Oral Medicine Pulpal Diseases Important Notes
1. Periapical Granuloma
- Many cases are usually asymptomatic
- Some may complain of mild pain on biting/ chewing solid food
- The tooth may be slightly elongated in the socket
- Histologically it mainly composed of macrophages, lymphocytes, and plasma cells
- Less frequently contains mast cells and eosinophils
2. Condensing Ostetitis
- It shows radiopacity which is not attached to the tooth
- Lamina dura is intact
- Periodontal space is widened
- The tooth may be vital or nonvital
3. Chronic Hyperplastic Pulpitis
- It is the excessive, exuberant proliferation of chronically inflamed pulp tissue
- Occurs in children and young adults
- Commonly involves large, open carious lesions
- Teeth commonly involved are deciduous molars and first permanent molars
4. Osteomyelitis
- Acute osteomyelitis does not show any radiographic changes in the early stages
- Later diffuse lytic changes appear in the bone
- Individual trabeculae become fuzzy
- Indistinct and radiolucent areas begin to appear
- Chronic osteomyelitis gives a mottled appearance in the early stages
- Established cases give a moth-eaten appearance due to the enlargement of medullary spaces and widening of Volk- Mann’s canal
Read And Learn More: Oral Medicine Question and Answers
5. Streptococcus
- It is a potent producer of hyaluronidase
- This dissolves hyaluronic acid and helps in the spread of infection
- Staphylococcus are not potent producers of hyaluronidase, thus they remain localized and do not spread infection
Oral Medicine Pulpal Diseases Short Essays
Question 1. Periapical abscess.
Answer:
Periapical Abscess
Periapical Abscess can be defined as a localized acute or chronic suppurative infection in the periapical region of a tooth.
Periapical Abscess Etiology:
- Extension of pulpal infection into periapical tissue
- Fracture of the tooth with pulp exposure
- Accidental perforation of the apical foramen during root canal treatment
- Extension of periodontal infection into the periapical tissues
- Anachoretic infection of the periapical tissues
Periapical Abscess Clinical Features:
- Acute abscess produces severe pain in the affected tooth
- There will be localized swelling and an erythematous change in the overlying mucosa
- The pain aggravates during percussion and when pressure is applied
- It causes extrusion of the tooth from its socket
- The associated tooth is non-vital and sometimes it can be mobile also
- The affected area of the jaw may be tendered on palpation
- The application of heat intensifies the pain
- Pus discharging sinus often develops
- A chronic periapical abscess often produces dull pain
Periapical Abscess Complications:
- Space infections
- Septicaemia
- Ludwig’s angina
- Cavernous sinus thrombosis
- Osteomyelitis
Periapical Abscess Radiographic Features:
- Widening of periodontal ligament space
- There is a loss of lamina dura
- An area of diffuse periapical rarefaction is seen
- Margins vary from well-defined to poor-defined
- In advanced cases, the trabeculae are destroyed
- Radiolucency may involve adjacent tooth
- Osteitis can occur at the side of the root
- Maxillary posterior teeth may lead to the destruction of a portion of the antral floor
- Roots of the affected teeth may show resorption
Periapical Abscess Management:
- Emergency opening of the pulp chamber through passing file into the periapical region
- Through and through the drain is placed in the abscess and irrigated with a 1:1 mix of 3% H2O2 and normal saline solution
- Antibiotics
- Penicillin 500 mg QID for 5 days
- Endodontic treatment
- Root canal treatment or extraction of the offending tooth as required, is carried out in 24-48 hours.
- Warm saline mouth rinse
Question 2. Clinical features and management of acute suppurative osteomyelitis.
Answer:
Acute suppurative osteomyelitis is a serious type of diffusely spreading acute inflammation of the bone characterized by extensive tissue necrosis.
Acute Suppurative Osteomyelitis Clinical Features:
- Age – It occurs after 30 years of age
- Sex – It is common among males
- Site – Mandible is commonly affected
- Presentation
- It often causes severe pain
- There is the presence of diffuse, large swelling of the jaw
- Often there is loosening and soreness of the regional teeth with difficulty in food intake
- Patients often complain of excessive salivation, difficulty in mouth opening, and bad breath
- Multiple intraoral or extraoral pus-discharging sinuses often develop
- Regional lymph nodes are enlarged and tendered to Paresthesia of the lip
- Reddening of the overlying skin or mucosa
Acute Suppurative Osteomyelitis Generalized Features:
- Fever, malaise
- Anorexia, vomiting
- Metastatic spread of infection
- Pathologic fracture
Acute Suppurative Osteomyelitis Management:
- Incision and drainage
- It is done over the fluctuant areas under antibiotic cover
- Irrigation and debridement of the area
- Debride any foreign bodies, necrotic tissue, or sequestra
- Irrigate the area with hydrogen peroxide and saline
- Antibiotic therapy
- Regimen 1- Aqueous penicillin 2 million units 4 4 hourly + oxacillin 1 gm IV 4 hourly
- Regimen 2 – Penicillin V 500 mg, 6 hourly, Dicloxacil- lin 250 mg, 4 hourly for 2 – 4 weeks
- Extraction – Extraction of the offending tooth
- Sequestrectomy – It is the removal of sequestra which are small pieces of necrotic bone that are avascular and harbor micro-organisms.
Question 3. Periapical Cemental Dysplasia.
Answer:
Periapical Cemental Dysplasia
- Periapical Cemental Dysplasia is a reactive fibro-osseous lesion derived from the odontogenic cells in the periodontal ligament
Periapical Cemental Dysplasia Etiology:
- Local factors – trauma, chronic irritation
- Nutritional deficiency
- Metabolic disturbances
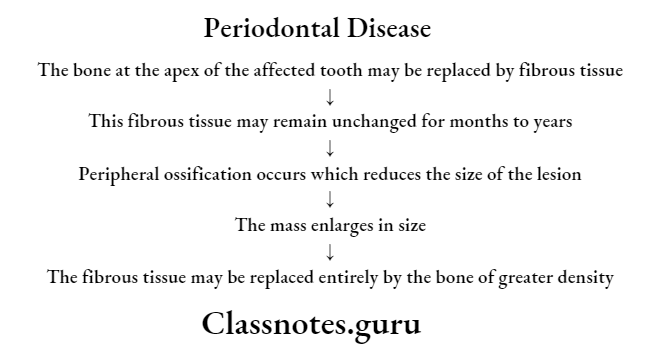
Periapical Cemental Dysplasia Pathogenesis:
Periapical Cemental Dysplasia Clinical Features:
- Age and Sex – It is common in women of middle age group
- Site – The mandibular anterior region is commonly affected
- Features
- The involved tooth is vital
- It produces pain and paresthesia in the area
- Hypercementosis is usually associated with it
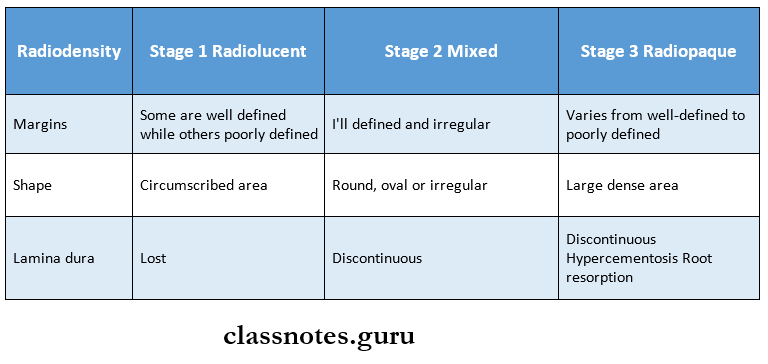
Periapical Cemental Dysplasia Radiographic Features:
- Site – It usually lies at the apex of the tooth
- Margins – Margins are well defined
Periapical Cemental Dysplasia Management:
- Maintenance phase – The patient is observed periodically
- Enucleation – It is carried out in case of larger lesions
Question 4. Internal Resorption.
Answer:
Internal Resorption
- Internal Resorption is a condition starting in the pulp, in which the pulp chamber or the root canals or both, of the tooth expand by resorption of the surrounding dentin
Internal Resorption Etiology:
- Inflammatory – Pulpal inflammatory hyperplasia
- Iatrogenic-pulpal treatment may stimulate odontoblast formation
- Idiopathic
- Trauma to teeth
Internal Resorption Types:
- Internal inflammatory resorption – It occurs due to intense inflammatory reaction within the pulp tissue
- Internal replacement resorption – In this pulpal and dentinal walls are resorbed and replaced by bone or cementum-like bone.
Internal Resorption Clinical Features:
- Age and Sex – Common in the 4th and 5th decade of life in males
- Sites – It may affect any tooth of primary as well as permanent dentition
- Symptoms – It is asymptomatic
- The affected tooth appears pink called the “pink tooth of mummery”
- It is due to the filling of the resorbed area by the hyperplastic pulp tissue
Internal Resorption Radiographic Features:
- Site – It is situated entirely on one side of the root
- Radiodensity – Homogenous radiolucency
- Pulp canal – There is an enlargement of the pulpal canal
- Root shape – Round, oval, inverted pear shape or irregular shape
- Margins – well defined
Internal Resorption Management:
- Root canal treatment of offending tooth
- Extraction, if perforation occurs
Oral Medicine Pulpal Diseases Short Answers
Question 1. Condensing Osteitis.
Answer:
Condensing Osteitis Clinical Features:
- Age – It occurs in young persons
- Site – The commonly affected tooth is the mandibular first molar
- Symptoms – Tooth is usually asymptomatic
- The patient may experience pain or tenderness on percussion in rare cases
Condensing Osteitis Radiographic Features:
- Site – Periapical area of the tooth
- Margins – vary from well-defined to diffuse
- Alveolar bone – The alveolar bone may be sclerosed between two adjacent teeth
- Surrounding structures – Narrowing of the inferior dental canal
Condensing Osteitis Management:
- Root canal treatment is carried out of the affected tooth
- Extraction of the hopeless tooth can be done
Oral Medicine Pulpal Diseases Viva Voce
- Condensing osteitis causes widening of PDL space
- Streptococcus is a potent producer of hyaluronidase
- Foam cells are present in periapical granuloma
