Diseases Of Blood And Lymphoreticular System Important Notes
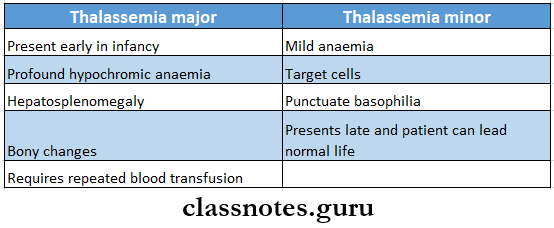
1. Thalassemia
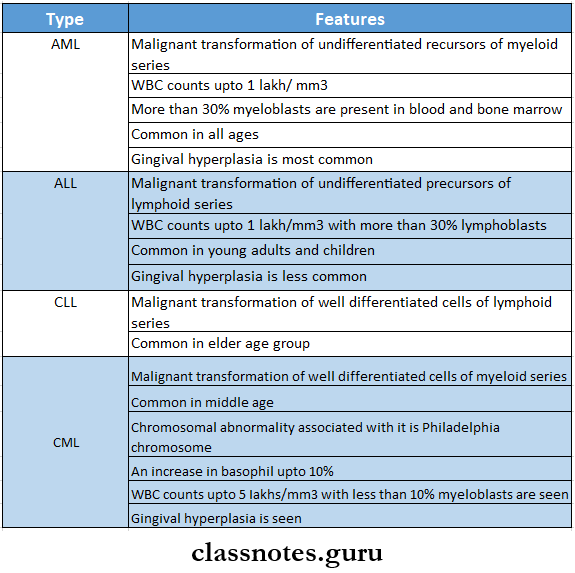
2. Types Of Leukemia
Diseases of blood and lymphoreticular system
3. Causes Of DIC
- Infections like E.coli, N. meningitis, strep. Pneumonia
- Cancers of the lung, prostate, pancreas
- Obstetric preeclampsia, amniotic fluid embolism
Read And Learn More: General Medicine Question and Answers
4. Complications Of Polycythemia Vera
- Elevated red cells
- Splenomegaly
- Leukocytosis
- Thrombosis
5. Components That Are Destroyed Quickly From Stored Blood Are
- WBC
- Clotting factors
- Platelets
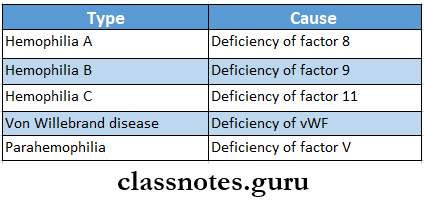
6. Types Of Hemophilia
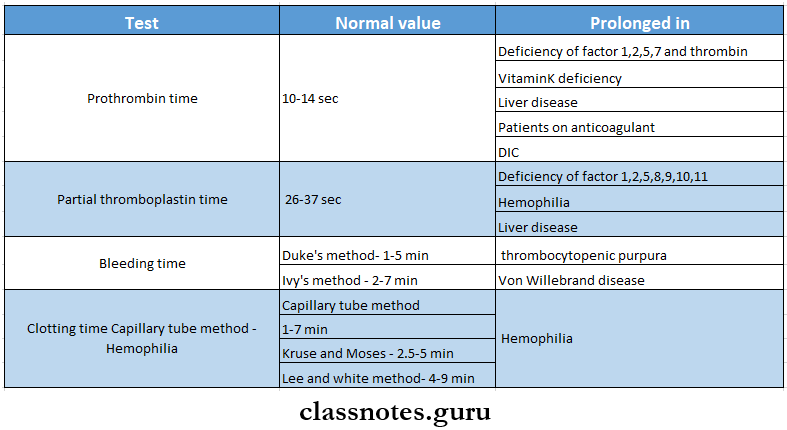
7. Bleeding Tests
8. Platelets
- Normal count 1.54 lakhs/mm3
- Increased in thrombocytosis
- Decreased in thrombocytopenic purpura
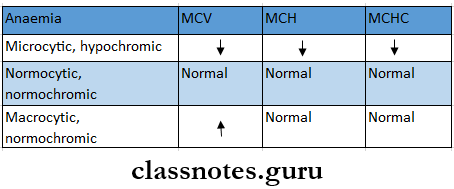
9. Anaemia
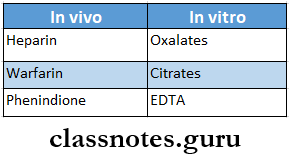
10. Anticoagulants
11. Erythroblastosis Foetalis
- When a Rh ve mother carries in a Rh +ve fetus, usually the first child escapes the complication of the Rh incompatibility
- When the mother conceives for the second time and carries an Rh +ve fetus, the Rh agglutinins enter the fetus and cause agglutination of fetal RBC and hemolysis
- Complications
- Hydrops fetalis
- Kernicterus
Diseases Of Blood And Lymphoreticular System Short Essays
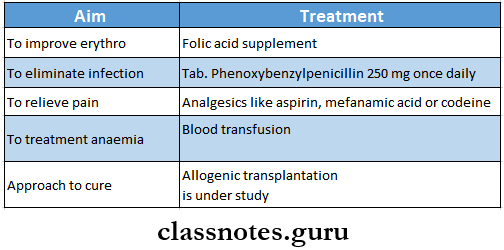
Question 1. Sickle Cell Anaemia
Answer:
Sickle Cell Anaemia
- Hb S is abnormal hemoglobin which gets polymerise and distorts the cell membrane to form abnormal sickle-shaped cell
Sickle Cell Anaemia Clinical features
- Chronic anemia features
- Fatigue
- Lassitude
- Breathlessness
- Cardiomegaly
- Increased susceptibility to infection
- Hyperplasia of bone marrow producing frontal bossing and malar prominence
- Mild jaundice
- Splenomegaly
- Poor healing ulcers
- Other features
- Pain due to blockage of small or large vessels
- Large swelling, pain, and tenderness of fingers and toes
- Acute abdominal colic, renal infarction
- Painful hematuria
- Aseptic necrosis of the head of the femur
- Fever, malaise
- Microembolisation of pulmonary vessels occurs in late pregnancy
Sickle Cell Anaemia Diagnosis
- Haemoglobin low
- Unconjugated bilirubin increases
- Peripheral blood smear shows
- Sickle cell, target cells, and Howell Jowel bodies
- Positive sickling test
- Presence of abnormal hemoglobin – HbS
Sickle Cell Anaemia Management
Blood disorders notes PDF
Question 2. Causes Of Megaloblastic Anaemia
Answer:
Causes Of Megaloblastic Anaemia
