Endocrine And Metabolic Diseases Important Notes
- Acromegaly:
- GH excess after epiphyseal closure results in acromegaly
- Clinical features:
- Skin thickening
- Enlarged nose and tongue
- Macroglossia
- Carpal tunnel syndrome
- Large hands and feet
- Prognathic lower jaw
- Diabetes mellitus
- Hypertension
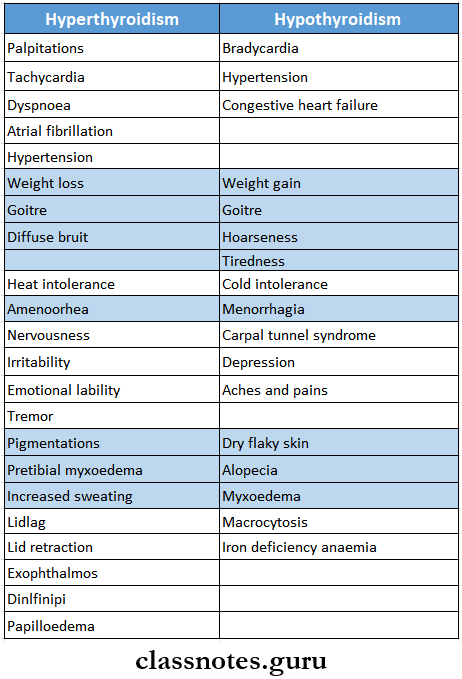
- Thyroid Storm/ Thyrotoxic Crisis, Thyrotoxicosis
- Thyroid Storm is an acute life-threatening hypermetabolic state induced by the excessive release of thyroid hormones
- Clinical features
- Fever
- Heat intolerance
- Exophthalmos
- Tachycardia
- Increased appetite
- Excessive Sweating
- Weight loss
- Systolic hypertension
- Cardiac arrhythmias
- Diabetes Mellitus
- Features
- Polyuria, polyphagia, polydipsia
- Glycosuria
- Ketoacidosis
- Kussmaul breathing
- Circulatory shock, coma
- Bone resorption, loosening of teeth
- Acetone breath
- Types
- Type 1 (Insulin-Dependent Diabetes Mellitus)
- Occurs in young age groups
- Occurs due to deficiency of insulin
- Destruction of beta cells during autoimmune diseases
- Destruction of beta cells by viral infection
- Congenital disorder
- Associated with acidosis ketosis or coma
- Type 2 (Non-Insulin-Dependent Diabetes Mellitus)
- Occurs after the age of 40 years
- Also called maturity-onset diabetes
- The structure and functions of beta cells are normal
- Occurs due to a reduced number of insulin receptors
- Associated with obesity and hereditary
- Rarely, associated with ketosis
- Type 1 (Insulin-Dependent Diabetes Mellitus)
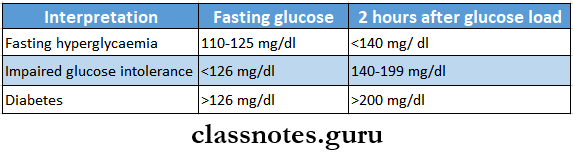
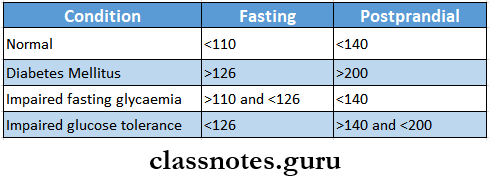
- Diagnosis
- Fasting blood sugar > 126 mg/ dl or random blood sugar > 200 mg/dl is suggestive of diabetes
- Features
- Blood Glucose Test
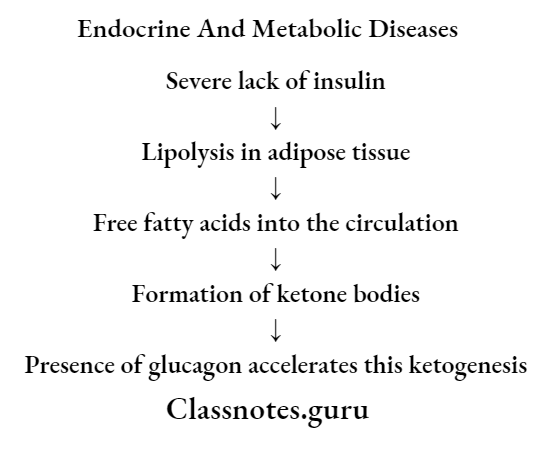
- Cardinal Features Of Diabetic Ketoacidosis
- Hyperglycaemia
- Hyperketonaemia
- Metabolic acidosis
- Hyperthyroidism And Hypothyroidism
- Hypoglycemia-Features
- Sweating
- Palpitation
- Hunger
- Confusion
- Drowsiness
- Incoordination
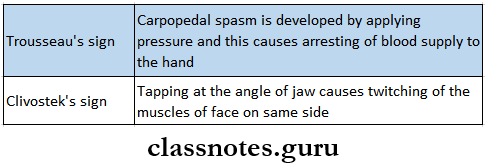
- Tetany
- Occurs when plasma calcium level falls below 6 mg%
- Signs of Tetany
- Risk Factors Of Osteoporosis
- Diet or calcium intake
- Immobility
- Thyrotoxicosis, hyperparathyroidism
- Rheumatoid arthritis
- Corticosteroids
- Smoking and alcoholism
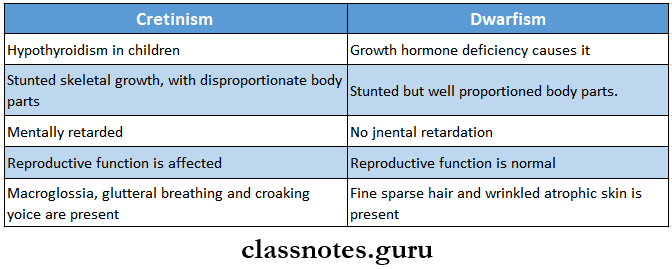
- Cretinism And Dwarfism
endocrine system short questions and answers
Endocrine And Metabolic Diseases Short Answers
Question 1. Tetany
Answer:
Tetany
- Tetany is a clinical condition characterized by low levels of ionized calcium leading to increased neuromuscular excitability
Tetany Clinical Features:
- In children
- Characteristic triad- carpopedal spasm, stridor and convulsion
- Carpopedal spasm- flexion at metacarpophalangeal joints and extension at interphalangeal joints with the opposition of the thumb
- Stridor- closure of glottis
- In adults
- Tingling sensation in peripheral parts of limbs or around the mouth
- Painful carpopedal spasm
- Rarely stridor and convulsions
- Signs
- Trousseau’s sign
- Raising the blood pressure above systolic level by inflation of the sphygmomanometer cuff produces carpal spasm within 3-5 minutes
- Chvostek’s sign
- A tap at the facial nerve at an angle of the jaw produces twitching of facial muscles
- Trousseau’s sign
Read And Learn More: General Medicine Question and Answers
Question 2. Causes Of Tetany
Answer:
Causes Of Tetany
- Hypocalcaemia
- Malabsorption
- Osteomalacia
- Hypoparathyroidism
