Salivary Glands Important Notes
1. Sialolith Is Common In The Submandibular Gland Due To
- The tortuous course of Wharton’s duct
- Higher calcium and phosphorous content
- Dependent position of submandibular salivary gland
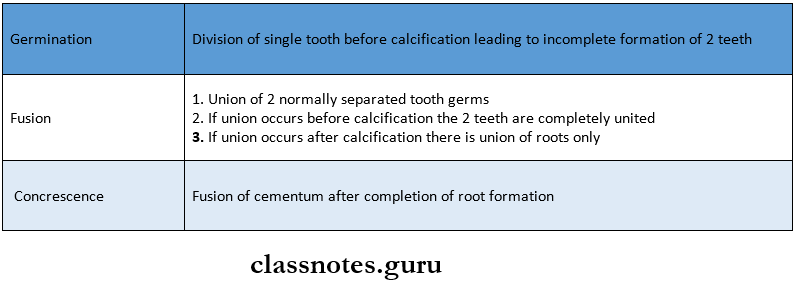
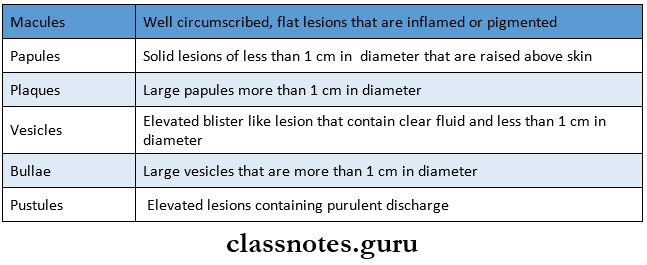
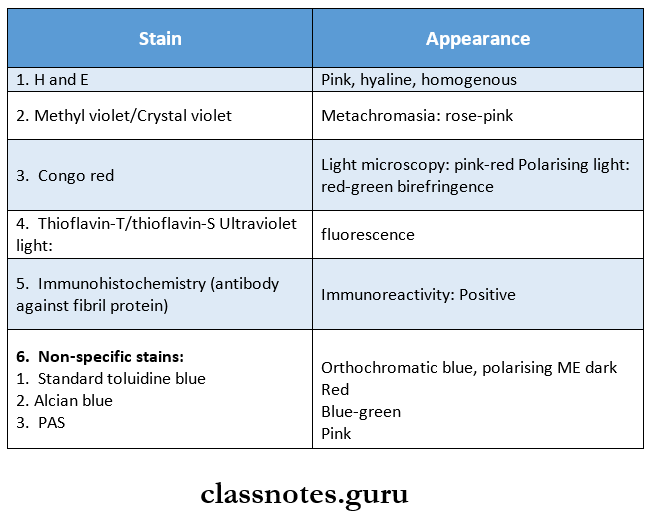
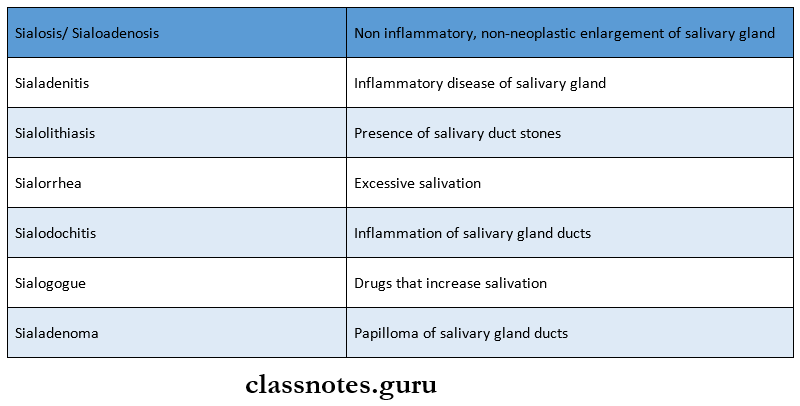
2. Various terms
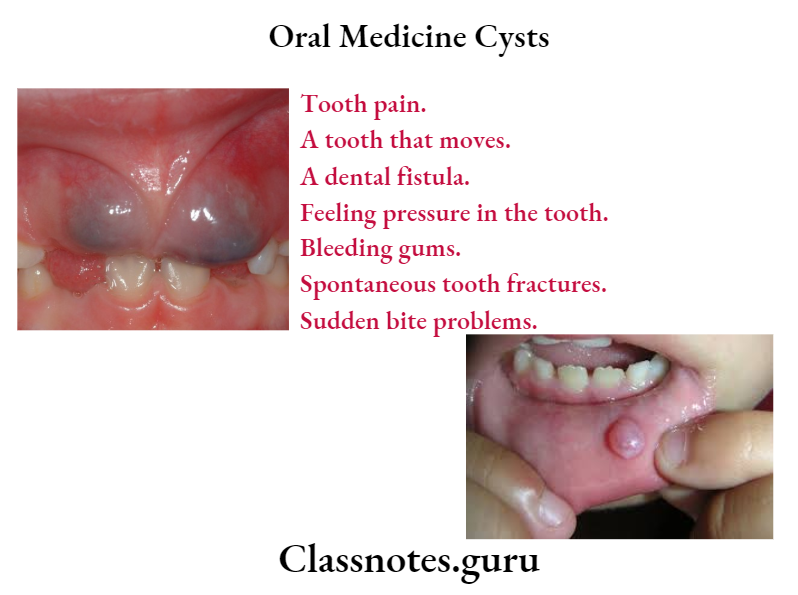
3. Mucocele
- Originates due to rupture of salivary duct following trauma
- Results in pooling of saliva
- Types
- Extravasation
- Retention
4. Ranula
- Associated with sublingual gland
- Causes swelling in the floor of the mouth below the tongue
