Infectious Diseases Long Essays
Question 1. What is the differential diagnosis of ulcers over the penis? How do you treat syphilis?
Answer:
Differential Diagnosis Of Ulcers Over Penis:
- Chancre
- Chancroid
- lymphogranuloma venereum
- Genital herpes
- Neoplasm
Syphilis:
- Syphilis is a sexually transmitted disease
Syphilis Clinical Features:
- Primary syphilis
- Incubation period- about 21 days
- Chancre develops
- Syphilis is a solitary, painless, indurated, non-tendered, ulcerated, or eroded lesion
- Initially, it was a dull red macule
- Later it becomes ulcerated
- Regional lymphadenopathy
- Secondary syphilis
- Appears about 6-8 weeks
- Skin lesions appear as macules, papules, fol-locules, or, papulosquamous patches
- Circinate lesions develop on the face
- Headache
- Fever, anorexia
- Joint and muscle pain
- Laryngitis, pharyngitis
- Generalised lymphadenopathy
- Lesions develop over the mucocutaneous junction
- Tertiary syphilis
- Develops about 5-10 years after primary infection
- Affects the skin, central nervous system, CVS, mucous membrane
- Lesions are called gumma
- Tertiary syphilis is localized, chronic granulomatous lesion with a nodular or ulcerated surface
- Causes generalized paresis, dementia, and strokes
- Bone lesions cause osteomyelitis and destruction of joints
infectious diseases long essay questions
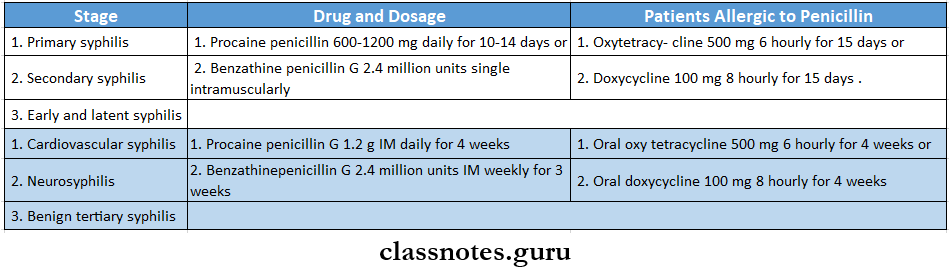
Syphilis Treatment:
Question 2. Describe clinical features, diagnosis, complications, and management of typhoid fever.
(or)
Discuss the etiology, clinical features, complications, and management of enteric fever.
Answer:
Typhoid Or Enteric Fever:
- Typhoid is an acute systemic illness
Etiology:
- Salmonella typhi
- Salmonella paratyphi
Enteric Fever Clinical Features:
- Incubation period- 10-14 days
- First 5-7 days
- High-grade, remittent fever with chills
- Headache
- Aches
- Malaise
- Constipation
- Leucopenia
- Dry cough
- Epistaxis
- Relative bradycardia
- Between 1st and 2nd week
- Rose spots develop over the trunk as small macules, red in color, and blanch on pressure
- Splenomegaly
- Bronchitis
- Abdominal pain
- Abdominal distension
- Diarrhea
- After 2nd week
- Confusion
- Delirium
- Toxaemia
- Coma
Read And Learn More: General Medicine Question and Answers
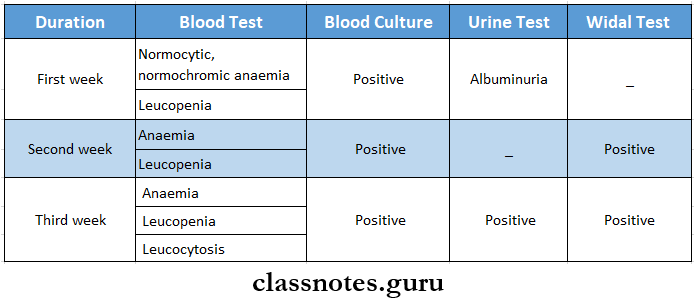
Enteric Fever Diagnosis:
Enteric Fever Complications:
- Intestinal complications
- Hemorrhage
- Paralytic ileus
- Perforation
- Peritonitis
- Extraintestinal complication
- Meningitis
- Cholecystitis
- Pneumonia
- Myocarditis
- Bone and joint infection
- Encephalopathy
- Granulomatous hepatitis
- Nephritis
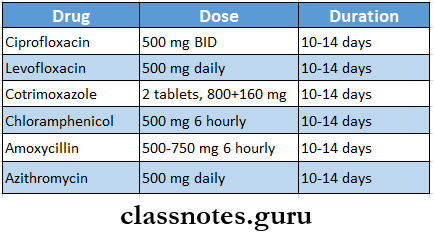
Enteric Fever Management
long essays on communicable diseases
Question 3. Describe the etiology, pathology, clinical features, and management of cervical TB lymphadenitis.