- Inadequate dietary intake
- Malabsorption
- Intrinsic factor deficiency
- Pernicious anaemia
- Gastrectomy
- Congenital lack of factor
- Intestinal causes
- Tropical sprue
- Ileal resection
- Crohn’s disease
- Removal of B12 from intestine
- Bacterial proliferation in intestinal blind loop syndrome
- Fish tapeworm infestations
- Drugs ex: PAS, neomycin
- Intrinsic factor deficiency
Question 3. Oral Manifestations Of Leukemia
Answer:
Gingiva
- Gingivitis
- Gingival hyperplasia
- Enlargement of interdental papilla
- Swollen gingival tissue
- Cyanotic bluish discoloration of gingiva
- Thrombosis of gingival vessels
Teeth
- Rapid loosening of teeth
- Alteration in developing tooth crypts
- Destruction of lamina dura
- Displacement of teeth
Oral mucosa
- Thinning of oral mucosa
- Petechiae and ecchymosis over oral mucosa
- Development of multiple large irregular necrotic ulcers
Other
- Large hematomas over the lower lip
- Oral infections
- Palatal ulcerations
- Mental nerve neuropathy
- Prolonged postoperative bleeding
- Osteomyelitis of jaw
Question 4. Iron Deficiency Anaemia
Answer:
Iron Deficiency Anaemia
- Iron Deficiency Anaemia is A chronic, microcytic, hypochromic anemia that occurs either due to inadequate absorption or excessive loss of iron from the body
Iron Deficiency Anaemia Clinical Features:
- Anaemia:
- Usual symptoms are weakness, fatigue, dyspnoea on exertion, palpitations, pallor of skin, mucous membranes, and sclera.
- Older patients may develop angina and congestive cardiac failure.
- Womenmenorrhagia is a common symptom.
- Epithelial tissue changes:
- Nails (koilonychia or spoon-shaped nails)
- Tongue (Atrophic glossitis)
- Mouth (angular stomatitis)
Iron Deficiency Anaemia Diagnosis:
- Serum iron and ferritin are low.
- Total iron binding capacity is increased Transferrin saturation is below 16%.
- Stool examination for parasites and occult blood is useful.
- Endoscopic and radiographic examination of GI tract is needed to detect the source of bleeding.
- Hematological findings: Examination of peripheral blood picture.
- Size: Microcytic anisocytotic a Chromicity: Anisochromia is present.
- Shape: Poikilocytosis is often present, pear-shaped tailed variety of RBC, elliptical form common.
- Reticulocytes: Present, either normal/reduced
- Osmotic fragility: slightly decreased
- ESR: Seldom elevated
- Absolute value: MCV, MCH, and MCEIC are reduced.
Bone Marrow Findings:
- Marrow cellularity increased due to erythroid hypoplasia micronormoblast.
- Marrow iron reduce reticuloendothelial iron stores and absence of siderotic iron granules from developing normoblasts.
