Clinical Topics Definition
Local anesthesia: It is loss of sensation in a circumscribed area of the body characterized by depression of excitation of nerve ending & inhibition of the conduction process of peripheral nerve.
Clinical Topics Important Notes
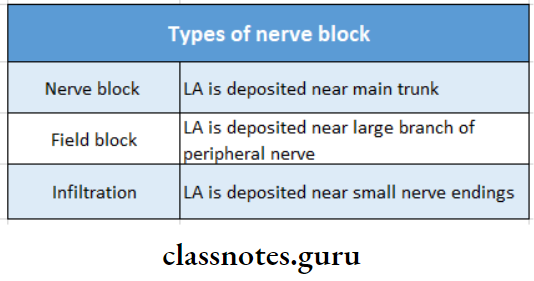
1. Types of nerve blocks:
2. Inferior nerve block:
- Areas Anaesthesized:
- LA is deposited near the main trunk
- LA is deposited near a large branch of the peripheral nerve
- LA is deposited near small nerve endings
- The body of the mandible and the inferior portion of the ramus
- Mandibular teeth
- Mucous membrane and underlying tissues anterior to the 1st mandibular molar
- Complications:
- Hematoma
- Trismus
- Transient facial paralysis
3. Gow Gates technique:
- It is open mouth technique
- Landmarks
- Extraoral
- The lower border of the tragus
- Corner of mouth
- Intraoral
- Mesiolingual cusp of the maxillary second molar
- Penetration of needle just distal to maxillary second molar
- Extraoral
4. Hematoma:
- It is commonly associated with a posterior superior alveolar nerve block and inferior nerve block
- Hematoma formation in the posterior superior alveolar nerve block is due to injury of the pterygoid plex which results in immediate swelling of the face
- To avoid this short needles are used
5. Extra oral techniques:
- Maxillary: In this, the needle is directed anterior to the lateral pterygoid plate into the pterygopalatine fossa
- Mandibular: In it the needle is inserted from below the zygomatic arch and is directed posterior to the lateral pt plate below the foramen ovale
6. Advantages of adding vasoconstrictor agents:
- Prevents rapid absorption of LA
- Prolongs the duration of action
- Reduces the toxicity of LA
- Bleeding in the area is minimized
7. Composition of LA:
- Local anesthetic-Ester or amide
- Vasoconstrictor- Epinephrine
- Antioxidant- Sodium metabisulphite.
- It competes with the vasoconstrictor for the available oxygen died to sodium bisulfate
- Preservative Methylparaben
- Fungicisde – Thymol
- Salt- Sodium chloride
- Vehicle- Distilled water or Ringer’s lactate solution
8. Theories of anesthesia:
- Surface charge theory
- Specific receptor theory Acetylcholine theory
- Membrane expansion theory
- Calcium displacement theory
9. Theories of pain:
- Specificity theory
- Pattern theory
- Gate control theory
10. Vazirani Akinosi technique:
- It is closed mouth mandibular nerve block
- Used in patients with a limited mandibular opening as a result of infection, trauma, or postinjection trismus
- Nerves anesthetized are
- Inferior alveolar
- Incisive
- Mental
- Lingual
- Mylohyoid
Clinical Topics Long Essays
Question 1. Describe the technique of inferior dental nerve block anesthesia. Enumerate complications of the technique.
Answer:
Inferior Alveolar Nerve Block:
- Nerves anesthetized: Inferior alveolar nerve & its branches
- Areas to be anesthetized: Mandibular teeth & its supporting tissues
Landmarks of Nerve Block:
- Mucobuccal fold
- Anterior border of coronoid process
- Coronoid notch
- Pterygomandibular raphe
- Retromolar pad
- Retromolar triangle
- External oblique ridge
The technique of Nerve Block:
- Position the patient in a semi-reclined position
- Move your index finger over the mesiobuccal fold up to the external oblique ridge
- Move it up & down to obtain depression
- This is a coronoid notch
- Retract the cheek
- Support the mandible
- Insert 1 5/8 inch 25 gauge needle from the lingual side
- Aspirate & Slowly deposit the solution
Read And Learn More: Oral and Maxillofacial Surgery Question and Answers
Positive Aspiration: 10-15%:
- Symptoms:
- Subjective: Tingling & numbness over the lower lip & lateral border of the tongue
- Objective: Instrumentation demonstrates the absence of pain
Complications of Nerve Block:
- Trismus
- Hematoma
- Transient facial paralysis
Question 2. Describe in detail the surgical anatomy, indications & contraindications & technique of the inferior alveolar nerve block.
