Clostridium Long Essays
Question 1. Discuss in detail about organisms causing gas gangrene.
Answer:
Gas gangrene is caused by Clostridium perfringes.
- It is also known as Clostridium Welchii.
The organism causing gas gangrene Morphology:
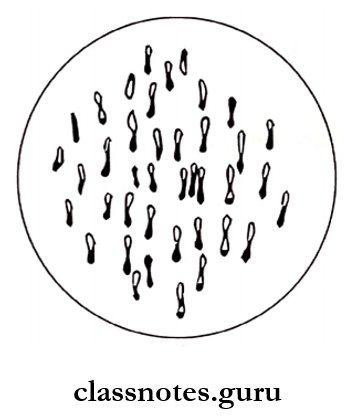
- Cl. Perfringes is Gram-positive, capsulated and non- motile bacilli.
- Size: large, 4 – 6 pm x 1
- It has subterminal spores.
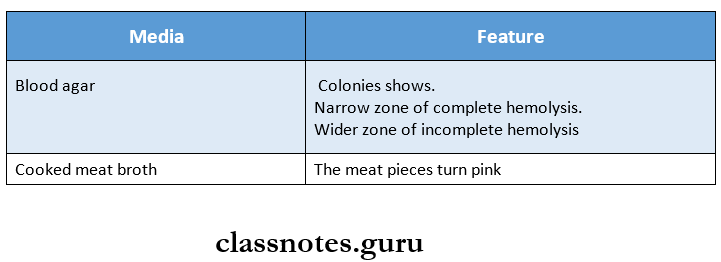
The organism causing gas gangrene Culture:
- Cl. Perfringes is anerobic.
- It grows within a temperature range of 20 – 50°C and pH -5.5-8.
The organism causing gas gangrene Biochemical Reaction:
It undergoes the following biochemical reactions.
- Ferments glucose, lactose, sucrose and maltose.
- It is indole negative.
- It leads to stormy fermentation.
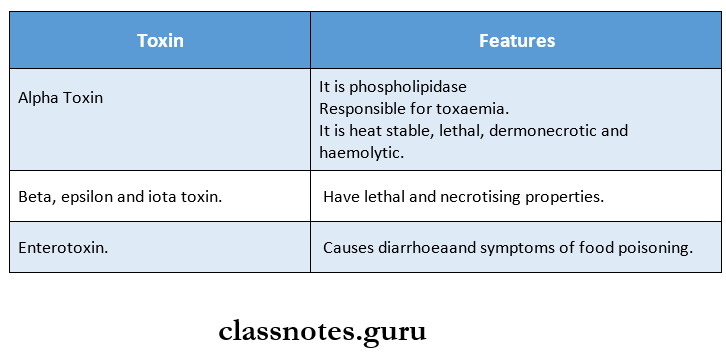
The organism causing gas gangrene Toxins:
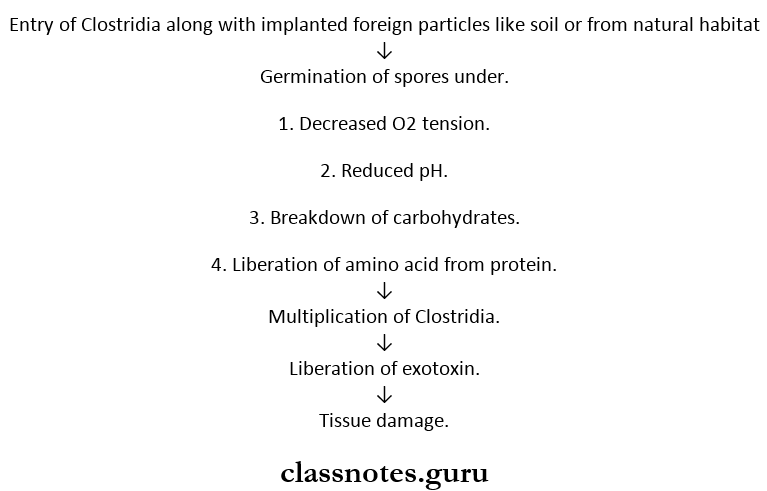
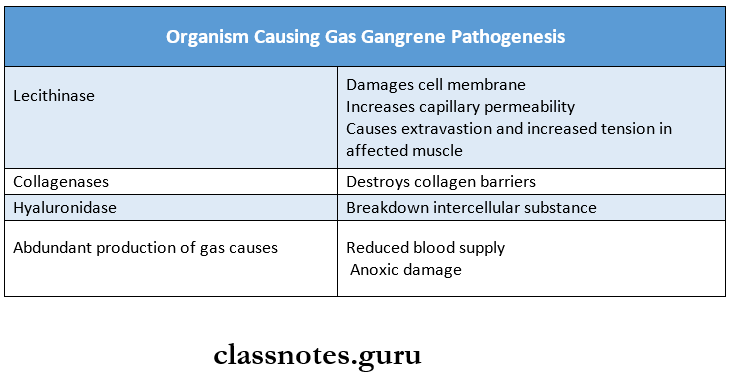
Organism causing gas gangrene Pathogenesis:
Read And Learn More: Microbiology Question and Answers
Organisms causing gas gangrene Diseases caused by them:
- Gas gangrene
- Food poisoning.
- Necrotising enteritis.
The organism causing gas gangrene Complications:
- Profound toxemia.
- Prostration
- Death due to circulatory failure.
The organism causing gas gangrene Laboratory diagnosis.
1. Specimens collected are
- Muscles – At the edge of the affected area.
- Tissue – In necrotic area.
- Exudate – In deeper parts of the wounds – in active regions.
2. Cultures:
- Aerobic and anaerobic cultures are made on fresh and heated blood agar.
- A plate of serum or egg yolk agar with C. Perfringes antitoxin spread on one half is used for Nagler re-action.
- Four tubes of Robortson’s cooked meat broth are inoculated and heated at 100oC for 5, 10, 15, and 20 min and then incubated at 45°C for 4 – 6 hours bacterial isolates are identified.
Question 2. Classify Clostridium. Describe lab diagnosis and prophylaxis of gas gangrene.
Answer:
Clostridium Classification:
1. Based on the shape and position of spores.
- Central or subterminal.
- C. Perfringes. o C. Botulinum
- Oval and terminal -C. Tertium.
- Spherical and terminal – C. Tetani.
2. Based on biochemical properties.
- Both proteolytic and saccharolytic.
- Proteolytic – predominating – C. histolyticum, C. Botulinum.
- Saccharolytic predominating – C. Welchii.
- (Slighly proteolytic but not saccharolytic – C. Tetani.
- Saccharolytic but not proteolytic -Botulinum.
- Neither proteolytic nor sacharolytic – C. Cochlearum.
2. Based on the disease.
- Gas gangrene – C. Welchii, C. Histolyticum
- Tetanus – C. Tetani.
- Food poisoning – C. Botulinum.
- Acute colitis – C. Difficile.
Clostridium Prophylaxis:
1. Surgical prophylaxis.
- Prompt removal of all damaged tissue.
- Irrigation of wound with an antiseptic solution.
- Uncompromising excision of all affected tissue.
2. Antibiotics – includes.
- Metronidazole.
- Penicillin.
- Sulphonamide.
- Tetracycline.
- Amoxycillin.
3. Antitoxin.
- Anti-gas gangrene serum provides passive immunization.
