Acute Inflammation Important Notes
1. Vascular events
- Hemodynamic changes
- Transient vasoconstriction
- Persistent progressive vasodilatation
- Elevation of local hydrostatic pressure
- Slowing or stasis of microcirculation
- Leucocyticmargination and emigration
- Changes in vascular permeability
2. Vasoactive amines
- They mediate inflammation
- They are histamine and serotonin
- Histamine
- It is released from mast cells, basophils, and platelets
- The actions are
- Vasodilation
- Increased vascular permeability
- Itching
- Pain
- Serotonin
- It is present in chromaffin cells of GIT, spleen, nervous tissue cells, and platelets
- Actions are similar to histamine but less potent
3. Interleukin – 1 (IL-1)
- It is secreted by monocytes and macrophages
- It is also known as leucocyte leucocyte-activating factor
- Together with the tumor necrosis factor it
- Increases chemotaxis
- Phagocytic activity of leukocytes
- Increases resorption of bone
4. Metabolites
- Metabolites of arachidonic acid
- Prostaglandins, thromboxane A2, prostacyclin
- Prostaglandin increases vascular permeability, vasodilation, and bronchodilation
- Metabolites of lipo-oxygenase pathway
- 5-HETE and leukotrienes
5. Bradykinin
- It acts in the early stages of inflammation
- Actions:
- Induces smooth muscle contraction
- Vasodilation
- Increased vascular permeability
- Pain
6. Macrophages
- Present in tissues
- Originates from circulating monocytes
- Has the limited capacity to divide
- Forms giant cells
- Survives for long periods
- Macrophages in tissues are called histiocytes
Read And Learn More: Pathology Question And Answers
7. Neutrophils
- They are dominant cells in acute inflammation in the First 24 hours
- They are short-lived
8. Cellular events in inflammation
- Exudation of leucocytes
- Phagocytosis
Acute Inflammation Long Essays
Question 1. Describe briefly the vascular phenomenon of inflammation.
(or)
Define inflammation. Describe the various vas¬cular changes of inflammation.
Answer:
Inflammation Definition:
- Inflammation is defined as a protective response intended to eliminate the initial cause of cell injury as well as necrotic cells and tissues resulting from the original insult.
Vascular changes of inflammation:
1. Haemodynamic changes:
Changes in the vascular flow and caliber of small blood vessels in the injured tissue take place in a sequence of events as follows:
- Transient’Vasoconstriction of arterioles:
- Duration: Immediately after the injury, lasting for about
- 3-5 seconds in minor injuries
- 5 minutes in more severe injuries
- Significance: restores normal blood flow.
- Duration: Immediately after the injury, lasting for about
- Persistent progressive vasodilation: It mainly involves the arterioles and to a lesser extent venules and capillaries.
- Duration: This lasts for about half an hour after injury.
- Significance: This results in increased blood vol¬ume in the microvascular bed of the area that is responsible for redness and warmth at the site of acute inflammation.
- A rise in local hydrostatic pressure: Due to progres¬sive vasodilatation, there is an elevation of the local hydrostatic pressure
- Result:
- Transudation of fluid into the extracellular space.
- Swelling at the local site of acute inflammation.
- Result:
- Slowing/stasis of microcirculation:
- Result: Increases concentration of RBCs, thereby viscosity of blood increases.
- Margination/peripheral orientation of leuko-cytes:
- Stasis is followed by leukocytic margination along the vascular endothelium, leukocytes then move and migrate through the gaps between the endo¬thelial cells into the extravascular space. This phenomenon is known as emigration.
2. Altered vascular permeability:
- Initially, the escape of fluid occurs due to vasodilation and due to the increased volume of blood flow, there is an elevation of hydrostatic pressure
- This results in the movement of fluid from capillaries into tissues, this fluid is called transudate.
- Later the characteristic inflammatory edema, exudate, appears by increased vascular permeability
- This results in decreased intravascular osmotic pressure; and increased osmotic pressure of interstitial fluid resulting in excessive outward flow of fluid into the intersti¬tial compartment which is the inflammatory exudate.
- Fluid accumulation in extravascular spaces is called edema.
Question 2. What are the cardinal signs of inflammation?