Answer:
Surgical Anatomy:
- It is a branch of the posterior division of the mandibular nerve i.e division of a trigeminal nerve
- It passes between the medial pterygoid muscle & ramus of the mandible
Passes through the mandibular foramen - On reaching the anterior teeth it divides into incisive & mental branches
- Before entering into the mandibular foramen it gives out a mylohyoid branch to supply the mylohyoid muscle
- Inferior Alveolar Nerve Block
Indications of Surgical Anatomy:
- Any surgery related to multiple mandibular teeth
- Buccal soft tissue anesthesia
- Lingual soft tissue anesthesia
Contraindications of Surgical Anatomy:
- Infections
- Lip biting
- Young children
- Physical & mentally handicapped children
- Nerves anesthetized: Inferior alveolar nerve & its branches
- Areas to be anesthetized: Mandibular teeth & its supporting tissues
Landmarks of Surgical Anatomy:
- Mucobuccal fold
- Anterior border of coronoid process
- Coronoid notch
- Pterygomandibular raphe
- Retromolar pad
- Retromolar triangle
- External oblique ridge
The Technique of Surgical Anatomy:
- Position the patient in a semi-reclined position
- Move your index finger over the mesiobuccal fold up to the external oblique ridge
- Move it up & down to obtain depression
- This is a coronoid notch
- Retract the cheek
- Support the mandible
- Insert 1 5/8 inch 25 gauge needle from the lingual side
- Aspirate & Slowly deposit the solution
- Positive Aspiration: 10-15%:
Question 3. Write the course of the maxillary nerve. And write the landmarks for the posterior superior nerve block.
Answer:
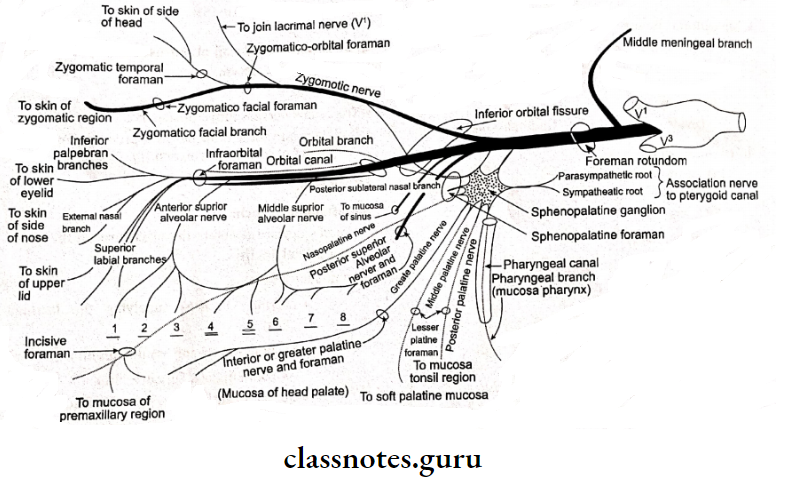
Maxillary Nerve:
- Originates at the middle of the semilunar ganglion
- Continues in the lower part of the cavernous sinus
- Passes to the foramen rotundum
- Enters pterygopalatine fossa
- Enters the inferior orbital fissure to enter the orbit
Branches of Maxillary Nerve:
1. In middle cranial fossa:
- Middle meningeal nerve to supply
2. In pterygopalatine fossa:
- Zygomatic nerve:
- Passes anteriorly & laterally
- Divides into
- Zygomaticofacial nerve- Pierces the orbicular oris & supplies prominence of cheek Zygomaticotemporal nerve
- Enters the temporal fossa & supplies the skin over the anterior temporal fossa region
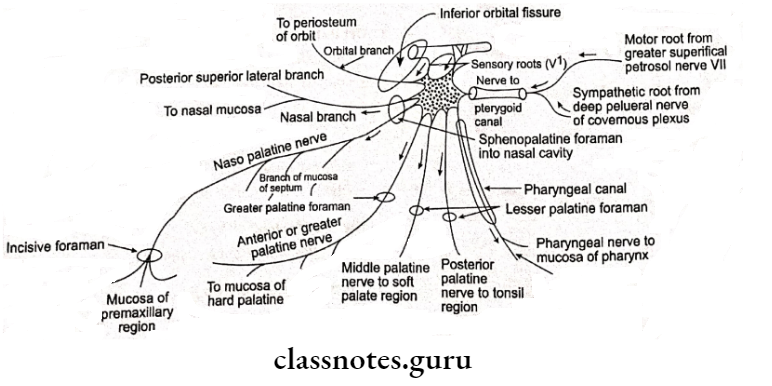
- Pterygopalatine nerve:
- Branches:
- Orbital branches: Using inferior orbital fissure, supplies periosteum of orbit, posterior ethmoid cells & sphenoid sinus
- Nasal branches: Divides into posterior superior lateral & medial or septal branches
- Branches:
- Palatine branches:
- Descends in the pterygopalatine canal, divides into
- Greater or anterior palatine- supply hard palate
- Middle palatine-sensory to soft palate
- Descends in the pterygopalatine canal, divides into
- Posterior palatine:
- Supplies mucous membrane to tonsil.
