Facial Neuropathology Definition
Trigeminal neuralgia: It is a sudden, severe, brief, stabbing, recurrent pain along the distribution of the trigeminal nerve
Facial Neuropathology Important Notes
1. Trigger zones for trigeminal neuralgia:
- Vermillion border of lips
- Around eyes
- Ala of nose
2. 5 hypotheses of Bell’s palsy:
- Rheumatic
- Cold
- Ischaemia
- Immunological
- Viral
3. Classification of nerve injuries:
- Seddon’s Classification:
- Neuropraxia:
- Axonotmesis
- Neurotmesis
- Sunderland’s Classification:
- First-degree injury
- Type 1: Mild compression of the nerve trunk
- Type 2: Moderate compression
- Type 3: Severe compression
- Second-degree nerve injury
- Third-degree nerve injury
- Fourth-degree nerve injury
- Fifth-degree nerve injury
- First-degree injury
Facial Neuropathology Long Essays
Question 1. Describe in detail bout trigeminal neuralgia, its etiology, clinical features & management.
Or
Define trigeminal neuralgia & describe in brief its etiology, clinical signs & symptoms & management.
Or
Tic Dolourex
Answer:
Trigeminal Neuralgia of Definition:
It is a sudden, severe, brief, stabbing, recurrent pain along the distribution of the trigeminal nerve
Etiology of Trigeminal Neuralgia :
- Pathological:
- Dental pathosis
- Allergic
- Traction on divisions of the trigeminal nerve
- Irritation to the ganglion
- Ischaemia
- Secondary lesions
- Aneurysm of internal carotid artery
Read And Learn More: Oral and Maxillofacial Surgery Question and Answers
Clinical Features of Trigeminal Neuralgia:
- AGE: Around 35 years
- Sex: Common in female
- Site: Right lower portion of the face, usually unilateral
- Duration: A few seconds to a few minutes
- As time passes duration between the cycles decreases
- Nature: stabbing or lancinating
- Aggravating factors: Activation of Trigger Zones These are the vermillion border of the lip, around the eyes, ala of the nose
Interference with other activities:
- The patient avoids shaving, washing their face, and chewing. Brushing, as these may aggregate pain
- These lead to a poor lifestyle
- Extreme cases: leads to “Frozen or Mask Like Face”
Medical management of Trigeminal Neuralgia:
- Medical:
- Carbamazepine: Initial dose: 100 mg twice daily until relief is achieved
- Dilantin: 300-400 mg in single or divided doses
- Gabapentin: 11200-3600 mg/day TID/QID
- Baclofen: 10 mg TID
- Amitriptyline: 25-75 mg/day QID
- Combination therapy: Dilantin + carbamazepine
- Surgical:
- Injection of alcohol in gasserian ganglion
- Nerve avulsion: Performed on lingual, buccal, or mental nerve
- Part of the nerve is sectioned
- Electrocoagulation of gasserian ganglion: Radiotherapyy is done
- Rhizotomy: Trigeminal sensory root is sectioned
- Newer technique: Tens
- Low-intensity current is used at high frequency and is applied to the skin through electrodes attached by a conduction paste

Facial Neuropathology Short Essays
Question 1. Facial nerve palsy.
Answer:
Etiology of Facial nerve palsy:
- Congenital
- Traumatic
- Infections
- Inflammation
- Neoplastic
- Idiopathic
Clinical Features of Facial nerve palsy:
- Unable to raise eyebrows
- Unable to blow cheeks
- Expressionless face
- Absence of wrinkling
- Absence of function of the mandibular nerve
- Lack of movement of the upper lip
- Unable to close one eye
- Absence of nasolabial fold
- Absence of taste sensation
- Drooling of the lower lip on the affected side
Bell’s Palsy:
- Idiopathic paralysis of the facial nerve of sudden onset
Etiology: 5 Hypothesis:
- Rheumatic
- Cold
- Ischaemia.
- Immunological
- Viral
Clinical Features of Bell’s Palsy:
- Pain in post auricular region
- Sudden onset
- Unilateral loss of function
- Loss of facial expression
- Absence of wrinkling Inability to close the eye
- Watering of eye Inability to blow the cheek
- Obliteration of nasolabial fold
- Loss of taste sensation
- Hyperacute
- Slurring of speech
Management Bell’s Palsy:
- Physiotherapy
- Facial exercises
- Massaging
- Electrical stimulation
- Protection to the eye:
- Covering of eye with a bandage
- Medical management:
- Prednisolone – 60-80 mg per day
- 3 tablets for 1st 4 days
- 2 tablets for 2nd 4 days
- 1 tablet for 3rd 4 days
- Surgical treatment:
- Nerve decompression
- Nerve grafting
Question 3. Diagnosis of trigeminal neuralgia.