Iron Deficiency Anaemia Management:
- Iron supplement
- Ferrous sulfate 300 mg 34 times/day for 6 months only
- Iron sorbitol 1.5 mg/kg body weight given parentally
Lymphoreticular system diseases
Question 5. Aplastic Anaemia clinical features
Answer:
Aplastic Anaemia
- Aplastic anemia is characterized by
- Anaemia
- Leukopenia
- Thrombocytopenia
- Hypocellular bone marrow
Aplastic Anaemia Clinical Features:
- Anaemia
- Excessive tendency to bleed
- Easy bruising
- Epilaxis
- Gum bleeding
- Heavy menstrual flow
- Petechiae
- Predisposition to infections
Question 6. Megaloblastic anaemia
Answer:
Megaloblastic Anaemia
- Megaloblastic Anaemia is macrocytic anaemia with megaloblasts in the bone marrow
Etiology:
- Inadequate dietary intake
- Malabsorption
- Intrinsic factor deficiency
- Pernicious anaemia
- Gastrectomy
- Congenital lack of factor
- Intestinal causes
- Tropical sprue
- Ileal resection
- Crohn’s disease
- Removal of B12 from the intestines
- Bacterial proliferation in intestinal blind loop syndrome
- Fish tapeworm infestation
- Drugs for example, PAS, neomycin
- Intrinsic factor deficiency
Megaloblastic Anaemia Clinical Features:
- Anemia,
- Glossitis
- Neurological manifestations numbness, paraesthesia, weakness, ataxia, diminished reflexes
- Others mild jaundice, angular stomatitis, purpura, malabsorption, anorexia
Megaloblastic Anaemia Management:
- Vitamin B12 deficiency
- Parenteral administration of hydroxocobalamin 1000 microgram twice a week during first week
- followed by 1000 microgram weekly for 6 weeks
- Maintenance therapy includes hydroxocobalamin 1000 microgram intramuscular every 3 months for rest of life
- folate deficiency
- Daily dose of 5 mg of folic acid as initial dose
- Dose of 5 mg of folic acid once a week as a maintenance dose
Question 7. Plummer Vinson syndrome
Answer:
Plummer Vinson Syndrome
- Plummer Vinson Syndrome is characterised by dysphagia, iron doccie anaemia, dystrophy of nails and glossits
Plummer Vinson Syndrome Clinical Features:
- Common in middle age females
- Dysphagia
- Angular chelitis
- Spasm in throat
- Sore mouth
- A smooth, red, and enlarged tongue
- Oral mucosa is pale and painful
- Dry mouth
- Spoon shaped nails
Plummer-Vinson Syndrome Diagnosis
- Biopsy shows:
- Atrophic epithelium
- Atrophy of the lamina propria and muscles
Plummer-Vinson Syndrome Management:
- Correction of anaemia
- Esophageal dilation
Anemia types and management
Question 8. Eosinophilia
Answer:
Eosinophilia Clinical features:
- Dysponea
- Orthopnoca
- Wheezing
- Cough with mucoid expectoration
- Chest pain
Eosinophilia Management:
- DiethvlrarbamaZine2 mg/kg three firms a day for 2 weeks
- Antihistamines are given to treat allergic reations
Question 9. Tropical Eosinophilia
Answer:
Tropical Eosinophilia
- It is characterised by the presence of hypereosinophilia, circulating filarial antibodies, microfilaria in tissues
- Commonly seen in tropical countries like India, and Sri Lanka. Indonesia, Pakistan and Southeast Asia
- Patient may have lymphadenopathy, splenomegaly,chronic, cough, nocturnal bronchospasm
Tropical Eosinophilia Diagnosis:
- History of prolong stay in endemic area
- Lack of microfilaria in peripheral blood
- Peripheral eosinophilia
- IgE levels of atleast 1000 units/ ml
Tropical Eosinophilia Management:
- Diethylcarbamazine-2 mg/kg three times a day for 2 weeks
- Antihistamines are given to treat allergic reactions
Question 10. Discuss An Approach To Bleeding Disorders
Answer:
- Investigations of disordered vasiular hemostasis
- Bleeding time
- It is based on the principle of formation of hemostatic plug following a standard incision on the ulnar aspect of the forearm and the time from incision to when bleeding stops is measured
- Normal-3-8 minutes
- Hess capillary resistance test
- This test is done by tying the sphygmomanometer cuff to the upper arm and raising the pressure in it between diastolic and systolic for 5 minutes
- After deflation, the number of petechiae appear in the next 5 minutes in 3 camera over the cubital fossa are counted
- Piesence of more than 20 petechiae is considered a positive test
- Bleeding time
- Investigation of blood coagulation
- Screening test
- Whole blood coagulation time
- The estimation of whole blood coagulation time done by various capillary and tube method
- Normal value-4-9 minutes
- Activated partial thromboplastin time (PTTK)
- This test is used to measure the intrinsic system factors as well as factors common to both intrinsic and extrinsic factors
- One stage prothrombin time measures the extrinsic system factor 6 as well as factors in the common pathway
- Whole blood coagulation time
- Special tests
- Coagulation factor assays
- These are based on the results of PTTK or prothrombin time tests
- Quantitative assays
- Done by immunological and other chemical methods
- Coagulation factor assays
- Screening test
Question 11. Clinical features and management of acute myeloid leukemia
Answer:
Acute myeloid leukemia is a heterogenous disease charaterised by the infiltration of malignant myeloid cells into the blood, bone marrow, and other tissues
Acute Myeloid Leukemia Clinical Features:
- Anemia-producing pallor, lethargy, dyspnoea
- Thrombocytopenia
- Spontaneous bruises
- Petechiae, bleeding from gums, and other bleeding tendencies
- Infections
- Fever
- Pain and tenderness of bones
- Lymphadenopathy
- Splenomegaly
- Hepatomegaly
- Leukemic infiltration of the kidney
- Gum hypertrophy
- Testicular swelling
Acute Myeloid Leukemia Management:
- Regular platelet transfusion
- Prophylaxis against infections
- Combination of three drugs is used
- Cytosine arabinoside
- Anthracyclines
- 6-thioguanine
- Bone marrow transplantation
Leukemia short essay
Question 12. Clinical Features And Management Of Chronic Myeloid Leukemia
Answer:
Chronic Myeloid Leukemia Clinical Features:
- Onset is usually slow, initial symptoms are often nonspecific.g: weakness, pallor, dyspnoea, and tachycardia.
