Infectious Diseases Short Question And Answers
Question 1. Four complications of viral hepatitis
Answer:
Four Complications Of Viral Hepatitis
- Hepatic necrosis
- Chronic hepatitis
- Cirrhosis of liver
- Hepatic failure
- Hepatocellular carcinoma
Question 2. Infectious Mononucleosis
Answer:
Infectious Mononucleosis
- Infectious Mononucleosis is an acute febrile illness associated with lymph node enlargement caused by Epstein Barr virus
- Features
- Affects adolescents and adults
- The incubation period is 7-10 days
- Clinical features
- Fever, malaise
- Conjunctival haemorrhage
- Maculopapular rash
- Sore throat
- Lymphadenopathy
- Splenomegaly
Infectious Mononucleosis Complications
- Chronic fatigue
- Hepatitis
- Hemolytic anemia
- Thrombocytopenia pleurisy
- Myocarditis
- Meningoencephalitis
- Rupture of an enlarged spleen
infectious diseases short questions and answers
Question 3. Rubella
Answer:
Rubella
- Rubella is a mild childhood disease
- Rubella may be acquired congenital or postnatally
Rubella Features:
- Infection is acquired by inhalation
- Incutwbon synod-2-3 weeks
- Fever, malaise
- Headache
- Mild conjunctivitis
- Lymphadenopathy
- Rasa develops on the forehead and face
- Rubella spreads downward to the trunk and extremities
- Rubella lasts for 1-5 days
Read And Learn More: General Medicine Question and Answers
Rubella Prevention:
- Rubella is prevented by MMR vaccine
Question 4. Mumps
Answer:
Mumps
- The incubation period is 12 – 18 days.
Mumps Clinical Features:
- Unilateral (or) bilateral swelling of parotid glands,
- Fever, malaise
- Local pain and tender
- The involvement of extra parotid sites can cause more serious problems as follows.
- CNS involvement may lead to
- Meningitis,
- Meningoencephalitis
- Orchitis
- CNS involvement may lead to
Question 5. Measles
Answer:
Measles Clinical Features:
- Insidious in onset
- Moderate fever
- Tachycardia
- Sore throat
- Formation of greyish-greenish pseudomembrane on tonsils
- Associated nausea and vomiting
- Bull neck- swollen neck
- Tender lymphadenopathy
- Xasal infection
- Hoarseness of voice
- Cough
- Respiratory obstruction
- Toxaemi
- Acute peripheral circulatory failure
- Nerve paralysis
- Dysphagia
- Dysphonia
- Paraesthesia
short Q&A on infectious diseases
Question 6. Prevention of measles
Answer:
Prevention Of Measles
- Active immunization
- One injection of live attenuated measles vaccine along -with mumps and rubella vaccines, MMR vaccine to children over 1 year
- Passive immunization
- Human normal immunoglobulin is used
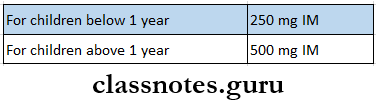
Dose:
Question 7. Diphtheria
Answer:
Diphtheria Clinical Features:
- Diphtheria is insidious at the onset
- Moderate grade fever
- Tachycardia
- Sore throat
- Formation of greyish-greenish pseudomembrane on the tonsils
- Swollen neck- Bull neck
- Tender lymphadenopathy
- Nasal infection
- Hoarseness of voice
- Cough
- Respiratory obstruction
- Acute circulatory failure
- Myocarditis
- Nerve palsies
- Dysphagia
- Dysphonia
- Paraesthesia in the limbs
Question 8. Ascariasis
Answer:
Ascariasis
- Infection caused by Ascaris lumbricoides is known as ascariasis
Ascariasis Features:
- Migrating larvae in the lungs cause dyspnoea, wheezing, cough, and signs of pneumonia
- Loss of appetite
- Malnutrition
- Fever
- Eosinophilic leukocytosis
- Appendicitis
- Liver abscess
Ascariasis Diagnosis:
