Wound Sinus And Fistula Important Notes
Definitions
Wound: Wound is discontinuity or break in the surface epithelium
Healing: Replacement of destroyed tissue by living tissue
Regeneration: Replacement of lost tissue by tissue similar in type
Repair: Replacement of lost tissue by granulation tissue followed by fibrosis and scar tissue formation
Asepsis: Precautions taken before surgical procedure against the development of infection
Nosocomial Infection: Infection acquired from hospital
Sinus: Sinus is a blind tract leading from the surface down into the tissues
Fistula: Fistula is an abnormal communication between 2 epithelial surfaces commonly between a hollow viscus and skin or between 2 hollow viscera
Wound sinus and fistula questions and answers
- Causes Of Wound
- Trauma
- Physical, chemical, and microbial agent
- Ischaemia
- Types Of Wounds
- Open Wounds
- Incised wound
- Lacerated
- Penetrating wound
- Crushed wound
- Closed wounds
- Contusion
- Abrasion
- Haematoma
- Open Wounds
- Types Of Wound Healing
- Healing by the first Intention
- When a wound is sutured primarily, the wound healing occurs with minimum scaring
- This is known as healing by the first intention
- Healing by Second Intention
- When there is irreparable skin loss or the wound becomes infected, primary suturing is not possible
- In such cases, the wound heals with more scar tissue and takes longer time to heal
- This is known as healing by secondary intention
- Healing by the first Intention
- Process Of Wound Healing
- Inflammation
- Epithelisation
- Granulation tissue formation
- Scar remodeling
- Complications Of Wound Healing
- Implantation cyst
- Painful scar
- Cicatrization
- Keloid formation
- Neoplasia
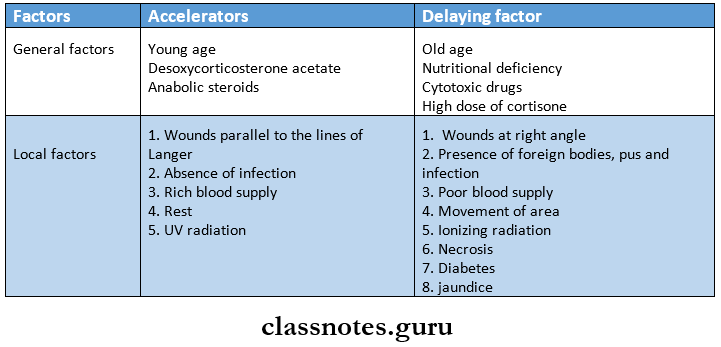
- Factors Affecting Wound Healing
- Types Of Sinus
- Congenital
- Preauricular
- Umbilical
- Acquired
- Pilonidal
- Osteomyelitis
- Actinomycosis
- Tuberculosis
- Congenital
Sinus and fistula Questions & Answers in surgery
Wound Sinus And Fistula Long Essays
Question 1. What is wound healing? What are the types? How do you manage compound fracture of the mandible?
Answer:
Wound Healing: Wound healing means replacement of lost tissues by living tissues
Read And Learn More: General Surgery Question and Answers
Wound Healing Types:
- Healing By The First Intention
- When a wound is sutured primarily, the wound healing occurs with minimum scarring
- This is known as healing by the first intention
- Healing By Secondary Intention
- When there is irreparable skin loss or the wound becomes infected, primary suturing is not possible
- In such cases, the wound heals with more scar tissue and takes a longer time to heal
- This is known as healing by secondary intention
Management Of Compound Fracture
- Immediate splinting and first aid are done
- Assessment of associated problems is done, like
- Shock
- Associated injuries
- Vessels and nerve involvement
- Type of fracture
- Resuscitation Is Carried Out By
- Blood transfusion
- Antibiotics
- 4 fluids
- Analgesics
- Wound debridement
- X-Ray Of The Fracture Part Is Taken
- The reduction of the part is done
- It means restoration of anatomical alignment
- It is done under general anesthesia with muscle relaxation
- A compound fracture requires open reduction
- It is carried out by screws, plates, and wires
- Immobilization
- Once reduced, it should be maintained by proper immobilization
- United fractured site is stiff due to immobilization
- Physiotherapy And Rehabilitation
- Stiffness is corrected by it
- A final x-ray is taken to confirm the proper union of fracture segments.