3. Posterior superior alveolar nerve:
- Divides into many branches & descends downward to supply maxillary molars & their supporting gingivae
4. Branches in infraorbital groove & canal:
- Middle superior alveolar nerve:
- Supplies the posterior part of the maxillary sinus
- Descends downward
- Divides & supplies maxillary bicuspids
5. Terminal branches on face:
- Inferior palpebral- Supplies lower eyelid
- External or lateral nasal – Supplies side of the nose
- Superior labial – Supplies upper lip
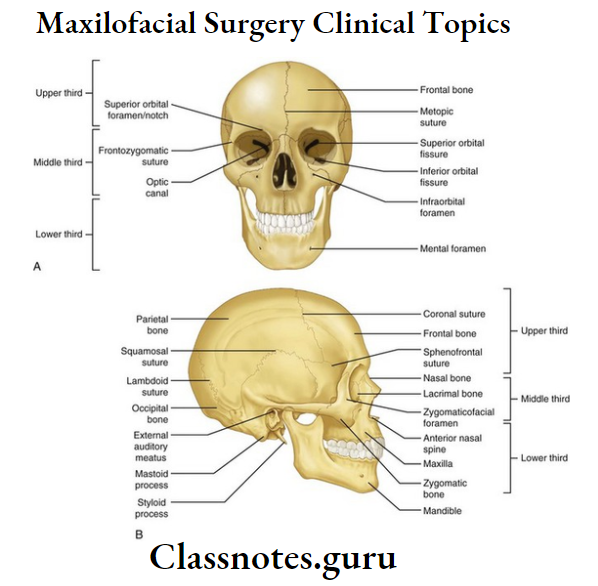
Landmarks Of Posterior Superior Alveolar Nerve Block:
- Zygomatic process of maxilla
- Mucobuccal fold
- infratemporal process of maxilla Coronoid process of mandible
Question 4. Enumerate the course of the mandibular branch of the trigeminal nerve & explain the technique of inferior alveolar nerve block.
Answer:
1. Divided nerve:
- Anterior Division
- External pterygoid
- Masseter
- Temporal
- Buccal
- Posterior
- Inferior alveolar
- Auriculotemporal
- Lingual
2. Undivided nerve:
- Nervus spinosus
- Internal pterygoid
Inferior Alveolar Nerve Block:
- Nerves anesthetized: Inferior alveolar nerve & its branches
- Areas to be anesthetized: Mandibular teeth & its supporting tissues
Landmark of Nerve Block:
- Mucobuccal fold
- Anterior border of coronoid process
- Coronoid notch
- Pterygomandibular raphe
- Retromolar pad
- Retromolar triangle
- External oblique ridge
The technique of Nerve Block:
- Position the patient in a semi-reclined position
- Move your Index finger over the mesiobuccal fold up to the external oblique ridge
- Move it up & down to obtain depression
- This is a coronoid notch Retract the cheek
- Support the mandible
- Insert 1 5/8 inch 25 gauge needle from the lingual side
- Aspirate & Slowly deposit the solution
- Positive Aspiration: 10-15%
Question 5. Describe in detail the extracranial course of the trigeminal nerve.
Answer:
- The trigeminal nerve is the fifth cranial nerve
- It divides into three branches as it proceeds from the convex border of the semilunar ganglion.