- Stool examination- demonstrates adult worms or eggs
- Barium meal- Demonstrate adult worms
- Serodiagnosis- detects antibodies
Ascariasis Treatment:
- Pyrantel pamoate-11 mg/kg given orally
- Mebendazole-100 mg twice daily for three days
Question 9. Hookworm Disease
(or)
Ankylostomiasis
Answer:
Hookworm Disease
- Hookworm disease is a symptomatic infection caused by Ankylostoma duodenal and Necatar Ameri- can
- Occurs in all tropical and subtropical countries
Hookworm Disease Clinical Features:
- Dermatitis
- Lesions in the lungs- bronchitis and bronchopneumonia
- Microcytic, hypochromic anemia
- Epigastric pain
- Dyspepsia
- Vomiting
- Diarrhea
Hookworm Disease Diagnosis:
- Blood examination
- Eosinophilia
- Microcytic, hypochromic anemia
- Stool examination
- Shows occult blood
Hookworm Disease Treatment:
- High protein diet
- Oral iron preparations
- Blood transfusion
- Drugs used are- mabendazole, albendazole, pyrantelpamoate
important short questions in infectious diseases
Question 10. Amoebic dysentery
Answer:
Amoebic Dysentery
- Amoebic dysentery is also known as intestinal amoebiasis
- Amoebic dysentery is a condition in which the infection is confined to the intestine and is characterized by the passage of blood and mucus in the stool
Amoebic dysentery Types:
- Acute amoebic dysentery
- Multiple ulcers occur
- These ulcers are deep and extensive
- Its complications are
- Pericaecal and pericolic abscess
- Amoebic appendicitis
- Perforation
- Generalized peritonitis
- Gangrene of guts
- Fistula
- Chronic amoebic dyssentery
- A single latent ulcer is present in the caecum while multiple small superficial ulcers are scattered throughout the large intestine
- Stricture formation occurs
- Amoeboma in the caecum and large intestine develops
Question 11. Treatment of malaria
Answer:
Treatment Of Malaria
- General management
- Use of analgesics and antipyretics to treat fever
- Administration of intravenous fluids
- Treatment of acute attack
- Chloroquine-600 mg followed by 300 mg in 6 hours and then 150 mg twice a day for 3 days
- Chloroquine-resistant cases- Dihydrochloride 600 mg salt three times a day by mouth for 5 days
- Followed by a single dose of sulphadoxine 1.5 g combined with pyrimethamine 75 mg
Question 12. Complication of malaria
Answer:
Complication Of Malaria
- Pernicious malaria
- Black water fever.
1. Pernicious Malaria:
- Pernicious Malaria is a life-threatening condition
Pernicious Malaria Cause:
- Pernicious Malaria is due to heavy parasitization.
Pernicious Malaria Clinical Features:
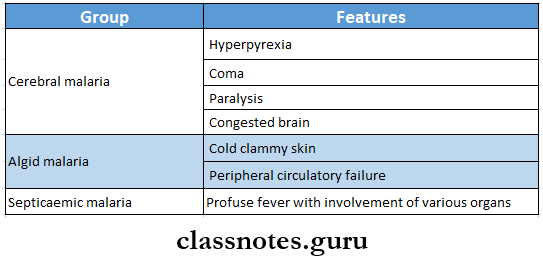
- Pernicious Malaria is grouped into the following:
2. Blackwater Fever:
- This occurs in persons who are previously infected and had inadequate doses of quinine
Blackwater Fever Clinical Features:
- Intravascular hemolysis,
- Fever,
- Haemoglobinuria
- Vomiting and prostration with the passage of dark red (or) blackish urine hence called backwater fever.
Blackwater Fever Mechanism:
- An autoimmune mechanism may be involved in hemolysis
- Parasitized erythrocytes during previous infection act as antigen
- Antibodies are formed against it
- Due to this antigen-antibody reaction, massive destruction of erythrocytes occurs
- There is excessive deposition of haemosiderin pigment in the liver, spleen, and kidneys.
- Sequel of black water fever include
- Circulatory failure
- Renal failure,
- Liver failure,
- Anaemia.
