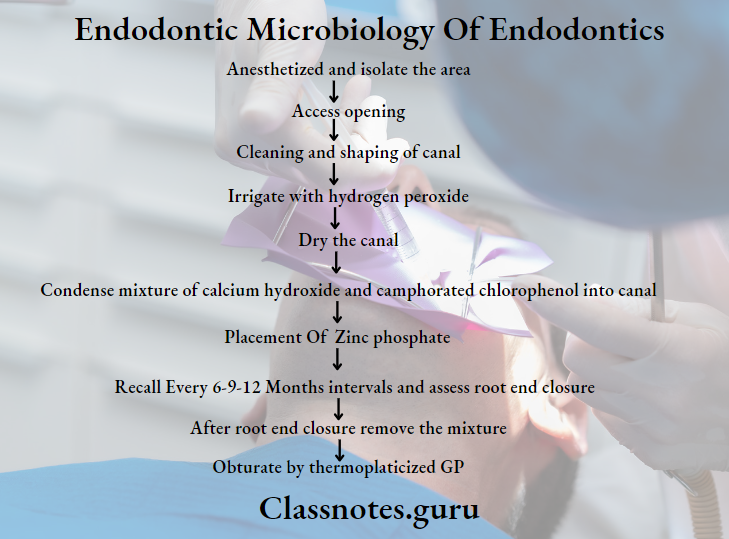
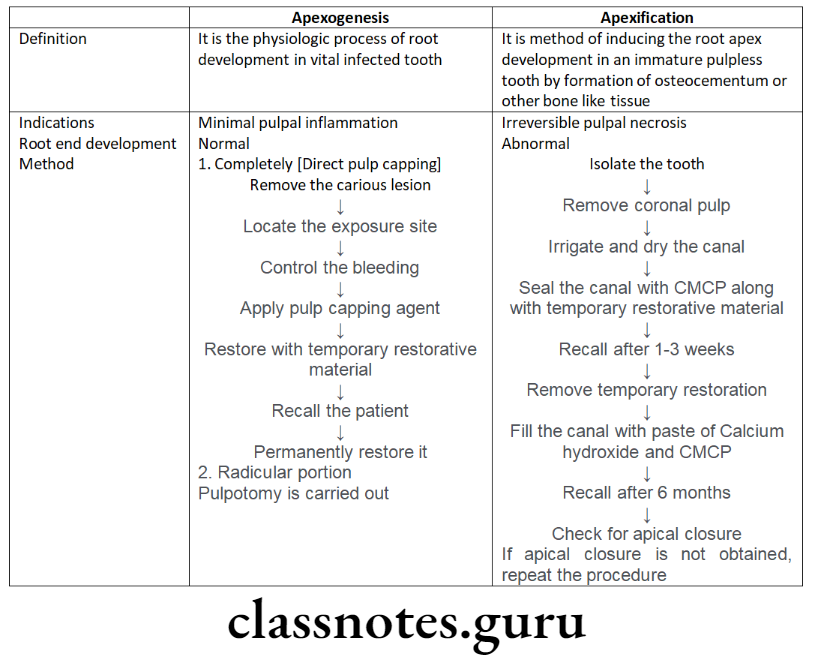
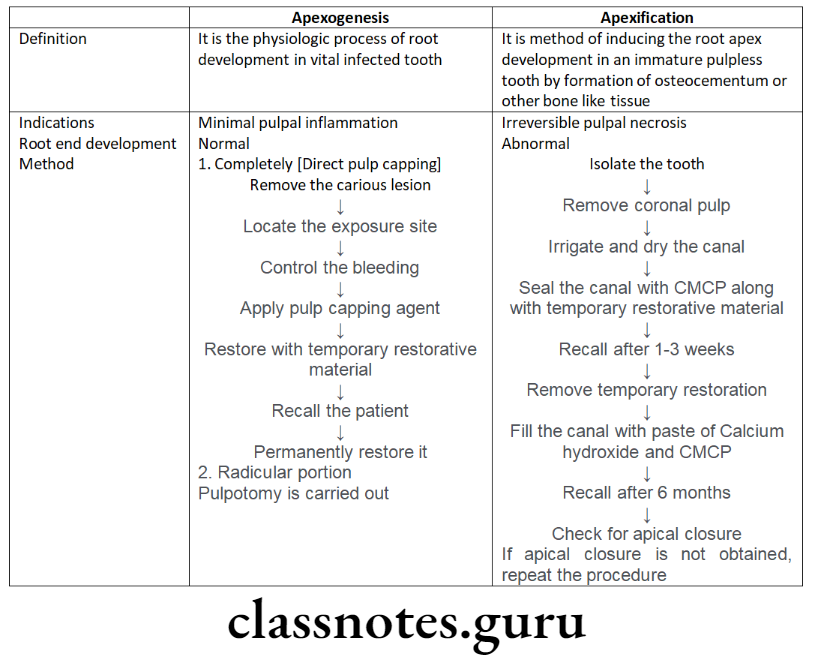
Question 1. Apexogenesis and apexification.