- Symptoms due to hypermetabolism such as weight loss, anorexia, night sweats.
- Splenomegaly is almost always present and is frequently massive. In some patients, it may be associated with acute pain due to splenic infarction.
- Bleeding tendencies such as bruising, epistaxis, menorrhagia, and heamatomas may occur.
- Visual disturbance, neurologic manifestations.
- Juvenile CML is more often associated with lymph node enlargement than splenomegaly.
Chronic Myeloid Leukemia Management:
- Imatinib oral therapy
- Allogenic bone marrow transplantation
- Interferon-alpha
- Chemotherapy drugs used are busulfan, cyclophosphamide, and hydroxyurea
Question 13. Oral manifestations of hematological disorders transfusion
Answer:
Oral Manifestations Of Hematological Disorders Transfusion
- Gingivasevere hemorrhage
- Soft tissue hematoma formation
- Jawrecurrent subperiosteal hematoma
- Tumourlike malformation B Teethhigh caries index
- Severe periodontal disease
- Oropharyngeal bleeding
- Severe bleeding at the injection site
Question 14. Complications of blood transfusion
Answer:
Complications Of Blood Transfusion
- Transfusion reactions
- Incompatibility due to
- Incompatible transfusion
- Transfusion of hemolysed blood
- Transfusion of expired blood
- Pyrexia reactions characterized by
- Pyrexia
- Chill
- Rigor
- Restlessness
- Headache
- Increased pulse rate
- Nausea and vomiting
- Allergic reactions
- Mild tachycardia
- Urticarial rash
- Fever
- Dyspnoea
- Sensitization to leucocytes and platelets
- Incompatibility due to
- Transmission of diseases like
- Hepatitis
- AIDS
- Bacterial infections
- Reactions caused by massive transfusion
- Acid base imbalance
- Hyperkalaemia
- Citrate toxicity
- Hypothermia
- Failure of coagulation
- Complication of general intravenous fluid transfusion
- Congestive cardiac failure
- Complication of general intravenous fluid transfusion
- Thrombophlebitis
- Air embolism
Lymphoma short notes
Question 15. Idiopathic thrombocytopenic purpura investigations and treatment
Answer:
Idiopathic Thrombocytopenic Purpura
- Idiopathic thrombocytopenic purpura is an autoimmune disorder due to antibodies directed against platelet membrane glycoprotein resulting in the premature clearance of these cells by the immune system
Idiopathic Thrombocytopenic Purpura Investigations:
- Chronic history of bleeding
- Bleeding time is prolonged
- Reduced platelet count
- Bone marrow shows increased megakaryocytes indicating peripheral destruction of platelets
Idiopathic Thrombocytopenic Purpura Management:
- Self-limiting in children
- Moderate to severe ITP is treated with prednisolone 2 mg/ kg daily orally
- In adults prednisolone 60 mg dialysis started and then continued for 24 weeks and then slowly withdrawn
- In severe cases, intravenous immunoglobulin IgG should be given in a dose of 1 g/kg
Diseases Of Blood And Lymphoreticular System Short Answers
Question 1. Sickle cell anaemia
Answer:
Sickle Cell Anaemia
- Hb S is abnormal hemoglobin which gets polymerise and distort the cell membrane to form abnormal sickle-shaped cell
Sickle Cell Anaemia Clinical features
- Chronic Anaemia Features
- Fatigue
- Lassitude
- Breathlessness
- Cardiomegaly
- Increased susceptibility to infection
- Hyperplasia of bone marrow producing frontal bossing and malar prominence
- Mild jaundice
- Splenomegaly
- Poor healing ulcers
- Other Features
- Pain due to blockage of small or large vessels
- Large swelling, pain and tenderness of fingers and toes
- Acute abdominal colic, renal infarction
- Painful hematuria
- Aseptic necrosis of head of femur
- Fever, malaise
- Microembolisation of pulmonary vessels occurs in late pregnancy
Question 2. Von Willebrand disease
Answer:
Von Willebrand Disease
- Von Willebrand Disease is coagulation disorder
Von Willebrand Disease Causes And Related Features
- Platelet Dysfunction Leads To
- Superficial bruising
- Epitaxis
- Menorrhagia
- GI bleeding
- Low Levels Of Von Willebrand Factor
- Depending on the level of vWF, 3 types of disease occur
Von Willebrand Disease Diagnosis:
- Abnormal platelet function
- Increased bleeding time
- Normal prothrombin time
- Decreased factor 8
- Reduced vWF
Question 3. Causes of pancytopenia
Answer:
Pancytopenia
- Pancytopenia is a simultaneous presence of anaemia, leucopenia, and thrombocytopenia
- pancytopenia Causes
- Aplastic anaemia
- Paroxysmal nocturnal hemoglobinuria
- Megaloblastic anaemia
- Bone marrow infiltration
Question 4. Peripheral smear in iron deficiency anaemia
Answer:
Peripheral Smear In Iron Deficiency Anaemia
- Hematological findings: Examination of peripheral blood picture.
- Size: Microcytic anisocytosis
- Chromicity: Anisochromia is present.
- Shape: Poikilocytosis is often present, pear-shaped tailed variety of RBC, elliptical form common.