Answer:
- Paroxysmal unilateral facial pain:
- Distribution of pain along branches of the trigeminal nerve
- Trigger zones positive
- Absence of symptoms between attacks
- No neurological deficit MRI for vascular lesions
- White & Sweet Criteria:
- Paroxysmal pain
- Stimulation of trigger zones causes pain
- Pain along the distribution of nerve
- Unilateral pain
- Normal neurological examination
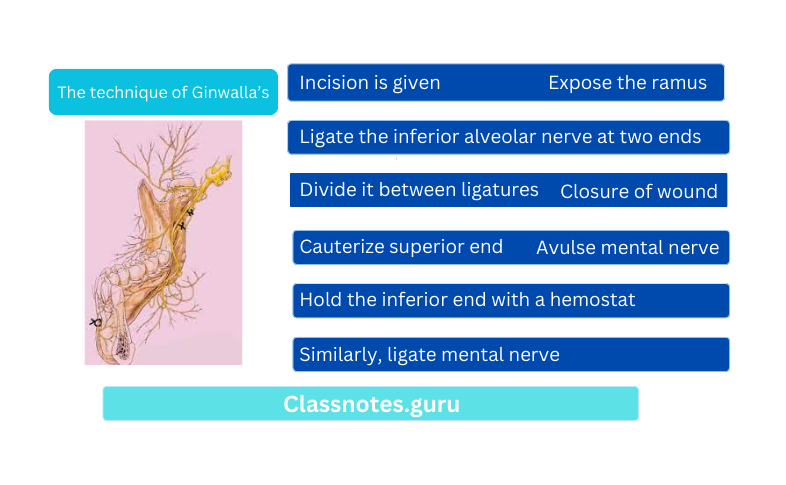
Question 4. Ginwalla’s technique.
Answer:
Ginwalla’s technique
Used for the management of trigeminal neuralgia
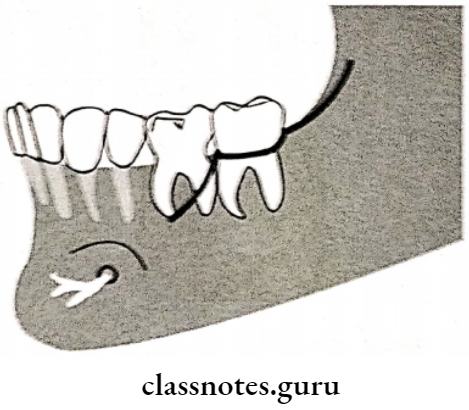
The extent of Incision of Ginwalla’s technique:
- Anterior border of the ramus up to the retromolar area
- It is split into 2 halves
- One extends lingually & the other buccally
- Results in Y-shaped incision
The technique of Ginwalla’s:
- Incision is given
- Expose the ramus
- Ligate the inferior alveolar nerve at two ends
- Divide it between ligatures
- Cauterize superior end
- Hold the inferior end with a hemostat
- Similarly, ligate mental nerve
- Avulse mental nerve
- Excise the remaining inferior alveolar nerve
- Closure of wound
Question 5. Nerve injuries in oral surgery.
Answer:
Seddon’s Classification:
- Neuropraxia:
- Results from mild insult to a nerve
- No axon degeneration occurs
- Mild paraesthesia present
- Axonotmesis:
- Severe injury
- Degeneration of afferent fibers
- Severe paraesthesia present
- Neuromimesis:
- Most severe injury of the nerve
- Complete destruction of nerve structure
- Anesthesia is present
- If the nerve is present within the bony canal, recovery can occur by the process of nerve degeneration
Sunderland’s Classification:
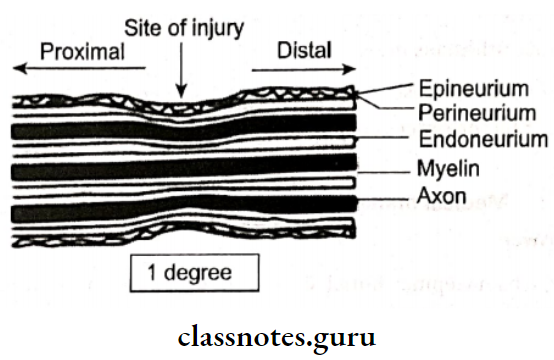
1. First-degree injury:
- Type 1:
- Mild compression of the nerve trunk
- Results in ischemia & conduction block
- No axonal degeneration
- Recovery within a day
- Type 2:
- Moderate compression
- Results in enema & conduction block
- Recovery within 1–2 days
- Type 3:
- Severe compression
- Disruption of myelin sheath
- Sensory loss
- Recovery in 1-2 months
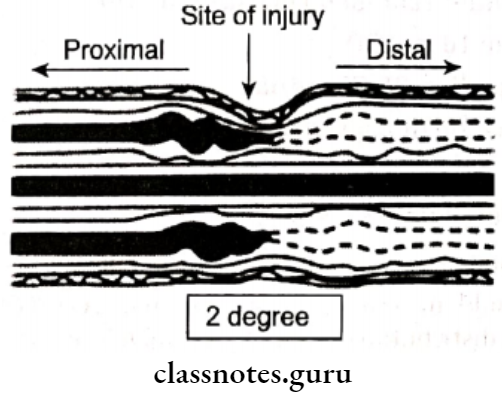
2. Second-degree nerve injury:
- Synonymous with Seddon’s axonotmesis
- Axonal damage occurs