Question 13. Complication of mumps
Answer:
Complication Of Mumps
- Orchitis
- Oophoritis
- Arthritis
- Nephritis
- Pancreatitis
- Thyroiditis and myocarditis.
infectious disease viva questions and answers
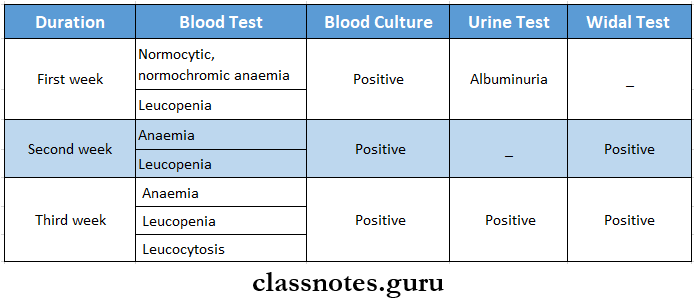
Question 14. Diagnosis of typhoid fever
Answer:
Diagnosis Of Typhoid Fever
Question 15. Complications of typhoid fever
Answer:
Complications Of Typhoid Fever
- Intestinal complications
- Hemorrhage
- Paralytic ileus
- Perforation
- Peritonitis
- Extraintestinal complication
- Meningitis
- Cholecystitis
- Pneumonia
- Myocarditis
- Bone and joint infection
- Encephalopathy
- Granulomatous hepatitis
- Nephritis
Question 16. Clinical features of typhoid fever
Answer:
Clinical Features Of Typhoid Fever
- Incubation period- 10-14 days
- First 5-7 days
- High-grade, remittent fever with chills
- Headache
- Aches
- Malaise
- Constipation
- Leucopenia
- Dry cough
- Epistaxis
- Relative bradycardia
- Between 1st and 2nd week
- Rose spots develop over the trunk as small macules, red in color, and blanch on pressure
- Splenomegaly
- Bronchitis
- Abdominal pain
- Abdominal distension
- Diarrhea
- After 2nd week
- Confusion
- Delirium
- Toxaemia
- Coma
Question 17. Lepromatous leprosy
Answer:
Lepromatous Leprosy
- Leprosy caused by mycobacterium leprae is of 2 types wepromatous leprosy represents low resistance and tuberculoid leprosy represents high resistance.
- Lepromatous leprosy is characterized by multiple symmetrical skin lesions that are hypopigmented and erythematous maculopapular/nodular.
- Nerve involvement is present with less severe sensory distribution.
- Histopathology involves the collection of foamy macrophages/lepra cells in the dermis separated from the epidermis by a clear zone.
Question 18. Lepra reaction
Answer:
Lepra Reaction
- Lepra reaction/reactional leprosy:
- There may be two types:
- Type 1 (Reversal reactions),
- Type 2 (Erythema, nodosum leprosum)
1. Type 1: the polar forms of leprosy donor undergo any change in clinical ami histopathological picture.
- Borderline groups are unstable and may move across the spectrum in either direction with upgrading/downgrading of patients’ immune stale.
- Upgrading Read Ion: Characterized by increased cell-mediated immunity and occurs in patients of borderline Icpromalous (BL) type on treatment who upgrade/shift towards tuberculoid type.
- Downgrading Reaction: Characterized by lowering of cellular immunity and is seen in borderline tuberculoid (BT) type who downgrade/shift towards Icpromalous type.
2. Type 2: Occurs in Icpromalous patients after treatment. It is characterized by tender cutaneous nodules, fever, iridocyclitis, synovitis, and lymph node involvement.