- Reticulocytes: Present, either normal/reduced
- Osmotic Fragility: slightly decreased
- ESR: Seldom elevated
- Absolute Value: MCV, MCH, and MCHC are reduced.
Question 5. Treatment Of Iron Deficiency Anaemia
Answer:
Iron Supplement
- Ferrous sulfate 300 mg 34 times/day for 6 months only
- Iron sorbitol 1.5 mg/kg body weight given parentally
Question 6. Iron therapy
Answer:
Iron Preparations:
- Oral iron preparations
- It is the preferred route of administration
- Preparations:
- Ferrous sulfate 200 mg tab
- Contains 20% hydrated salt and 32% dried salt
- It is inexpensive
- Produces metallic taste in mouth
- Ferrous gluconate 300 mg tab
- Contains 12% of iron
- Causes less gastric irritation
- Ferrous fumarate 200 mg tab
- Contains 33% iron
- It is less water soluble and tasteless
- Ferrous succinate 100 mg tab, 35% iron
- Better absorbed and expensive
- Iron calcium complex 5% iron
- Better absorbed and expensive
- Ferric ammonium citrate 45 mg tab
- Better absorbed and expensive
- Ferrous sulfate 200 mg tab
- Dose:
- Total 200 mg given daily in 3 divided doses
- Prophylactic dose 30 mg daily
- Indications:
- Iron deficiency anaemia
- Adverse Effects:
- Nausea, vomiting, epigastric pain
- Heart bum
- Staining of teeth
- Metallic taste
- Constipation
- Parenteral iron preparations
- Intramuscular injection of iron is given deep in the gluteal region using Z technique
- Intravenous is given slowly over 510 minutes
- Preparations:
- Iron dextran
- It is colloidal solution containing 50 mg elemental iron
- It is given intravenously and Intramuscularly
- Iron sorbitol citric acid complex
- Contains 50 mg elemental iron
- Can be given only IM
- If given 4 it quickly saturates transferrin stores
- Due to it free iron levels in the plasma rises and causes toxicity
- Iron dextran
- Dose:
- It is calculated using formula:
- Iron requirement ( in mg) = 4.4 * body weight (in kg) * Hb deficit (in g/ dl)
- Indications:
- When oral iron is not tolerated
- Failure of absorption of oral iron
- Noncompliance
- In presence of severe deficiency with chronic bleeding
- Along with erythropoietin
- Adverse Effects:
- Pain at the site of injection
- Pigmentation of skin
- Sterile abscess
- Fever
- Headache
- Joint pain, flushing, palpitation
- Chest pain, dyspnoea
- Anaphylactic reaction
Classification of anemia short essay
Question 7. Megaloblastic anaemia
Answer:
Megaloblastic Anaemia
- Megaloblastic Anaemia is macrocytic anaemia with megaloblasts in the bone marrow
Etiology:
- Inadequate dietary intake
- Malabsorption
- Intrinsic factor deficiency
- Pernicious anaemia
- Gastrectomy
- Congenital lack of factor
- Intestinal causes
- Tropical sprue
- Ileal resection
- Crohn’s disease
- Removal of B12 from the intestines
- Bacterial proliferation in intestinal blind loop syndrome
- Fish tape worm infestation
- Drugs, for example, PAS, neomycin
- Intrinsic factor deficiency
Megaloblastic Anaemia Clinical Features:
- Aneamia
- Glossitis
- Neurological manifestations numbness, paraesthesia, weakness, ataxia, diminished reflexes.
- Othersmild jaundice, angular stomatitis, purpura, malabsorption, anorexia
Question 8. Four causes of anaemia
Answer:
Four Causes Of Anaemia
- Anaemia due to increased blood loss
- Acute posthaemorrhagic anaemia
- Chronic blood loss
- Anaemias due to impaired red cell production
- Cytoplasmic maturation defects
- Deficient Haem Synthesis:
- Iron deficiency anaemia
- Deficient Globin Synthesis:
- Thalassaemic syndromes
- Deficient Haem Synthesis:
- Nuclear maturation defects
- Vitamin B12 and/or folic acid deficiency:
- Megaloblastic anaemia
- Defect in stem cell proliferation and differentiation
- Aplastic anaemia
- Pure red cell aplasia
- Anaemia of chronic disorders
- Bone marrow infiltration
- Congenital anaemia
- Cytoplasmic maturation defects
- Anaemias due to increased red cell destruction (Haemolytic anaemias).
- Extrinsic (Extracorpuscular) red cell abnormalities
- Intrinsic (Intracorpuscular) red cell abnormalities
Question 9. Causes of iron deficiency anaemia
Answer:
Causes Of Iron Deficiency Anaemia
- Inadequate intake of iron in diet
- Malabsorption of iron due to diarrhea
- Increased requirement in growing child and in pregnanacy
- Increased loss of iron due to injury, epitaxis, and peptic ulcer
- Gastrotomy
Question 10. Hemolytic anaemia
Answer:
Hemolytic Anaemia Definition:
- Hemolytic Anaemia is an abnormal exessive destruction of red cells that overwhelms the compensatory capacity of the bone marrow
Etiology:
- Congenital
- Abnormalities of red cell membrane
- Disorders of haemoglobin
- Red cell enzyme defects
- Acquired
- Immune defects
- Nonimmune defects
Question 11. Two drugs used in eosinophilia
Answer:
Two Drugs Used In Eosinophilia
- Drugs used in eosinophilia are
- Prednisolone
- Diethylcarbamazine
Question 12. Classification of leukemia
Answer:
Leukemia
- Based on cell types predominantly involved.