Answer.
Apexogenesis and apexification
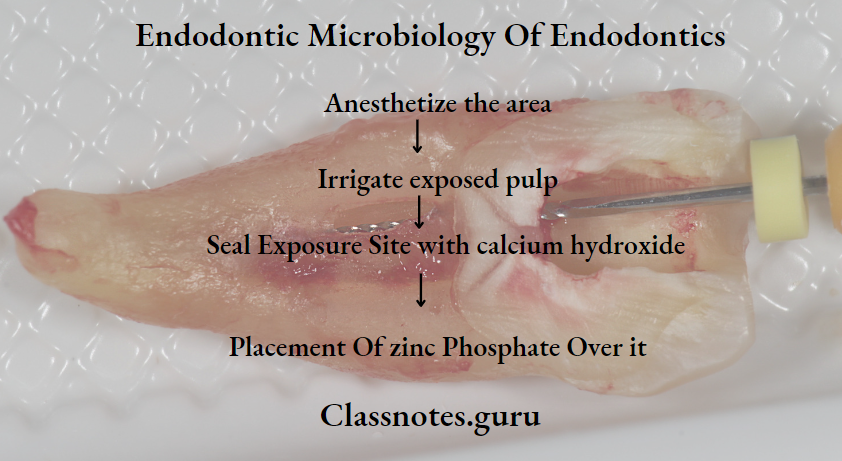
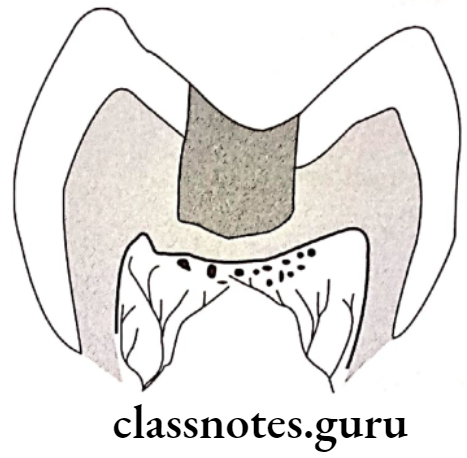
Question 2. Pulpotomy.
Answer.
Pulpotomy Definition
Pulpotomy is complete removal of coronal part of dental pulp followed by placement of suitable dressing or medicament which promotes healing and preserves tooth vitality
Pulpotomy Technique
Anaesthesize and isolate the tooth
- Remove the carious lesion
- Entire roof of coronal pulp is removed
- With the help of spoon excavator cut out the coronal pulp
- Irrigate the pulp chamber
- Control the bleeding with the help of moist cotton pellet
- Dry the pulp chamber
- Now place a cotton moistened with 1.5 concentration of Buckley’s formocreson solution into the canal
- Keep it for 5 minutes
- Now remove it and dry the canal
- Restore the tooth with thick paste of zinc oxide eugenol
- Place base of zinc polycarboxylate cement over it
- Finally, permanently restored with stainless steel crown
Pulpitis Symptoms And Treatment
Question 3. Acute Reversible Pulpitis.