Branches of Trigeminal nerve :
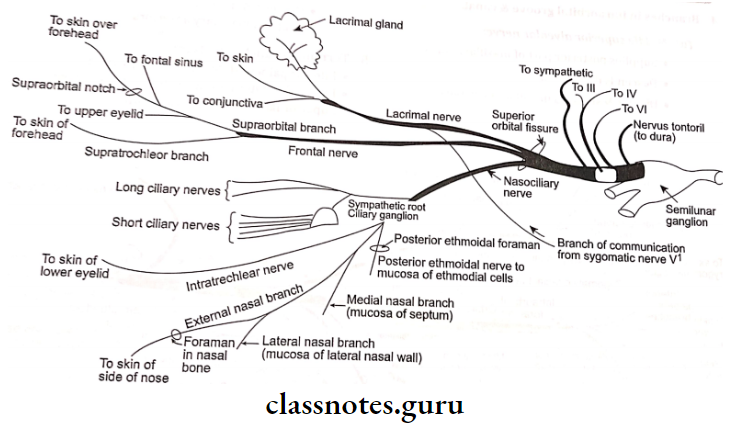
1. Ophthalmic branch:
- Passes upward & enters the orbit through the superior orbital fissure
- It divides into
- Lacrimal branch- supplying the lacrimal gland
- Frontal branch- further divides into
- Supraorbital & Supratrochlear
- Supplies canthus of eye & side of the face
- Nasociliary nerve: Divides into
2. Orbital branches:
- Long ciliary ganglion
- Long ciliary nerve
- Posterior ethmoid- Supply posterior ethmoidal cells & sphenoidal sinus
- Anterior ethmoidal- Supply anterior ethmoidal cells & frontal sinus
- Divides into internal & external nasal
3. Nasal branches:
- Supplies vomer & nasal mucosa
4. Terminal branches on face:
Supplies lower eyelid, upper lip & side of nos
Question 6. Definition, composition & ideal properties of local anesthesia. Describe its mechanism of action.
Answer:
Definition of anesthesia:
It is loss of sensation in a circumscribed area of the body characterized by depression of excitation of nerve endings & inhibition of the conduction process of peripheral nerve
Composition of Anaesthesia:
- Local anesthetic – Ester or amide
- Vasoconstrictor- Epinephrine
- Antioxidant- Sodium metabisulphite
- Preservative- Methylparaben
- Vehicle- Distilled water or Ringer’s lactate solution
Ideal Properties of Anaesthesia:
- Nonirritant
- No permanent damage to the nerve
- Low systemic toxicity
- Effective
- The short onset of action
- Long-lasting effect
- Potent
- Free of allergens
- Stable & biocompactible
- Able to sterilize it
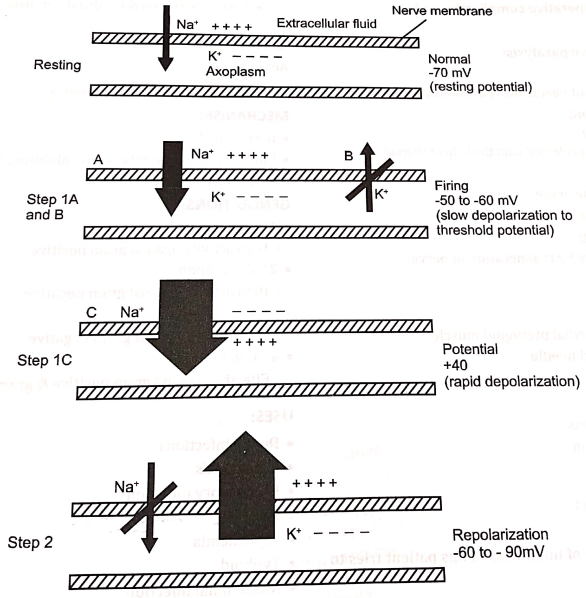
Mechanism Action of Anaesthesia:
- Displacement of calcium ions from sodium channel receptor site which permits
- The binding of the LA molecule to this site produces
- Blockade of the sodium channel & a
- Decrease in sodium conductance, which leads to
- Depression of rate of electrical depolarization
- Failure to achieve the threshold potential level along with a
- Lack of development of propagated action potential which is called
- Conduction blockade
Question 7. Classify local anesthetic drugs. Discuss lignocaine hydrochloride.
Answer:
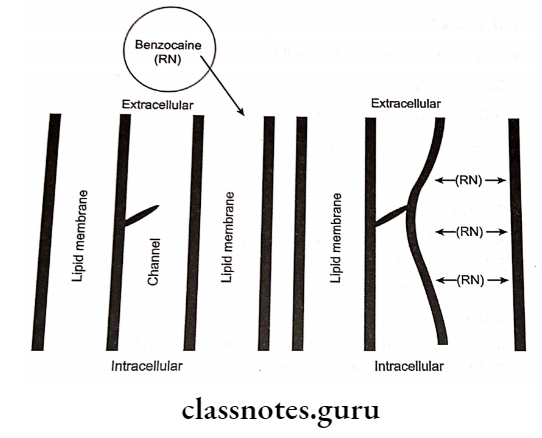
Based on the Site of Action:
- Class 1: Agents acting on the external surface of the membrane
- Example: Biotoxins
- Class 2: Agents acting on the internal surface of the membrane
- Example: Quaternary ammonium compounds
- Class 3: Agents acting by an independent mechanism
- Example: Benzocaine
- Class 4: Agents acting by combination mechanisms
- Example: Articaine, Bupivacaine
Based On Group of Drugs:
- Esters:
- Esters of Benzoic Acids:
- Butacaine
- Cocaine
- Hexylcaine
- Tetracaine
- Esters of Paraamino Acids:
- Chloroquine
- Procaine
- Esters of Benzoic Acids:
- Amides:
- Atricalno
- Bupivacaine
- Etidocaine
- Quinolone:
- Centbucridine
Lidocaine HCL:
- Classification: Amide
- Potency: 2
- Metabolism: Microsomal oxidase
- PKA: 7,9
- pH of plain solution:6.5
- pH of Vasoconstrictor: 5-5.5 Plasma Half-Life 16-hour
- Effective Concentration: 2%
- Maximum Recommended Dose: 7 mg/kg body weight
Question 8. Write about it Indications & contra-indications of local anesthesia.