4. Introduction of hyperbaric oxygen.
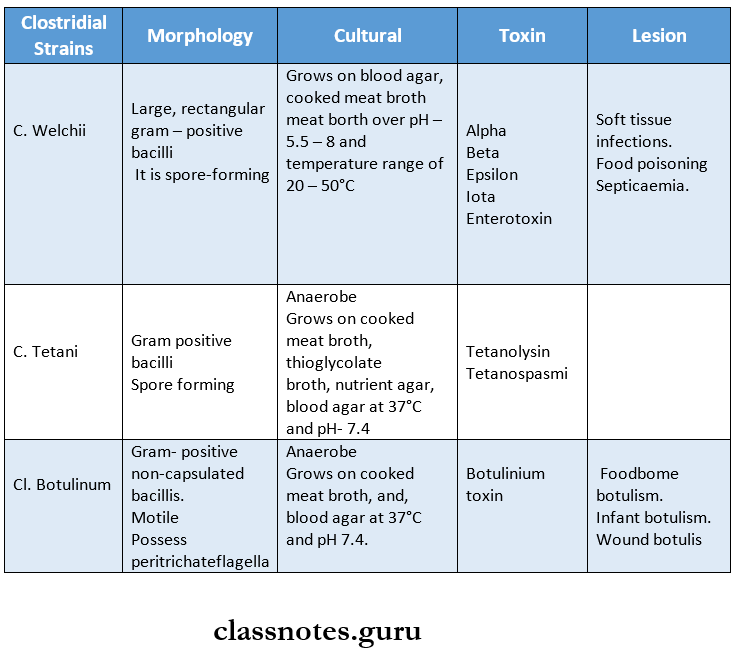
Question 3. Describe morphology, cultural characteristics, toxins liberated, and lesions produced by clostridial stains:
Answer:
Some of the clostridial strains are as follows:
Question 4. Enumerate the various pathogenic Clostridia. Describe morphology, cultural characteristics and laboratory diagnosis of Clostridium tetani.
Answer:
Pathogenic Clostridia:
- C. Welchii.
- C. Tetani.
- C. Botulinum.
- C. Septicum.
- C. histolyticum.
- C. Bifermentans.
- C. Difficle.
Pathogenic Clostridia Morphology:
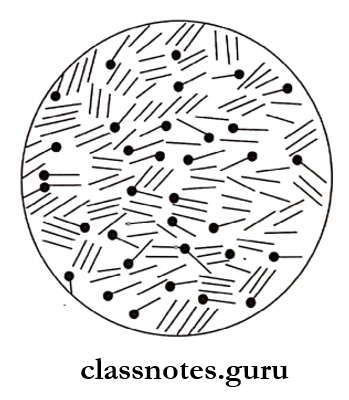
- Cl. Tetani is gram-positive, slender bacilli.
- Size – 4 – 8 pm x 0.5 pm.
- It has a straignt axis, parallel sides, and rounded ends.
- It is non-capsulated.
- It has spherical terminal spores which gives it a drum-stick appearance.
- It is motile and possess peritrichate flagella.
- It occurs singly and occasionally in chains.
Pathogenic Clostridia Cultural characteristics:
- Cl. Tetani is strictly an anaerobe.
- It grows at 37°C and pH. 7.4.
1. Robertson cooked meat broth.
- Growth occurs as turbidity.
- Some gas formation occurs.
- Meat is not digested but turns black on prolonged incubation.
2. Blood agar media.
- Produces swarming growth.
3. Horse blood agar media.
- Produces alpha-hemolytic colonies.
- These develop into beta-hemolytic due to the production of hemolysin.
Pathogenic Clostridia Laboratory diagnosis:
1. Direct microscopy.
- Gram staining shows gram-positive bacilli with drums tick appearance.
2. Culture.
- Blood agar media.
- The specimen is inoculated on one-half of blood agar plate at 37oC for 24 – 48 hours anaerobically.
- It shows swarming growth.
- Cooked meat broth (CMB)
- The specimen is inoculated in three tubes of CMB.