Answer.
Acute Reversible Pulpitis
Acute Reversible Pulpitis is an acute inflammatory response to noxious stimuli
Diseases Of Pulp And Periapical Tissues
Acute Reversible Pulpitis Etiology:
- Trauma
- Thermal injury
- Chemical stimulus
- Deep restoration
Acute Reversible Pulpitis Symptoms:
- Sharp sudden pain on stimulus
- Pain relieves on removal of stimuli
Acute Reversible Pulpitis Diagnosis:
- Clinically – caries
- Traumatic occlusion
- Percussion test – Negative
- Radiograph – Normal PDL and lamina dura
- Vitality – Early response
Acute Reversible Pulpitis Treatment:
- No endodontic treatment required
- Sedative dressing placed
- Desensitize the tooth
- Use of cavity varnish
Question 4. Phoenix Abscess.
Answer.
Phoenix Abscess
Phoenix Abscess is an acute inflammatory reaction superimposed on existing chronic lesions
Phoenix Abscess Etiology:
- Influx of necrotic products
Phoenix Abscess Symptoms:
- Tender tooth
- Elevation of a tooth from socket
- Tender soft tissue
Phoenix Abscess Diagnosis:
- Pulp test – Negative
- Radiograph – radiolucency at the apex
Phoenix Abscess Treatment:
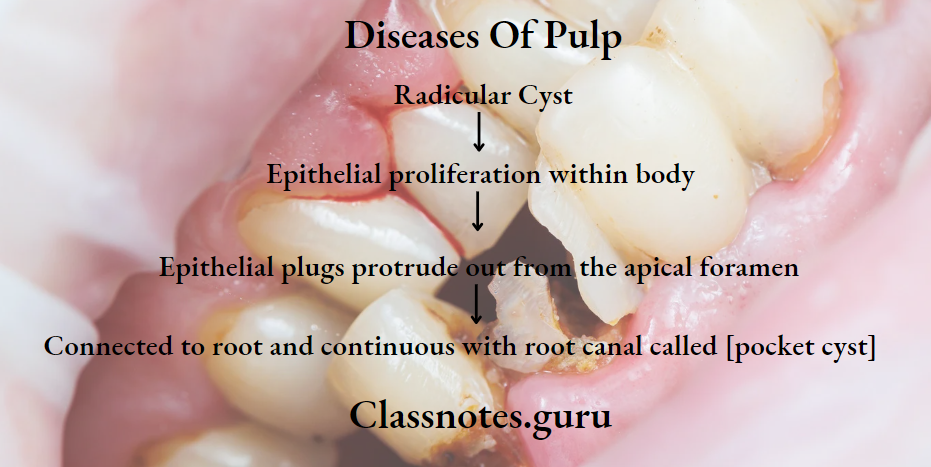
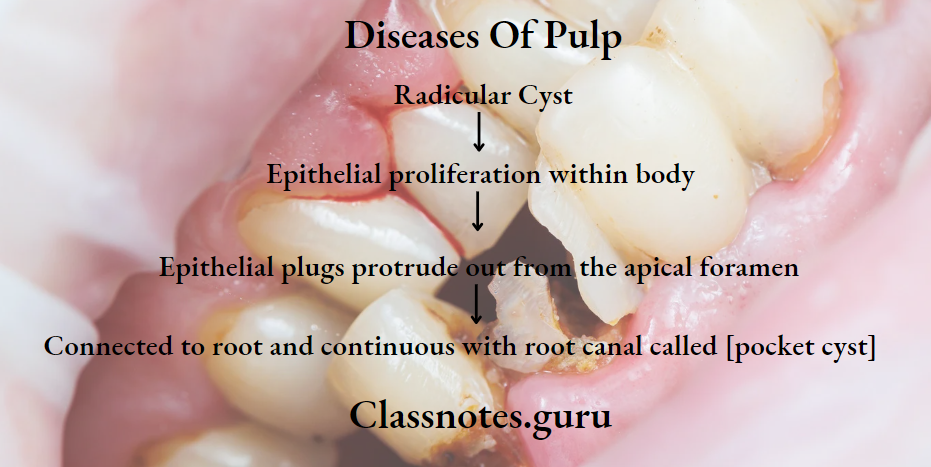
Question 5. Radicular Cyst.
