Tumours Of Salivary Glands Long Essays
Question 1. Classify salivary gland tumors. Write about histogenesis and clinical features of pleomorphic adenoma
(or)
Enumerate benign tumors of salivary glands. Describe clinical and histopathological features of pleomorphic adenoma
Answer:
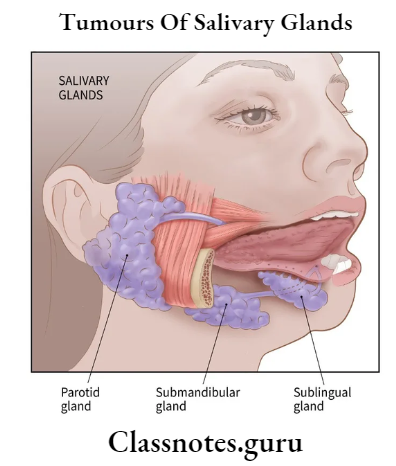
Salivary Gland Tumors Classification:
- Based On The Spread Of Tumors
- Benign tumors
- Pleomorphic adenoma
- Cystadenoma
- Myoepithelioma
- Canalicular adenoma
- Oxyphilic adenoma
- Malignant tumors
- Malignant pleomorphic adenoma
- Mucoepidermoid carcinoma
- Adenoid cystic carcinoma
- Acinar cell adenocarcinoma
- Epidermoid carcinoma
- Benign tumors
- Histological Classification
- Adenoma
- Pleomorphic adenoma
- Myoepithelioma
- Basal cell adenoma
- Warthin’s tumour
- Canalicular adenoma
- Cystadenoma
- Carcinoma
- Acinic cell carcinoma
- Mucoepidermoid carcinoma
- Adenoid cystic carcinoma
- Adenocarcinoma
- Squamous cell carcinoma
- Nonepithelial tumours
- Malignant lymphomas
- Secondary tumours
- Unclassified tumours
- Tumor like lesions
- Sialoadenesis
- Oncocytosis
- Necrotizing sialometaplasia
- Salivary gland cyst
- Adenoma
Pleomorphic Adenoma: It is a benign mixed tumor of the salivary gland
Pleomorphic Adenoma Clinical Features:
- An age-5th-6th decade of life
- Sex- common in females
- Site- common in parotid gland
- Appears as slow growing, exophytic, solitary lesion
- Swelling of gland
- The smooth surface of the lesion
- Painless lesion
- Superficial lesion- located near the angle of the mandible
- Deeper lesions- present over the lateral wall of the oropharynx
- Minor gland neoplasm exhibits a firm and nodular swelling
- Palatal lesions cause surface ulceration
- In buccal mucosa presents as a small, planless nodular lesion
Pleomorphic Adenoma Histopathological Features:
- It has a pleomorphic nature of epithelial and mesenchymal tissue
- Epithelial Component
- Proliferation of glandular, basophilic epithelial cells in the form of diffuse sheets or clusters
- Such cells are polygonal, spindle, or stellate-shaped
- They form duct-like structure
- Arranged in clumps or interlacing strands
- Each duct-like structure exhibits an inner row of cuboidal or columnar cells and an outer row of spindle-shaped myoepithelial cells
- The center of it contains clear eosinophilic material
- Myoepithelial cells are cuboidal, flattened, or spindle-shaped surrounded by connective tissue stroma
- Epithelial cells proliferate around the salivary gland duct
- They exhibit squamous metaplasia
- Connective Tissue Wtroma
- Exhibits metaplastic changes
- Presence of hyaline, elastic, or myxochon-droid elements
- Consist of a delicate network of collagen bundles
- The fibrous area consists of dense collagen bundles
- In myxoid areas- strands of epithelial cells are surrounded by mucoid material
- The fibro myxoid area contains abundant elastic tissues
- The chondroid area consists of isolated, rounded epithelial cells lying within lacunae within mucoid material
- Mucoid material is composed of glycosaminoglycans and chondroitin sulfate
- Epithelial Component
Read And Learn More: Oral Pathology Questions and Answers
Question 2. Discuss in detail mucoepidermoid carcinoma
Answer:
Mucoepidermoid Carcinoma: It is a malignant tumor of the salivary gland
Mucoepidermoid Carcinoma Clinical features:
- Age 30-50 years of age
- Sex- common in females
- Site Involved
- Parotid gland
- Minor salivary glands of palate, lips, buccal mucosa, tongue, and retromolar area
- Characterized by slow-growing, painless swelling
- Hemorrhage, ulceration, and paraesthesia may occur
- Jaw involvement causes bony expansion
