Small And Large Intestines Question And Answers
Question 1. Describe in detail about the different parts of the duodenum and its relations.
Answer:
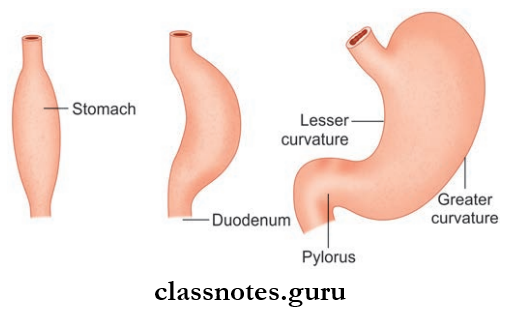
Duodenum
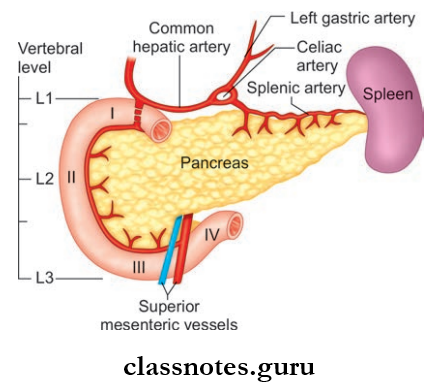
Duodenum Parts:
- Superior
- Descending
- Horizontal
- Ascending
- The first part of small intestine
- It is the shortest and widest part of small intestine
- Length: 25 cm
- Extend: Pylorus to duodenojejunal flxure
- It is generally retroperitoneal except for its beginning
- It is C-shaped
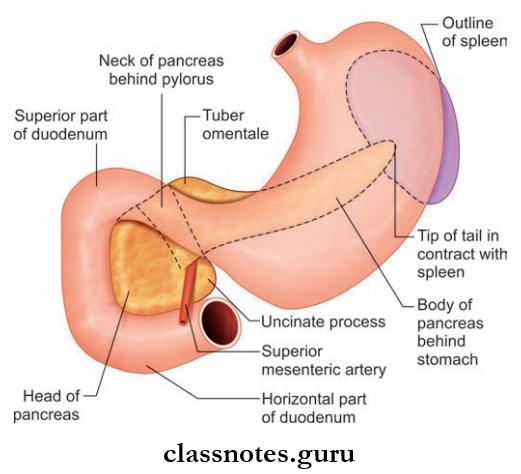
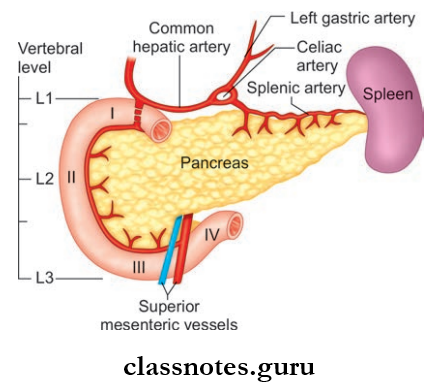
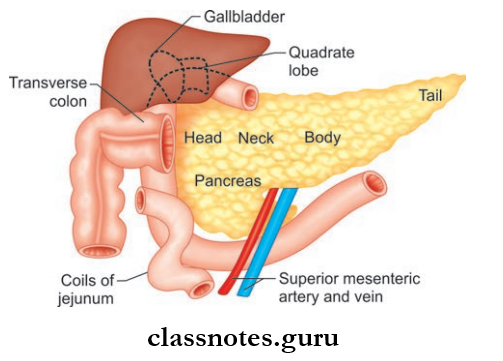
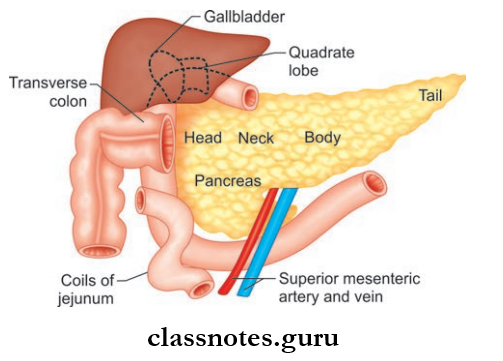
- It encloses the head of pancreas in the concavity of ‘C’
- Vertebral level—L1, L2, L3
Small And Large Intestine Important Questions And Answers
Read And Learn More: Abdomen And Pelvis
Duodenum is divided into 4 parts:
1. Duodenum First Part/Superior Part
- Foregut derivative
- Partly retroperitoneal
- Length: 5 cm
- Extend: Pyloric orifice to neck of the gallbladder
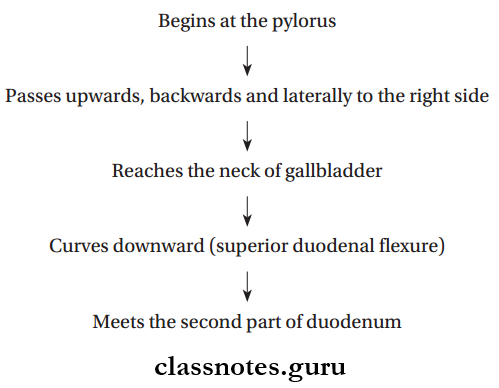
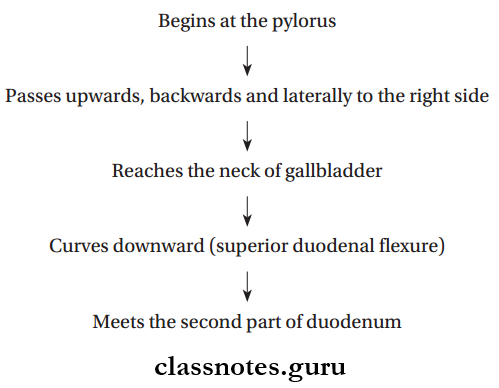
Duodenum First Part Or Superior Part Course:
Duodenum First Part Or Superior Part Relations:
- Peritoneal Relations
- Proximal 2.5 cm
- The intraperitoneal part, it is movable
- Attached To:
- Lesser Omentum:
- Above
- Greater Omentum:
- Below
- Distal 2.5 cm
- Retroperitoneal part, it is fied
- Visceral Relations
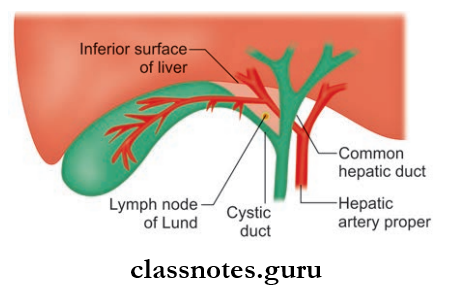
- Anteriorly
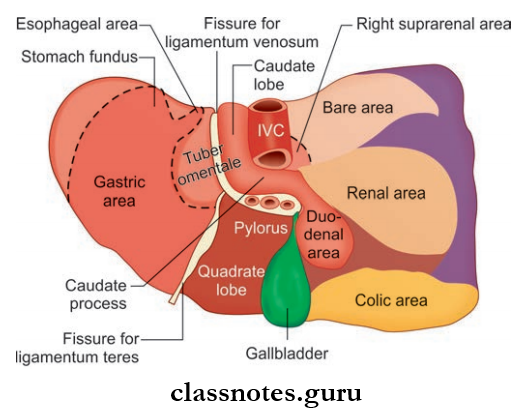
- Quadrate lobe of liver
- Gallbladder
- Posteriorly
- Gastroduodenal artery
- Common bile duct
- Portal vein
- Superiorly: Epiploic foramen
- Inferiorly: Head and neck of the pancreas
Duodenum First Part Or Superior Part Applied Anatomy
- The first part of the duodenum is overlapped by the liver and gallbladder; either of these structures can adhere to the duodenum, and may be eroded by the duodenal ulcer, if present
- It is in the first part of the duodenum where the majority of ulcers are present.