- Myeloid
- Lymphoid.
- Based on natural history of disease:
- Acute
- Chronic.
WHO Classification Of Myeloid Meoplasm:
- Myeloproliferative Diseases:
- Chronic myeloid leukaemia (CML), {Ph chromosome t(9;22), BCR/ABLpositive}
- Chronic neutrophilic leukaemia
- Chronic eosinophilic leukaemia/ hypereosinophilic syndrome
- Chronic idiopathic myelofibrosis
- Polycythaemia vera (PV)
- Essential thrombocythaemia (ET)
- Chronic myeloproliferative disease, unclassifiable
- Myelodysplastic/Myeloproliferative Diseases:
- Chronic myelomonocytic leukaemia (CMML)
- Myelodysplastic Syndrome (MDS):
- Refractory anaemia (RA)
- Refractory anaemia with ring sideroblasts (RARS)
- Refractory cytopenia with multilineage dysplasia (RCMD)
- RCMD with ringed sideroblasts (RCMD-RS)
- Refractory anaemia with excess blasts (RAEB-1)
- RAEB-2
- Myelodysplastic syndrome unclassified (MDS-U)
- MDS with isolated del 5q
- Acute Myeloid Leukaemia (AML):
- AML with recurrent cytogenetic abnormalities
- AML with t(8;21)
- AML with abnormal bone marrow eosinophils
- Acute promyelocytic leukaemia (t(15;17)
- AML with 11q23 abnormalities (MLL)
- AML with multilineage dysplasia
- With prior MDS
- Without prior MDS
- AML and MDS, therapy-related
- Alkylating agent related
- Topoisomerase type 2 inhibitor-related
- Other types
- AML, not otherwise categorised
- AML, minimally differentiated
- AML without maturation
- AML with maturation
- Acute myelomonocytic leukaemia (AMML)
- Acute monoblastic and monocytic leukaemia
- Acute erythroid leukaemia
- Acute megakaryocytic leukaemia
- Acute basophilic leukaemia
- Acute panmyelosis with myelofibrosis
- Myeloid sarcoma
- AML with recurrent cytogenetic abnormalities
- Acute Biphenotypic Leukaemia
Diagnosis and treatment of hemophilia
Question 13.Chronic myeloid leukemia
Answer:
Chronic Myeloid Leukemia Clinical Features:
- Onset is usually slow, initial symptoms are often nonspecific.g: weakness, pallor, dyspnoea, and tachycardia.
- Symptoms due to hypermetabolism such as weight loss, anorexia, and night sweats.
- Splenomegaly is almost always present and is frequently massive. In some patients, it may be associated with acute pain due to splenic infarction.
- Bleeding tendencies such as bruising, epistaxis, menorrhagia, and hematomas may occur.
- Visual disturbance, neurologic manifestations.
- Juvenile CML is more often associated with lymph node enlargement than splenomegaly.
Question 14. Agranulocytosis
Answer:
Agranulocytosis
- The term agranulocytosis is used to describe a stale of severe neutropenia.
- A reduction in the number of granulocytes in blood is known as neutropenia.
Agranulocytosis Causes:
- Neutropenia can be caused by following reasons.
- Drug induced: Anti-cancer, antibiotics, anticonvulsants, antithyroid drugs
- Haematological Disease: Aplastic anaemia, acute leukaemia etc.
- Infections: Malaria, TB, typhoid,
- Autoimmune: Systemic lupus erythematosis
- Congenital: Cyclic neutropenia.
Agranulocytosis Clinical Features:
- Initally patient develops malaise, chills, and fever, with subsequently marked weakness and fatiguability.
- Massive growth of microorganisms due to inability to produce leukocyte response.
- Infections are usually present as ulcerating, necrotizing lesions of gingiva, the floor of the mouth, buccal mucosa, and other sites within oral cavity known as agranulocytic angina.
- Lymphadenopathy and hepatosplenomegaly may be present.
Agranulocytosis Treatment:
- Patients with neutropenia and fever must be sent to the hospital.
- In severe infections, neutrophil transfusion must be done.
- Broad-spectrum antibiotics and antifungal drugs are to be given.