Answer.
Radicular Cyst
Inflammatory cyst
Radicular Cyst Etiology:
- Caries
- Trauma
- Developmental defects
Radicular Cyst Symptoms:
- Asymptomatic
- Gradual swelling
- Palatal expansion
- Non-vital tooth
Radicular Cyst Radiograph:
- Round, pear/ovoid radiolucency
- Narrow radiopaque margin
Radicular Cyst Treatment:
- Endodontic treatment
- Apicoectomy
- Extraction
- Enucleation
Diseases Of Pulp Short Questions And Answers
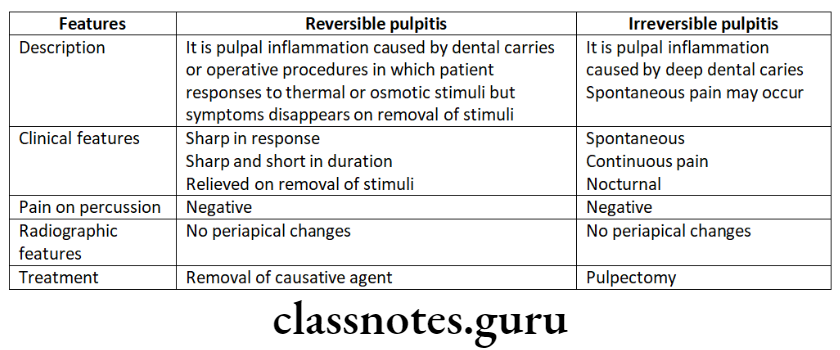
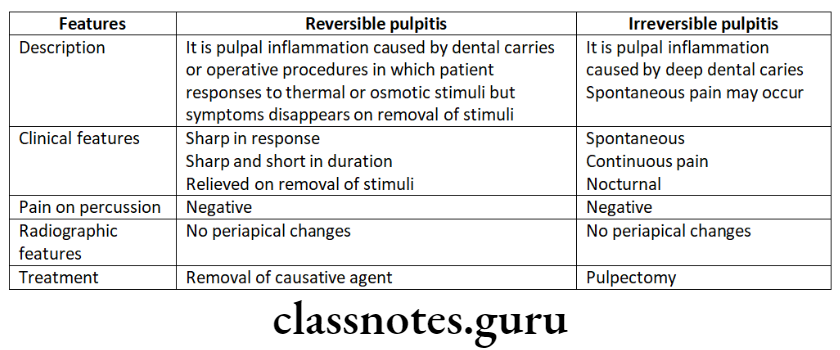
Question 1. Reversible and irreversible pulpitis – differences
Answer.
