Orofacial And Neck Infections Definition
Ludwig’s angina: It is rapidly spreading cellulitis involving simultaneously all three spaces i.e. Submandibular, sublingual & submental spaces
Cellulitis: It is a nonsuppurative infection spreading along subcutaneous tissues & connective tissue planes & caused by hemolytic streptococcus
Osteomyelitis: Infection of bone that results in inflammation of bone involving the surrounding periosteum & Haversian system
Osteoradionecrosis: It is necrosis of bone occurring secondary to radiation exposure
Orofacial And Neck Infections Important Notes
1. Classification of fascial spaces:
- According to Killey & Kay:
- In relation to mandible: Submental
- Submandibular
- Sublingual
- Buccal
- Submassetric
- Pterygomandibular
- Peritonsillar
- In relation to maxilla:
- Canine space
- Palatal space
- Parotid space Infratemporal space
- In relation to mandible: Submental
- According to Topazlan:
- Face
- Buccal
- Canine
- Masticator
- Masseter
- Pterygold
- Zygomaticotemporal
- Parotid
- Suprahyold
- Sublingual
- Submandibular
- Pharyngomaxillary
- Infrahyoid
- Anterovisceral
- Spaces of total neck
- Retropharyngeal
- Danger space
- Face
Read And Learn More: Oral and Maxillofacial Surgery Question and Answers
2. Boundaries of pterygomandibular space:
- Medially: Medial pterygoid
- Laterally: Ramus of the mandible
- Superiorly: Lateral pterygoid
- Inferiorly: Medial pterygoid
- Posteriorly: Parotid gland
- Anteriorly: Pterygomandibular raphe
3. Masticatory space consists of:
- Pterygomandibular space
- Sub masseteric space
- Superficial temporal space
- Deep temporal spaces
4. Primary spaces:
- Mandibular spaces:
- Submental
- Sublingual
- Submandibular
- Buccal
- Maxillary spaces:
- Canine space
- Buccal space
- Infratemporal space
5. Ludwig’s angina:
- Described by Wilhelm Fredrich Von Ludwig in 1836
- It is rapidly spreading cellulitis involving simultaneously all three spaces i.e.
- Submandibular, sublingual & submental spaces
Clinical Features:
- Generalized symptoms:
- Dehydration
- Fever
- Dysphagia
- Dyspnoea
- Hoarseness of voice
- Stridor
- Extraoral features:
- Brawny hard swelling of the neck involving all three spaces
- Erythematous skin covering it
- Tender
- Local rise in temperature
- Drooling of saliva
- Respiratory distress
- Intraoral features:
- Trismus
- Raised floor of the mouth
- Airway obstruction
- Increased salivation
6. Hyperbaric oxygen therapy
- Involves intermittent daily inhalation of 100% oxygen at 2-3 atmospheric pressure
Advantages of Hyperbaric oxygen therapy:
- Increases vascular supply
- Increased oxygen perfusion to ischaemic areas of infection
- Increased bactericidal and bacteriostatic action of increased oxygen concentration
7. Treatment of osteomyelitis:
- Antibiotic therapy
- Hyperbaric oxygen
- Incision and drainage
- Sequestrectomy
- Saucerization
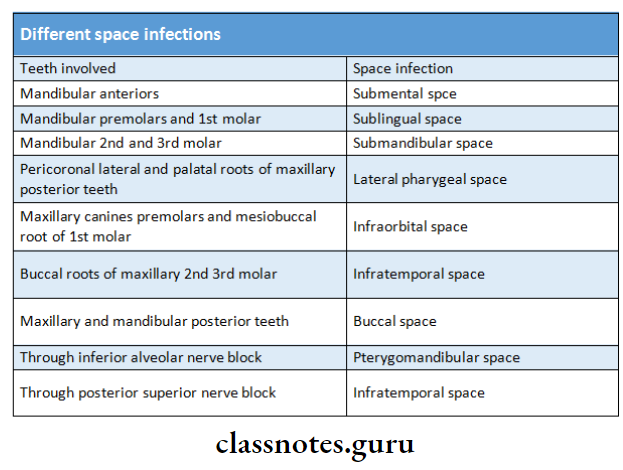
8. Teeth involved in different space infections:
9. Cavernous sinus thrombosis:
- It is the infectious thrombosis of the cavernous sinus
- Infections to cavernous sinus can spread to two routes
- The anterior route is composed of ophthalmic veins and facial veins.