Wound healing, sinu, and fistula questions
Question 2. Describe types of wounds and their management.
Answer:
Wound:
- The wound is a discontinuity or break in the surface epithelium.
- It May Be Caused By.
- Trauma.
- Physical-chemical and microbial agents.
- Ischaemia.
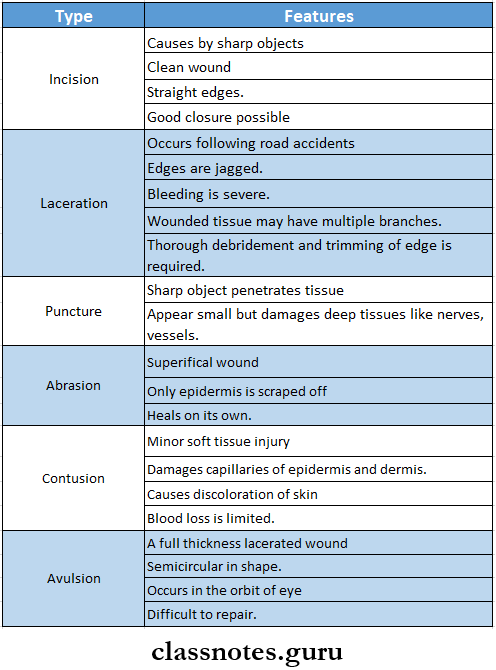
Types Of Wounds:
According To The Morphology.
- Open Wounds.
- Incised Wounds
- These are usually caused by a sharp knife or razor.
- They are relatively clean wounds.
- The wound can bleed a lot and quickly.
- Incised Wounds
- Open Wounds Management:
- Application of pressure to stop bleeding.
- Cleaning with septic solution.
- Closure by primary suturing.
- Repair of all damaged tendons, nerves, and major blood vessels within 6 hours of injury.
- Open Wounds Management:
- Lacerated Wounds
- It commonly occurs following road traffic accidents.
- Edges of wounds are jagged with certain lacerated and devitalized structures inside the wound.
- Bleeding may be severe.
- Injury may involve skin and subcutaneous tissue.
- Lacerated Wounds Management:
- Thorough debridement of the wound.
- Trimming of edges.
- Repair of tendons and nerves is delayed till complete healing of the wound occurs due to the risk of contamination.
- Lacerated Wounds
- Penetrating Wound
- Occurs due to a stab injury.
- Involves more depth than an incised wound.
- Example: stab injuries of the abdomen.
- Penetrating Wound Management:
- Observe the patient for at least 24 hours.
- Layer-by-layer exploration followed by primary suturing is done.
- Penetrating Wound
- Crushed Wounds
- Occurs due to industrial, road traffic, and wear injuries.
- They cause severe hemorrhage, death of the tissues, and crushing of blood vessels.
- Crushed Wounds Management:
- Good debridement.
- Removal of all necrotic and dead tissues.
- Late,r delayed primary suturing should be performed.
- Crushed Wounds
- Closed Wounds
- Closed Wounds Contusion
- Minor soft tissue injury without a break in the skin.
- It produces discoloration of the skin due to the collection of blood underneath.
- Closed Wounds Contusion
- Closed Wounds Management:
- Rest the injured site.
- Apply ice for 10-15 min for every 2 hours to close blood vessels.
- Compress and wrap firmly with a bandage.
- Abrasion
- In it, the epidermis of the skin is scraped off.
- Caused by a sliding fall onto a rough surface.
- Abrasion Management:
- Heal on their own within 1-2 weeks.
- Just needs cleaning of the area with a septic solution.
- Hematoma
- Hematoma refers to the collection of blood.
- Common in patients who have bleeding tendencies.
- Hematoma Management:
- Pressure is applied in the form of bondage to reduce hemorrhage and swelling.