Reversible And Irreversible Pulpitis
Necrosis Of Dental Pulp
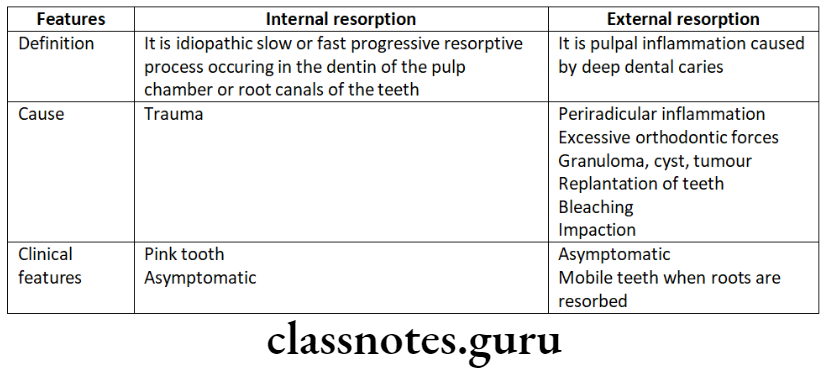
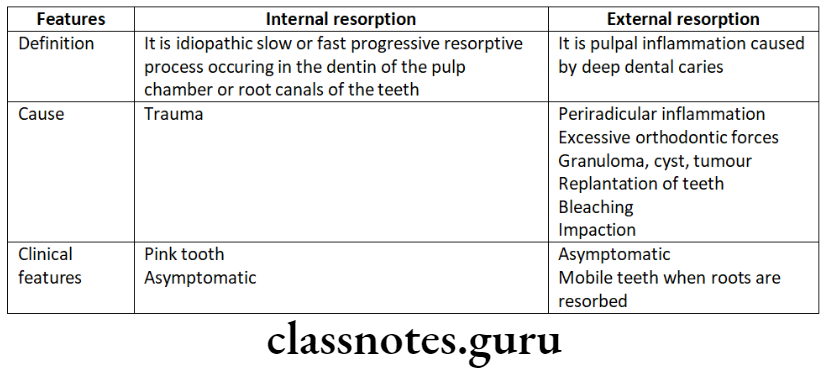
Question 2. Differences between internal and external resorption.
Answer.
Difference Between Internal And External Resorption
Question 3. Root resorption.
Answer.
Root Resorption
Resorption of teeth can be defined as chronic progressive damage or loss of tooth structure due to the action of odontoclasts
Root resorption Classification
- Physiological:
- Resorption of roots of deciduous teeth
- Pathological:
- External resorption
- Internal resorption
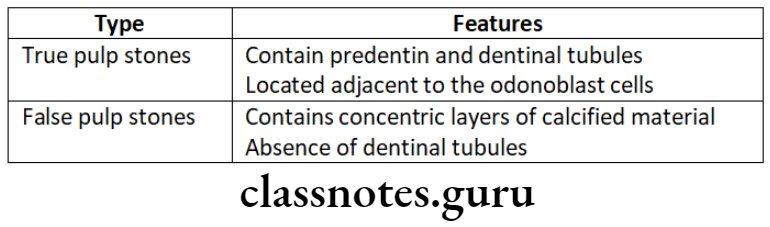
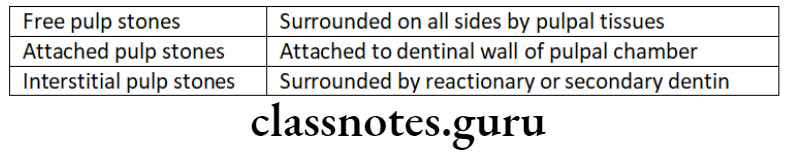
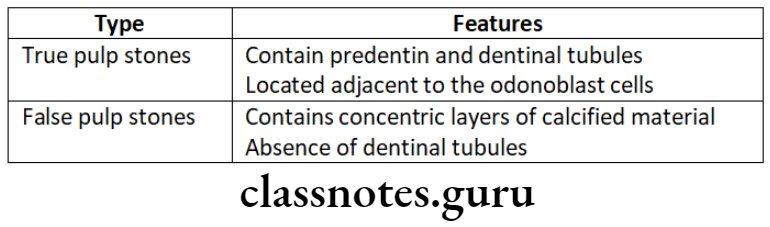
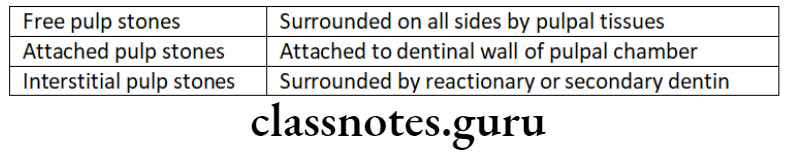
Question 4. Pulp stones.