Answer:
Cardinal Signs Of Inflammation:
There are four cardinal signs of inflammation as follows
1. Rubor- redness
- Due to Vasodilatation in the area of inflammation, there is increased blood volume
- This causes redness
2. Tumor- swelling
- Local hydrostatic pressure is increased
- This results in the transudation of fluid into the extracellular space
- This causes swelling
3. Calor-heat
- Vasodilatation is responsible for it
4. Dolor- pain
- These four signs were described by Celsus in the first century A.D.
- A fifth sign called function less- loss of function was later added by Virchow
- These signs were demonstrated by Lewis’s experience
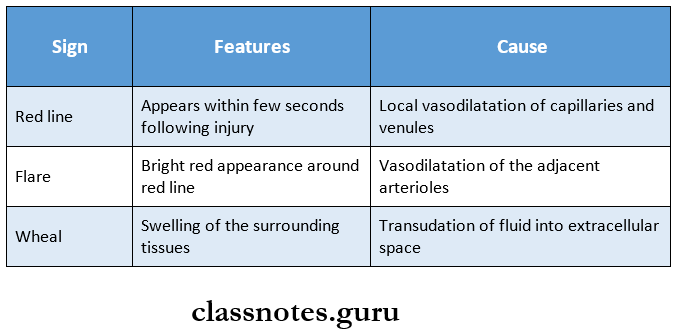
Lewis Experiment:
- To elicit the signs of inflammation, Lewis induced the changes in the skin of the inner aspect of the forearm by firm stroking with a blunt point
- The reaction is called a triple response or red-line response
- It consists of:
Question 3. Discuss cellular events in acute inflammation.
Answer:
Cellular events: Cellular events in acute inflammation can be described by
- Exudation of leucocytes
- Phagocytosis.
1. Exudation of leucocytes: The escape of leucocytes from the lumen of the microvasculature to the interstitial tissue is the most important feature.
- In acute inflammation, polymorph nuclear neutrophils (PMNs) comprise the first line of body defense, followed later by monocytes and macrophages.
- The changes leading to the migration of leukocytes are as follows:
Margination: In the early stage of inflammation there is vasodilation, subsequently slowing/stasis of the bloodstream takes place/
- Due to stasis, changes take place in microcircu¬lation.
- Central steam of the cell widens and the peripheral becomes narrower, this phenomenon is known as margination.
- RBC’s leukocytes are present in central steam;
- peripheral there is a cell-free layer due to margination,
- Neutrophils come close to the vessel wall, which is known as pavement.
Rolling and adhesion:
- Peripherally marginated and pavemented neutrophils slowly roll over the endothelial cells lin¬ing the vessel’s wall this is called as rolling.
- This is followed by the transient bond between the leukocytes and endothelial cells becoming firmer known as adhesion.
- Selectins, integrins, vascular and intercellular adhesion molecules, etc. bring about rolling and adhesion.
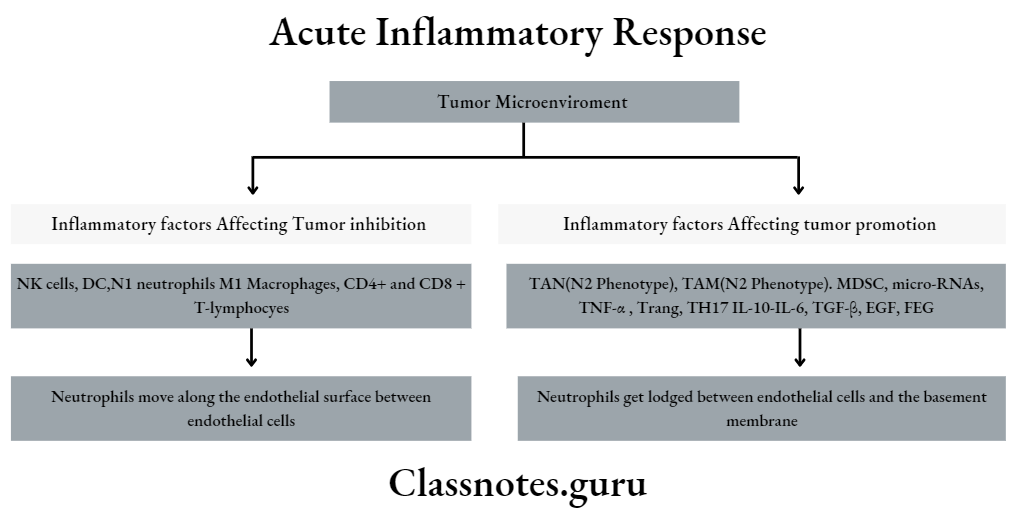
Emigration:
- Neutrophils move along the endothelial surface between endothelial cells
- Here neutrophiles give out cytoplasmic pseudo-pods.