Answer:
Tuberculous Lymphadenitis:
- Tuberculous Lymphadenitis is defined as achronic specific granulomatous inflammation with caseation necrosis of the lymph node
Etiology:
- Mycobacterium tuberculosis complex which includes M. tuberculosis, M. bovis, M. africanum, M. canetti, and M.caprae
Pathology:
- Pathological stages of the disease are:
- Stage 1- lymphoid hyperplasia
- Formation of tubercles and granulomas occurs without cassation necrosis
- Stages 2 and 3
- Caseation necrosis in the affected lymph nodes occurs
- It is followed by the destruction of capsules of lymph nodes
- Periadenitis
- Stage 4
- There is a rupture of caseous material into the surrounding soft tissue
- Formation of abscess cavity
Tuberculous Lymphadenitis Clinical Features:
- Persistent, painless swelling of the lymph nodes
- Release of discharge of fluid
- Fever
- Weight loss
- Fatigue
- Night sweats
tuberculous LymphadenitisManagement:
- Anti-tubercular therapy
- Isoniazid, Rifampicin, Pyrazinamide, and Ethambutol are given for 2 months
- Followed by Isoniazid and Rifampicin for the next 4 months
- DOTS therapy
- Surgery- indicated in
- Persistent fluctuant lesions
- Failure with chemotherapy
- Symptomatic relief
Question 4. Describe the etiology, clinical features, and management of intestinal amoebiasis.
Answer:
Intestinal Amoebiasis
Caused by entamoeba histolytic
- E. histolytica can cause two types of pathological lesions as follows
1. Primary (or) Intestinal Amoebiasis:
- This condition is called amoebic dysentery.
- These ulcers may be generalized (or) may be localized to the ileocaecal (or) sigmoidorectal region.
- Occasionally ulcers may involve deeper tissues and cause perforation (or) peritonitis.
- Erosion of blood vessels may lead to bleeding.
- The superficial lesions generally heal without scarring.
- Deep ulcers form scars leading to strictures, partial obstruction, and thickening of the gut wall.
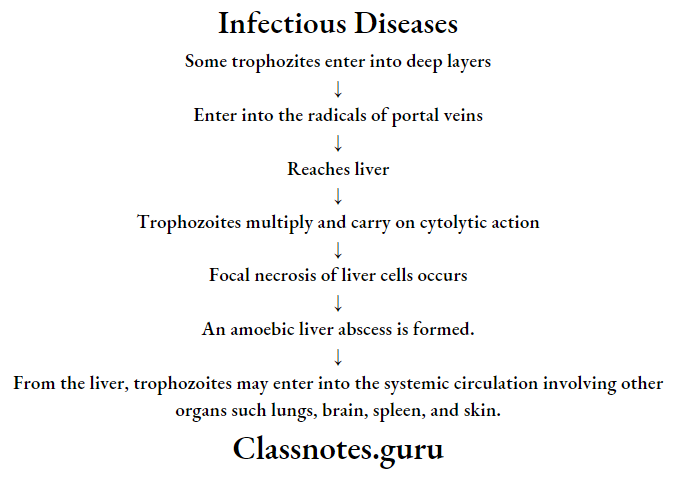
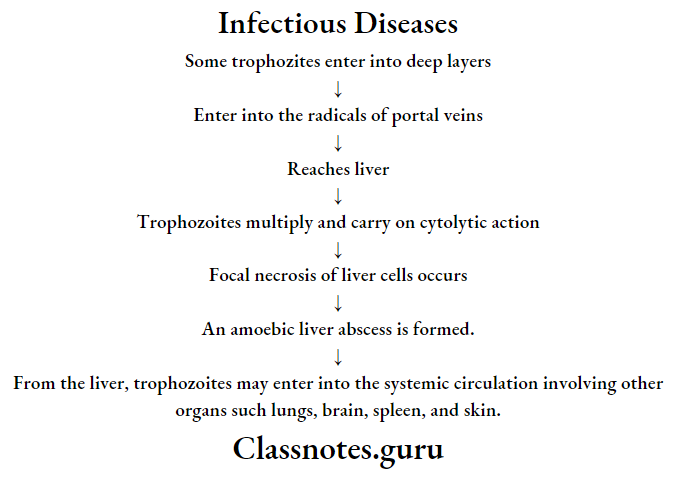
2. Extra-intestinal amoebiasis (or) secondary (or) metastatic lesions.
- Amoebic liver abscess:
long answer questions on infectious diseases
Question 5. Diphtheria etiology, Clinical Feature Management
Answer:
Etiology:
- Etiology is caused by Corynebacterium diphtheria
Diphtheria-etiology Clinical Features:
- Diphtheria-etiology is insidious at the onset
- Moderate grade fever
- Tachycardia
- Sore throat
- Formation of greyish-greenish pseudomembrane on the tonsils
- Swollen neck- Bull neck
- Tender lymphadenopathy
- Nasal infection
- Hoarseness of voice
- Cough
- Respiratory obstruction
- Acute circulatory failure
- Myocarditis
- Nerve palsies
- Dysphagia
- Dysphonia
- Paraesthesia in the limbs
infectious diseases long essays for mbbs
Diphtheria-Etiology Management:
- Antitoxin diphtheric serum (ADS)
- The dose varies from 20,000 to 1,00,000 units depending on the duration and severity of the disease
- In mild cases, a lesser dose may be used
- Antibiotics
- Penicillin G-6,00,000 units every 12 hourly intravenously or
- Amoxycillin 500 mg 8 hourly for 7-10 days
- Patient allergic to penicillin
- Erythromycin- 500 mg 6 hourly or
- Azithromycin 500 mg daily or
- Rifampicin 600 mg daily
- Tracheostomy