- Chronic renal failure
- Acute pancreatitis
- Alkalosis andhypokalaemia
- Repeated vomiting
- Excessive intake of alkalies
- Primary hyperaldosteronism
- Hypomagnesaemia
Question 3. Treatment Of Tetany
Answer:
Treatment Of Tetany
- Treatment of hypocalcemia
- Injection of 20 ml of 10% calcium gluconate
- Treatment of alkalosis
- Intravenous administration of isotonic saline
- Withdrawal of alkalies
- Inhalation of 5% C02 in oxygen- to treat hyperventilation
- Psychotherapy
Endocrine Disorders Short Answer Questions
Question 4. Diabetes mellitus-complications
Answer:
Acute Metabolic Complications:
- Diabetic ketoacidosis
- Develop in patients with severe insulin deficiency
- Clinical Features:
- Nausea, vomiting, anorexia
- Deep and fast breathing
- Mental confusion
- Coma
- Hyperosmolar hyperglycemia non-ketotic coma
- It is a complication of type 2 diabetes mellitus
- Caused by severe dehydration which leads to sustained hyperglycemia diuresis
- Hypoglycaemia
- Develop in type 1 diabetes mellitus
Late Systemic Complications:
- Atherosclerosis
- Common in both type 1 and type 2 diabetes mellitus
- Atherosclerosis may lead to Myocardial in fraction cerebral stroke
- Gangrene of toes and feet
- Diabetic microangiopathy
- It is the basement membrane thickening of small blood vessels and capillaries of different organs and tissues
- Occurs due to increased glycosylation of hemoglobin and other proteins
- Diabetic nephropathy
- It is a severe complication of diabetes mellitus
- Occurs in both types
- Diabetic neuropathy
- Effects all parts of the nervous system
- Diabetic retinopathy
- It is the cause of blindness
- Infections
- Diabetic patients are more susceptible to infections like tuberculosis, pyelonephritis, otitis, carbuncles, and diabetic ulcers
Question 5. Oral complications of diabetes mellitus
Answer:
Oral Complications Of Diabetes Mellitus
- Periodontium
- Alter response of the periodontal lesion to local irritants
- Retards healing of tissues
- GCF contains more glucose
- Periodontal abscess formation
- Tooth mobility
- Severe and rapid bone resorption
- Tongue
- Altered taste sensation
- Median rhomboid glossitis
- Impaired local immune response
- Decreased Langerhans cell
- Oral candidiasis
- Alveolar bone
- Localized osteitis
- Mouth
- Burning mouth syndrome
- Dvsgeusia
- Dysesthesia
- Xerostomia
- Increased caries activity
- Diabetic siaiadenosis- involving trigeminal nerve
- Angular cheilosis
- Oral lichen planus
Question 6. Diagnosis of diabetes mellitus
Answer:
Diagnosis Of Diabetes Mellitus
- Detection of glycosuria
- It is detected by a dipstick test
- The green color indicates urinary glucose concentration between 10-20 mg% or more
- Urine for ketone bodies
- Ketonuria indicates diabetes
- Oral glucose tolerance test
- Advise tire patient to take an unrestricted carbohydrate diet for 3 days before the test
- Overnight fast
- Collect a fasting sample of blood
- Administer 75 g of glucose dissolved in 300 ml of water
- Collect blood and urine samples at half-hour intervals for 2 hours
Short questions on metabolic disorders
Question 7. Glucosuria
Answer:
Glucosuria
- Glucosuria is the condition of glucose excretion in urine
- Glucose appears in urine when the plasma glucose concentration exceeds the renal threshold for glucose
Glucosuria Types:
- Renal glycosuria
- It is a benign condition
- Occurs due to a reduced renal threshold for glucose
- It is unrelated to diabetes
- Alimentary glllucosuria