Answer:
Indications anesthesia:
- Periodontal surgery
- Extraction
- Impaction
- Endodontic procedures Implant placement
- Minor surgical procedures
Contraindications of anesthesia:
- Absolute contraindications:
- Local anesthetic agent allergy
- Bisulfite allergy
- Relative contraindications:
- Liver disorders
- Renal disorders
- Cardiac disorders
- Methemoglubenimela
Question 9. Write in detail about local & systemic complications of local anesthesia.
Or
Post Operative complications of LA
Answers:
Local Complications:
1. Needle breakages:
- Due to the sudden movement of the patient’s Narrow gauge needle
- Broken needle
- Bent needle
Management:
- Due to the sudden move
- Radiograph to locate it
- Expose the site and remove it
2. Facial nerve paralysis
Causes :
- Insertion of needle into the parotid capsule
Management:
- Self-curing
- The eye can be protected with the help of a keypad
3. Paraesthesia:
Cause:
- Injury to the nerve
Management:
- Self-recovery by regeneration of nerve:
4. Trismus:
Cause:
- Trauma to medial pterygoid muscle:
- Contaminated needle
Management:
- Analgesic
- Muscle relaxants
- Hot fomentation
- Physiotherapy
5. Pain on injection:
Cause:
- Blunt needle
- Broader gauge needle
Management:
- Use of short, narrow-gauge needle
6. Burning on injection:
Cause:
- An acidic solution of LA
- Contaminated needle
Management:
- Isotonic solution by addition of bicarbonate
- Use of disposable needle
7. Soft tissue injury:
Cause:
- Due to being unaware of numbness of lips patient tries to do lip-biting
Management:
- Explain to the patient the numbness
- Use of lifeguards in children
8. Hematoma:
Cause:
- Injury to blood vessels
Management:
- Assure of proper anatomy of landmarks & nerve
- Massage the area
- Antibiotics
- Hot fomentation
9. Infection:
Causes:
- Contaminated needle
Management:
- Use of disposable needle
- Antibiotics
- Drainage of space involved
- Physiotherapy
10. Necrosis of tissues:
Causes:
- Seen in palatal injection
- This region is tightly bound to the underlying bone
- Thus excessive pressure is required for the insertion of the needle
- This leads to the blanching of the area
- Vasoconstriction & localized necrosis
11. Edema:
Causes:
- Injury to nerve
- Contaminated needle
Management:
- Subsidies on their own
- Avoid application of hot fomentation
- Application of cold fomentation
- As it acts as vasoconstrictor & analgesic
12. Post anaesthetic lesions:
- Ulcers
- Allergic reactions
Causes:
- Trauma
- Allergy to LA agent
Systemic Complications:
1. Overdose:
Causes of Overdose:
- Excessive dose of LA
- Systemic disorders of metabolism
Features of Overdose:
- Nausea
- Vomiting
- Diplopia
- Tremors
- Acidosis
- Respiratory distress
- Chest pain
- Bradycardia
- Hypotension
- Dizziness
Management of Overdose:
- Reassure the patient Maintain the patient’s airway
- Intubate if necessary
- Cardiac life support given
- IV fluids & vasopressors were given for hypotension
2. Hypersensitivity:
Causes of Hypersensitivity:
- Allergy to LA
- Allergy to preservatives used
Features of Hypersensitivity:
- Pruritis
- Utricaria
- Dyspnoea
- Wheezing
- Nausea, vomiting
Management of Hypersensitivity:
- Stop the procedure
- Mild allergy- Corticosteroids
- Severe allergy- Epinephrine 1: 1000 of 0.3-0.5 ml
- SC If symptoms continue 5 ml of 1: 10000 epinephrine given IV
Question 10. Discuss the metabolism of ester & amide groups of anesthesia.