- Angular vein, infraorbital vein, inferior palpebral vein
- The posterior route constitutes of pterygoid venous plexus
- Diagnosis criteria:
- Known site of infection
- Paralysis of 3,4,6 nerves
- Proptosis of the eye due to increased venous pressure in superior and inferior veins of the orbit
10. Sites of secondary infections from pterygomandibular space infection are:
- Infratemporal space
- Retropharyngeal space
- Buccal space
- Submandibular space
11. Hot potato voice is seen in:
- Retropharyngeal space infection
- Lateral pharyngeal space infection
- Ludwig’s angina
- Peritonsillar abscess
- Acute epiglottitis
- Laryngeal tumors
12. Uses of incision and drainage:
- To get rid of toxic purulent material decompress the edentulous tissues
- To allow better perfusion of blood containing antibiotics and defensive elements
- To increase oxygenation of the infected area
Orofacial And Neck Infections Long Essays
Question 1. Classify fascial spaces. Describe in detail Ludwig’s angina.
Or
Classify fascial spaces. Write clinical features, etiology, and management of Ludwig’s angina. Add a note on systemic complications
Or
Define Ludwig’s angina. Describe etiology, clinical signs & symptoms & steps in its management.
Or
Write etiopathogenesis, microbiology & management of Ludwig’s angina.
Or
Define cellulitis. Write etiopathogenesis, microbiology & management of Ludwig’s angina.
Answer:
Classification of fascial spaces:
1. According to Killey & Kay:
- In relation to mandible:
- Submental
- Submandibular
- Sublingual
- Buccal
- Submassetric
- Pterygomandibular
- Peritonsillar
- In relation to maxilla:
- Canine space
- Palatal space
- Parotid space
- Infratemporal space
2. According to Topazian
- Face:
- Buccal
- Canine
- Masticator
- Masseter
- Pterygoid
- Zygomaticotemporal
- Parotid
- Suprahyoid:
- Sublingual
- Submandibular
- Pharyngomaxillary
- Infrahyoid:
- Anterovisceral
- Spaces of total neck:
- Retropharyngeal
- Danger space
Cellulitis:
- It is a nonsuppurative infection spreading along subcutaneous tísues & connective tissue planes & caused by hemolytic streptococcus
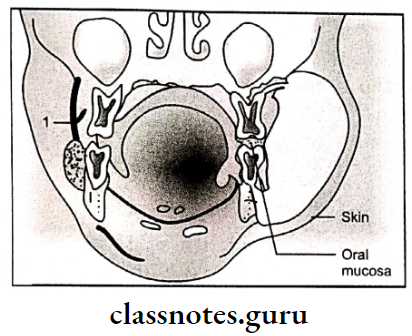
Ludwig’s Angina:
Described by Wilhelm Fredrich Von Ludwig in 1836 It is rapidly spreading cellulitis involving simultaneously all three spaces i.e. Submandibular, sublingual & submental spaces
Etiology of Ludwig’s Angina:
- Odontogenic infection
- Traumatic injuries
- Infective conditions
- Pathologic conditions
Microbiology of Ludwig’s Angina:
- The microorganism involved is streptococci
- They produce hyaluronidase & fibrinolysin
- This causes the destruction of hyaluronic acid & fibrin This spreads through tissues
- This later changes into an anaerobic infection
- Other organisms involved are pseudomonas, staphyloma-crocus, bacteroids, peptostreptococci, fusospirochaetes
Clinical Features of Ludwig’s Angina:
- Generalized symptoms:
- Dehydration
- Fever
- Dysphagia Dyspnoea
- Hoarseness of voice
- Stridor
- EExtraoralfeatures:
- Brawny hard swelling of the neck involving all three spaces
- Erythematous skin covering it
- Tender
- Local rise in temperature
- Drooling of saliva
- Respiratory distress Intraoral features Trismus
- Raised floor of the mouth
- Airway obstruction
- Increased salivation
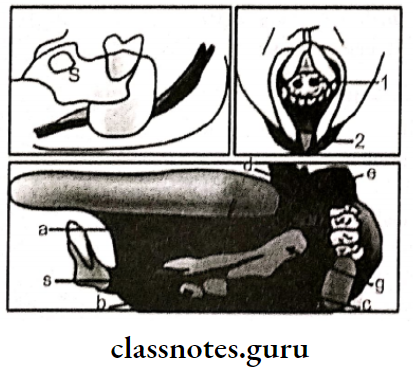
Management of Ludwig’s Angina:
- Airway maintenance:
- Intubation is contraindicated
- Tracheostomy is advisable
- Parenteral antibiotics:
- Penicillin G: 2-4 million units IV 4-6 hourly
- Gentamycin 80 mg IM BD
- For anaerobic infections: metronidazole 400 mg 8 hourly
- Erythromycin 600 mg 6-8 hourly
- Amoxicillin 500 mg 6-8 hourly orally
- Surgical management:
- The semilunar incision is given over the swelling to drain pus, and to relieve pressure over the airway
- Hydration of patient:
- IV fluids are given
- Removal of cause:
- The offending tooth is removed
Complications of Ludwig’s Angina:
- Death
- Abscess
- Septicemia
- Mediastinitis
- Carotid blow out
Question 2. Describe Classify osteomyelitis classification, features & management.