Human Small And Large Intestine Questions And Answers
2. Duodenum Second Part/Descending Part
- Upper Half Of 2nd Part Up To Ampulla Of Vater: Foregut derivative
- Lower Half Of 2nd Part From Ampulla Of Vater: Midgut derivative
- Length: 7.5 cm
- Duodenum Second Part/Descending Part Extend: Neck of gallbladder to lower border of L3 vertebrae
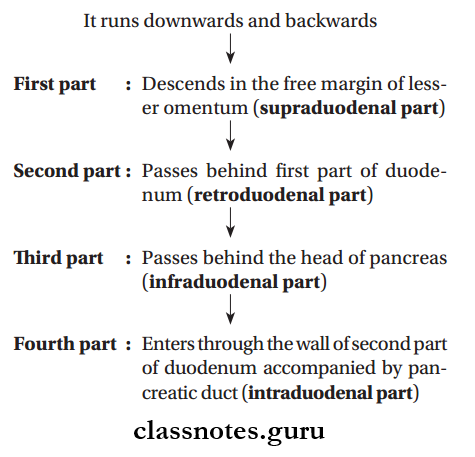
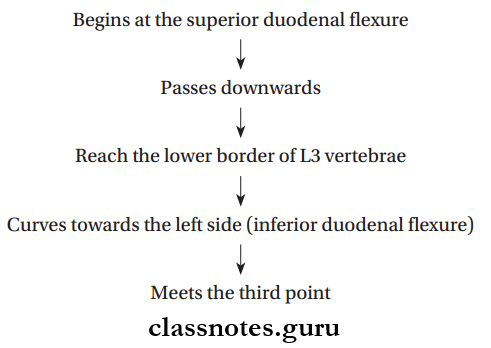
Duodenum Second Part/Descending Part Course:
Duodenum Second Part/Descending Part Relations
- Peritoneal
- Retroperitoneal
- Fixed
- The anterior surface is covered by the peritoneum mostly
- Except at a region near the middle of the second part (here it is in direct contact with the colon)
- Visceral
- Anteriorly
- Right lobe of liver
- Gallbladder
- Transverse colon
- Transverse mesocolon
- Coils of intestine
- Posteriorly
- Anterior surface of right kidney
- Right renal vessels
- Right edge of inferior vena cava
- Right psoas major
- Medially
- Head of the pancreas
- Bile duct
- Laterally
- Right lobe of liver
- Right colic flexure
- Ascending colon
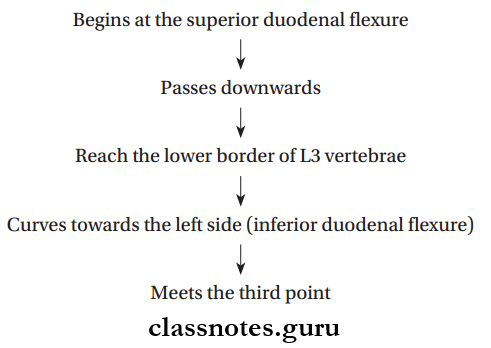
3. Duodenum Third Part/Inferior Part
- Derived from midgut
- Longest part
- Length – 10 cm
Intestines Anatomy And Function MCQs
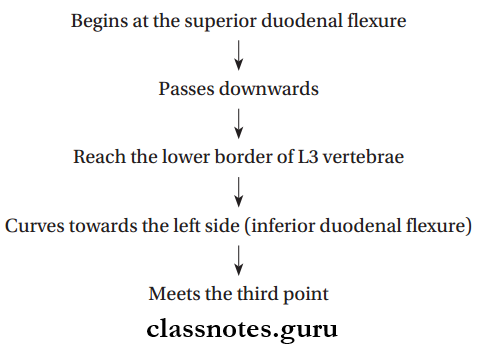
Duodenum Third Part/Inferior Part Course:
Duodenum Third Part/Inferior Part Relations
- Peritoneal
- Retroperitoneal, fied
- The anterior surface is covered by the peritoneum all over except at the regions in the median plane, where it is crossed by superior mesenteric vessels and root of the mesentery
- Visceral
- Anteriorly
- Root of mesentery
- Superior mesenteric vessels
- Coils of jejunum
- Posteriorly
- Right ureter
- Right psoas major
- Inferior vena cava
- Abdominal aorta
- Right testicular/ovarian vessels
- Superiorly: Head of pancreas and it’s uncinate process
- Inferiorly: Coils of jejunum
Duodenum Fourth Part/Ascending Part
- Derived from midgut
- Retroperitoneal
- Length – 2.5 cm
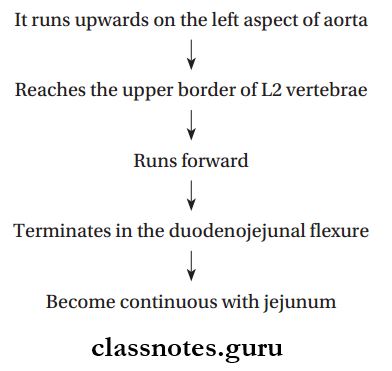
Duodenum Fourth Part/Ascending Part Course:
Duodenum Fourth Part/Ascending Part Relations
- Peritoneal
- Anteriorly covered by peritoneum
- Terminal part is mobile and suspended by the mesentery
- Visceral
- Anteriorly
- Transverse colon
- Transverse mesocolon
- Lesser sac
- Posteriorly
- Left psoas major muscle
- Left sympathetic chain
- Left renal artery
- Left gonadal artery
- Inferior mesenteric vein
- Superiorly: Body of pancreas
- To The Right: Upper part of the root of mesentery
- To The Left:
Small Intestine Vs Large Intestine – Differences
Question 2. Describe briefly about the interior of duodenum.
Answer:
The Interior Of Duodenum:
Mucosa Shows Plica Circularis: The permanent spiral folds, villi—permanent figer-like projections of lamina propria that extend into the intestinal lumen, microvilli—the cytoplasmic extensions that cover the apices of intestinal absorptive cells—all these aids the absorption better
The Interior Of 2nd Part Of the Duodenum Has The Following Special Features:
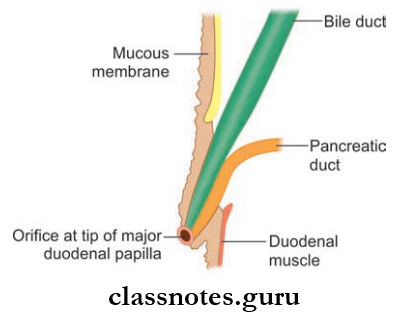
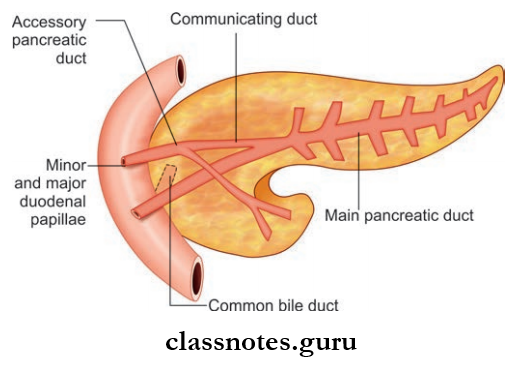
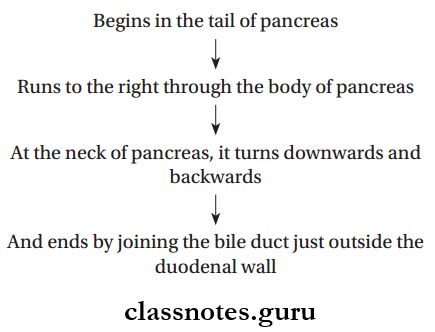
- Major Duodenal Papilla:
- It is an elevation present on the posteromedial wall of the duodenum
- Situated 8–10 cm distal to pylorus
- The common hepatopancreatic duct opens at the summit of the papilla.