Answer.
Pulp Stones
Deposition of calcified mass within the dental pulp for no apparent reason is called pulp calcification
Pulp Stones Types:
- Depending On The Microscopic Structure:
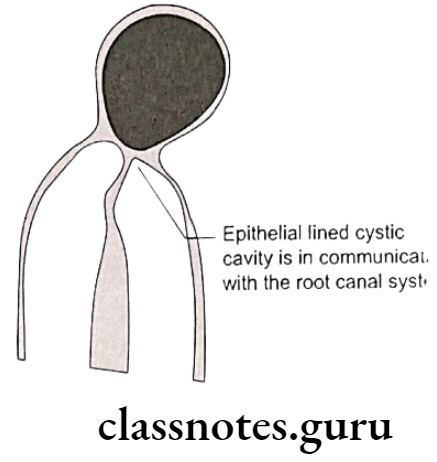
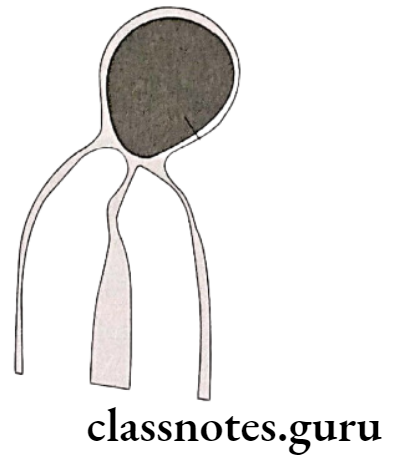
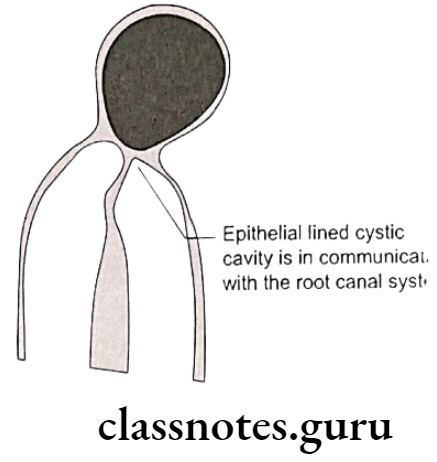
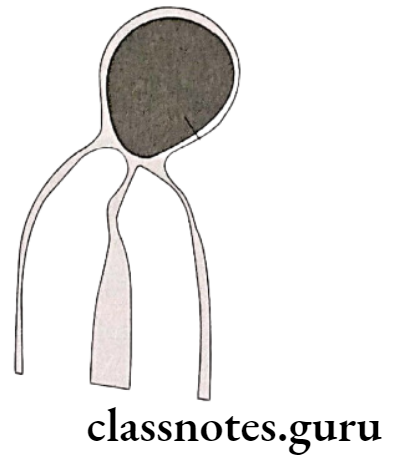
Question 5. Pocket Cyst.
Answer.
Pocket Cyst
Pocket Cyst is the variation of the radicular cyst.
Pocket Cyst Athogenesis:
Reversible Vs Irreversible Pulpitis
Question 6. Pink tooth.
Answer.
Pink Tooth Etiology:
- Trauma, Chronic pulpitis:
Pink Tooth Pathogenesis:
Pink Tooth Symptoms:
- Asymptomic
- Appears pink due to inflamed pulp
Pink Tooth Treatment:
Question 7. Pulpal Diseases Classification.
Answer.
Pulpitis:
Pulpal Degeneration:
Necrosis:
Question 8. Classification of Periradicular Diseases.
Answer.
- Acute peroradiculae diseases.
- Acute alveolar abscess
- Acute apical periodontitis
- Chronic periradicular disease.