- Closed Wounds Management:
Differences between sinus and fistula Questions & Answers
According To The thickness of the Wound:
- Superficial – involves epidermis and dermis upto dermal papillae.
- Partial Thickness – involves upto the lower dermis.
- Full Thickness – involves the skin and subcutaneous tissues.
- Deep Wounds – wounds penetrate an organ or tissue.
According To The Involvement Of Other Structures:
- Simple Wounds – comprise only one organ/tissue.
- Combined Wounds – mixed tissue trauma.
According To Time Elapsed:
- Fresh Wounds – upto 8 hours from trauma.
- Old Wounds – after 8 hours from trauma.
According To Bacterial Contamination Of Wound:
- Clean Wounds – made by the doctor during an operation or under sterile conditions.
- Clean-Contaminated wounds.
- Contaminated wounds.
- Dirty wounds.
Question 3. Discuss the pathology and healing of wounds.
Answer:
Pathology Of Wounds: Pathology Of Wound Healing Consists Of The Following Events:
1. Inflammation: Inflammation begins immediately at the time of injury and causes:
Aggregation of platelets.
↓
Initiation of coagulation cascade
↓
Formation of platelet plugs to stop bleeding.
↓
Transient vasoconstriction.
↓
Vasodilation.
↓
Release of histamine which produces local vasodilation and increases vascular permeability.
↓
Release of kinins, kalikerin enzyme, and prostaglandin.
↓
Chemotaxis.
↓
Initially, migration of polymorphonuclear leucocytes occurs followed by monocytes at the site.
↓
Phagocytosis occurs to ingest cell debris.
2. Wound Contraction:
- Wound contraction occurs 3-4 days after injury.
- The period when there is no wound contraction is called an initial lag period.
- After this period, there is a period of rapid contraction, which is completed by the 14th day.
- The wound is reduced to approximately 80% of its original size.
- The amount of contraction depends on the amount of skin available surrounding the wound to be stretched over the wound.
- It Occurs Due To
- Removal of fluid by drying.
- Contraction of collagen.
- Contraction of granulation tissue.
3. Epithelisation:
- The epidermis immediately adjacent to the wound edge thickens on the first day.
- Marginal basal cells lose their attachment to the underlying dermis and migrate into the wound.
- Basal cells proliferate, and the daughter cells formed migrate to the site.
- Within 48 hours, the entire wound surface is re-epithelialized.
4. Granulation Tissue Formation:
- Hematoma within the wound is replaced by granulation tissue consisting of new capillaries and fibroblasts.
5. Scar Remodeling:
- Scar Remodeling is the last stage of wound healing.
- On about the 7th day, wounds show a delicate fine reticulum of young collagen fibers to form a scar.
- Scar strength increases gradually.
- Maturation takes many months.
- As Time Proceeds, The Following Changes Occur.
- Change in bulk and form of scar.
- Anatomical arrangement.
- Fibers become thicker.
- Non-oriented fibers disappear.
- Fibers form 3-dimensional networks.
Healing Of Wound:
- Healing By The First Intention.
- When a wound is sutured primarily, wound healing occurs with minimum scarring.
- This is known as healing by first intention.
- It occurs in wounds in which the anatomical location and the size allow the skin continuity to be restored.
- Healing By The Second Intention.
- When there is irreparable skin loss or the wound becomes infected, primary suturing is not possible.
- In such cases, the wound heals with more scar tissue and takes a longer time to heal.
- This is known as healing by secondary intention.
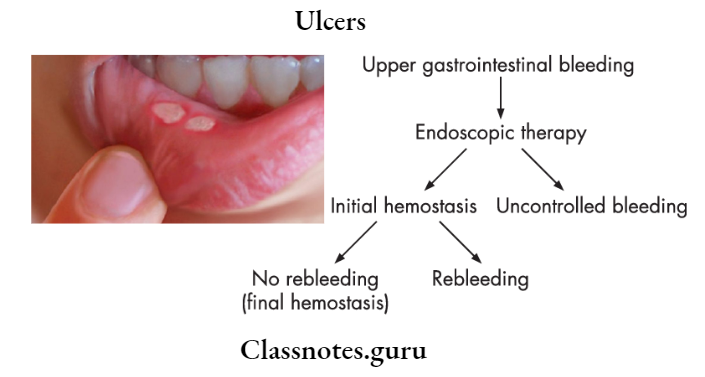
- Example: healing of abrasions, ulcers, etc.