- Parotid lesions are present as a well-defined, focal, movable nodular swelling
- Size- varies between 1-4 cm in diameter
- Facial nerve paralysis
- Low-grade tumors are fluctuant, non-ulcerated with a slight bluish color of growth
- High-grade tumors are firm
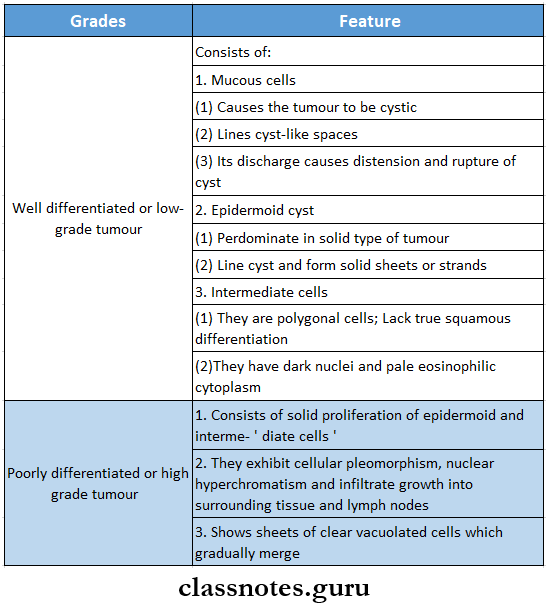
Mucoepidermoid Carcinoma Histopathology:
- Mucoepidermoid carcinoma consists of three types of cells
- Large pale mucous-secreting cells
- Epidermoid cells
- Intermediate type of cells
- According to the distribution of cells, the tumor is divided into 2 grades
Mucoepidermoid Carcinoma Treatment:
- Surgical excision
- Radiotherapy
Question 3. Discuss in detail adenoid cystic carcinoma
Answer:
Adenoid Cystic Carcinoma: It is a malignant neoplasm arising from the glandular epithelium of the salivary gland
Adenoid Cystic Carcinoma Clinical Features:
- Age-50-70 years of age
- Sex- common in females
- Site Involved
- Commonly in the submandibular gland
- Minor glands over the tongue and palate
- Characterized by slow enlarging growth with surface ulceration
- Parotid tumours are asymptomatic
- They are located surrounding the nerve trunk
- Anesthesia, paraesthesia, or palsy
- Fixation and induration of tumor to underlying structures
- Submandibular tumors are large
- Palatal lesions cause toothache, loosening of teeth, and delayed healing of socket
Adenoid Cystic Carcinoma Histopathology:
- Characterized by the presence of numerous small, polygonal, or cuboidal cells
- They have hyperchromatic nuclei and minimum mitotic activity
- Double layer of tumor cells are arranged in a duct-like pattern
- Gives Swiss cheese appearance
- Connective tissue stroma surrounds the tumour cells forming cylinders
- Tumour cells spread through perineural or intraneural spaces
Adenoid Cystic Carcinoma Subtypes:
- Cribiform Pattern
- Consist of small, uniform, polygonal cells with basophilic cytoplasm
- These cells are penetrated by numerous cylindrical spaces
- Solid Pattern
- Tumor cells proliferate to form solid masses with central necrosis
- Tubular pattern
- Tumor cells proliferate as small tubular units with a single central lumen
Adenoid Cystic Carcinoma Treatment: Surgical excision
Question 4. Discuss in detail about clinical features and histological features of Sjogren’s syndrome
Answer:
Sjogren’s Syndrome:
- Sjogren’s Syndrome is a chronic autoimmune disease
- Characterized by oral and ocular dryness, exocrine dysfunction, and lymphocytic infiltration
Sjogren’s Syndrome Clinical Features:
- Decreased salivary function
- Dry mouth
- Difficulty in chewing, swallowing, and speech
- Increased risk of caries
- Altered taste
- Dry cracked lips
- Angular cheilitis
- Mucosa reveals fissuring and lobulation on the surface resulting in the cobble-stone appearance
- Mucosa appears red, dry, tender, and smooth
- It is called the parchment-like appearance of the mucosa
- Minimal salivary pooling
- The tooth is smooth and painful
- Erosion of enamel
- Susceptible to infection
- Increased risk of developing malignant lymphoma
- Difficulty in wearing dentures
- Diffuse, firm, painless enlargement of major salivary glands
- High risk of bacterial sialadenitis
- Keratoconjunctivitis
- Burning sensation in the eye
- Blurred vision and itching sensation in the eye
Sjogren’s Syndrome Histopathological Features:
- Infiltration of lymphocytes in the intralobular ducts of involved salivary gland replacing entire lobule
- Atrophy of salivary gland acini and proliferation of ductal epithelial cells
- Ductal epithelial hyperplasia obliterates the ductal lumen
- Formation of discrete islands of epithelial tissue called myoepithelial islands
Question 5. Write about clinical features and histopathology of Warthin’stumour.