Short questions on bacterial and viral infections
Question 19. Diagnosis of AIDS
Answer:
Tests for AIDS:
- ELISA( Enzyme-Linked Immunosorbent Assay)
- It is a color reaction test
- Method:
- A serum containing antibodies is developed from the patient’s blood sample
- Tests for AIDS is added to the ELISA plate
- Wash off the inactive antibodies
- A second layer of antibodies called conjugate is added
- Excess antibodies are again washed off
- A substrate is added to it
- Result:
- Color becomes darker- positive test
- No color change- negative test
- Western blot
- Method
- Viral proteins from the patient’s blood sample are passed through a gel
- The separated proteins are then passed through an electric current
- Human serum is added
- A chromogen is added to it
- Method
- Result:
- A specific band of viral protein is detected
Question 20. Quinolones
Answer:
Quinolones
- Quinolones are a group of synthetic antimicrobial agents
Quinolones Uses:
- Uncomplicated UTI
- Diarrhea
Quinolones Adverse Effects:
- Hemolytic anemia
- Allergic reactions
- Headache
- Myalgia
- Drowsiness
Examples:
- Nalidixic acid
- Oxalinic acid
- Cinoxacin
Question 21. Cephalosporins
Answer:
Cephalosporins
- Cephalosporins are semi-synthetic antibiotics with a beta-lactam ring
Cephalosporins Uses:
- Gram-negative infections
- Surgical prophylaxis
- Gonorrhea
- Meningitis
- Mixed aerobic and anaerobic infection
- Typhoid
- Nosocomial infection
- Orodental infection
Cephalosporins Adverse Reactions:
- Hypersensitivity reactions
- Nephrotoxicity
- Diarrhea
- Bleeding
- Low WBC count
- Pain at the injection site
- Disulfiram like reaction
Question 22. Triple vaccine, Dan PT
Answer:
Triple Vaccine, DPT
- DPT is used as an active immunization
- Triple vaccine, DPT is combination of Diphtheria toxoid, pertusis vaccine and tetanus toxoid
DPT Route Of Administration:
- Intramuscular
DPT Dose:
- Initial dose- 6 weeks
- Three doses are completed at intervals of 4-6 weeks
- Booster doses-18 months and 5 years
DPT Adverse Reactions:
- Transient local inflammation
- Fever
- Occthe asional convulsions
DPT Advantages:
- Minimizes the number of injections
- Improves immune response
Question 23. Anti-amoebic drugs
Answer:
Anti-Amoebic Drugs
- Anti-amoebic drugs are drugs used in amoebiasis
Anti-Amoebic Drugs Classification:
- Drugs effective in both intestinal and extra-intestinal amoebiasis
- Metronidazole
- Tinidazole
- Secnidazole
- Omid azole
- Satranidazole
- Emetine
- Drugs effective in intestinal amoebiasis
- Diloxanide furoate
- Quiniodochlo
- Iodoquinol
- Tetracyclines
- Drugs effective in extraintestinal amoebiasis
- Chloroquine
Question 24. Quinsy
Answer:
Quinsy
- Quinsy is an infection in connective tissue between the tonsil and the superior constrictor
- Quinsy is also called peritonitis sellar abscess
Quinsy Fethe Features:
- Acute pain in the throat
- Pain radiates to the ear
- Dysphagia
- Nausea
- Constipation
- Poor oral hygiene
- Body ache
- Headache
- Enlarged lymph nodes
- Dyspnoea
- Trismus
- Deviation of uvula
- Hoarseness of voice
- Foul breath
Quinsy Management:
- Antibiotics
- Incision over the most prominent part
- Analgesics
- Warm saline gargles 4 fluids
- Tonsillectomy
Infectious Diseases Short Case Questions
Question 25. Rabies prevention
Answer:
Rabies Prevention
- Rabies vaccines are two types
- Neural
- Non-neural
1. Neural Vaccines:
- Semple vaccine:
- The most widely used vaccine
- Developed by Semple at Central Research Institute, Kasauli.
- It is a 5% suspension of infected sheep brain and inactivated by 5% phenol at 37°C leaving no residual live virus.
- Beta Propiolactone (BPL) Vacine:
- Modified sample vaccine
- Instead of phenol, BPL is used as an activating agent.
- Infant brain vaccine:
- Used widely in America to Reduce neurological complications.
- Vaccination Schedules:
- Nowadays it’s not used.
- In the past, they were given subcutaneously on the anterior abdominal wall.