(or)
Define & classify osteomyelitis. Discuss features & management of it.
Or
Clinical features and management of chronic Osteomyelitis
Answer:
Definition of Osteomyelitis:
Infection of bone that results in inflammation of bone involving the rounding periosteum & Haversian system
According to duration & severity:
- Acute
- Chronic
Clinical types:
- Acute suppurative
- Primary chronic
- Secondary chronic
- Nonsuppurative
Presence of pus:
- Suppurative
- Acute
- Chronic
- Infantile
- Nonsuppurative
- Sclerosing
- Garre’s
- Actinomycotic
Etiology of Osteomyelitis:
- Odontogenic infections
- Traumatic injury
- Periostitis
- Hematogenous spread
Predisposing Factors of Osteomyelitis:
- Conditions reducing host defenses
- Diabetes
- Malnutrition
- Leukemia
- Alcoholism
- Conditions compromising vascularity
- Radiation
- Paget’s disease
- Fibrous disease
- Malignancy
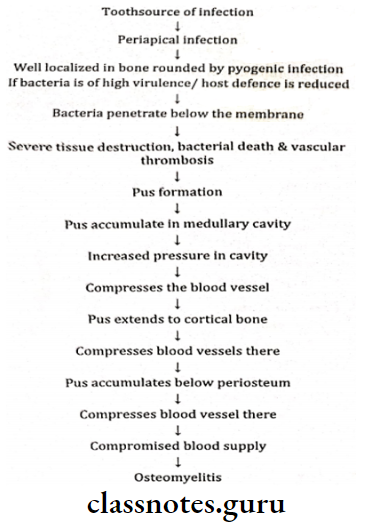
Pathogenesis of Osteomyelitis:
Features of Osteomyelitis:
- NoNontoxiconstitutional symptoms: fever, tachycardia
- Pus discharge
- Age: Before 20 years
- Site: Mandibular first molar is common
- The affected tooth is carious
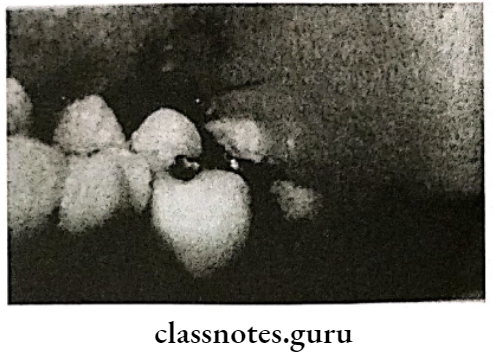
Radiographic Features of Osteomyelitis:
- Presence of sequestrum
- Presence of involucrum
- Motheaten appearance
Management of Osteomyelitis:
1. Medical management:
- Systemic antibiotics:
- Penicillin
- Metronidazole
- Clindamycin
- Given for about 2-4 months
- Local application of antibiotics:
- Due to decreased blood supply, systemic antibiotics cannot reach the desired area.