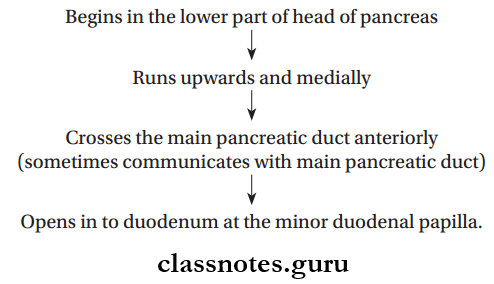
- Minor Duodenal Papilla:
- It is a small conical elevation situated 6–8 cm distal to the pylorus
- The accessory pancreatic duct opens at the summit of the papilla.
- Arch Of Plica Semicircularis:
- They are permanent folds of mucous membrane and form complete or incomplete circles
- They begin in the second part of duodenum
- It forms an arch above the major duodenal papilla like a hood.
- Plica Longitudinalis:
- Vertical tortuous fold of mucous membrane
- Extends downwards from major duodenal papilla.
Question 3. Write a note on the blood supply, lymphatic drainage, and nerve supply of different parts of the duodenum.
Answer:
Different Parts Of The Duodenum
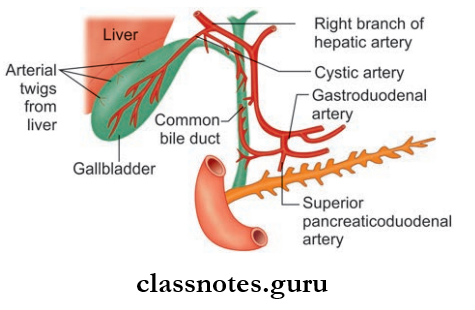
Blood Supply of Duodenum
- Duodenum is developed from the foregut up to the level of opening of the bile duct into the 2nd part
- Below this level, it is derived from the midgut
- So Part Of The Duodenum:
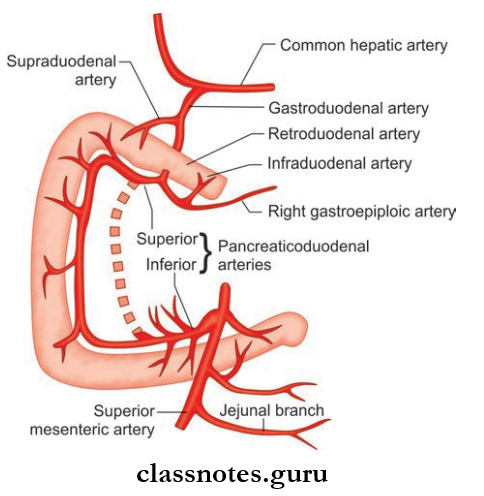
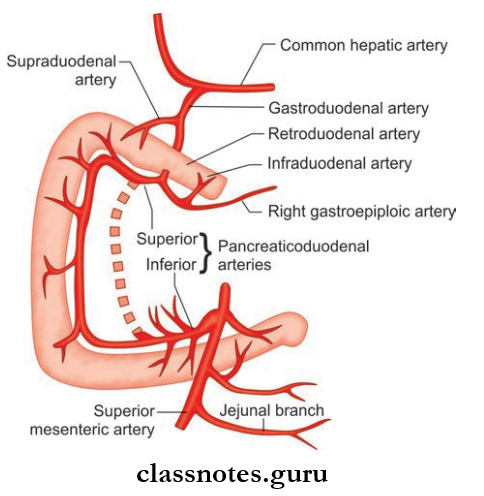
- Derived From Foregut: Supplied by superior pancreaticoduodenal artery, a branch of the celiac trunk (artery of foregut)
- Derived From Midgut: Supplied by the inferior pancreaticoduodenal artery, a branch of the superior mesenteric artery (artery of midgut)
- Both these arteries give of anterior and posterior branches
- These branches anastomose and forms anterior and posterior pancreaticoduodenal arterial arcades and supply duodenum
- Additional supply for the first part of the duodenum
- Right gastric artery
- Supraduodenal artery of Wilkie
- Retroduodenal artery
- Infraduodenal artery.
Duodenum Venous Drainage: Veins drain into
- Splenic vein
- Superior mesenteric vein
- Portal vein.
Duodenum Lymphatic Drainage
Lymph flows into pancreaticoduodenal nodes—it lies at the junction of the pancreas and duodenum (inner curve of the duodenum)
Duodenum Nerve Supply
- Sympathetic Supply: From T9–T10 spinal segments
- Parasympathetic Supply: From vagus, through celiac plexus and superior mesenteric plexus.
Question 4. What is the duodenal cap?
Answer:
Duodenal cap
In a barium meal procedure, after intake of contrast, the first part of the duodenum becomes visible in the radiograph as a triangular shadow called the duodenal cap and is emptied to the jejunum every one minute.
Digestive System Questions On Intestines
Question 5. Write a note on the ligament of Treitz.
Answer:
Ligament of Treitz
- Suspensory muscle of duodenum
- It consists of a fibromuscular band, suspending the duodenojejunal flexure from the right crus of the diaphragm
Ligament Of Treitz Attachments:
- Upper end: Right crus of the diaphragm
- Lower end: Posterior aspect of duodenojejunal flexure
- This band comprises of 3 types of fibers (from above to below)
- Striated muscle fibers
- Elastic fibers
- Non-striated muscle fibers
Ligament Of Treitz Functions
- Fixes the duodenojejunal flexure and prevents the pulling down by loop of the intestine
- In the radiological investigation of the duodenum, the position of the ligament of Treitz is of utmost importance, normally it should be demonstrated to the left of and at the same level or above of the first part of the duodenum.
- Change in position indicates malrotation of the duodenum
- Embryologically, it is derived from mesoderm.
Question 6. Differentiate between jejunum and ileum.
Answer:
Difference Between Jejunum And Ileum
- The mobile part of the intestine
- Extend: Duodenojejunal flexure to the ileocecal junction
- They are suspended from the posterior abdominal wall by mesentery, which gives them considerable mobility
- The jejunum is located in the left upper quadrant and the ileum in the right lower quadrant of the abdomen.
Jejunum
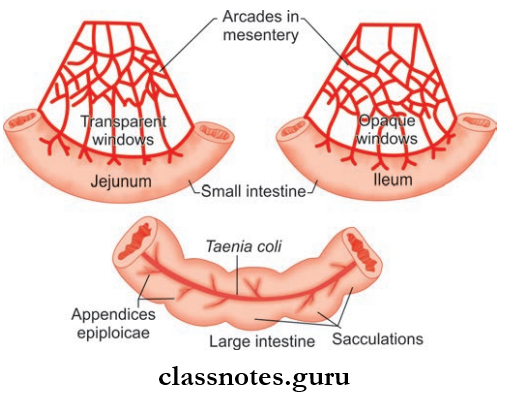
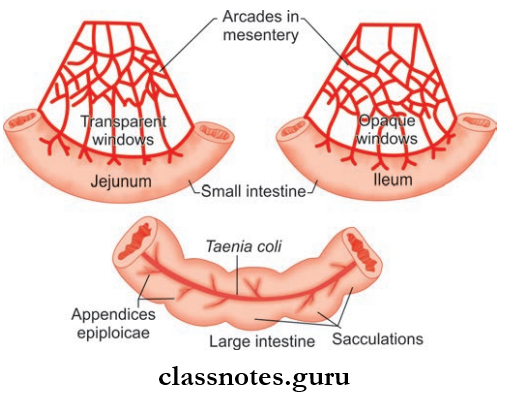
- Length: Upper 2/5th of the mobile part of small intestine
- Wall: Thicker and more vascular
- Lumen: Wider (diameter–4 cm) and often empty
- Villi: Larger, thicker, and leaf-like and numerous
- Plica circulars: Longer and more closely set
- Mesentery: Contains less fat
- 1 or 2 arterial arcades
- Vasa recta are longer and fewer
- Windows present
- Peyer’s patches: Absent
Ileum
- Length: Lower 3/5th of the mobile part of small intestine
- Wall: Thinner and less vascular
- Lumen: Narrower (diameter-3.5 cm) and often full
- Villi: Shorter thinner and figer like
- Plica circulars: Smaller and sparsely set
- Mesentery: Contains more fat
- 3–6 arterial arcades
- Vasa recta shorter and numerous
- Windows absent
- Peyer’s patches: Present
Small And Large Intestine Neet Questions
Question 7. Write a note on the blood supply, lymphatic drainage, and nerve supply of the jejunum and ileum.