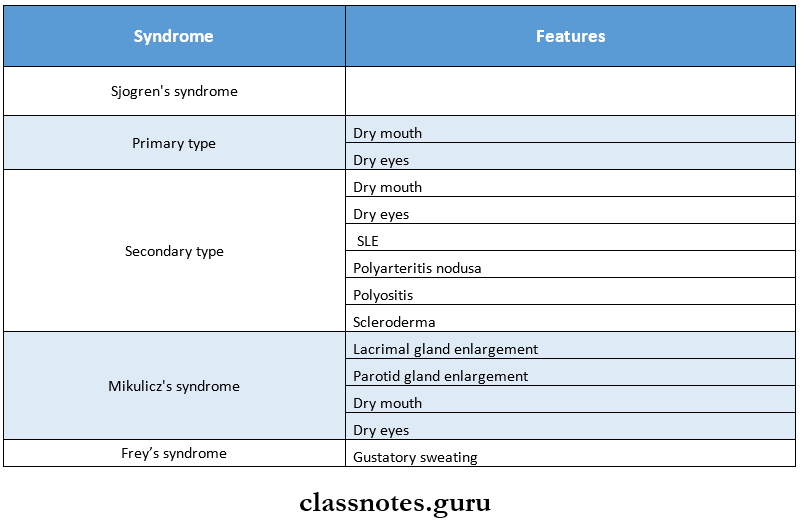
5. Syndrome
Read And Learn More: Oral Medicine Question and Answers
6. Causes Of Xerostomia
- Duct calculi
- Sialadenitis
- Drugs like anticholinergic, sympathomimetics, tricyclic antidepressants, bronchodilators, diuretics
- Sjogren’s syndrome
- Patients under radiotherapy
- Ectodermal dysplasia
- Parkinson’s disease
- Diabetes
Oral Medicine Salivary Glands Long Essays
Question 1. Enumerate autoimmune diseases. Discuss clinical features, diagnosis, And management of Sjogren’s syndrome
or
Classify functional disorders of salivary glands. Discuss the etiology, clinical features, diagnosis, and management of Sjogren’s syndrome.