- So topical application is done
- Antibiotic-impregnated beads:
- Poly methyl methacrylate beads are impregnated with antibiotics & are placed into the desired bone
- This provides an increased concentration of antibiotics in the desired area
2. Surgical management:
- Sequestromy:
- Sequestrum is a dead bone
- It may get infected
- It may get revascularized
- It may get resorbed
- As it is avascular, antibiotics cannot reach it
- Thus antibiotics are continued till sequestrum is completely formed
- Then it is removed surgically
- Saucerization:
- It is to eliminate dead space which is created after the removal of the sequestrum
- Bony margins are trimmed to create saucer shaped defect
- This cannot accumulate blood clot
- The area is packed with medical dressings & replaced periodically
- Decortication:
- In it l, lateral & inferior cortical bone is removed
- Irrigate the underlying bone
- Debride effectively
- Resection & reconstruction:
- It is done if the above procedures fail
- Resect the infected part
- Reconstruct it with an autologous graft
- Hyperbaric oxygen:
- It is effective because:
- It enhances lysosomal degradation
- Oxygen-free radicals are toxic
- Oxygen neutralizes the exotoxins
- Elevates tissue oxygen levels
- Helps in neoangiogenesis
- It is effective because:

Question 3. Define osteonecrosis. Describe the l effects of radiation on oral & perioral structures.
Answer:
Definition of Osteonecrosis:
It is necrosis of bone occurring secondary to radiation exposure
Radiation Effects On Oral Tissues:
- Oral Mucous Membrance:
- Mucositis
- Desquamation of epithelial layer Infection of the oral cavity
- Candidiasis
- Atrophic mucosa
- Ulceration
- Radiation necrosis
- Taste buds:
- Degeneration
- Loss of taste sensation
- Salivary glands:
- Xerostomia
- Loss of salivary secretion
- Difficult & painful swallowing
- Decreased buffering capacity
- Susceptibility to radiation caries
- Teeth:
- Retards growth of teeth Inhibit cellular differentiation
- Premature eruption
- Retard root formation
- Fibroatrophy of pulp
- Radiation Caries
- Bone:
- Osteonecrosis
- Hypocellularity
- Hypoxia
- Hypovascularity
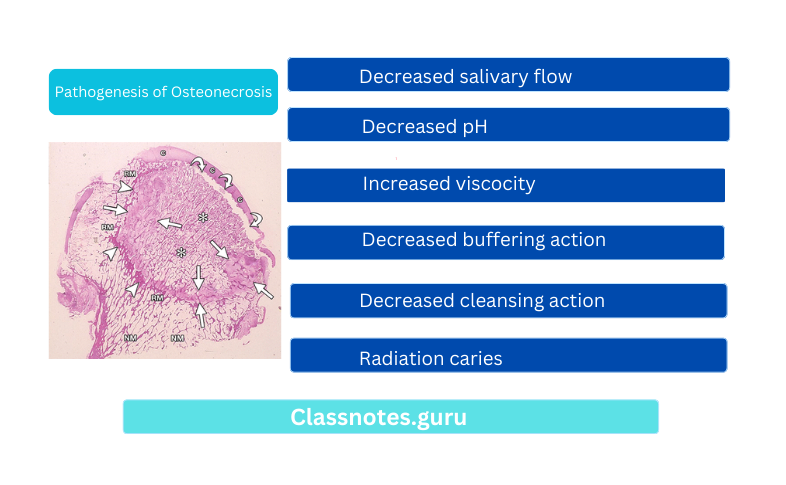
Pathogenesis of Osteonecrosis:
- Decreased salivary flow
- Decreased pH
- Decreased buffering action
- Increased viscosity
- Decreased cleansing action
- Radiation caries
Types of Osteonecrosis:
- Superficial
- Involving cervical region
- Dark pigmentation
Question 4. Describe the read of odontogenic infections and in detail about pterygomandibular space infections.