Short and long answer questions on wound sinus fistula
Question 4. Discuss the stages of wound healing for closed and open wounds. What are the factors affecting wound healing?
Answer:
Stages Of Wound Healing: Whether it is closed or open wounds, the stages of healing remain the same.
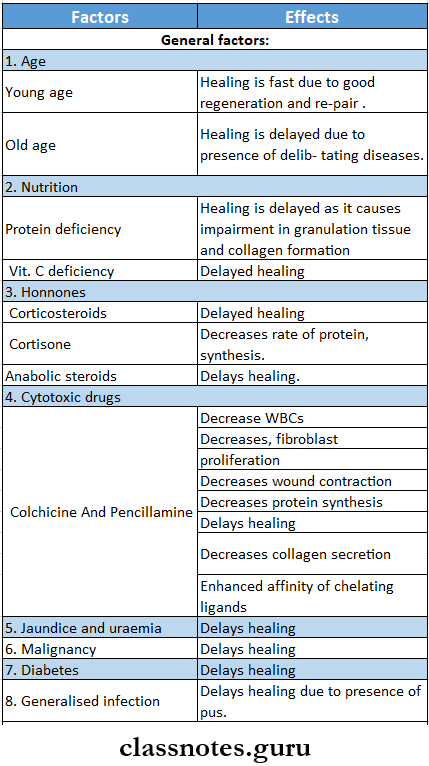
Factors Affecting Wound Healing:
- General Factors:
- Age: In young age, healing is faster, while in old age it is delayed due to the presence of debilitating diseases.
- Nutrition:
- Protein Deficiency: Protein Deficiency causes impairment of granulation tissue and collagen formation.
- Vitamin C Deficiency: Causes failure of collagen formation.
- Vitamin A Deficiency: Vitamin A is required for proper epithelialization.
- Zinc, copper, calcium, and manganese deficiency.
- Causes failure of granulation tissue formation.
- Hormones:
- Corticosteroids may delay wound healing because of their anti-inflammatory activity.
- Cortisone decreases the rate of protein synthesis and inhibits normal inflammatory reactions.
- Anabolic steroids like testosterone increase the speed of wound healing.
- Cytotoxic Drugs: Prevent or delay wound healing.
- Jaundice and Uraemic: Delay wound healing due to poor fibroblastic repair.
- Diabetes: Causes a delay in healing.
- Generalized Infection: The Presence of pus delays healing
- Malignancy, Anemia: Delays healing
- Local Factors:
- Position Of Skin Wound:
- When skin wounds are parallel to the lines of langer, they heal faster.
- If wounds are present at the right angle to these lines, healing is delayed.
- Blood Supply: Wounds with poor blood supply heal slowly.
- Tension: Tension at the wound while suturing delays healing.
- Infection: The presence of infection delays healing.
- Haemotoma: Precipitates infection and delays healing.
- Oxygen: Oxygen enhances the killing of pathogens by macrophage, increases the production of fibroblasts, and enhances healing
- Movement: Movement of the injured site delays healing.
- Radiation Exposure:
- Radiation affects vascularity.
- Causes delay in the formation of granulation tissue.
- Inhibits wound contraction.
- Wound healing is delayed.
- Ultraviolet Light: Increases the rate of healing.
- Other Factors Which Delay Healing Are:
- Faulty technique of wound closure.
- Presence of foreign bodies.
- Adhesion to bony surface.
- Necrosis.
- Impairment of lymphatic drainage.
- Position Of Skin Wound:
Question 5. Classify wound infections. Write briefly about hospital-acquired infections and their prevention.
Answer:
Hospital-Acquired/Nosocomial Infections:
- Nosocomial Infections is defined as an infection that results from treatment in a hospital or any health service unit.