- Neutrophils get lodged between endothelial cells and the basement membrane
- It secretes collagenases which damage the basement membrane and they escape out into extravascular space phenomenon known as emigration.
- Simultaneous to the emigration of leukocytes, RBCs also escape through the gap known as diapedesis
Chemotaxis:
- After extravasating from the blood, leukocytes migrate toward the sites of infection/injury.
- Chemotaxis is defined as the chemotactic factor me¬diated transmigration of leukocytes after crossing several barriers to reach the interstitial tis¬sues
- These chemotactic agents are also called chemokines and they carry specific receptors.
2. Phagocytosis: Phagocytosis is defined as the process of engulfment of solid particulate material by the cells. The cells performing this function are called phagocytes.
The main types of phagocytic cells are:
- Poly morpho nuclear neutrophils (PMNs): They appear early in the acute inflammatory response. Also called macrophages.
- Macrophages: These are circulating monocytes and fixed tissue mononuclear phagocytes.
Phagocytosis consists of the following steps:
1. Recognition and attachment:
- The microorganism is to be phagocytosed and the phagocytic cell repel each other due to both having a negatively charged surface.
- To overcome this repulsion, the microorganism gets coated with a naturally occurring factor in the serum called opsonins and gets targeted for phagocytosis by a process called opsonization.
- The 2 main opsonins in the serum and their cor¬responding receptors on the cell surface are as follows.
- IgG opsonin and its corresponding receptor is an Fc fragment of immunoglobulin on the sur¬face polymorphs and monocytes.
- Cgb opsonins fragment of complement and corresponding receptor for 03^ on the phagocytic cell surface.
2. Engulfment stage:
- The opsonized particle bound to the phagocyte surface is engulfed by the formation of cytoplasmic pseudopods around the particle and enveloping it in a phagocytic vacuole
- Eventually, the membrane of the phagocytic vacuole breaks from the cell surface so that the membrane-lined phagocytic vacuole lies free in the cyto¬plasm.
- This is converted into phagolysosome/phagosome on its fusion with the lysosomes of the cell.
3. Killing and degradation:
- In this stage, microorganisms are killed by the antibacterial substances and digested/degraded by hydrolytic enzymes.
Acute Inflammation Short Essays
Question 1. Classify and discuss chemical mediators of acute inflammation.
Answer:
- Chemical mediators are also called permeability factors/ endogenous mediators of increased vascular permeability; these are large and increasing numbers of endogenous compounds that can enhance vascular permeability.
- The substances acting as chemical mediators of inflammation may be released from the cells, plasma, or the damaged tissue itself.
- They are broadly classified into 2 groups as follows:
- Mediators are released by cells.
- Mediators originated from plasma
Chemical Mediators of Acute Inflammation:
1. Cell-Derived Mediators:
- Vasoactive amines [Histamine, 5-hydroxyethyl- time, neuropeptides)
- Arachidonic acid metabolites (Eicosanoids)
- Metabolites via cyclo-oxygenase pathway (prostaglandins, thromboxane A2, prostacyclin, re-solving)
- Metabolites via lipo-oxygenase pathway (5- HETE, leukotrienes, lipoxins)
- Lysosomal components (from PMNs, macrophages)
- Platelet-activating factor
- Cytokines (IL-1, TNF-a, TNF-|3, IFN-y, chemokines)
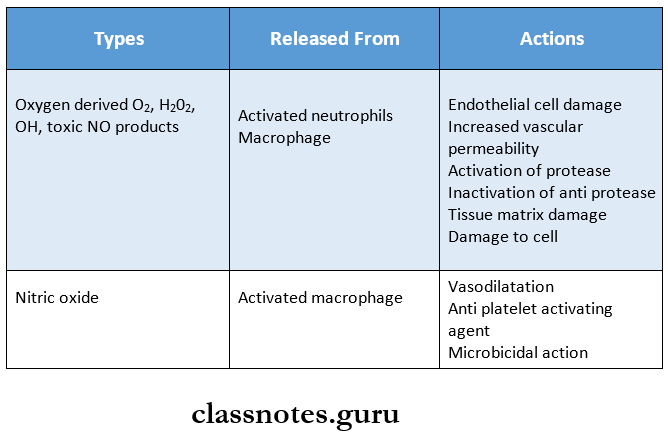
- Free radicals (Oxygen metabolites, nitric oxide)
2. Plasma-derived mediators (Plasma Proteases)
- Products of:
- The kinin system
- The clotting system
- The fibrinolytic system
- The complement system
Question 2. Chemotaxis:
Answer:
- Chemotaxis is defined as the chemotactic factor medi¬ated transmigration of leucocytes after crossing several barriers (endothelium, basement membrane, perivas¬cular, myofibroblastic, and matrix) to reach the intersti¬tial tissues.