Answer:
Spread Of Odontogenic Infection
- The pathway of the spread of infection is as follows:
- Invasion of the dental pulp by bacteria after the decay of a tooth
- Inflammation, edema, and lack of collateral blood supply
- Venous congestion or avascular necrosis
- Reservoir for bacterial growth
- Periodic egress of bacteria into surrounding alveolar bone
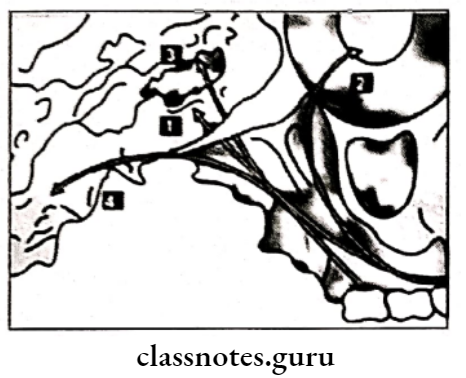
Pterygomandibular Space Infection:
1. Boundaries of Infection:
- Medially: Medial pterygoid
- Laterally: Ramus of the mandible
- Superiorly: Lateral pterygoid
- Inferiorly: Medial pterygoid
- Posteriorly: Parotid gland
- Anteriorly: Pterygomandibular raphe
2. Spread of Infection:
- From the lower third molar
3. Features Infection:
- Extreme trismus
- Minimum extraoral swelling
- Intraoral swelling over the ramus of the mandible
4. Management Infection:
- The intraoral incision is given at the angle of the mandible
- Insertion of sinus force
- Drainage of pus
- Extraorally: Incision is given 2 cm below the lower border of the mandible
- Insertion of sinus forceps
- Pus is drained
Orofacial And Neck Infections Short Essays
Question 1. Submandibular space.
Or
Submandibular space infection.
Answer:
It is the potential space between the mesial surface of the posterior aspect of the mandible
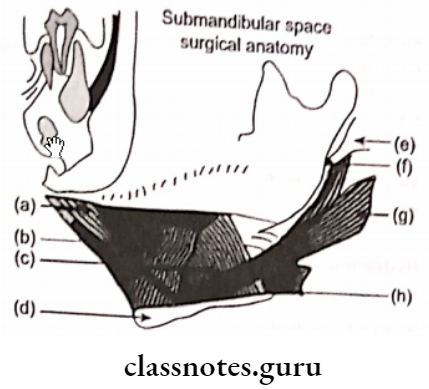
Boundaries of Submandibular Infection:
- Laterally: Body of the mandible
- Medially: Hyoglossus
- Anteriorly: Mylohyoid muscle
- Inferiorly: Digastric muscle
- Posteriorly: Hyoid bone
Spread of Submandibular Infections:
- Infected lower molars
- Maxillary sinus
- Upper molars
- Cheek
- Palate
- The floor of the mouth
Clinical Features of Submandibular Infection:
- Brawny swelling
- Intraoral pus discharge
- Vital teeth
Management of Submandibular Infection:
- The incisions are given 2cm below the border of the mandible
Question 2. Buccal space.
Or
Spread of infection from mandibular third molar
Or
Spread of infection from lower first molar its management.
Answer:
Boundaries of Buccal space:
- Anteromedially: Buccinator muscle
- Pusteromedially: Masseter
- Inferiorly: Deep cervical fascia
- Superiorly: Zygomatic process
Spread of Buccal space:
- From lower & upper molar

Features of Buccal space:
- Firm swelling in the cheek
- Extend: from angle of mouth to masseter anteroposte rich From zygomatic process to lower border of man
Management of Buccal space:
- Usually, an intraoral incision is given in the buccal vestibule
- Can be extraoral also
- The incision is placed over the angle of the mandible
- Penetrate deep into the skin & subcutaneous tissue
Insert closed forceps - Open the forceps
- Placement of drain
Question 3. Submassetric space.
Answer:
Boundaries of Submandibular Infection:
- Superiorly: Zygomatic arch Inferiorly: masseter
- Medially: Lateral of ramus
Spread Submandibular Infection:
- From the lower third molar
Features of Submandibular Infection:
- Swelling
- Extend: From the angle of mouth to masseter anteroposteriorly.
- From the geomatic process to loathing the lower border of the mandible
Complete trismus - Reddening of the overlying skin
- Tenderness
- Pus drainage
- In chronic cases, osteomyelitis occurs
Management Submandibular Infection:
- The intraoral incision is given along the anterior border of the mus
- Extraorally: Incision is given behind the mandible
Question 4. Cavernous sinus Thrombosis
Answer:
Etiology of Thrombosis:
- Furunculosis
- Infected hair follicle
- Extraction of the tooth in the presence of infection
Route of Transmission:
- External route:
- Infection from the face & lip
- Passes through facial & angular veins
- Reaches superior orbital fissure through a superior ophthalmic vein
- Reaches cavernous sinus
- Internal route:
- Dental infection
- Reaches pterygoid plexus
- Enters inferior orbital fissure
- Through the inferior ophthalmic vein enters the thsuperioror orbital fissure
- Finally reaches the cavernous sinus
Features of Thrombosis:
- Exophthalmos
- Chemosis
- Periorbital edema
- Loss of corneal reflex
- Brudanski’s sign
- Constitutional symptoms: Fever, chills, delirium, shock
Investigations of Thrombosis:
- Leucocytosis
- Parameningeal inflammation.