Answer:
Jejunum And Ileum Arterial Supply
- Jejunum: Jejunal arteries from the superior mesenteric artery
- Ileum: Two arteries
- Ileal Arteries: Branch of superior mesenteric artery
- Ileal branch from the ileocolic artery
- These arteries enter the mesentery and get divided into smaller branches
- Smaller branches anastomoses and form arterial arcades
- Arterial arcades are more complex in the ileum
- From the concavities of arterial arcades, small parallel, and straight vessels arise, known as vasa recta, supplies the opposite surface of the small intestine.
Jejunum And Ileum Venous Drainage
Drained by corresponding veins of the arteries, into superior mesenteric vein.
Jejunum And Ileum Lymphatic Drainage
Lymph vessels of small intestine mesenteric lymph nodes superior mesenteric nodes.
Jejunum And Ileum Nerve Supply
- Sympathetic Supply: From T10–T11 segments, through splanchnic nerves and superior mesenteric plexus
- Parasympathetic Supply: From the vagus nerve, through celiac and superior mesenteric plexuses
- Due to T10 Supply: Pain is referred to as umbilicus (T10 segment).
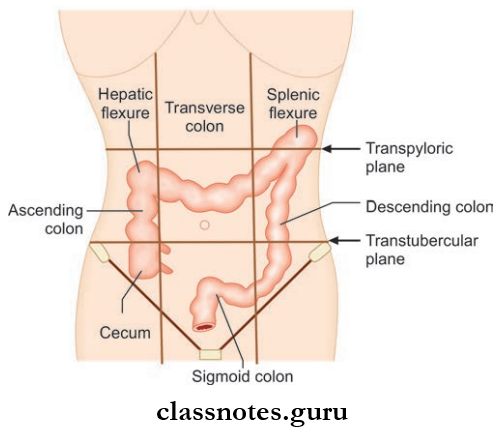
Question 8. Mention about the features of the large intestine.
Answer:
Large Intestine
- Wider than the small intestine
- Length: 1.5 m
- Extend: Ileocecal junction to anus
Large Intestine Divided into:
- Cecum
- Ascending colon
- Transverse colon
- Descending colon
- Sigmoid colon
- Rectum
- Anal canal
Large Intestine Appendix: It is a narrow diverticulum present at the angle between the cecum and the terminal part of the ileum
The Gross Distinguishing Features Of The Large Intestine Are: Taenia coli
- They are three ribbon-like bands of the longitudinal muscle coat
- Proximally these bands converge at the base of the appendix and spread out to become continuous with a longitudinal muscle coat of the rectum
- Based on the position of taenia coli on the cecum, ascending colon, descending colon, and transverse colon they are named accordingly:
1. Taenia Libera Mesocolic
- Position In The Cecum, Ascending Colon, And Descending Colon: Anterior
- Position In The Transverse Colon: Inferior
2. Taenia Mesolica
- Position In The Cecum, Ascending Colon, And Descending Colon: Posteromedial
- Position In The Transverse Colon: Posterior
3. Taenia Omentalis
- Position In Cecum, Ascending Colon, And Descending Colon: Posterolateral
- Position In The Transverse Colon: Superior
Intestines Viva Questions And Answers
Large Intestine Appendices Epiploic:
- Fat filed bags of visceral peritoneum attached to taenia coli
- Thy are seen on all parts of the large intestine except in the appendix, rectum, and anal canal
Large Intestine Sacculations Or Haustrations:
Dilated parts in between the taenia coli, gives the characteristic puckered appearance to the large intestine.
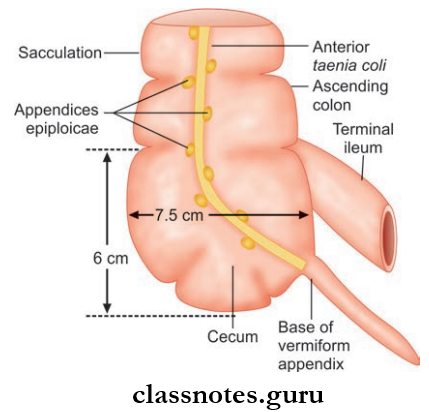
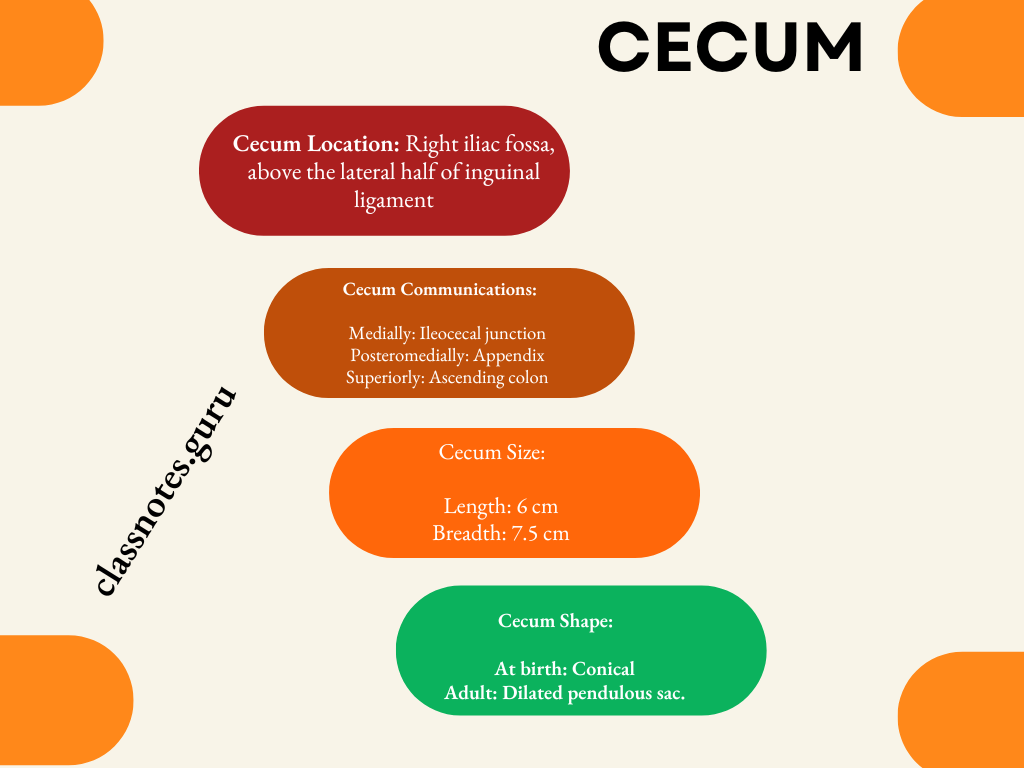
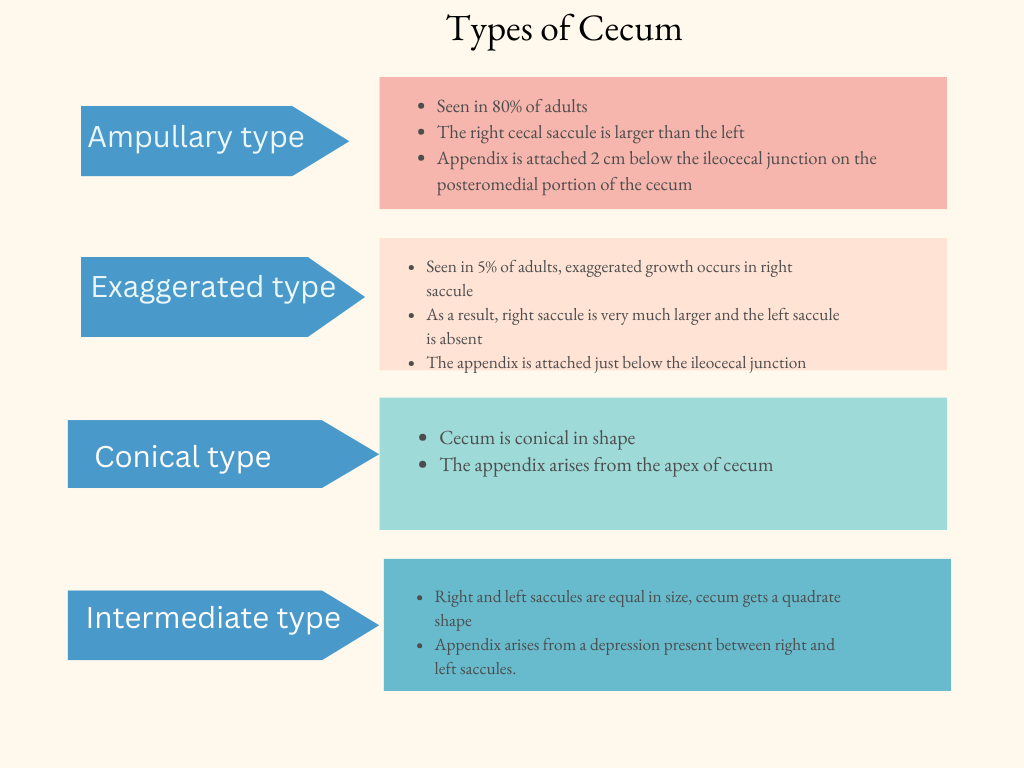
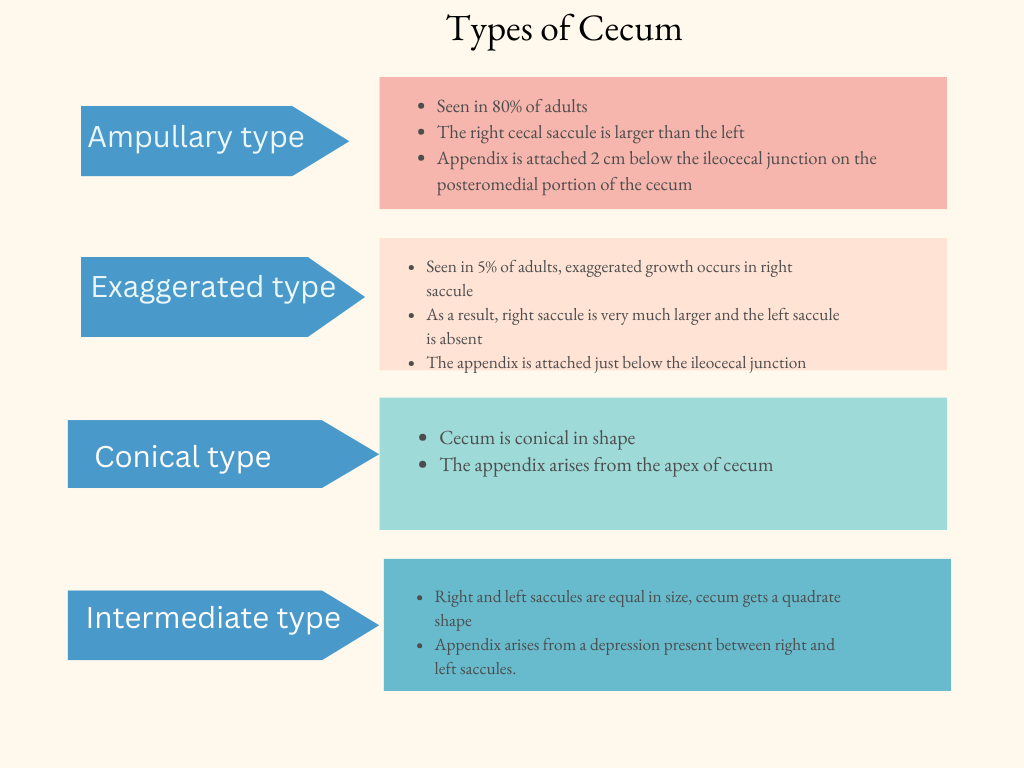
Question 9. Explain in detail about the cecum and briefly mention its development.
Answer:
Cecum
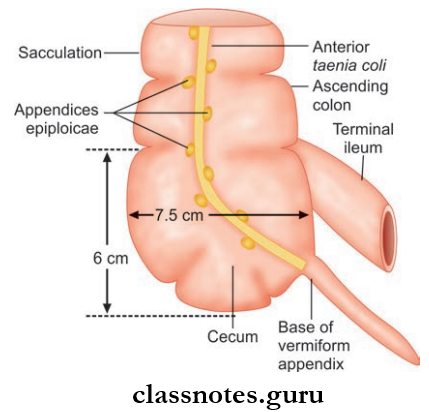
- Dilated sac
- Forms the first part of large intestine
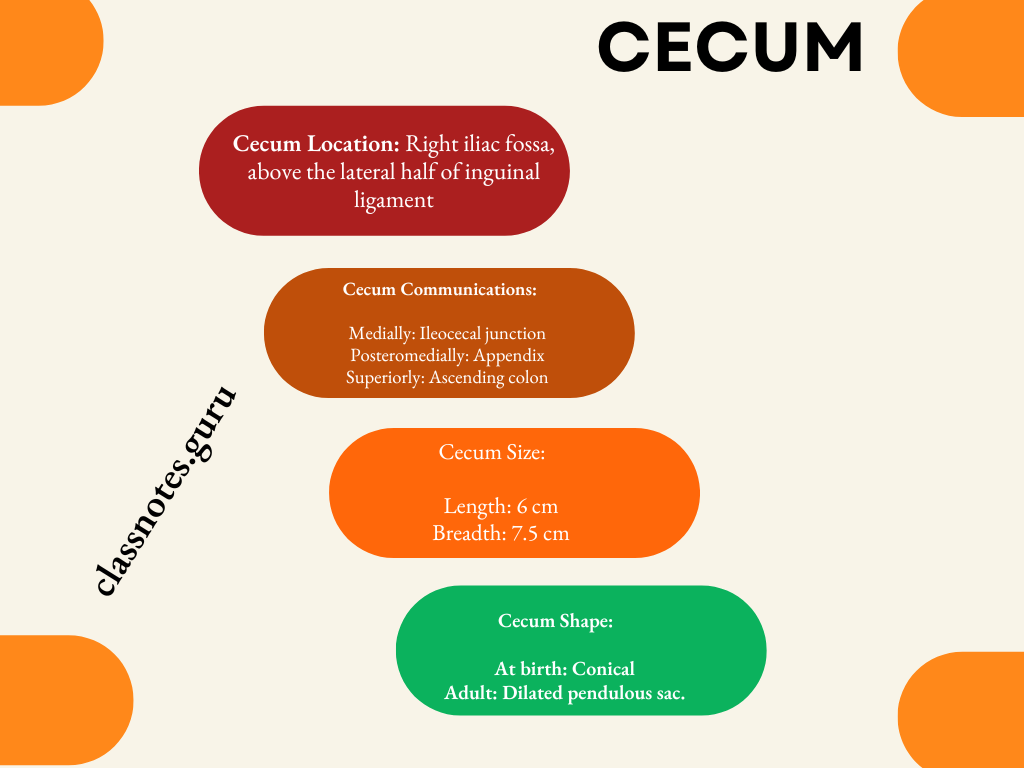
Cecum Relations
- Anteriorly
- Coils of small intestine
- Anterior abdominal wall
- Greater omentum
- Posteriorly
- Muscles: Right psoas major, iliacus
- Vessels: Right gonadal vessels, right iliac artery (sometimes)
- Nerves: Femoral nerve, genitofemoral nerve, lateral cutaneous nerve of thigh
- Retrocecal recess containing the appendix.
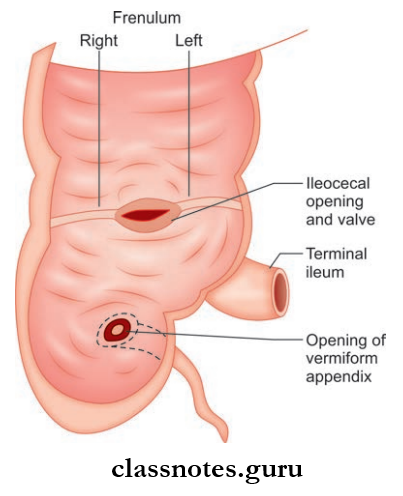
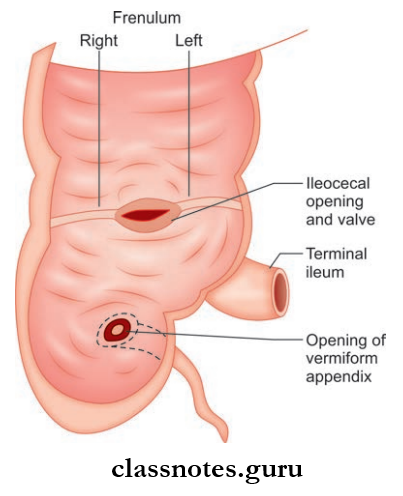
Cecum Orifies And Valves: Cecum has 2 orifices, guarded by their respective valves:
1. Ileocecal Orifice:
- Location: Posteromedial aspect of cecocolic junction
- Measures 2.5 cm transversely
- It is guarded by ileocecal valve.
The Ileocecal Valve Has Two Lips:
- Upper Smaller Horizontal Lip: Lies at ileocolic junction
- Lower Longer Concave Lip: Lies at the ileocecal junction
- The two lips fuse at the ends of the opening and form two frenula—right and left cecal frenulum
- The Valves Are Closed By:
- Sympathetic innervation
- Mechanically by distension of cecum
Ileocecal Orifie Applied Anatomy: The ileocecal valve prevents the reflux of contents from the cecum to the ileum.
2. Appendicular Orifice
- Small circular orifice
- Location: 2 cm below and posterior to ileocecal orifice
- This orifice is also guarded by a semicircular mucous membrane fold known as the valve of Gerlach
Appendicular Orifie Blood Supply
- Arterial Supply: Anterior and posterior cecal branches of the ileocolic artery (branch of a superior mesenteric artery)
- Venous Drainage: Veins accompany the arteries and drain into a superior mesenteric vein, then into portal vein
- Lymphatic Drainage: Lymphatics drain into → Ileocolic nodes → Superior mesenteric group of preaortic lymph nodes.
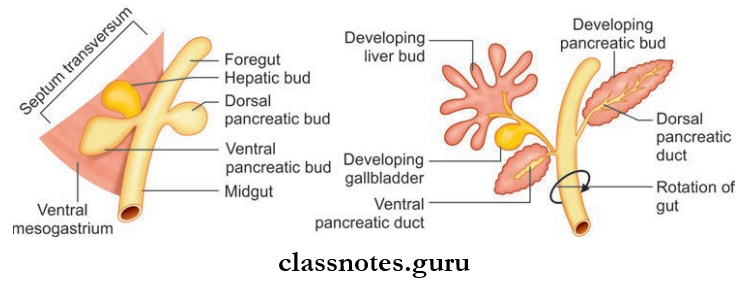
Development Of Cecum
Cecum develops from the proximal part of the cecal bud arising from the caudal limb of the primitive intestinal loop.
Intestines Short Questions And Answers
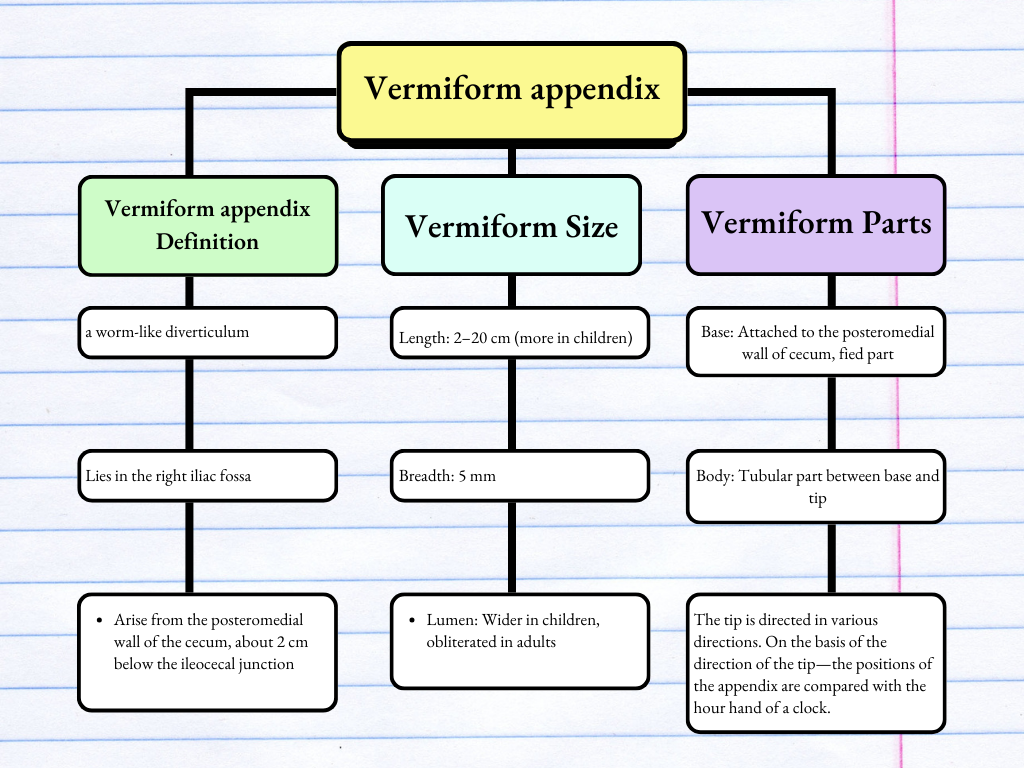
Question 10. What is a vermiform appendix, what are its features and what is its surgical importance?
Answer:
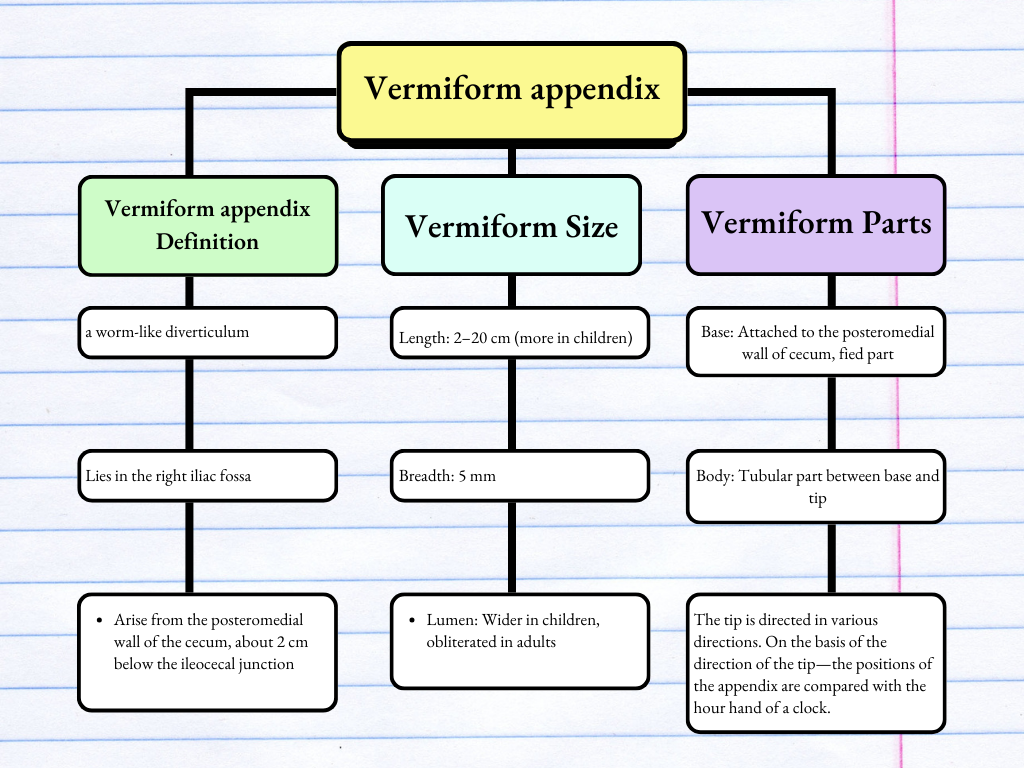
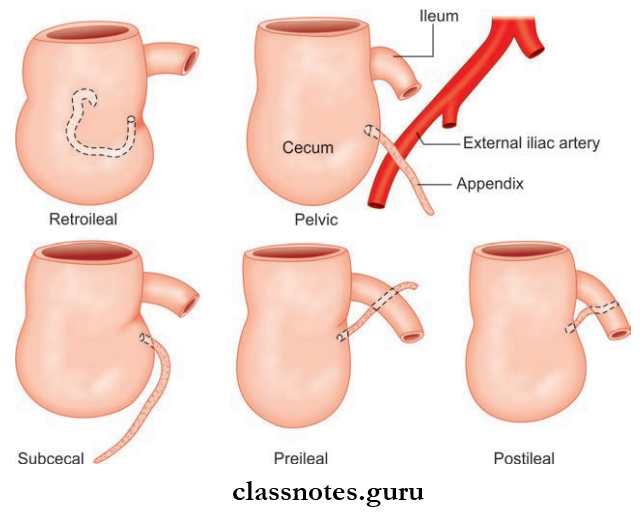
Positions Of Appendix
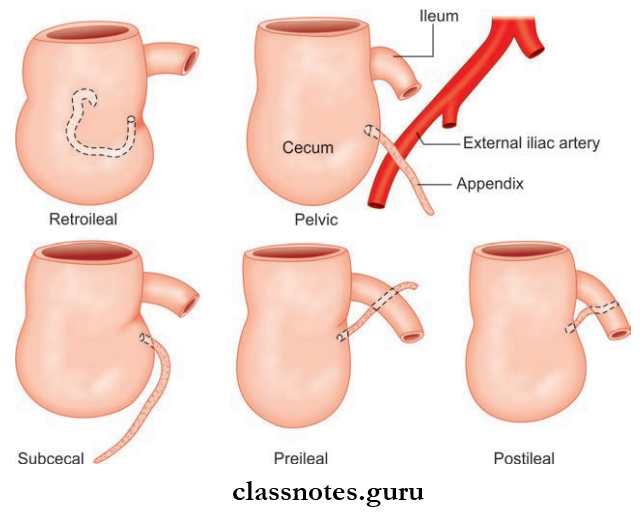
Vermiform Directions Or Positions Of Appendix
- Paracolic/11 ‘O’ Clock Position (2%)
- Appendix is directed upwards and to the right
- Retrocecal/12 ‘O’ Clock Position (65%)—Most Common
- Directed upwards
- Lies behind the cecum and ascending colon
- Splenic/2‘O’ Clock Position
- Directed upwards and to the left
- Pointed towards the spleen
- The Appendix May Be:
- Anterior To Ileum—preileal
- Posterior To Ileum—post-ileal
- Promonteric/3‘O’ Clock Position (<1%)
- Directed horizontally and to the left pointing to the sacral promontory
- Pelvic/4‘O’ Clock Position (30%)
- The appendix descend into the pelvis
- Midinguinal/6‘O’ clock Position
- Directed vertically downwards
- Pointed towards the inguinal ligament
- Lies behind cecum
Development Of Vermiform Appendix
Vermiform appendix develops from the distal part of the cecal bud arising from the caudal limb of the primitive intestinal loop.
Vermiform Applied Anatomy
- In preileal position—infection of the appendix can spread into general peritoneal cavity, so this position is considered as the most dangerous
- Peritoneal Relations
- Intraperitoneal
- It is suspended by mesoappendix/appendicular mesentery (small triangular fold of peritoneum)
- The appendicular artery runs through the mesoappendix
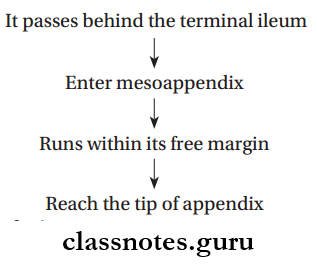
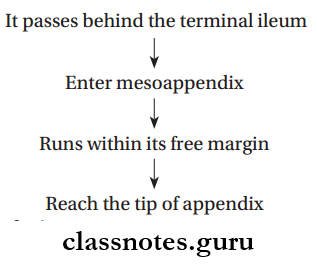
Vermiform Blood Supply
- Arterial supply
- By Appendicular Artery (end artery): Branch of the inferior division of ileocolic artery
Vermiform Course:
Vermiform Venous drainage: Veins accompany the arteries, drains into superior mesenteric vein, and from it to portal vein
Vermiform Lymphatic drainage
- Most lymphatics drain directly into ileocolic lymph nodes
- Few lymphatics drain indirectly through appendicular nodes (present in the mesoappendix) in to ileocolic lymph nodes.
Vermiform Nerve supply
- Sympathetic supply: From T10 spinal segments through lesser splanchnic nerve and superior mesenteric plexus
- Parasympathetic supply: From both vagus.
Vermiform Applied Anatomy
- Acute appendicitis: Acute inflammation of the appendix, commonly due to obstruction of its lumen, the pain is referred initially to the umbilical region (Because both are supplied by same spinal segment-T10)
- Mcburney’s point: It is the point of maximum tenderness during appendicitis.
- It is a point at the junction of the lateral 1/3rd and medial 2/3rd of the line joining anterosuperior iliac spine and umbilicus.
Question 11. Explain in detail about the divisions of the colon. Also, mention about the colic flexures.
Answer:
Ascending colon, transverse colon, descending colon, and sigmoid colon.
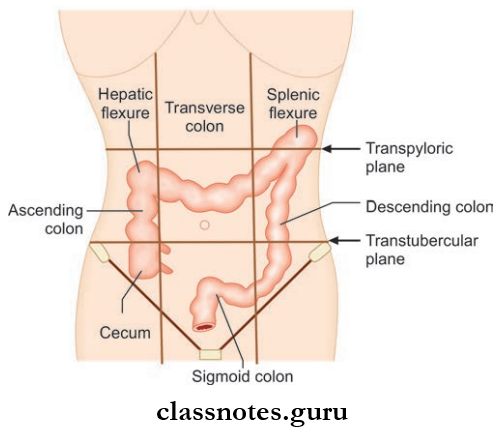
Ascending Colon
- Upward continuation of cecum
- Lies in right paracolic gutter
- Length: 2.5 cm
- Extent: Cecum to the inferior surface of right lobe of liver
- It is enclosed by peritoneum on 3 sides
- The posterior surface lies on 3 muscles:
- Transversus abdominis
- Quadratus lumborum
- Iliacus
Ascending Colon Relations
- Anteriorly
- Anterior abdominal
- Right edge of the greater omentum
- Coils of the small intestine
- Posteriorly
- Muscles: Transversus abdominis, quadratus lumborum, iliacus
- Kidney
- Nerves: Ilioinguinal, iliohypogastric, lateral cutaneous nerve.
Right Colic Flexure/Hepatic Flexure
- It lies at the junction of ascending colon and transverse colon in the right lumbar region
- Vertebral level: L2
- Here the distal end of ascending colon bends forwards, downwards and to the left forming the flexure.
Transverse Colon
- Largest and most mobile part of the large intestine
- Length: 50 cm
- Extent: From right colic flexure (in the right lumbar region) to left colic flexure (in the left hypochondrium)
- The transverse colon is not actually transverse, it hangs low as a loop in front of loops of small intestine suspended by transverse mesocolon
- This attains an ‘U’ shape (with limbs of unequal length)
- Lower most point of loop usually extends up to the umbilicus (sometimes it can extend in to the pelvis)
Transverse Colon Relations:
- Anteriorly: Greater omentum and anterior abdominal wall
- Posteriorly: Second part of the duodenum, head of the pancreas, coils of the small intestine.
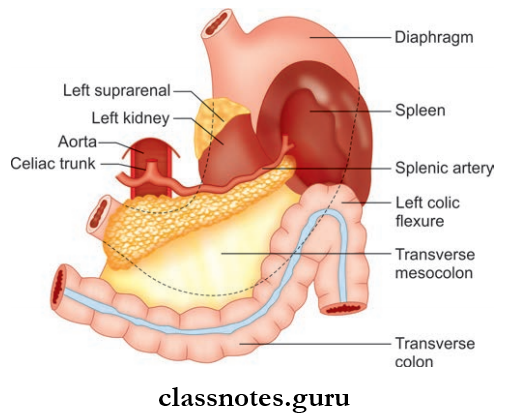
Left Colic Flexure/Splenic Flexure
- Lies at the junction of transverse colon and descending colon in the left hypochondrium
- Level: T12 vertebrae
- Here the distal end of the transverse colon bends downwards and backwards forming the flexure
- It is attached to the diaphragm by the phrenicocolic ligament.
Descending Colon
- Length – 25 cm
- Extent: From left colic flexure to sigmoid colon
- From the left colic flexure, the descending colon descends through the left lateral region, and the left inguinal region to reach the left side of the brim of the true pelvis
- Here it meets up with sigmoid colon
Descending Colon Relations:
- Anteriorly: Coils of small intestine
- Posteriorly
- Muscles: Transversus abdominis, quadratus lumborum, iliacus, and psoas
- Nerves: Ilioinguinal and iliohypogastric nerves, lateral cutaneous nerve, femoral nerve.
Sigmoid Colon
- Length: 37.5 cm
- S-shaped
- Extent: From lower end of descending colon to 3rd piece of sacrum
- The sigmoid colon forms a convoluted loop
- It is enclosed on all sides by the peritoneum
- It is attached to posterior abdominal wall by sigmoid colon.
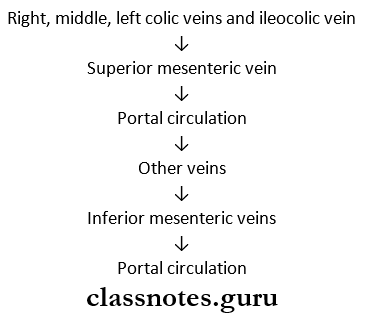
Blood Supply Of Colon
- Arterial Supply
- Right, middle, and left colic arteries
- Ileocolic artery
- Sigmoid artery
- Superior rectal artery.
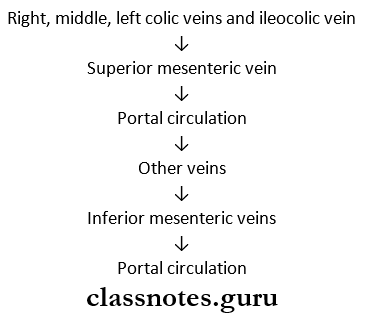
- Venous Drainage
- Lymphatic Drainage
- Paracolic nodes
- Intermediate colic nodes
- Epiploic nodes.
Intestines Exam Questions With Answers
Question 12. Write a note on Meckel’s diverticulum and what is the rule of 2.
Answer:
Meckel’s Diverticulum
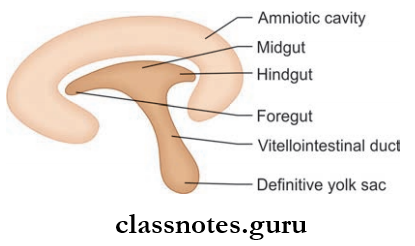
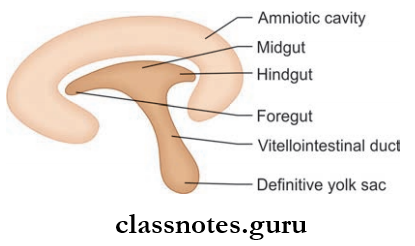
- Midgut communicates with the yolk sac at the embryological stage through the vitellointestinal duct
- Normally vitellointestinal duct involutes and disappears; occasionally the duct closes at the umbilical end but remain patent at the intestinal end
- Patent vitellointestinal duct gives rise to Meckel’s diverticulum
- This patent part appears as out pocketing of ileum
- Rule of 2: Occurs in 2% of subjects, 2 inches long and situated 2 ft. proximal to ileocecal valve, occurs most commonly in children under 2, and is symptomatic in 2% of patients.
Small And Large Intestines Multiple Choice Questions
Question 1. Most of the small intestine receives its blood supply from branches of the _____ artery:
- Middle colic
- Celiac
- Gastroduodenal
- Inferior mesenteric
- Superior mesenteric
Answer: 5. Superior mesenteric
Question 2. All the following are features of the large intestine except:
- Has leaf-like villi
- Absorbs salt and water
- Appendices epiploic
- The epithelium contains goblet cells in large numbers
- Presence of Brunner’s glands
Answer: 1. Has leaf-like villi And 5. Presence of Brunner’s glands
Question 3. Payer’s patches are seen in the:
- Ileum
- Duodenum
- Jejunum
- All of the above
Answer: 1. Ileum
Question 4. All of these supply the first 2 cm of duodenum, except:
- Left gastric artery
- Right gastric artery
- Supraduodenal artery
- Gastroduodenal artery
Answer: 1. Left gastric artery
Question 5. Which portion of the primordial gut differentiates into the portion of the duodenum proximal to the opening of the bile duct?
- Foregut
- Midgut
- Hindgut
- Biliary system
Answer: 1. Foregut
Question 6. Which is intraperitoneal?
- Pancreas
- 2nd and 3rd part of the duodenum
- Ascending colon
- Transverse colon
- Descending colon
Answer: 4. Transverse colon