- 7 – 14 injections depend on the degree of risk.
- Vaccination Schedules:
- Used widely in America to Reduce neurological complications.
2. Non-Neural Vaccines:
- Duck Egg Vaccine:
- BPL is used as an inactivating agent
- It has poor immunogenicity so not used now.
- Tissue culture vaccines:
- Following cell culture vaccines are available in India.
- Human diploid cell strain vaccine [HDCS]
- The HDCS vaccine is prepared by growing rabies virus on human diploid cells and is inactivated with BPL.
- This vaccine is highly antigenic and free of side effects
- Human diploid cell strain vaccine [HDCS]
- Purified chick embryo cell vaccine [PCEC]
- PCEC is now widely used.
- It is cheaper
- It contains BPL inactivated flurry LEP strain
- Purified Vero cell vaccine [PVC]
- This vaccine is under study
- Following cell culture vaccines are available in India.
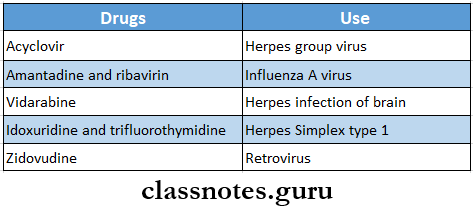
Question 26. Antiviral drugs
Answer:
Antiviral Drugs
Question 27. BCG
Answer:
BCG
- The Bacille Calmette Guerin (BCG) vaccine was prepared by Calmette and Guerin in 1921
- Used for protection against tuberculosis infections
BCG Forms:
- Liquid form
- Freeze-dried form- commonly used
Dose and Administration:
- 0.1 ml is administered intradermally soon after birth
BCG Result:
- A small nodule develops at the injection site in about 2-3 weeks
- it gradually increases in size upto 441 mm in diameter
- It breaks into a shallow ulcer leaving a 4-8 mm diameter round scar
BCG Contraindications:
- AIDS patients
- Eczema
- Pertussis
- Measles
- Patients on steroids
Question 28. Complications of Hepatitis B
Answer:
Complications Of Hepatitis B Are:
- Cirrhosis of liver
- Liver failure
- Hepatocellular carcinoma
Question 29. Chloroquine
Answer:
Chloroquine
- Chloroquine is antimalarial drug
- Chloroquine is a synthetic 4-arninoquinolone
Chloroquine Uses:
- Malaria
- Extra-intestinal amoebiasis
- Photogenic reactions
- Lepra reactions
Chloroquine Adverse Reactions:
- Severe nausea and vomiting
- Pruritis
- Headache
- Visual disturbances
- Insomnia
- Skin rashes
- Cardiomyopathy
- Peripheral neuropathy
- Psychiatric problems
- Blurring of vision
- Confusion
- Bleaching of hair
Question 30. Human insulins
Answer:
Human Insulins
- Human insulin is produced by recombinant DMA technology
- They are expensive
- Absorbed rapidly
Human Insulins Forms:
- Regular B Lente
- Isophane insulin
- Lente
- Ultralente preparations
Human Insulins Advantages:
- Less antigenic
- More stable
- Fewer chances of resistance
- Less chances of lipodystrophy
Human Insulins indications:
- Allergy to conventional preparations
- Insulin resistance
- Lipodystrophy at the injection site
- Pregnancy
Infectious Diseases Important One Liners
Question 31. Four causes of lymphadenopathy
Answer:
Lymphadenopathy Causes:
- Inflammatory
- Acute lymphadenitis
- Chronic lymphadenitis
- Granulomatous lymphaleukemiaeoplastic
- Benign
- Malignant
- Lymphatic leukemia
- Autoimmune disorders
- Juvenile rheumatoid arthritis
- Collagen diseases like systemic lupus erythematosus, polyarteritis nodosa
- Generalised lymphadenopathy
- Tuberculosis
- Syphilis- secondary stage
- Infectious mononucleosis
- Sarcoidosis
- Toxoplasmosis
- Hodgkin’s disease
- Lymphosarcoma