Management of Thrombosis:
- Broad spectrum antibiotics
- Heparin therapy
- Steroids to reduce inflammation
- Treat the primary cause
Question 5. Osteoradionecrosis / ORN.
Answer:
Definition of Osteoradionecrosis:
It is necrosis of bone occurring secondary to radiation exposure
Pathophysiology of Osteoradionecrosis:
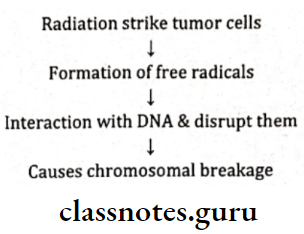
Changes of Osteoradionecrosis:
- At cellular level
- Cell may die
- DNA damage
- At the tissue level:
- Hylanization
- Thrombosis of vessels
- At the organ level:
- Hypocellular
- Hypoxia
- Hypovascular
Clinical Features of Osteoradionecrosis:
- Chronic pain
- Necrosis of bone
- Infection of tissues
- Hypovascularity of site
- Sequestration of bone
- Bone deformity
Treatment of Osteoradionecrosis:
- HBO Therapy protocol
- Stage 1: 30 dives of HBO given
- If response, the remaining 30 dives are given
- If doesn’t respond, enter stage 2
- Stage 2: 30 dives
- Sequestromy
- If the condition improves, the remaining 30 dives
- If not, enentertage 3
- Stage 3
- Resection
- Remaining 30 dives
- After 10 weeks additional 60 dives are given
- Chemotherapy
- Bleomycin
- Cisplatin
- 5 Fluorouracil
Question 6. HBO.
Or
Hyper baric oxygen
Answer:
Hyper baric oxygen
Used in the treatment of osteomyelitis & osteonecrosis
Reasons of HBO:
- Enhances lysosomal degradation
- This leads to the formation of oxygen-free radicals
- These are toxic to the anaerobic organism
- Elevated pressure of oxygen inactivates exotoxins released from pathogens
- Helps in the healing of tissues
- Helps in neoangiogenesis
- Improves vascularity
- Elevated pressure of oxygen inactivates exotoxins released from pathogens
Technique of HBO:
- The patient is made to breathe 100% oxygen through the lot’s mask
- The patient is exposed to 2.4 atmospheres of absolute pressure
- Oxygen exposure is for 90 minutes, once a day for 5 days a week
- Each exposure to hyperbaric oxygen HBO is called a “Dive”
Question 7. Sublingual space.
Answer:
Boundaries of Sublingual space:
- Anteriorly & Laterallymedial surface of the mandible
Superiorly: Sublingual mucosa - Inferiorly: Mylohyold muscle
- Posteriorly: Hyoid bone
- Medially: Genioglossus, geniohyoid, styloglossus
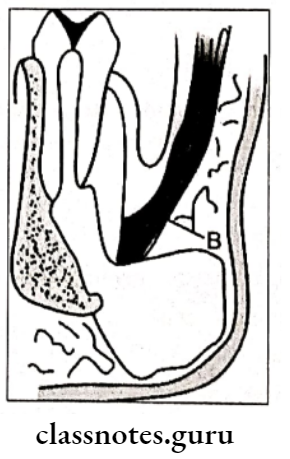
Spread of Sublingual space:
- Lower anterior
- Lower premolars
- Rarely lower first molar
Clinical Features of Sublingual Space:
- Painful swelling in the floor of the mouth
- Elevation of tongue
- Difficulty in swallowing
- Enlarged submental & submandibular lymph nodes
Management of Sublingual space:
- Extraction of the offending tooth
- Incision & drainage
- The incision in the floor of the mouth
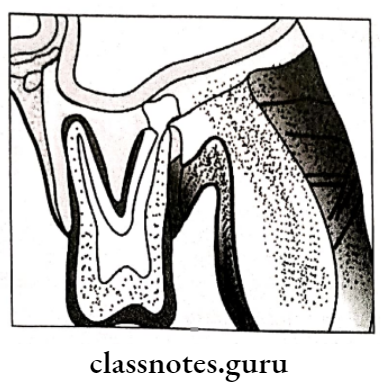
Question 8.Pericoronitis.