- In certain individuals, blood glucose rapidly increases after meals which gets excreted in urine
- This is known as alimentary glucosuria
- It is observed in
- Normal individuals
- Individuals with
- Hepatic diseases
- Hyperthyroidism
- Peptic ulcer
Question 8. Insulin
Answer:
Insulin
- Insulin is a hormone required for the regulation of blood glucose level
Insulin Secreted By:
- Beta cells of the islets of Langerhans of the pancreas
- Functions:
- Lowers blood glucose level
- Promotes glucose utilization and storage
- Inhibits glucose production
- Required for glucose uptake
- Increases glycolysis
- Decreases gluconeogenesis
- Promotes lipogenesis from glucose
- Reduces lipolysis and ketogenesis
- Enhances protein synthesis
Question 9. Oral hypoglycaemic drugs
Answer:
Oral Hypoglycemic Drugs Classification:
- Sulphonylureas
- First generation
- Tolbutamide
- Chlorpropamide acetohexamide
- Tolazamide
- Second generation
- Clibendamide
- Glipizide
- Gliclazide
- First generation
- Biguanides- Metformin
- Meglilinides- repaglinide, nateglinide
- 4.Thiazolidinediones- Troglitazone, rosiglitazon
- Alpha-glucosidase inhibitors- Acarbose, miglitol
- Newer drugs
- Amylin analog- pramlintide
- GLP-1 analog- exenatide
- DPP-4 inhibitor- Sitagliptin
Oral Hypoglycemic Drugs Features:
- They are used in mild and early non-insulin-dependent diabetes mellitus
- Oral Hypoglycemic Drugs lowers blood glucose levels
- They are noninvasive drugs
Question 10. Sulphonylurea
Answer:
Sulphonylurea
- Sulphonylurea were the first oral hypoglycaemic drugs
Sulphonylurea Classification:
- First generation
- Tolbutamide
- Chlorpropamide acetohexamide
- Tolazamide
- Second generation
- Glibenclamide
- Glipizide
- Gliclazide
Sulphonylurea Mechanism of Action:
- Sulphonylurea reduces the blood glucose levels by:
- Stimulating the release of insulin from the pancreatic beta cells
- Increasing the sensitivity of peripheral tissues to insulin
- Increases the number of insulin receptors
- Suppresses hepatic gluconeogenesis
- Stimulating the release of insulin from the pancreatic beta cells
endocrine system viva questions with answers
Question 11. Metformin
Answer:
Metformin
- Metformin is biguanide
Metformin Mechanism of Action:
- Suppresses hepatic gluconeogenesis
- Inhibits glucose absorption from the intestines
Metformin Use:
- In obese patients with type-2 diabetes mellitus either alone or in combination with sulphonylureas
Metformin Adverse Effects:
- Nausea
- Diarrhea
- Metallic taste
- Mild lactic acidosis
- Anorexia
- Loss of appetite
Question 12. Glibenclamide
Answer:
Glibenclamide
- Glibenclamide is second generation sulphonylurea
Glibenclamide Mechanism of Action:
- Glibenclamide reduces the blood glucose levels by:
- Stimulating the release of insulin from the pancreatic beta cells
- Increasing the sensitivity of peripheral tissues to insulin
- Increases the number of insulin receptors
- Suppresses hepatic gluconeogenesis
- DOSE- 5-15 mg
- HALF-LIFE- 4-6 hours
- DURATION OF ACTION-18-24 hours
Question 13. Treatment of diabetic ketoacidosis
Answer:
Treatment Of Diabetic Ketoacidosis
- Correction of hyperglycemia
- Administration of regular insulin 0.1 U/kg bolus followed by 0.1 U/kg/hour by continuous 4 infusion till the patient recovers
- Correction of dehydration
- Normal salinelitersion of 1 litre m the first hour
- Then 1 litre over the next 4 hours
- Then quantity is titrated
- Correction of acidosis
- Use of sodium bicarbonate
- Potassium
- 10-20 mEq/ hour potassium chloride is added to the drip for rapid correction of hyperglycemia