Answer:
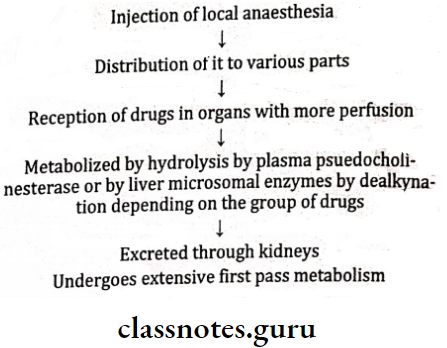
Metabolism Of Ester Group:
- Metabolized by hydrolysis by plasma pseudocholinesterase
- The end product of it is PABA
- If the patient is allergic to it alternative drug is used
- Examples- Cocaine, cocaine, etc.
Metabolism of Amide Group:
- Metabolized in the liver by microsomal enzymes
- Used with caution in patients with liver disease
- Example of enzyme: P-450 3A4
- Example of drugs: Lidocaine
Question 11. Discuss in detail about infraorbital nerve block. Write its landmarks, technique, and complications.
Answer:’
Nerve of Anaesthesize:
- Infraorbital nerve
- Inferior palpebral
- Super labial
Areas of Anaesthesized:
- Maxillary incisors, canines
- Underlying periosteum
- Side of nose Upper lip Lower eyelid
Landmarks of Anaesthesized:
- Mucobuccal fold
- Infraorbital notch Infraorbital foramen
The technique of Anaesthesized:
- Position the patient
- The maxillary occlusal plane must be parallel to the floor
- Palpate infraorbital foramen, below the infraorbital ridge
- Below feel the depression
- Simultaneously retract the upper lip
- Insert a 15/8 inch 25 gauge needle by either placing the
needle parallel to incisors or bisecting - Slowly deposit the solution
- Positive Aspiration: 0.79%
Complications of Anaesthesized:
- Hematoma may develop across the lower eyelid and the tissues between it and the infraorbital foramen
- It is a very rare complication
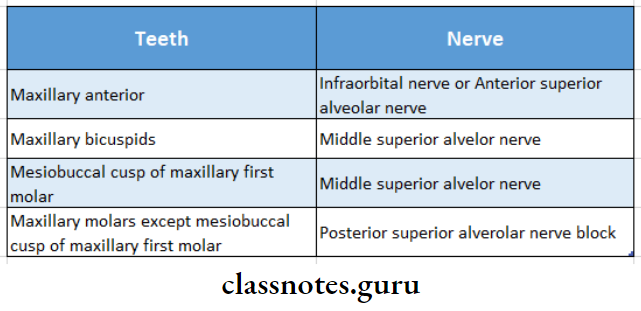
Question 12. Write nerve supply to maxillary teeth.
Answer:
Nerve Supply To Maxillary Teeth:
Symptoms of Maxillary Teeth:
- Subjective: No subjective symptoms
- Objective: Instrumentation demonstrates the absence of pain
Complications of Maxillary Teeth:
- Hematoma
- Produces by inserting the needle too far posteriorly Into the pterygoid plexus
- Varying degrees of mandibular anesthesia
- Produces due to deposition of solution lateral to the desired location
Question 13. Explain In detail the theories and mechanism of action of local anesthesia.
Or
Theories of local anesthetic action
Answer:
Theories of local anesthesia:
- Acetylcholine theory:
- States that besides being a neurotransmitter, it helps the inaction of local anesthetic agent
- It has not proved yet
- Calcium displacement theory:
- States that calcium displaces sodium ions from the receptor site
- But when demonstrated in calcium baths gave false results
- Surface charge theory:
- States that the LA agent binds to the ions on the membrane surface & causes a change in electric potential
- But action of
- LA occurs inside the membrane rather than outside
- Membrane expansion theory:
- LA agents enter the membrane & bind to the hydrophobic groups of the membrane & expand it
- Accepted one
- Specific receptor theory:
- LA binds to the specific receptors present over the sodium channels
Mechanism Of Action:
- Displacement of calcium ions from sodium channel receptor site which permits
- The binding of the LA molecule to this site produces
- Blockade of the sodium channel & a
- Decrease in sodium conductance, which leads to
- Depression of rate of electrical depolarization Failure to achieve the threshold potential level along- with a
- Lack of development of propagated action potential which is called
- Conduction blockade
Clinical Topics Short Essays
Question 1. Classification & indications of corticosteroids.