Answer:
Definition of Pericoronitis:
Inflammation of gingival & surrounding soft tissues of an incompletely erupted tooth
Types of Pericoronitis:
- Acute
- Chronic
- Subacute
Features of Pericoronitis:
- Red, erythematous lesion
- Tenderness
- Radiating pain
- Difficulty in closing jaws
- Foul taste
- Swelling of the cheek region
Sequele of Pericoronitis:
- Pericoronal abscess
- Cyst formation
- Lymphadenitis
- Cellulitis
- Ludwig’s angina
Treatment of Pericoronitis:
- Cleanse the area Anesthetize the area
- Reflection of flap
- Debridement
- Postoperative instructions
- Recall
- Next visit decide whether to retain or extract the tooth
- For extraction impaction
- For retaining
- Wedge-shaped incision
- Removal of tissue
- Placement of periodontal dressing
Question 9. Epulis.
Answer:
Epulis
It is swelling situated on the gums
Types of Epulis:
- Granulomatous epulis:
- Due to caries tooth, dentures, poor oral hygiene
- Soft to firm swelling
- Bleeds on touch
- Treatment:
- Maintenance of oral hygiene
- Restoration of carious tooth
2. Fibrous epulis:
- Fibroma arising from the periodontal membrane
- Undergoes sarcomatous change
- Firm. Polypoid mass
- Slowly growing
- NoNontenderreatment:
-
- Surgical Excision.
3. Giant cell epulis:
- Synonym: Myeloid epulis
- Soft to firm swelling over gums
- Expansion of bones
- May ulcerate
- Treatment:
- Small tumors: Curettage
- Large tumors: Radical excision
4. Carcinomatous epulis:
- Arises from the mucous membrane of the alveolar margin
- Nonhealing, painful ulcer
- Infiltrate bone
- Lymph node involvement
- Treatment:
- Wide excision
- Radiotherapy
Question 10. Garre’s Osteomyelitis.
Answer:
Garre’s Osteomyelitis
- Represents reactive periosteal osteogenesis in response to low-grade infection or trauma
- Characterized by focal thickening of the involved bone due to subperiosteal new bone deposition
Factors of Garre’s Osteomyelitis:
- Chronic periapical abscess
- Chronic periapical granuloma
- Chronic periapical cyst
- Chronic parotid abscess
- Chronic periodontal infection
- Chronic trauma
Clinical Features of Garre’s Osteomyelitis:
- Age: Children & young adults
- Site: Common in the mandible
Presentation of Garre’s Osteomyelitis:
- Involved teeth carious, nonvital
- Swelling
- Thickness of bone upto 1 cm
- Slight tenderness
- The overlying skin is normal
- Slight pyrexia
- Moderate leukocytosis
Radiographic Features:
- Radiolucent lesion
- Bony overgrowth duplication of the cortex
- Onion skin appearance
Treatment of Garre’s Osteomyelitis:
- Elimination of the causative agent
- Extraction of the offending tooth
- Spontaneous re-modeling of the cortical swelling
Question 11. Incision & drainage.
Answer:
Technique of Incision:
Orofacial And Neck Infections Short Question And Answers
Question 1. Peritonsillar abscess/ Quinsy.
Answer:
Peritonsillar abscess
Infection in the connective tissue between tonsil & superior constrictor
Spread of Peritonsillar abscess:
- From the lower third molar
Features of Peritonsillar abscess:
- Acute pain in the throat
- Radiates to ear
- Dysphagia
- Nausea
- Constipation
- Poor oral hygiene Body aches & headache
- Enlarged lymph nodes
- Dyspnoea
- Trismus
- Deviation of uvula
- Hoarseness of voice
- Foul breath
Management of Peritonsillar abscess:
- Antibiotics
- Incision over the most prominent part
- Analgesics
- Warm saline gargles
- IV fluids
- Tonsillectomy
Question 2. Microbiology of odontogenic infections.