Question 14. Prevention of tetanus
Answer:
Prevention Of Tetanus
- Surgical
- Removal of foreign bodies, blood clots
- Cleansing
- Radical excision
- Antibiotics
- Long-acting penicillin injection or erythromycin may be given
- Immunization
- Active immunization
- DPT vaccine
- It is combination of Diphtheria toxoid, pertusis vaccine and tetanus toxoid
- Route Of Adminis Tration:
- Intramuscular
- Dose:
- Initial dose- 6 weeks
- Three doses are completed at intervals of 46 weeks
- Booster doses-18 months and 5 years
- Passive immunization
- Antitetanus serum is used in a dose of 1500 IU by intramuscular route
- Combined prophylaxis
- Active immunization
Question 15. Cretinism
Answer:
Cretinism
- Cretinism is a characteristic feature of infantile hypothyroidism
Cretinism Clinical Features:
- Mental retardation
- Delayed milestones of development
- Protruding tongue
- Flat nose
- Dry skin
- Sparse hairs
- Enlarged skull
- Generalised edema
- Hypotension
- Atrophy of sweat glands
- Protruded abdomen
Cretinism Oral Manifestations:
- Delayed eruption and exfoliation of deciduous teeth
- Macroglossia
- Thick lips
- Constant drooling of saliva
- Malocclusion
- Underdevelopment of mandible
- Wide face
important short questions in endocrinology
Question 16. Albuminuria
Answer:
Albuminuria
- The presence of albumin in the urine is known as albuminuria
- The Dipstick test is a standard test for it
- It identifies the presence of renal disease or urinary infection in diabetic individuals
- It detects urine albumin greater than 300 mg/1 and even smaller amounts of urinary albumin
Question 16. Phenylketonuria
Answer:
Phenylketonuria
- Phenylketonuria is a common metabolic disorder
Phenylketonuria Causes:
- Deficiency of the hepatic enzyme phenylalanine hydroxylase
Phenylketonuria Mechanism:
2. Phenylalanine is diverted to alternate pathways
Phenylketonuria Clinical Features:
- Effects on CNS
- Mental retardation
- Failure to walk or talk
- Retarded growth
- Seizures and tremors
- Low IQ
- Effect on pigmentation
- Hypopigmentation
- Urine
- Contains phenylalanine and its metabolic products
- Mousthe ey odor due to press ence of phenylacetate
Phenylketonuria Treatment:
- Intake of diet with low phenylalanine content
- Use of synthetic amino acid preparation
- Provide tyrosine in the diet
- Administration of 5-hydroxytryptophan and dopa in serious conditions
Question 17. Hyperpituitarism
Answer:
Hyperpituitarism
- Hyperpituitarism in infancy leads to gigantism and among adults it produces acromegaly
Hyperpituitarism Causes:
- Hypersecretion of growth hormone
- Increased function of the anterior pituitary
Hyperpituitarism Gigantism:
- Generalized symmetric overgrowth of the body
- Gentital underdevelopment
- Excessive sweating
- Headache
- Lassitude
- Joint and muscle pain
- Defective vision
Question 18. Goitre
Answer:
Goitre
- Goitre refers to enlargement of the thyroid gland irrespective of its cause
Goitre Classification:
- Simple goitre
- Diffuse hyperplastic goitre
- Nodular goitre
- Colloid goitre
- Toxic goitre
- Diffuse toxic goitre
- Toxic nodular goitre
- Toxic nodule
- Neoplastic goitre
- Benign tumours
- Malignant tumours
- Thyroiditis
- Other rare conditions
Question 19. Exophthalmos
Answer:
Exophthalmos
- Exophthalmos is defined as abnormal protrusion of the eyeball anteriorly out of the orbit
Exophthalmos Causes:
- Inflammatory/Infection:
- Graves’ disease
- Orbital cellulitis
- Mucormycosis
- Orbital pseudotumor