Answer:
Classification of corticosterolds:
- Short Acting:
- Cortisone
- Hydrocortisone
- Intermediate Acting:
- Prednisolone
- Methylprednisolone
- Long Acting:
- Paramethasone
- Dexamethasone
Indications of corticosterolds:
- Rheumatoid arthritis
- Osteoarthritis
- Eye diseases
- Bronchial asthma
- Collagen diseases
- GIT diseases
- Renal diseases
- Organ transplantation
- Lung diseases
- Malignancies
- Allergic diseases
- Skin diseases
Question 2. Gow gates technique.
Answer:
Nerves To Be Anaesthesized:
- Inferior alveolar nerve
- Mental
- Incisive
- Lingual
- Mylohyoid
- Buccal
- Auriculotemporal
Areas To Be Anaesthesized:
- All mandibular teeth & its associated parts
Landmarks Anaesthesized:
- Extraoral:
- Corner of mouth
- Intertragic notch
- Intraoral:
- Coronoid process
- Maxillary occlusal plane
Technique of Anaesthesized:
- Locate intraoral & extraoral landmarks
- Make the patient open his mouth widely
- Insert needle such that it coincides with extraoral & intraoral landmarks
- The depth of penetration of the needle is increased by at least 3/4th of its length
- Aspirate
- Slowly deposit the solution
Symptoms of Anaesthesized:
- Subjective
- Tingling & numbness in the area
- Objective
- Instrumentation demonstrates the absence of pain
Question 3. Cephalosporins.
Answer:
Cephalosporins
- Group of semisynthetic antibiotics
Mechanism of Cephalosporins:
- Bactericidal
- Inhibits cell wall synthesis by inhibiting transpeptidase enzyme
Generations of Cephalosporins:
- 1st generation
- High activity against gram-positive
- 2nd Generation
- High activity against gram-negative
- 3rdGeneration
- More active against gram-negative
- 4th Generation
- Effective against gram-positive & gram-negative
Uses of Cephalosporin:
- Dental infections
- Prophylaxis
- Respiratory infections
- UTI
- Septicaemia
- Typhoid
- Nosocomial infection
Adverse Reactions of Cephalosporin:
- Pain after injection
- Diarrhea
- Nephrotoxicity
- Bleeding
- Low WBC count
- Disulfiram-like reaction with alcohol
Question 4. Electrophysiology of nerve conduction.
Answer:
Step 1: Excitation
- Initially Slow depolarization:
- Interior of the membrane becomes less negative than the outside
- The rapid phase of depolarization:
- Also called Threshold potential/firing potential
- Reversal of potential:
- Interior becomes more positive i.e. + 40 mV
Step 2: Repolarization outside:
- The interior of the membrane becomes more negative than
- Upto resting potential reaches 70 mV’
Question 5. Metabolism of local anesthesia.
Answer:
Metabolism of local anesthesia
Question 6. Forcep design.
Answer:
Forcep design:
- Forcep is designed in such a way that it delivers teeth from the socket
- Parts: HBeaks, Joint & Handles
- Cross-hatching on handles is present for grip overhand
- Serrations are present interiorly to obtain a grip over the tooth
- Beaks are pushed apically to form a grip
Types of Forcep design:
Type 1:
- Mandibular forceps:
- Beaks are at a right angle to the handles
- Maxillary forceps:
- The beaks are in the same line as the handles
Type 2:
- American forceps:
- The Joint is designed in a horizontal pattern Used for upper extractions
- English type:
- Joint present in a vertical pattern
- Used for lower extractions
Question 7. Role of vasoconstrictors in local anesthetics.
Answer:
Role of vasoconstrictors in local anesthetics
- Actions of vasoconstrictor in local anesthesia.
- By constricting blood vessels, vasoconstrictors decrease blood flow to the site of drug administration.
- Absorption of local anesthetic into the cardiovascular system is slowed resulting in lower anesthetic blood levels.
- Decreases the risk of local anesthetic toxicity.
- Increases duration of action of local anesthetics.
- Decreases bleeding at the site of administration.
Question 8. Ester group of local anesthetic agents.
Answer:
1. Esters of benzoic acids:
- Butacaine
- Cocaine
- Hexylcaine
- Tetracaine.
2. Esters of para-amino acids.
- Chloroquine
- Procaine.
Metabolism of benzoic acids:
- Metabolized by hydrolysis by plasma pseudo-choli-esterase
- The end product of it is PABA
- If the patient is allergic to it alternative drug is used
- Example: Coccaine, procaine, etc.
Clinical Topics Short Question And Answers
Question 1. Eutectic mixture of local anesthesia.