- Chronic alveolar abscess
- Granuloma
- Cyst
- Condensing osteitis
- External root resorption
- Diseases with non-endodontic origin
Question 9. Irreversible Pulpitis.
Answer.
Irreversible Pulpitis
Irreversible Pulpitis is a persistent inflammatory condition of pulp.
Irreversible Pulpitis Classification:
Irreversible Pulpitis Etiology:
Irreversible Pulpitis Features:
- Sharp piercing, shooting, continuous pain that remains even after removal of stimulus
- Referred pain
- Difficult to localize
- D/D – Reversible Pulpitis
Irreversible Pulpitis Treatment:
Diseases Of Dental Pulp
Question 10. Causes of Pulpal diseases.
Answer.
Causes Of Pulpal Diseases
- Pulpal Diseases Physical:
- Mechanical:
- Trauma
- Pathologic wear
- Crack tooth syndrome
- Barodontalgia
- Thermal injury
- Electrical injury
- Pulpal Diseases Chemical:
- Phosphoric acid
- Acrylic monomer
- Pulpal Diseases Bacterial:
Question 11. Anachoresis.
Answer.
Anachoresis
Question 12. Aerodontalgia.
Answer.
Aerodontalgia
- Dental pain occuring due to change in altitude
Aerodontalgia Features:
- Asymptomatic at ground level
- Pain occurs after few hours of reaching high altitude or into deep sea
Aerodontalgia Reason:
Question 13. Reversible Pulpitis.
Answer.
Reversible Pulpitis
Reversible Pulpitis is an acute inflammatory response to noxious stimuli
Reversible Pulpitis Etiology:
- Trauma
- Thermal injury
- Chemical stimulus
- Deep restoration
Reversible Pulpitis Symptoms:
- Sharp sudden pain on stimulus
- Pain relieves on removal of stimuli
Reversible Pulpitis Diagnosis:
- Clinically – caries
- Traumatic occlusion
- Percussion test – Negative
- Radiograph – Normal PDL and lamina dura
- Vitality – Early response
Reversible Pulpitis Treatment:
- No endodontic treatment is required
- Sedative dressing placed
- Desensitize the tooth
- Use of cavity varnish
Pulp Diseases In Endodontics
Question 14. Acute alveolar abscess
Answer.
Acute Alveolar Abscess
- Acute alveolar Abscess is a localized collection of pus in the alveolar bone at the root apex of the tooth following the death of pulp with the extension of the infection through the apical foramen into periarticular tissue
Acute Alveolar Abscess Etiology:
- Invasion of bacteria from necrotic pulpal tissue
- Trauma, chemical or mechanical
- Chemical or mechanical treatment causing periapical tissue irritation during root canal treatment
Acute Alveolar Abscess Clinical Features:
- Fever, increased WBC count
- Tooth is non-vital
- Rapid onset of pain
- Slight tenderness to intense throbbing pain
- Marked pain to biting
- Swelling
- Mobility
Acute Alveolar Abscess Treatment:
- Drainage of abscess
- Incision and drainage
- Extraction
Diseases Of Pulp Viva Voce
- In acute apical abscess, pain is due to the build-up of pressure periodically due to the accumulation of pus
- Internal resorption is also known as Pink tooth of mummery
- The sinus tract prevents exacerbation of the lesion by providing continuous drainage of the periradicular lesion
- Anachoresis refers to the attraction or fixation of blood-borne bacteria in areas of inflammation
- Internal resorption is due to asymptomatic and chronic irreversible pulpitis
- Abnormally exaggerated subjective response to painful stimuli is called hyperpathia
- Allodynia is spontaneous pain
- Dysasthesia pain arises from the pulp and periradicular tissues
- The hallmark sign of neuropathic pain is hyperalgesia
- Enamel cracks can be better disclosed by using a dye or by transilluminating the tooth with fiber-optic
- Chronic pulpitis is difficult to diagnose because the patient does not have any subjective symptoms
- Diagnosis of cracked tooth syndrome is made by biting on a solid object and releasing pressure