- Infection can be from the patient’s organism or external sources.
Causative Organisms: They are classified as:
- Conventional Pathogens could cause disease in healthy persons in the absence of any immunity.
- Conditional Pathogens could cause disease only in persons with lower resistance.
- Opportunistic Pathogens that could cause generalized infections.
- Example: staphylococci, gram-negative organisms.
Wound Infections Types:
- Surgical wounds and other soft tissue are infectious through discharging wounds.
- Urinary tract infections – infected urine, feces.
- Respiratory tract infection – infected sputum.
- Gastroenteritis.
- Meningitis.
Wound Infections Prevention:
- Isolation.
- Proper ventilation of the ward.
- Cleaning of the hospital environment.
- Preventing transmission from the environment.
- Surface sanitation.
- Proper scrubbing and gloving before any procedure.
- Autoclaving, sterilisation of instrument.
- Safe injection practice.
- Proper disposal of wastes.
- Uses of disinfectant.
- Avoid unnecessary use of antibiotics to prevent the development of resistance.
Sinus and fistula MCQs with answers
Question 6. Discuss bleeding wounds on the face.
Answer:
Bleeding Wounds On The Face
Types of wounds sinus and fistula questions
Wound Sinus And Fistula Short Essays
Question 1. Discuss factors affecting wound healing.
Answer:
Factors Affecting Wound Healing

Question 2. Healing by primary Intention.
Answer:
Primary Intention Definition:
- When a wound is sutured primarily, wound healing occurs with minimum scarring.
- This is known as healing by primary or first intention.
Primary Intention Stages:
1. Initial Bleeding.
- The space between the surfaces of the incised wound is filled with blood.
- Disruption of blood vessels occurs.
- Results in formation of fibrin-rich haemal- toma.
2. Acute Inflammation.
- Following Changes Occur.
Vasoconstriction
↓
Increased capillary permeability
↓
Release of vasoactive substances
↓
Migration of polymorphs to the site
↓
Phagocytosis.
3. Organization: Minimum granulation tissue formation occurs
4. Proliferation: Basal cells present at the wound margin proliferate and migrate towards the space.
5. Remodeling: New matrix synthesis occurs.
Primary Intention Contraindications:
- An acute wound of more than 6 hours old.
- Presence of foreign bodies.
- Active oozing of blood from the wound.
- Dead space under the skin closure.
- Too much tension is present while suturing.
Surgical management of sinus and fistula Questions & Answers
Question 3. Healing by secondary intention.
Answer:
Secondary Intention Definition:
- When there is irreparable skin loss, primary suturing is not possible.
- So the wound heals with more scar tissue and takes a longer time to heal.
- This is known as healing by secondary intention.
Secondary Intention Stages:
- Initial Inflammation.
- Inflammation is prolonged due to the presence of more necrotic tissues and bacteria.
- It affects surrounding tissues.
- The wound is filled with coagulum.
- Wound Contraction.
- Occurs due to stretching of the surrounding skin to close the defect.
- After 2-3 days, dermal edges move towards each other.
- After 5-10 days, it moves rapidly while after 2 weeks it slows down.
- Granulation Tissue Formation.
- Granulation tissue completely covers the exposed wound gradually.
- Granulation Tissue Formation forms a temporary protective layer till epi-realization begins.
- Epithelialisation.
- Epithelium gradually grows over granulation tissue.
- Epithelial cells slide into the wound forming a thin tongue of cells between granulation tissue and clot.
- Remodeling.
- Remodeling is prolonged.
- Remodeling of granulation tissue and scar occurs.
- As a result, the wound area forms a flat scar.