Question 15. Management of acute leukemia
Answer:
Management Of Acute Leukemia
- Regular platelet transfusion
- Prophylaxis against infections
- Combination of three drugs is used
- Cytosine arabinosidc
- Anthracyclines
- 6thioguanine
- Bone marrow transplantation
Question 16. Purpura
Answer:
Purpura Types:
- Nonthrombocytopenic purpura
- It is due to defect of capillaries
- Thrombocytopenic purpura
- It is due to decreased number of platelets
Purpura Clinical Features:
- Antiplatelet globulin or antibodies to platelets in blood are present
- Spleen is not palpable
- Severe and profuse gingival bleeding
- Platelet count is less than 60,000 per mm2
- Increased bleeding time
- Cessation of bleeding
Purpura Treatment:
- Splenectomy
Question 17. Thrombotic thrombocytopenic purpura
Answer:
Thrombotic Thrombocytopenic Purpura
- Thrombotic Thrombocytopenic Purpura is lethal disorder of vascular endothelial damage
Thrombotic Thrombocytopenic Purpura Cause:
- Deficiency of a protease called ADAMTS 13
Thrombotic Thrombocytopenic Purpura Clinical Features
- Florid purpura
- Fibrin microthrombi
- Thrombocytopenia
- Microangiopathic hemolytic anemia
- Fever
- Renal failure
- Fluctuating levels of consciousness
- Focal neurological signs
Thrombotic Thrombocytopenic Purpura Treatment:
- Exchange transfusion
- Plasmapheresis combined with infusion of fresh frozen plasma
Question 18. Idiopathic thrombocytopenic purpura
Answer:
Idiopathic Thrombocytopenic Purpura
- Idiopathic Thrombocytopenic Purpura is characterized by Immunologic destruction of platelet and normal or increased megakaryocytes in the bone marrow
Idiopathic Thrombocytopenic Purpura Types:
- Acute ITP
- Chronic ITP
Idiopathic Thrombocytopenic Purpura Clinical Features:
- Usual manifestations are petechial hemorrhage, purpura, easy bruising, epistaxis, mucosal bleeding such as menorrhagia in women, nasal bleeding, bleeding from gums, and haematuria.
- Intracranial hemorrhage is rare.
- Splenomegaly and hepatomegaly may also occur.
Immunodeficiency disorders short notes
Question 19. Importance of hemophilia to dental surgeon
Answer:
Importance Of Hemophilia To Dental Surgeon
- It is essential to prevent accidental damage to the oral mucosa when carrying out any procedure in the mouth
- Blood loss can be controlled locally with direct pressure or periodontal dressings with or without topical anlifibrinolytie agents
- Patients with bleeding disorders can be given dentures as long as they are comfortable
- Fixed and removable orthodontic appliances may be used along with regular preventive advice and hygiene therapy
- Endodontic treatment is generally low risk for patients with bleeding disorders
- Aspirin should not be used
Question 20.Burkitt’s lymphoma
Answer:
Burkitt’s Lymphoma
- Burkitt’s lymphoma is a rare type of non-Hodgkin’s lymphoma (NHL).
- Epsteinbarr virus (EBV) and HIV are associated with the development of Burkitt’s lymphoma.
- This is the most rapidly progressive tumour first described in African children.
- Most patients present with lymphadenopathy and abdominal mass.
- It has a tendency to metastasize to the CNS.
- Treatment should be initiated promptly with intensive chemotherapy. Prophylactic chemotheiapy is also given. 70-80% patients may be cured.
Question 21. Drugs used in Hodgkin’s lymphoma
Answer:
Drugs Used In Hodgkin’s Lymphoma Are
- Vinblastin sulfate
- Bleomycin
- Mustargen
- Chlorambucil
- Cyclophosphamide
Question 22. Hypersplenism
Answer:
Hyperspleenism
- Hypersplenism is defined as a clinical condition in which spleen removes excessive quantites of erythrocytes, granulocytes, and platelets from the circulation
Hyperspleenism Clinical Features:
- Cirrhosis of the liver with portal hypertension
- Accelerated destruction of one or more elements of blood
- Pancytopenia
- Infections
- Easy bruising
- Excessive bleeding tendencies
Hyperspleenism Treatment:
- Treatment of the underlying disorder
- Splenectomy
- Supportive antibiotics
- Blood transfusion
Question 23. Splenomegaly
Answer:
Spleenomegaly
- Enlargement of spleen is called spleenomegaly
Splenomegaly Causes:
- Infective disorders
- Bacterial
- Endocarditis
- Tuberculosis
- Septicaemia
- Salmonella
- Viral
- Hepatitis
- AIDS
- Infectious mononucleosis
- Protozoal
- Malaria
- Leishmaniasis
- Spirochaetal
- Syphilis
- Fungal
- Histoplasmosis
- Bacterial
- Inflammatory disorders
- Rheumatoid arthritis
- SLE
- Sarcoidosis
- Congestive splenomegaly
- Hepatic vein thrombosis
- Chronic congestive heart failure
- Pericardial effusion
- Diseases associated with hemolysis
- Spherocytosis
- Sickle cell disease
- Infiltrative disease of spleen
- Miscellaneous
- Iron deficiency anaemia
- Idiopathic
- Sarcoidosis
Question 24. Causes of massive spleenomegaly
Answer:
Causes Of Massive Spleenomegaly
- Hemolytic anaemia thalassaemia
- Infectionsmalaria, kalaazar
- Collagen vascular disorder rheumatoid arthritis
- Congestionportal hypertension
- Malignant infiltration leukemia
Question 25. Bone marrow aspiration
Answer:
Bone Marrow Aspiration
- Bone marrow aspiration is used for bone marrow examination
Bone Marrow Aspiration Uses:
- To study cell markers
- Karyotyping
- Accurate diagnosis
- Assessment of malignant diseases
- Assessment of cellularity
- Details of developing blood cells
- Detect ratio between erythroid and myeloid cells
- Assess iron stores
Bone Marrow Aspiration Indications:
- Infiltrative disorders
- Parasitic diseases
- Cytopenic disorders
- Infective disorders
Question 26. ESR
Answer:
ESR
If a sample of blood with an anticoagulant is allowed to stand in a vertical tube, the RBC settles down due to gravity as compared to plasma with a clear supernatant layer of plasma. The rate at which the cells settle down is called ESR.