- Epineurium, perimetrium & endoneurium is intact
- Paraesthesia & anaesthesia present
- Spontaneous recovery
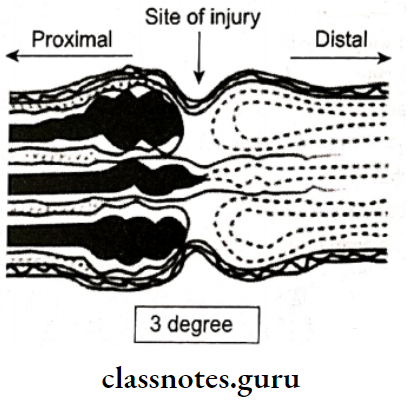
3. Third-degree nerve injury:
- Synonymous with Seddon’s axonotmesis
- Axonal damage
- Damage to epineurium
- Paraesthesia & anesthesia present
- Regeneration of axon is blocked
- Incomplete sensory recovery Surgical repair needed
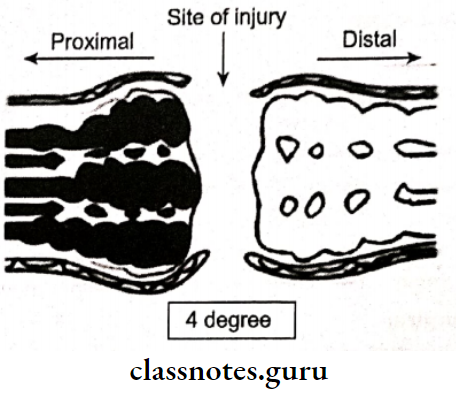
4. Fourth-degree nerve injury:
- Synonymous to Seddon’s axonotmesis Damage epineurium, endoneurium & axons
- Intact epineurium
- Sensory impairment
- Poor recovery
- Surgical intervention needed
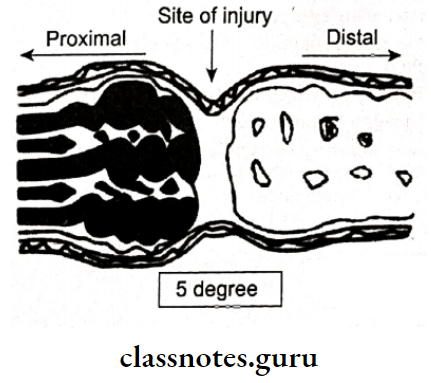
5. Fifth-degree nerve injury:
- No conduction of impulses
- Even epimerism is destroyed
- Poor prognosis
Facial Neuropathology Short Question And Answers
Question 1. Bell’s sign.
Answer:
Bell’s sign
- Seen in Bell palsy
- The inability to close the eye occurs in it
- On attempting to close the eye, the eyeballs roll upwards
- This peculiar sign is called the “Bells Sign”
Question 2. Trigger zones.
Answer:
Trigger zones
- These are cutaneous zones located along the distribution of divisions of the nerve
- Stimulation of these zones occurs by the following
- Shaving, washing face, chewing, brushing, applying lotion, cosmetics, eating, touching, strong breeze
- Leads to pain
Question 3. Neurectomy.
Answer:
Neurectomy
- This is palliative treatment in which peripheral branches of the nerve are avulsed
- This prevents transmission of the peripheral impulses to the central trigeminal system
- It can be done over
- Infraorbital nerve
- Mental nerve
- Inferior alveolar nerve
- Lingual nerve
Facial Neuropathology Viva Voce
- Classic Bell’s palsy results from a lesion involving the glossopharyngeal nerve
- The trigeminal nerve is a mixed nerve
- A gasserian ganglion is found in a space known as Merkel’s cavity
- The initial stage of paralysis of the facial nerve is the tongue deviates to the same side on the protrusion
- Tic douloureux treatment includes carbamazepine
- Damage to a seventh cranial nerve is associated with Bell’s palsy
- Trigeminal neuralgia is characterized by sharp pain when pressure is applied to the affected area