Answer:
Microbiology of odontogenic infections
Microorganisms involved are
- Gram +ve:
- Streptococci
- Staphylococci
- Gram -ve:
- Neisseria
- Corynebacterium
- Hemophilia
- Anaerobic:
- Gram +ve
- Streptococci
- Peptostreptococci
- Gram -ve
- Actinomycetes
- Fusobacterium
- Gram +ve
Question 3. Sequestrum.
Answer:
Sequestrum
- A fragment of dead tissue, usually bone, that has separated from healthy tissue as a result of injury/disease
- It is avascular
Types of Sequestrum:
- Primary Of Sequestrum:
- A piece of dead bone that completely separates from sound bone during the process of necrosis
- Secondary of Sequestrum:
- A piece of dead bone that is partially separated from sound bone during the process of necrosis but may be pushed back into position
- Management of Sequestrum:
- It appears as radiopaque foci
- It is surgically removed by sequestrum
Question 4. Involucrum.
Answer:
Involucrum
- It is an enveloping sheath/ membrane such as the sheath of new bone that forms around a sequestra
- Occurs when the acute phase of disease subsides Formed over the inflammatory focus
Question 5. Masticatory space infection.
Answer:
Masticatory space infection
These are potential spaces present around the muscles of mastication.
- Involves infection from the third molar
- A common clinical feature is trismus due to spasms of muscles
Involves of Masticatory space:
- Sub masseteric space
- Pterygomandibular space
- Temporal space
Question 6. Infratemporal space.
Answer:
Infratemporal space
Also called retro zygomatic space by Sicher
Boundaries of Infratemporal space:
- Laterally ramus of the mandible, temporalis muscle, and its tendons
- Medially- Medial pterygoid plate, lateral pterygoid muscle, medial pterygoid muscle, the lower part of the temporal fossa of the skull, and lateral wall of the larynx
- Superiorly- Infratemporal surface of the greater wing of the sphenoid and zygomatic arch
- Inferiorly-Lateral pterygoid muscle
- Anteriorly-Infratemporal surface of maxilla
- Posteriorly-Parotid gland
Spread of Infratemporal space:
- Buccal roots of maxillary second and third molars
- LA injections from contaminated needles in the tuberosity
- Other space infection
Features of Infratemporal space:
- Trismus
- Bulging of the temporalis muscle
- Marked swelling of the face on the involved side
- Proposed eye
- Swelling in the tuberosity area
- Elevated temperature
Question 7. Boundaries and contents of canine space
Answer:
Boundaries of Canine Space:
- Superiorly
- Levator labii superioris alaque nasi
- Levator labii superioris
- Zygomaticus minor muscle
- Inferiorly
- Caninus muscle
- Anteriorly
- Orbicularis oris
- Posteriorly
- Buccinator muscle
- Medially
- Anterolateral surface of maxilla
Contents of Canine Space:
- Infraorbital foramen
- Branches of infraorbital nerves and vessels
Orofacial And Neck Infections Viva Voce
- A deficit of the function of the abducent nerve is one of the early signs of cavernous sinus thrombosis
- RoThe roof pterygomandibular space is formed by lathe lateral pterygoid
- The severe complication of canine space infection is cavernous sinus thrombosis
- Osteoradionecrosis occurs due to damage to the blood vessels
- Infection from a maxillary first molar region spreads to buccal space
- Fascial spaces are filled by loose connective tissue
- The characteristic feature of Infection of masticator space is trismus
- Incision and drainage of masticator space should be attempted extraoral in the angular region
- Infections from the mandibular 1st molar spread to sub-lingual space
- In Ludwig’s angina, submandibular, sublingual a, and submental spaces are involved bilaterally
- In Ludwig’s angina, the incision should be placed deep upto mucous membrane of the floor of the mouth
- Infection of lateral pharyngeal space can transverse to the posterior mediastinum
- Infections from submandibular space and submental space usually transverse to the anterior mediastinum
- Osteomyelitis begins as an inflammation of the medullary bone
- Osteomyelitis is common in the mandible
- Osteomyelitis is most commonly caused by staphylococcus
- In treating osteomyelitis, hyperbaric oxygen used consists of 100% oxygen at 3 atm
- Dangerous area of the face the area of the upper lip, commissure, and lower lip
- Danger space potential space between the alar space and prevertebral fascia.