Answer:
Warthin’stumour Clinical features
- Age: 50-70 years
- Sex: common in males
- Site: common in the parotid gland especially in the lower part overlying angle of the mandible
- Characterized by slow enlarging, well-circumscribed soft, painless swelling of the gland
- Well-capsulated and movable
- Present over angle of mandible
- Size – 2-4 cm in diameter
- Shape- spherical
- Occurs bilaterally
- Produces compressible and doughy feeling on palpation
Warthin’stumour Histopathology Presence of multiple cystic spaces
Warthin’stumour Cells:
- Columnar Cells
- Pseudostratified tall columnar cells line the cystic spaces
- Epithelial Cells
- Arranged in a double layer
- Nuclei are arranged in basilar row of the bottom row and superior aspect of the upper row
- They cover papillary folds
- Goblet Cells
- Goblet Cells are interspersed within neoplastic pseudostratified epithelial cells
Tumours Of Salivary Glands Short Essays
Question 1. Mumps
Answer:
Mumps
- Mumps is an acute viral infection caused by RNA paramyxovirus
- Mumps is transmitted by direct contact with salivary droplets
Mumps Clinical Features:
- Age- 4-6 years
- Incubation period- 2-3 weeks
- Characterized by salivary gland inflammation and enlargement
- Preauricular pain
- Fever, malaise
- Headache
- Myalgia
- Edema of the surrounding skin
- Ducts become inflamed without purulent discharge
- Swelling is usually bilateral and lasts for approx. 7 days
Mumps Complications:
- Meningitis and encephalitis
- Deafness
- Myocarditis
- Thyroiditis
- Pancreatitis
- Ophoritis
- Epididymitis, orchitis, testicular atrophy
Mumps Treatment: Symptomatic treatment is done
Mumps Prevention: By MMR vaccination
Question 2. Mucocele
Answer:
Mucocele
Mucocele is a swelling caused by the accumulation of saliva at the site of a traumatized or obstructed minor salivary gland duct
Mucocele Types:
- Extravasation Type
- It is formed as a result of trauma to a minor salivary gland excretory duct
- It is more common
- It does not have an epithelial cyst wall
- Retention Type
- Caused by obstruction by the calculus of duct
Mucocele Clinical Features:
- Site Involved
- Extravasation Type
- Lower lip
- Buccal mucosa
- Tongue
- Floor of mouth
- Retromolar area
- Retention Type
- Palate
- The floor of the mouth
- Extravasation Type
- Appears as discrete, painless, smooth surface swelling
- Size- varies from a few millimeters to a few centimeters
- Color
- Superficial lesios- bluish in color
- Deep lesion- Covered by normal mucosa
Mucocele Treatment:
- Surgical excision
- Aspiration of fluid
- Intralesional injection of corticosteroids
Question 3. Mikulicz’s disease
Answer:
Mikulicz’s Disease
Mikulicz’s disease is a progressive autoimmune disease of the salivary gland characterized by the replacement of gland acini by a dense infiltrate of T lymphocytes
Mikulicz’s Disease Etiology:
- Genetic abnormality
- Defective cell-mediated immunity
Mikulicz’s Disease Clinical Features:
- Age- middle-aged or elderly adults
- Sex- common in males
- Site involved
- Parotid gland
- Submandibular gland
- Lacrimal gland
- There is unilateral or bilateral diffuse swelling of the involved gland
- Swelling is soft, movable, and painless
- Size- a few centimeters in diameter
- Associated with xerostomia
- Fever
- Upper respiratory tract infection
- Oral or orofacial infection
Mikulicz’s Disease Histopathological Features:
- Replacement of salivary gland acini by benign infiltration of lymphocytes and squamous metaplasia of ductal epithelium
- The presence of several myoepithelial islands persisting in salivary gland ducts
- Proliferating epithelial cells obliterate the lumen of ducts
- Presence of eosinophilic hyaline material
Mikulicz’s disease Treatment: 20-30 mg of prednisolone to control the disease
Question 4. Necrotizing sialometaplasia
Answer:
Necrotizing Sialometaplasia
- Necrotizing sialometaplasia is a benign, self-limiting reactive inflammatory disorder of salivary tissue
- It is characterized by necrosis of minor salivary glands of the palate along with the surface epithelium and underlying connective tissue
Necrotizing Sialometaplasia Etiology:
- Idiopathic
- Local ischaemia
- Infection
- Immune response to unknown antigen
Necrotizing Sialometaplasia Clinical Features:
- Site involved
- Palate
- Lips
- Retromolar region
- Initially, the lesion occurs as a tender erythematous nodule
- Later mucosa breaks and deep ulceration with a yellowish base is formed
- Lesions can be large and deep
- It has rolled borders
- The surface consists of granular lobules
- Patient complaints of a burning sensation
- The lesion can occur shortly after oral surgical procedure, restorative dentistry, or administration of LA
Necrotizing Sialometaplasia Treatment:
- Self-limiting condition
- Healing by secondary intention occurs in approx. 6 weeks
- Debridement and saline rinses
Question 5. Sialolithiasis
Answer:
Sialolithiasis
Sialoliths are calcified organic matter that forms within the secretory system of the major salivary glands
Sialolithiasis Etiology:
- Sialolithiasis is unknown
- Several factors like:
- Inflammation,
- Irregularities in the duct system
- Local irritants and anti-cholinergic medication
- May contribute to stone formation
Sialolithiasis Composition:
- Hydroxyapatite
- Calcium phosphate and carbon
- A trace amount of magnesium, potassium chloride, and ammonium
Sialolithiasis Occurrence:
- Submandibular gland (80-90%): Because
- The torturous course of Wharton’s duct
- Higher calcium and phosphate level
- Position of gland
- Parotid (5-15%)
- Sublingual (2-5%)
Sialolithiasis Clinical presentation:
- Acute, painful, and intermittent swelling
- Eating initiates salivary gland swelling
- Stone totally or partially blocks the flow of saliva, causing salivary pooling within the ductal system
- There is little space for expansion, so enlargement causes pain
- Stasis of saliva may lead to infection, fibrosis, and gland atrophy
- Fistula, sinus tract, or ulceration may occur over the stone in chronic cases
- The soft tissue surrounding the duct may show edema and inflammation
Sialolithiasis Complications:
- Separative or non-sup purified retrograde bacterial infection can occur
- Acute sialadenitis
- Ductal stricture
- Ductal dilatation
Sialolithiasis Diagnosis:
- Occlusal radiograph for submandibular gland
- AP view of face for parotid
- CT images have 10 folds with greater sensitivity for detecting calcification
- FXAC is used when differential diagnosis includes: cyst or humor
- Sialoendoscopy:
- It is a relatively new technique
- A small probe(<l mm diameter) attached to a specially designed endoscopic unit can explore the primary and secondary ductal system
- The unit has a surgical tip to obtain soft tissue biopsy and help to remove calcified material
Differential Diagnosis of Sialolithiasis:
- Gas Bubbles:
- Introduced during sialography
- Avoid Bone:
- Seen bilaterally on panoramic film
- Myositis Ossificans:
- Restriction of mandibular movements occurs
Sialolithiasis Treatment:
- Acute Phase:
- Supportive treatment includes analgesics, antibiotics, hydration, and antipyretic
- In Exacerbation:
- Surgical intervention – drainage or removal of stone
- Stones at or near the duct are removed transorally by milking the gland
- Deeper stones are removed by surgery or Sia- endoscopy
- Smaller stones are removed by gently massaging the gland
- Sialogogues, moist heat, and increased fluid intake may also promote the passage of stone
- Large sialoliths are surgically removed
- Ultrasonography – it will detect stones of diameter >2 mm
- Lithotripsy – it will fragment the stone
Question 6. Xerostomia
Answer:
Xerostomia refers to a subjective sensation of a dry mouth, but is not always, associated with salivary hypofunction
Xerostomia Etiology:
- Developmental:
- Salivary gland aplasia
- Water/ metabolic Loss:
- Impaired fluid intake
- Hemorrhage
- Vomiting/diarrhea
- Latrogenic:
- Medications:
- Antihistamines: diphenhydramine
- Decongestants: pseudoephedrine
- Antidepressants: amitriptyline
- Antipsychotic: haloperidol
- Antihypertensive: methyldopa, CCB
- Anticholinergic: atropine
- Radiation Therapy Of The Head And Neck:
- Both stimulated and unstimulated salivary flow decreases with increasing radiotherapy.