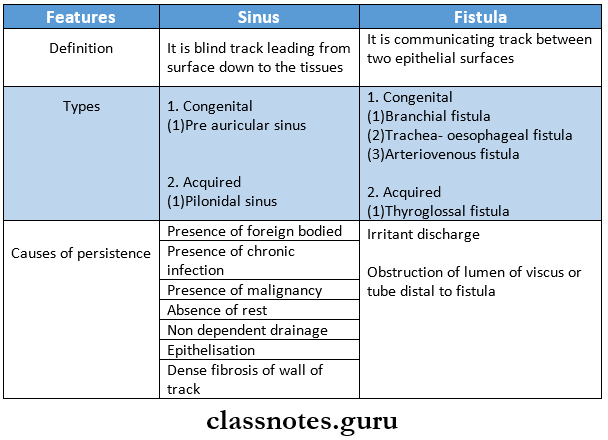
Question 4. What is sinus and fistula? What are its causes?
Answer:
Sinus and fistula
- A sinus is a blind track leading from the surface down to the tissues.
- There may be a cavity in the tissues that is connected to the surface through the sinus.
- The sinus is lined by granulation tissue.
Fistula:
- A fistula is a communicating track between two epithelial surfaces, commonly between a hollow viscus and the skin.
- The fistulais lined by granulation tissue.
- Fistula may be abnormal communication between vessels.
Fistula Types:
- Blind – with only one open end.
- Complete – with both external and internal openings.
- Incomplete, with an external skin opening which does not connect to any internal organ.
Fistula Causes:
- Congenital – preduricular sinus, branchial fistula, trachea-oesophageal fistula, arteriovenous fistula.
- Acquired.
- Bursting of sinus-example: fistula-in-ano.
- Trauma or medical treatment.
- Due to tooth abscess – median mental sinus.
- The pilonidal sinus and thyroglossal fistula are examples of the acquired type.
Question 5. Difference between sinus and fistula.
Answer:
Difference Between Sinus And Fistula
Wound care and fistula treatment questions
Wound Sinus And Fistula Short Answers
Question 1. Types of wounds.
Answer:
According To The Morphology:
- Open Wounds.
- Incised wounds
- Lacerated wounds
- Penetrating wounds
- Crushed wounds
- Closed Wounds
- Contusion
- Abrasion
- Hematoma.
According To The Thickness Of The Wound:
- Superficial
- Partial thickness
- Full-thickness.
- Deep wounds.
According To The Involvement Of Other Structures.
- Simple wound
- Combined wounds
According To The Time Elapsed:
- Fresh wounds
- Old wounds.
According To The Bacterial Contamination:
- Clean wounds
- Clean contaminated wounds
- Contaminated wounds
- Dirty wounds.
Question 2. Healing by primary intention.
Answer:
Healing Primary Intention Stages:
- Initial bleeding
- Acute inflammation
- Organization
- Proliferation
- Remodeling
Clinical features of fistula and sinus questions
Question 3. Healing by secondary intention.
Answer:
Secondary Intention Stages:
- Initial inflammation
- Wound contraction
- Granulation tissue formation
- Epithelisation
- Remodeling.
Question 4. Enumerate three factors influencing wound healing.
Answer:
Factors Influencing Wound Healing
Healing of wounds sinus and fistula notes
Question 5. Causes of persistence of sinus and fistula.
Answer:
Causes Of Persistence Of Sinus And Fistula
- Causes of persistence of sinus and Fistula:
- Presence of foreign body or necrotic tissue
- Absence of rest.
- Non-dependant or inadequate drainage of the abscess.
- Presence of chronic infections like tuberculosis, actinomycosis, etc.
- Epithelialization of the track.
- Distal obstruction of the track.
- Malignancy.
- Irradiation.
- Dense fibrosis around the wall of the track.
Question 6. Hypertrophic scar.
Answer:
Hypertrophic Scar
- A hypertrophic scar is characterized by hypertrophy or proliferation of mature fibroblasts or fibrous tissues without any proliferation of blood vessels.
- Hypertrophic Scar remains localized and gradually regresses.
Hypertrophic Scar Features:
- Hypertrophic Scar never gets worse.
- Hypertrophic Scar is non-tender.
- Doesn’t spread to surrounding normal tissue.
- Once treated it does not recur.
- Hypertrophic Scar regresses after 6 months.
- Common in.
- Young individual
- The scar crossing normal skin creases
- Over sternum.
Hypertrophic Scar Treatment:
- Regress on its own.