Answer:
Eutectic mixture of local anesthesia
- Topical application of anesthesia
- Contains 2.5% prilocaine & 2.5% lignocaine
Uses of local anesthesia:
- Needle phobic patients
- Painful superficial procedures
- Circumcision
- Leg ulcer debridement
- Gynecological procedures
Contraindications of local anesthesia:
- Methemoglobinaemia
- Infants of less than 12 months may lead to methemoglobinemia
Question 2. Adrenaline.
Answer:
Mode of Action: On α & β adrenergic receptors
Actions:
- ↑ Systolic & diastolic pressure
- ↑ Cardiac output
- ↑ Stroke volume
- ↑ Heart rate
- ↑ Contraction
- ↑ Myocardial oxygen consumption
ADR: Bronchodilation
- Anxiety
- Dizziness
- Headache
- Tremors
- Weakness
Uses of Adrenaline: Allergic reactions
- ↑Depth of anesthesia
- ↑Duration of anesthesia
- Bronchospasm
- Cardiac arrest
- Hemostasis
Question 3. Bupivacaine.
Answer:
Bupivacaine
- Classification: Amide
- Potency: 4 times of lignocaine
- Metabolism: Hepatic amidase
- PKA: 8.1
- pH of plain solution: 4.5-6 pH of
- Vasoconstrictor: 3-4.5
- Plasma Half-Life: 2.7 hours
- Effective Concentration: 0.5%
- Maximum Recommended Dose: 1.3 mg/kg body weight
Question 4. Inferior alveolar nerve block complication.
Answer:
Inferior alveolar nerve block complication
- Transient facial nerve paralysis: If the needle is inserted into the parotid capsule
- Trismus: Due to spasm of medial pterygoid muscle
- Hematoma: Due to injury to vessels
Question 5. Landmarks for extraoral maxillary nerve block.
Answer:
Landmarks for extraoral maxillary nerve block
- The lower border of the zygomatic arch
- Coronoid process of mandible
- Sigmoid notch
- Lateral pterygoid plate
Question 6. Vasoconstrictor./ Use of vasoconstrictor in local anesthesia.
Answer:
Use of vasoconstrictor in local anesthesia
- Actions of Vasoconstrictor in local anesthesia
- By constricting blood vessels, vasoconstrictors decrease blood flow to the site of drug administration
- Absorption of the local anesthetic into the cardiovascular system is slowed resulting in lower anesthetic blood levels
- Decreases the risk of local anesthetic toxicity Increases duration of action of local anesthetics
- Decreases bleeding at the site of administration
Question 7. Posterior superior alveolar nerve block.
Answer:
The technique of nerve block:
- Position the patient
- Area of insertion- Height of mesiobuccal fold above the maxillary second molar
- Retract the patient’s cheek.
- Insert a 27-gauge needle into the height of the mesiobuccal fold over the second molar
- Advance the needle slowly in an upward, inward, and backward direction
- Advance the needle to the desired depth Aspirate in two planes
- Slowly deposit 0.9-1.8 ml of anesthetic solution Slowly withdraw the needle
Clinical Topics Viva Voce
- The posterior portion of the hard palate and overlying structures upto the first premolar on the injected side are anesthetized by greater palatine nerve block
- A decrease in interstitial fluid pH will decrease the effectiveness of a local anesthetic block
- Epinephrine is added to local anesthetics because it decreases the rate of absorption of the local anesthetic at the injection site
- The maxillary branch of the trigeminal nerve passes through the foramen rotundum
- A nerve is refractory during depolarization
- The local anesthetics act on the nerve membrane
- Tachyphylaxis occurs due to repeated use of local anesthesia
- Local anesthetics are excreted through the kidneys
- The rebound phenomenon is most commonly seen with the use of epinephrine
- Bupivacaine is the least toxic local anesthetic
- Bupivacaine is a long-acting local anesthetic agent
- Local infiltration should be para periosteal
- In greater palatine nerve block needle should be perpendicular to the mucosa
- Gow Gates technique is for mandibular nerve block
- The target of the Gow Gates technique is the neck of the condyle
- For extraoral maxillary nerve block, the target area is anterior to lateral pterygoid plate
- Aspiration should be done in at least two planes
- Local anesthetics produce anesthesia by inhibiting the influx of sodium ions through the nerve membrane
- The most potent vasodilator local anesthetic agent is procaine
- Amide type of local anesthetic agents undergo biotransformation primarily in the liver
- Infiltration in the maxillary first molar region is not effective due to zygomatic buttress bone in the region
- The most common complication after surgical removal of a mandibular tooth is