- Systemic Diseases:
- Sjogren’s syndrome
- Diabetes mellitus
- Diabetes insipidus
- HIV infections
- Psychological disorders
- Graft-versus-host disease
- Local Factors:
- Decreased mastication
- Smoking
- Mouth breathing
- Local Factors Clinical Features:
- Reduction in salivary secretion
- Residual saliva is either foamy or thick
- Mucosa appears dry
- The dorsal tongue is fissured with atrophy of filiform papilla
- Difficulty in mastication and swallowing
- Food adheres to the oral membranes while eating
- Some patients who complaints of dry mouth may appear to have adequate salivary flow
- The degree of saliva production can be assessed by measuring resting and stimulated saliva
- Increased prevalence of candidiasis because of reduction in cleansing and antimicrobial activity
- More prone to dental decay, especially cervical and root caries
- Local Factors Treatment:
- Artificial saliva may help the patient
- Sugarless candy can stimulate salivary flow
- Use of oral hygiene products like Biotene toothpaste, oral balance gel
- If dryness is secondary to medications, discontinue it or reduce its dose
- Systemic pilocarpine is used:
- It is a parasympathomimetic agonist
- Doses: 5-10 mg, 3-4 times a day
- ADR: excessive sweating,
- Increased heart rate and BP
- Cevimeline hydrochloride
- Acetylcholine derivative
- Approved by the U.S. Food and Drug Administration
- Both these drugs are contraindicated in narrow-angle glaucoma
- To prevent dental decay, office, and daily home fluoride application
- Chlorhexidine mouthwash minimizes plaque built-up
- Local stimulation of saliva
- Chewing gums, mints, paraffin, and citric acid
Question 7. Sialolith
Answer:
Sialolith
- Sialolith is a calcified stone found in the salivary duct
- Obstructs duct
Sialolith Composition:
- Calcium phosphate
- Calcium carbonate
- Salts of Mg, Zn, etc
- Glycoproteins
- Mucopolysaccharides
- Cellular debris
Question 8. Ranula
Answer:
Ranula
- Ranula is special type of mucocele
- It resembles the belly of a frog
Ranula Site:
- The floor of the mouth
- Superficial or deep to mylohyoid muscle
Ranula Cause: Trauma to duct
Ranula Features:
- Slow-growing unilateral lesion
- It is a soft and freely movable lesion
- Superficial lesion
- It is a thin-walled bluish lesion
- Deeper lesions
- Well circumscribed
- Covered by normal mucosa
Ranula Types:
- Simple type
- Plunging ranula
Ranula Treatment: Marsupialisation
Question 9. Sialography
Answer:
Sialography
Sialography is used for the investigation of sialolith
Sialography Procedure:
- Identification of duct
- Exploring duct
- Introduction of cannula
- Introducing starting media lipid or water-soluble agents
- Radiograph is taken
Question 10. Salivary Analysis
Answer:
Salivary Analysis
- Salivary analysis is a new diagnostic tool used in oral cancers
- Salivary Analysis evaluates, biochemical and immunological parameters in the saliva of oral squamous cell carcinoma patients
- Salivary parameters include
- Sodium
- Calcium
- Inorganic phosphate
- Magnesium
- Total protein
- Albumin
- Lactate dehydrogenase
- Amylase
- Total immunoglobulin G
- Secretory immunoglobulin A
- Epidermal growth factor
- Insulin growth factor I
- Metalloproteinases
Question 11. Autoimmune sialosis
Answer:
Autoimmune Sialosis
- Autoimmune Sialosis Is a rare chronic Inflammatory disease of the submandibular mill very gland
- Autoimmune Sialosis Is characterized by an enlarged, firm, and painful unilateral or bilateral salivary gland
Autoimmune Sialosis Treatment:
- Elimination of causative agent
- Surgical excision
Tumours Of Salivary Glands Viva Voce
- Myoepithelial cells are a major component of pleomorphic adenoma
- Swiss cheese or honeycomb pattern of cells is seen in adenoid cystic carcinoma
- Sialolith is common in submandibular salivary gland
- Sialolith are composed of calcium and phosphorous
- Mumps is caused by RNA paramyxovirus
- Mikulicz disease is the abnormal enlargement of salivary glands and lacrimal glands