Answer:
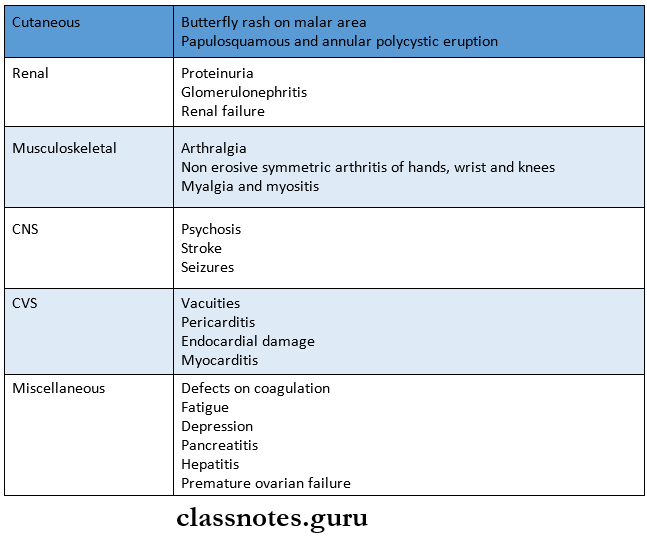
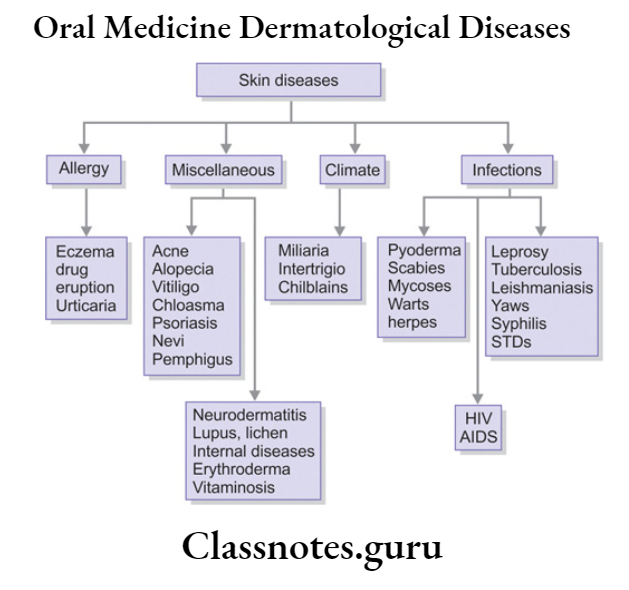
Autoimmune Disorders:
- Associated With Mucocutaneous Leions « Recurrent Aphthous Ulcer
- Behcet’s disease
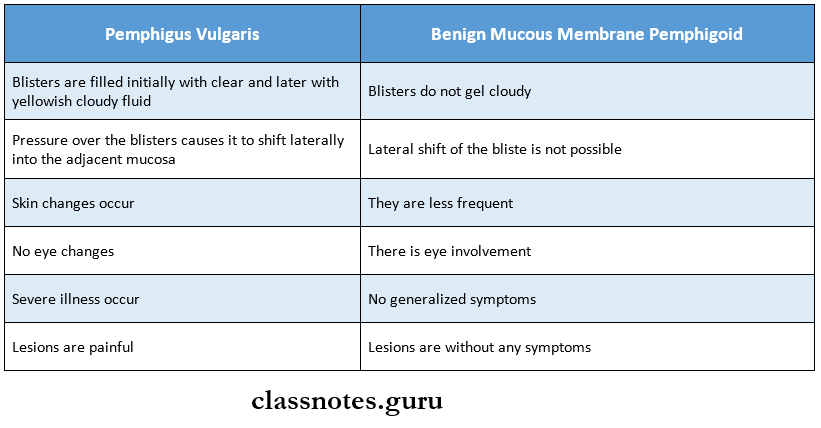
- Pemphigus
- Salivary Gland
- Mikulicz’s disease a Sjogren’s syndrome
- Blood Disorder
- Pernicious anemia
- Purpura
- Collagen Disorder
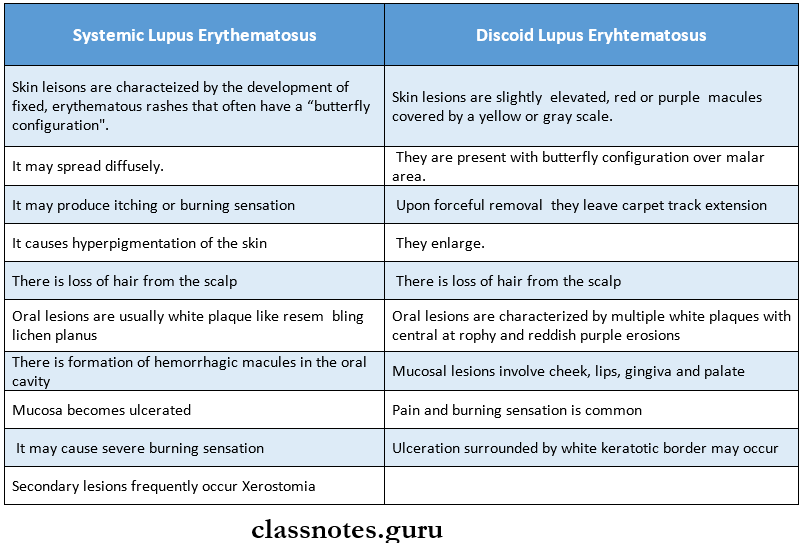
- Systemic lupus erythematous
- Scleroderma
- Rheumatic arthritis
- Miscellaneous
- Myasthenia gravis
- Oral submucous fibrosis
Salivary Glands Functional Disorders:
- Sialorrhoea
- Xerostomia
Sjogren’s Syndrome:
- It is a chronic autoimmune disease
- Characterize by oral and ocular dryness, exocrine dysfunction, and lymphocytic infiltration
Salivary Glands Types:
1. Primary:
- It involves the salivary and lacrimal gland
2. Secondary:
- It also involves other connective tissue diseases (rheumatoid arthritis, scleroderma)
Etiology:
- It is unknown
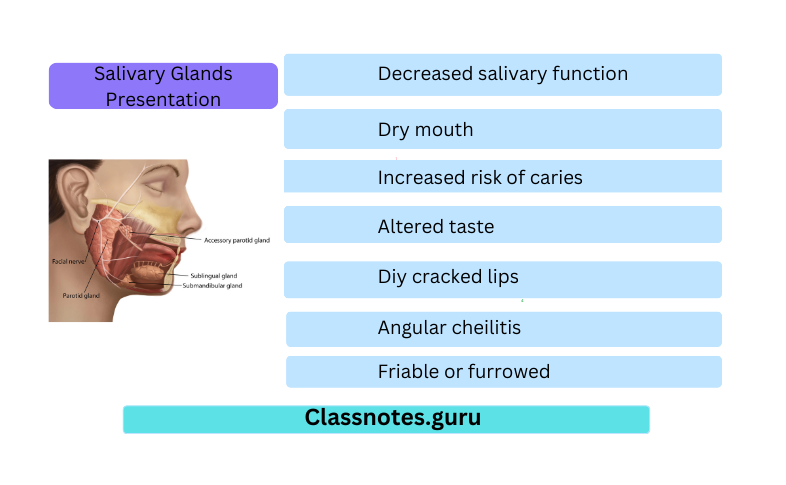
Salivary Glands Presentation:
- Decreased salivary function
- Dry mouth
- Difficulty in chewing, swallowing, and speech
- Increased risk of caries
- Altered taste
- Diy cracked lips
- Angular cheilitis
- Mucosa is painful and sensitive to species
- Mucosa is pale and dry
- Friable or furrowed
- Minimal salivary pooling
- The tongue is smooth and painful
- Increased dental caries and erosion of enamel
- Susceptible to infection
- Increased risk of developing malignant lymphoma
- Difficulty in wearing dentures
- From one-third to one-half of the patients have diffuse, firm enlargement of major salivary glands