Method Of Estimation Of ESR: There are two standard methods as follows:
- Wintrobe’s And Landsberg’s Method: ESR is measured in undiluted blood in a hematocrit tube.
- Westergren’s Method: ESR is measured in venous blood diluted accurately with 31.3 g/L trisodium citratein the proportion of 1:4 (1 volume of 3.8% sodium citrate and 4 volume of blood).
The conditions were ESR is markedly raised are as follows:
- Infective: Tuberculosis, kala-azar, in most of the chronic infections.
- Inflammation: Rheumatoid arthritis, rheumatic fever, other connective tissue disorders.
- Neoplastic: Multiple myeloma, lymphoma, paraproteinaemia.
- Miscellaneous: Aplastic anaemia, autoimmune disorders, mixed connective tissue disorders.
Question 27. Three causes of neutropenia
Answer:
Three Causes Of Neutropenia
Neutropenia can be caused by following reasons.
- Drug-induced: Anti-cancer, antibiotics, anticonvulsants, antithyroid drugs
- Hematological Disease: Aplastic anaemia, acute leukaemia etc.
- Infections: Malaria, TB, typhoid.
- Autoimmune: Systemic lupus erythematosis
- Congenital: Cyclic neutropenia.
Question 28. Folic acid deficiency
Answer:
Folic Acid Deficiency
- Folic acid deficiency leads to:
- Megaloblastic anaemia
- Glossitis
- Diarrhoea
- Weakness
Question 29. Blood groups
Answer:
Blood Groups Classification:
- It is based on the presence or absence of a specific agglutinogen or antigen on the surface of the red cell membrane
- Important blood groups are:
- ABO system
- It is based on the presence or absence of antigen A and antigen B
- Rh blood group
- Rh fator is an antigen present in RBC
Blood Groups Uses:
- In blood transfusion
- For matching tissues in organ transplantation
- Investing cases of paternity disputes
- Helpful in emergency conditions
- In pregnancy
- For research purposes
- Anthropological purposes
Question 30. Hematological and bone marrow findings of multiple myeloma
Answer:
Hematological And Bone Marrow Findings Of Multiple Myeloma
- Blood examination shows
- Anaemia
- Neutropenia
- Thrombocytopenia
- Raised ESR
- Reversal of albumin globulin ratio
- Presence of BenceJones proteins
- Bone marrow examination
- Exhibits the presence of at least 10% atypical plasma cells in the total marrow cell population
Question 31. Clotting time
Answer:
Clotting Time
- Clotting Time is the time interval from the oozing of blood after a cut or injury till the arrest of bleeding
Normal Duration:
- 3-8 minutes
Prolonged In:
- Hemophilia
Question 32. Prothrombin time
Answer:
Prothrombin Time
Prothrombin time measures the extrinsic system factor 7 as well as factors in the common pathway
In it, tissue thromboplastin and calcium are added to the test
Normal Time:
- 10-14 seconds
Prolonged In:
- Administration of oral Anticoagulants
- Liver disease
- Vitamin K deficiency
- Disseminated intravascular coagulation
Question 33. DIC
Answer:
DIC
Disseminated intravascular coagulation is a complex thrombo-hemorrhagic disorder occurring as a secondary complication in some systemic diseases
Etiopathogenesis:
- Pathogenesis of DIC includes the following events
- Activation of coagulation
- Etiological factors like massive tissue injury, the presence of infections, and endothelial damage cause activation of coagulation by the release of tissue factor
- Thrombotic phase
- Endothelial damage from various thrombogenic stimuli causes:
- Generalized platelet aggregation
- Platelet adhesion
- Deposition of small thrombi and emboli throughout microvasculature
- Endothelial damage from various thrombogenic stimuli causes:
- Consumption phase
- Consumption of coagulation factors and platelets occurs
- Secondary fibrinolysis
- The fibrinolytic system is secondary activated
- This causes the breakdown of fibrin resulting in the formation of FDPs in circulation
Structure and function of lymph nodes
Question 34. Folic acid
Answer:
Folic Acid
Folic acid is important in one-carbon metabolism
Folic Acid Sources:
- Green vegetables, liver, yeast, egg, milk, and some fruits
Folic Acid Functions:
- The Coenzyme of it, tetrahydrofolate (THF), serves as an acceptor or donor of one carbon units
- It is involved in the synthesis of important compounds like
- PurinesIncorporated into DNA and RNA
- Pyrimidine nucleotide-deoxy thymidylic acid is involved in the synthesis of DNA
- Aminoacids-Glycine, serine, ethanolamine, and choline
- N-FormylmethionineInitiator of protein biosynthesis
Folic Acid Deficiency Manifestations:
- Megaloblastic anemia
- Glossitis
- Diarrhea
- Weakness
VIVA VOCE
- Chlorambucil is the drug of choice for chronic lym, paid leukemia
- Busulfan, and hydroxycarbamide are drugs of choice in chronic myeloid leukemia
- Hemophilia is transmitted as an X-linked recessive trait
- Von Willebrand’s disease is transmitted as an autosomal dominant trait