- High-altitude cerebral edema
- Wegener’s granulomatosis
- Neoplastic:
- Leukemias
- Meningioma, (of the sphenoid wing)
- Nasopharyngeal angiofibroma
- Hemangioma, cavernous
- Cystic:
- Dermoid cyst
- Vascular:
- Carotid-cavernous fistula
- Aortic insufficiency
- Others:
- Orbital fracture: apex, floor, medial wall, zygomatic
- Retrobulbar hemorrhage
- Cushing’s syndrome
Exophthalmos Complications:
- Corneal dryness and damage
- Keratoconjunctivitis
- Blindness due to compression of optic nerve and vessels
short answer type questions endocrine system
Question 20. Hyperparathyroidism
Answer:
Hyperparathyroidism
- Hyperparathyroidism is an endocrine disorder occurring due to an excess of circulating parathyroid hormone
Hyperparathyroidism Types:
- Primary hyperparathyroidism
- Occurs due to tumor of glands
- Secondary hyperparathyroidism
- Occurs in response to hypocalcemia
- Tertiary hyperparathyroidism
- Occurs after long-standing secondary hyperparathyroidism
Hyperparathyroidism Clinical Features:
Age and sex- common in middle-aged women
- Classic triad
- Kidney stones
- Bone resorption
- Duodenal ulcers
- Renal symptoms
- Renal calculi
- Hematuria
- Back pain
- Psychological symptoms
- Emotionally unstable
- GIT symptoms
- Anorexia
- Nausea, vomiting
- Skeleta
- Bone pain
- Pathologic fractures
- Bone deformities
- Hypercalcemia
- Generalised symptoms
- Muscle weakness
- Fatigue
- Weight loss
- Insomnia
- Headache
- Olydipsiaand polyuria
- Oral manifestations
- Intraoral and extraoral swelling
- Gradual loosening of teeth
- Drifting and loss of teeth
- Malocclusion
Question 21. Risus sardonicus
Answer:
Risus sardonicus
- Risussardonicus or rictus grin is a highly characteristic, abnormal, sustained spasm of the facial muscles that appear to produce grinning.
Risus sardonicus Causes:
- Tetanus
- Poisoning with strychnine
Question 22. Gynaecomastia
Answer:
- Gynaecomastia is the presence of glandular breast tissues in males
Risus sardonicus Causes:
- Idiopathic
- Physiological
- Drug-induced
- Hypogonadism
- Androgen resistance syndromes
- Oestrogen excess
Risus sardonicus Investigations:
- Ultrasonography
- Mammography
- Random blood sample
Risus sardonicus Treatment:
- Self regressing
- Surgical excision for cosmetics reasons
- Androgen replacement
Question 23. Thyroxin
Answer:
Thyroxin
- Thyroxin is a hormone secreted by the thyroid gland
- The thyroid gland secretes mainly thyroxin, T4, and small amount of triiodothyronine, T3
- T3 is the active form of the hormone, Most of the T4 is converted into T3 in peripheral tissues
- Thyroid hormones are carried in plasma in the bound form with a plasma protein while a small amount circulates unbound
- Free form enters cells and exerts its metabolic effects
- its level is measured by thyroid function tests
endocrinology short questions mbbs
Question 24. Anti-thyroid drugs
Answer:
Anti-Thyroid Drugs
- These are used to restore the patient to a euthyroid state and maintain it
- They are:
- Propylthiouracil
- Dose: 100-300 mg every 6-8 hours
- Carbimazole
- Dose: 10-20 mg every 6-8 hours
Anti-Thyroid Drugs Side Effects:
- Skin rashes
- Fever
- Peripheral neuritis
- Polyarteritis
- Agranulocytosis
- Aplastic anemia
- Prothrombin deficiency
VIVA VOCE
- Acetone breath is seen in diabetes mellitus
- Congestive heart failure occurs in hypothyroidism
- Carpal tunnel syndrome occurs in hypothyroidism
- Metformin is a biguanide hypoglycaemic drug
- Severe neurological and cardiac changes occur at calcium levels> 16 mg/ dl