- Swelling is usually bilateral
- Maybe non-painful or slightly tender
- May be intermittent or persistent
- Due to decreased salivary flow, there is a high risk of bacterial sialadenitis
Salivary Glands Lab Investigations:
- Hypergammaglobulinemia
- Autoantibodies: anti-SS-A and anti-SS-B
- Elevated sedimentation rate
- Decreased WBC
- Monoclonal gammopathies
- Hypocomplementemia
- Rose Bengal test:
- Keratoconjunctivitis sicca is characterized by corneal keratotic lesion, which stains pink when rose Bengal dye is used
- Schirmer’s test:
- A strip of filter paper is placed in between the eye & eyelid to determine the degree of tears measured in mm
- If it is < 5 mm in 5 min, it is positive
- Sialometry:
- It estimates the salivary flow rate
- In Sjogren’s syndrome, it is reduced to 0.5- ml/min(Nl-1.5)
Radiographic Features:
- Sialography:
- It typically demonstrates a “cherry blossom” appearance
- Scintigraphy:
- It shows the decreased flow and delayed emptying of iso¬tope
Salivary Glands Differential Diagnosis:
- Chronic bacterial and granulomatous infection
- Multiple parotid cysts associated with HIV
- Diffuse cervical lymphadenopathy is common in HIV but not in Sjogren’s syndrome
Salivary Glands Management:
- Treated symptomatically
- Dry eyes managed by periodic use of artificial tears
- Conserve the tear film by using sealed glasses to prevent evaporation
- For Xerostomia: use of sugarless candy or gum
- Use of oral hygiene products that contain lactoperoxidase,
- lysozyme and lactoferrin
- Ex: Biotene toothpaste and mouth rinse, oral balance gel
- Sialogogues such as pilocarpine (dose: 5 mg TDSj are used