- This concept is well illustrated by Boyden’s chamber experiment.
- In this, a Millipore filter (20m pore size) separates the suspension of leucocytes from the test solution in a tissue culture chamber. If the test solution contains chemotactic agents, the leucocytes migrate through the pores of the filter toward the chemotactic agent.
- The following agents act as potent chemotactic substances) chemokines for neutrophils.
- Leukotriene B4 is a product of the lipoxygenase pathway of arachidonic acid metabolites.
- Components of complement system (C5a and C3a in particular)
- Cytokines (Interleukins, in particular, IL-8)
- Soluble bacterial products (such as formulated pep-tides)
Acute Inflammation Short Question And Answers
Question 1. Lymphokines
Answer:
- Cytokines are polypeptide substances that are produced by activated lymphocytes and monocytes.
- Those cytokines which are produced by activated lym¬phocytes are called lymphokines.
- These agents may act on ‘self cells producing them/on other cells.
- TNF-p and IFN-y are produced by activated T-cells.
- They act as mediators of inflammation.
Question 2. Varieties of inflammation
Answer:
Types of inflammation: Depending on the host immune levels of the duration of response, inflammation can be classified as acute or chronic.
1. Acute inflammation:
- Acute inflammation is a rapid repose to injury or microbes and other foreign substances that is designed to deliver leukocytes and plasma proteins to sites of injury.
- The outcome of acute inflammation may be the removal of the exudate with the restoration of normal tissue architecture, transition to chronic inflammation or extensive destruction of the tissue resulting in scarring.
2. Chronic inflammation:
- Chronic inflammation is inflammation of prolonged duration about weeks to months to years in which active inflammation, tissue injury, and healing pro¬ceed simultaneously. Examples: tuberculosis, leprosy, fungal infection.
- Chronic infection is characterized by.
- Infiltration with mononuclear cells including macrophages, lymphocytes, and plasma cells.
- Tissue destruction is largely induced by the products of inflammatory cells.
- Repair, involving new vessel proliferation i.e., angiogenesis and fibrosis.
Question 3. The vascular phenomenon in inflammation
Answer:
Vascular changes in inflammation:
- Alteration in microvasculature i.e., capillaries, venules, and arterioles, is the first response to tissue injury.
- Alternations include Hemodynamic changes and changes in vascular permeability.
Hemodynamic changes:
- It is the earliest sign of inflammation, that results from changes in the vascular flow and caliber of small blood vessels in the injured tissue.
- It takes place as a sequence of events.
- Transient vasoconstriction of arterioles
- Persistent vasodilation of arterioles, venules, and capillaries
- Rise in local hydrostatic pressure.
- Slowing/stasis of microcirculation.
- Stasis is followed by leukocytic margination/peripheral orientation of leukocytes along the vascular endothelium.
- After sticking briefly to the vascular endothelium, the leukocytes migrate through the gap between the endothelial cells into the extravascular space, this is known as margination
Altered Vascular Permeability: Increased vascular permeability is seen during inflammation which may be due to.
- Contraction/retraction of endothelial cells.
- Injury to endothelial cells.
- Leakiness in neovascularization.
Question 4. Mention the role of histamine in inflammation
Answer:
- Role of histamine in inflammation:
- Vasodilatation
- Increases vascular permeability
- Causes itching and pain
Question 5. What are Free Radicals? Give two examples.
Answer: