Mycology Important Notes
1. Classification Of Fungi
- Phycomycetes or zygomycetes
- Ascomycetes
- Basidiomycetes
- Fungi imperfect
Read And Learn More: Microbiology Question and Answers
2. Types Of Spores.
- Sexual spores – oospore, ascospore, zygospore, and basidiospore
- Vegetative or asexual spores- blastospores, arthrospores, chlamydospores
3. Lab Diagnosis Used For Fungal Infection
- KOH mounts
- Wood’s lamp
- Sabouraud’s glucose agar and cornmeal agar culture media
- Microscopic examination
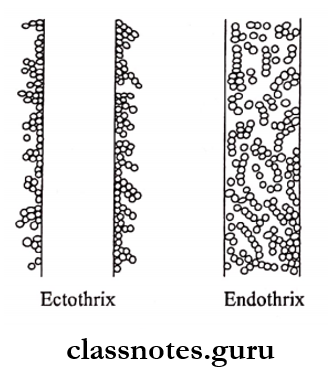
4. Types Of Hair Infection
- Endothrix
- Ectothrix
5. Candidiasis
- Causative agent – Candida albicans
- Classification
- Acute
- Pseudomembranous
- Acute atrophic
- Chronic
- Chronic hyperplastic
- Chronic atrophic
- Complications
- Intestinal Candidiasis
- Bronchopulmonary Candidiasis
- Septicemia
- Endocarditis
- Meningitis
Mycology Short Essay Questions and Answers
6. Aspergillosis
- It is the most opportunistic pathogen
- Caused by inhalation
- Diseases caused by it are
- Aspergillus asthma
- Bronchopulmonary aspergillosis
- Colonizing aspergillosis
- Invasive or disseminated aspergillosis
- Superficial infections
Mycology Long Essays
Question 1. Give an account of infections caused by Can¬dida albicans. Describe the laboratory diagnosis of Candida.
Answer:
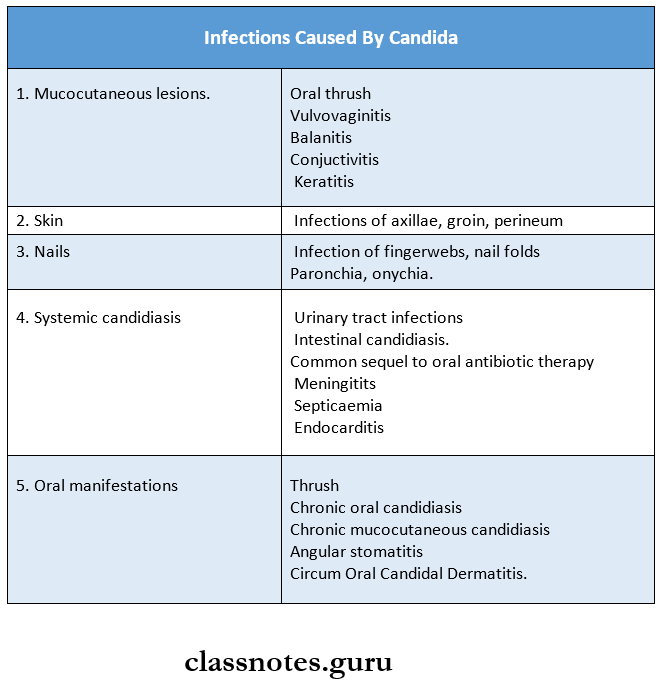
Infections Caused By Candida:
Lesions caused by Candida are as follows.
1. Oral Thrush Features:
- The lesions appear soft, white, and slightly elevated plaques
- Sites:
- Buccal mucosa
- Tongue
- Gingiva
- Palate
- The floor of the mouth
- The entire oral cavity is involved in severe cases
- Person Affected Are
- HIV patients
- Cancer patients undergoing chemotherapy or radiotherapy
- Neonates and infants
- Debilitated and chronically ill patients
Virology Long Essay Questions with Answers
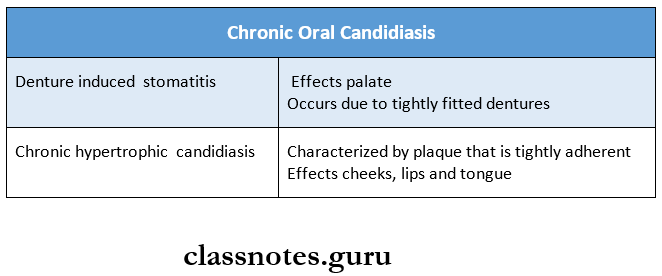
2. Chronic Oral Candidiasis
- Caused by denture-induced stomatitis or chronic hypertrophic candidiasis
3. Chronic Mucocutaneous Candidiasis
- Integral lesions are similar to other types
- Extraoral lesions involve skin, nails, and mucous
4. Angular Stomatitis
- Effects lips
- Common in immunocompromised patients
5. Circumoral Candidal Dermatitis
- Involves lips and area around lips
Candida Laboratory Diagnosis:
1. Direct Microscopy:
- Gram-stained smears and KOH mounts from le¬sions of skin, nail (or) mucous membrane are used
- These show budding Gram-positive yeast cells.
2. Culture:
- Sabouraud’s Dextrose Agar Media (SDA)
- SDA is inoculated and incubated at 25 – 37° C for 24 hours.
- Cream-coloured smooth pasty colonies appear.
- On gram staining of it shows gram positive bud¬ding yeast cells.
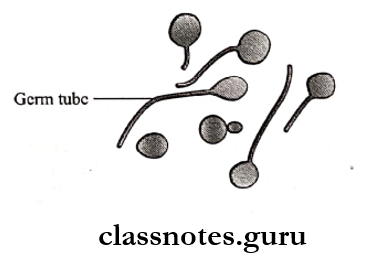
3. Identification: Candida albicans can be identified by
- Germ Tube Test:
- When incubated in human serum at 37oC, C. al-beans form germ tubes within two hours. – This is called the Reynolds braude phenomenon
- Chlamydospores.
- Chlamydospores develop in cornmeal agar at; 20 degrees C.
4. Biochemical Reactions:
- C. albicans can be identified by the assimilation and fermentation of sugar.
5. Serology:
- C. Albicans can also be identified by the precipita¬tion test with a carbohydrate extract of group A an¬tigens.
Mycology Short Essays
Question 1. Mycetoma/Madhura foot.
Answer:
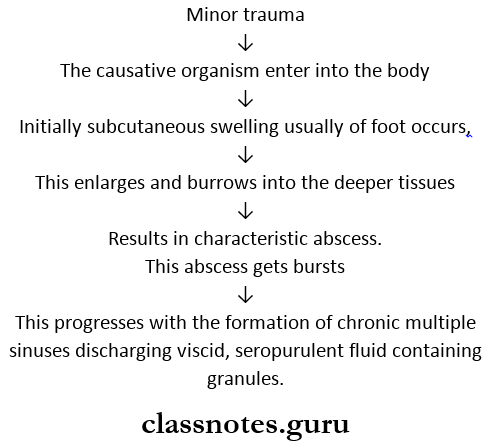
- Mycetoma is a chronic granulomatous infection of the subcutaneous tissue
- It usually affects the foot but rarely even other parts of the body
- Commonly seen in tropical countries.
Mycetoma Synonyms:
- Madhura foot it was first described in Madurai South India.
- Madhuramycosis.
Mycetoma Etiology: Causative agents are
- Eumycetoma
- Madhuvella mycetomi
- Acremonium falciforme.
- Actinomycetoma.
- Actinomadura Madurai
- Nocardia
- Streptomyces.
Mycetoma Pathogenesis:
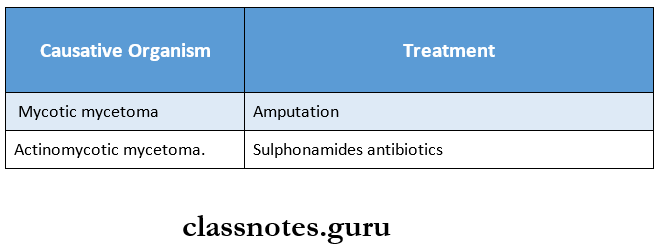
Mycetoma Treatment:
Question 2. Actinomycosis.
Answer:
Actinomycosis is a chronic granulomatous disease
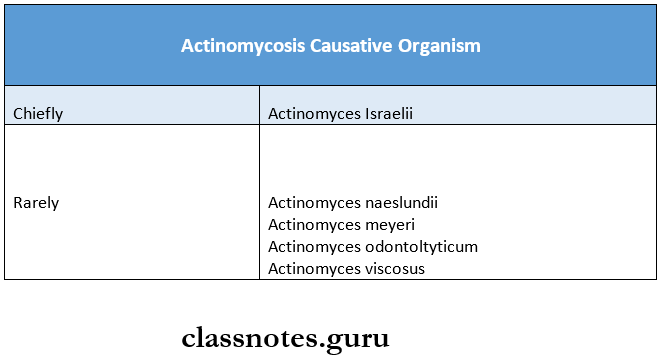
Actinomycosis Causative Organism:
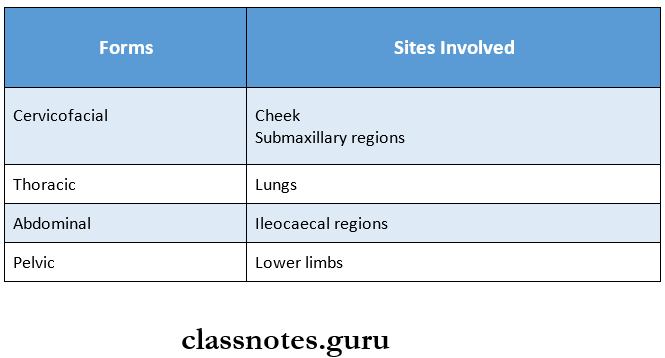
Actinomycosis Forms:
Actinomycosis Features: It is characterized by
- Multiple abscesses
- Tissue destruction
- Fibrosis
- Formation of multiple sinuses
- Painless indurated swelling
- It may cause gingivitis and periodontitis
Medical Mycology and Virology Notes PDF
Actinomycosis Diagnosis:
1. Microscopy
- Steps
- Dilute the pus with saline in a test tube
- Allow it to settle
- Sulfur granules are obtained from it
- These granules are crushed between slides
- Smears are prepared
- One of them is Gram stained and the other is acid-fast stained
- Observe these smears
- Observations
- The gram-stained smear shows Gram-positive filaments surrounded by peripheral radiating Gram-negative clubs
- This results in a sun-ray appearance
- Acid-fast smears show the central part of non-acid fast clubs surrounded by acid-fast clubs
2. Culture Cultural media used are
- Thioglycollate broth
- Brain heart infusion agar
- Blood agar
- They are incubated anaerobically and aerobically with 5% CO2 at 37 degrees C for 2 weeks
- It results in spider colonies
Actinomycosis Treatment:
- It involves surgical removal of the affected part
- The antibiotic used in such cases is penicillin
Question 3. Pathogenesis of Candida albicans.
Answer:
- Candidiasis is an opportunistic endogenous infection
- Predisposing factors are:
- Diabetes
- Immunodeficiency
- Malignancy
- Prolonged administration of antibiotics
- Patients on immunosuppressive drugs and intra¬venous catheters
- Lesions caused by it:
Mycology Short Question And Answers
Question 1. Ray fungus
Answer:
- Actinomyces are known as ray fungus
- They are
- Gram-positive
- Non-motile
- Non-sporing
- Non arid fast organism
- They appear as granules in the pus.
- When these granules are crushed between two slides and Gram stained, they show a central filamentous mycelium surrounded by a peripheral zone of swollen radiating club-shaped structures
- This gives it a sun-ray appearance
- They cause actinomycosis
Question 2. Rhinosporidiasis.
Answer:
Rhinosporidiosis is a chronic granulomatous disease.
Rhinosporidiasis Causative Organism:
- Rhinosporidium seeberi.
Rhinosporidiosis Mode of Infection:
- Frequent contact with stagnant water.
Rhinosporidiosis Features:
- Friable polyps
- Sites involved- nose, mouth, and eye
- Oral manifestations are Oropharyngeal lesions
- They appear as soft red polypoid growth and spread to the pharynx and larynx.
- These lesions contain mucoid discharge and are vascular.
Fungi and Viruses – Medical Microbiology Essays
Rhinosporidiosis Diagnosis:
- H and E stained tissue sections show a large number of endospores within the sporangia
- These are embedded in a stroma of connective tissue, and capillaries
Question 3. Cryptococcosis?
Answer:
It is caused by Cryptococcus neoformans, a capsulated yeast
Cryptococcosis Morphology:
- A spherical budding cell having a prominent polysaccharide capsule.
- It is a true yeast and gram-positive.
Cryptococcosis Pathogenesis:
- Occurs through inhalation
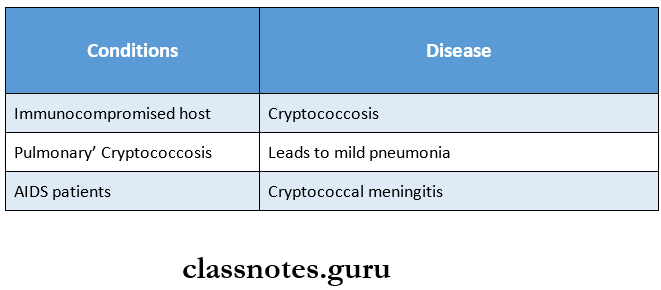
Sites Involved:
- Skin
- Lymph nodes
- Bones
- Cutaneous lesions characterized by small ulcers to large granuloma
Laboratory Diagnosis:
- Laboratory diagnosis is done by direct microscopy, culture, latex agglutination test, and animal inoculation test
Question 4. Aspergillosis?
Answer:
Aspergillosis Etiology:
- Aspergillosis is caused by inhalation of aspergillus conidia (or) mycelia fragments which are present in the decaying matter, soil (or) air.
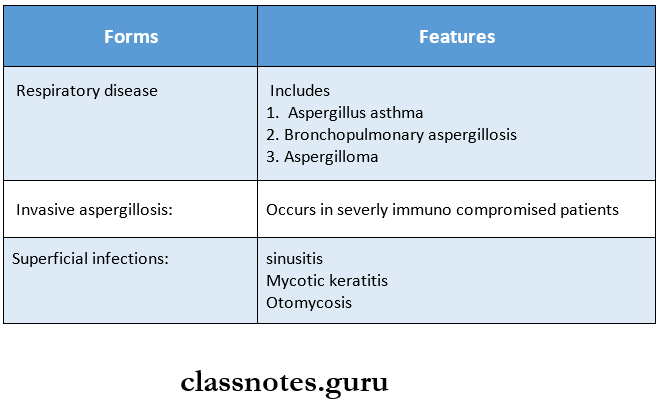
Aspergillosis Forms:
3 clinical forms of aspergillosis are
Aspergillosis Laboratory Diagnosis:
- KOH smears show non-pigmented septate hyphae with characteristic dichotomous branching.
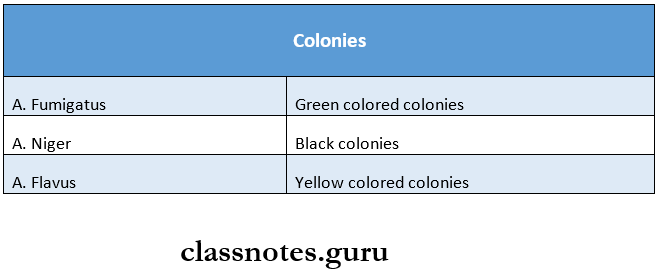
Aspergillosis Culture:
- The clinical specimen is inoculated on SDA without cycloheximide and incubated at 25oC.
- Colonies appear within 2 days
Aspergillosis Colonies:
- It shows a velvety to powder surface and is colored.
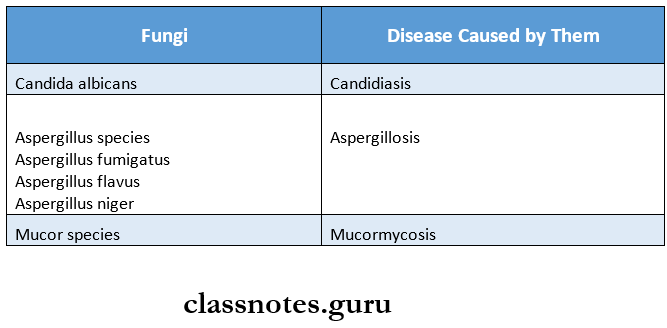
Question 5. Name three opportunistic fungi.
Answer:
- Some saprophytic fungi usually do not produce disease but may cause infection under special conditions such as immune-compromised individuals and terminal stages of chronic disease.
- These are called as opportunistic fungi.
Examples are:
Predisposing Conditions:
- Widespread use of antibiotics, corticosteroids
- Immunosuppressive drugs
- Immunosuppressive diseases like AIDS.
Question 6. Mention two important media for culturing fungi.
Answer:
- Sabouraud’s dextrose agar (SDA)
- SDA medium with antibiotics
- Brain heart infusion (BHI) agar with blood and antibiotics.
- Fungi are incubated at 37 degrees C and 25 degrees C for 3 weeks in SDA medium
- Chloramphenicol is added in the culture medium to suppress the growth of contaminating bacteria while cyloheximide is incorporated to suppress the contaminating fungi.
Question 7. Fungus affecting hair
Answer:
- Dermatophytes are the group of fungi affecting hair.
- Favus is a chronic type of ringworm involving the hair follicles
Fungus Affecting Hair Features:
- Alopecia
- Scarring
- Sparse hyphal growth
- Formation of air spaces within the hair shaft
Fungus Affecting Hair Types:
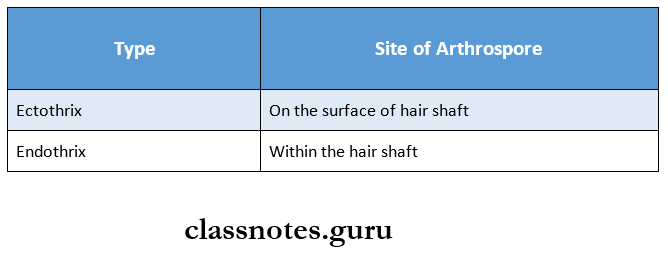
Question 8. A quick method of diagnosing Cryptococcus neoformans.
Answer:
- The latex agglutination test is a quick method for diagnosing Cryptococcus neoformans
- In this test, polystyrene latex particles are employed to absorb the antigen
- Latex agglutination tile is used in it
- The antigen detected is Cryptococcal capsular polysaccharide antigen
- The specimen used is CSF, serum, or urine.
Mycology and Virology Question Bank for NEET PG
Question 9. Mention two oral fungal infections
Answer:
- Oral fungal infections are:
- Rhinosporidiosis
- Sporotrichosis
- Histoplasmosis
- Blastomycosis
- Candidiasis