- If necessary excision can be done.
Question 7. Keloid scar.
Answer:
Keloid Scar
Keloid scar is characterized by the proliferation of immature fibroblasts and immature blood vessels.
Keloid Scar Features: Commonly in:
- Black race
- Tuberculosis patients
- Over sternum.
- In women.
Keloid Scar Etiology
- Tuberculosis.
- Hereditary.
- Dislocation of hair follicles.
- Incision crossing lines of Langer.
Keloid Scar Presentation
- Has claw-like processes.
- Keloid Scar always itch.
- Looks smooth, and pink, and raised patch.
- Gets worse even after 1 year.
- Recurs after excision.
- The margin is tender, and vascular.
- Spreads and affects normal surrounding tissue
Keloid Scar Treatment:
- Conservative treatment:
- Intrakeloidal injection of steroids.
- Intrakeloidal hyaluronidase injection.
- Intrakeloidal injection of Vitamin A.
- Intrakeloidal injection of methotrexate.
- Deep. X-ray therapy.
- Ultrasonic therapy.
- Surgical treatment.
- Excision and resuturing
- Shaving away the excess scar tissues and then resurfacing the area with a skin graft.
Pathophysiology of sinus and fistula
Question 8. Lacerated wound
Answer:
Lacerated Wound Causes:
- Injury by blunt objects
- Fall on a stone
- Road traffic accidents
Lacerated Wound Features
- Involves skin and subcutaneous tissue
- Crushing of tissues
- Edges are jagged
- Results in
- Necrosis of tissues
- Bruising
- Hematoma
Lacerated Wound Treatment
- Wound excision and primary suturing
Question 9. Pre auricular sinus
Answer:
Pre Auricular Sinus
- May be unilateral or bilateral
- Usually asymptomatic
- If infected it causes pain
Pre Auricular Treatment
- Uninfected sinus can be left untreated
- Infected pro-auricular sinus is treated as
- Antibiotics
- Drainage
- Excision
Question 10. Types of healing
Answer:
Types Of Healing
- Healing By Primary Intention
- When a wound is sutured primarily, the wound healing occurs with minimum scarring
- This is known as healing by primary intention
- Healing By Secondary Intention
- When there is irreparable skin loss or the wound becomes infected primary suturing is not possible
- In such cases, the wound heals with more scar tissue and takes longer time to heal
- This is known as healing by secondary intention
Management of non-healing wounds and fistulas
Question 11. Abscess
Answer:
Abscess Definition: Abscess is a collection of pus in the body
Abscess Classification
- Pyogenic
- Pyaemic
- Cold abscess
Abscess Clinical Features
- Rubor – redness over the area
- Dolor – throbbing pain
- Color – the inflamed area is hot
- Tumor – swelling of the involved area
- Functlolacsa – Impairment of function
Abscess Treatment
- Incision and drainage of pus
Difference between abscess sinus and fistula
Question 12. Orocutaneous fistula
Answer:
Orocutaneous Fistula
- Orocutaneous Fistula is pathological communication between the cutaneous surface of the face and the oral cavity
- Orocutaneous Fistula leads to esthetic and functional problems due to continuous leakage of saliva
Orocutaneous Fistula Causes
- Malignancy
- Osteoradionecrosis
- Residual lesions of cysts and tumors of the oral cavity
- Inflammation
- Trauma
Causes and complications of sinus and fistula
Wound Sinus And Fistula Viva Voce
- The pilonidal sinus is usually found in the natal cleft
- Granulation tissue formation occurs by 2 processes – stage of vascularization and stage of vascular- citation
- Type 1 collagen is found in tendons, ligaments, skin, and bone
- Type 2 collagen is in cartilage
- Type 3 collagen is found in the fetal dermis
- The period when no wound contraction is seen is called the initial lag period
- Within 48 hours of the wound, the entire wound gets re-epithelioid
- Wound contraction occurs from the 4th day to the 14thday
- In the first 48 hours, polymorphonuclear leukocytes are dominant
- Monocytes become the dominant cell type by the 5th day.