- Due to the high risk of caries in these individuals daily fluo¬ride application is done
Question 2. Classify salivary gland disorders. Write in detail about the etiology, clinical features, and management of bacterial sialadenitis.
Answer:
Salivary Glands Classification:
1. Developmental Anomalies:
- Agenesis
- Atresia
- Hypoplasia
- Ectopic
2. Obstructive Lesions
- Mucocele
- Sialolithiasis
3. Infective Lesions:
- Bacterial sialadenitis
- Viral sialadenitis
4. Immune Disorders:
- Sjogren’s syndrome
- Mikulicz’s disease
5. Functional Disorders:
- Ptyalism
- Xerostomia
6. Salivary Glands Tumours:
- Epithelial Tumours:
- Adenomas
- Pleomorphic adenoma
- cystadenoma
- Basal cell adenoma
- Warthin’s tumour
- Carcinoma
- Adenocarcinoma
- Epidermoid carcinoma
- Non Epithelial Tumours:
- Fibroma
- Lipoma
- Lymphoma
- Malignant Lymphoma
- Secondary Tumours
- Unclassified Tumours
- Tumour Like Lesions
- Sialadenitis
- Oncocytosis
- Necrotizing sialometaplasia
Bacterial Sialadenitis:
- Bacterial Sialadeniti is a bacterial infection of the salivary glands
Bacterial Sialadeniti Etiology:
- Microorganism: staphyloma/streptococci
- Decreased host resistance
- Poor oral hygiene
- Dehydration
Bacterial Sialadeniti Clinical Features:
- Age: older age
- Site: common in the parotid
Bacterial Sialadeniti Presentation:
Unilateral enlarged and tender gland
↓
Elevation of ear lobes
↓
Redness of overlying skin
↓
Generalized symptoms
↓
Cervical lymphadenopathy
Bacterial Sialadeniti Management:
- Maintenance of oral hygiene
- Soft diet
- Maintenance of electrolyte balance
- Surgical drainage if the above measures fail