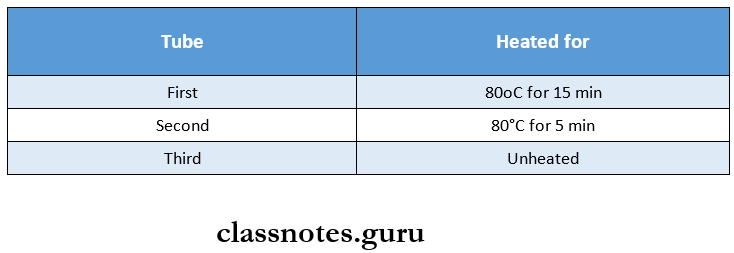
-
- Heating kills vegetative bacteria.
- These tubes are incubated at 37°C and subcultured on blood agar plates for 4 days.
3. Pathogenicity test.
- Blood agar plates are used.
- Tetanus antitoxin – 1500 units/ml is spread over one-half of the plate.
- The suspected C. Tetani strains are stab-inoculated on each half of the plate.
- This is incubated anaerobically for 2 days.
Pathogenicity test Result:
- Toxigenic strains shows hemolysis around colonies in one half of the plate which does not contain antitoxin.
4. Animal inoculation.
- 0.2 ml of 2 – 4 days old cooked meat culture is injected into the tail of 2 mice.
- One of them that has received tetanus antitoxin – 1000 units one hour before acting as a control.
Animal inoculation Result:
- Test animal (without antitoxin)
- Symptoms begin within 12 – 24 hours.
- Stiffness of tail occurs.
- Rigidity then proceeds to one leg, another leg, the trunk, and the forelimb.
- Death occurs within 2 days.
- Control animal (with antitoxin)
- No change occurs due to neutralization of toxin with antitoxin.
Clostridium Short Essays
Question 1. Immunization against tetanus
(or)
Prophylaxis of tetanus.
Answer:
1. Surgical prophylaxis.
- Aims at the removal of foreign bodies, blood clot, etc.
- It involves procedures like simple cleansing to radical excision.
2. Antibiotic prophylaxis.
- It destroys or inhibits tetanus bacilli.
- By this production of toxins is prevented.
- It involves use of long-acting penicillin or erythromycin.
3. Immunization.
- Active immunization.
- It is achieved by tetanus toxoid which is available as a plain toxoid or adsorbed on aluminum hydroxide or phosphate (APT),
- Three doses of 0.5 ml are given intramuscularly.
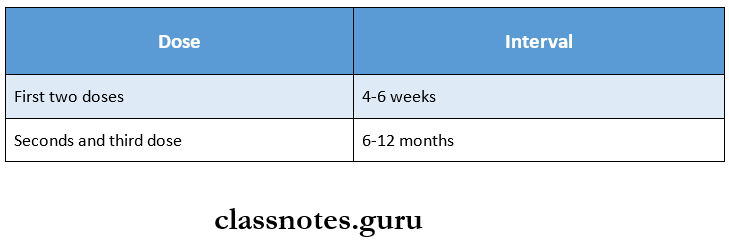
-
- Booster dose is given after 10 years.
- Tetanus toxoid is given along with diphtheria toxoid and pertussis vaccine (DPT).
- First dose – 6 weeks
- Second dose – 10 weeks
- Third dose – 14 weeks
- Booster dose – 18 months or 5 years
- Passive immunization.
- It is achieved by antitetanus serum (ATS) prepared from hyperimmune horses.
- 1500 IU of it is given intramuscularly immediately after wounding.
- It may cause hypersensitivity, to avoid it human antitetanus immunoglobulin (HTIG) is given as 250 units.
- Combined immunization.
- It involves the first dose of
- Tetanus toxoid – on one arm.
- ATS or HTIG – on another arm.
- Second and third doses of tetanus toxoid are given at monthly intervals.
- It involves the first dose of
Question 2. Tetanus OR lockjaw.
Answer:
Tetanus is an acute infection of the nervous system characterized by intense activity of motor neurons and resulting in severe muscle spasms.
Tetanus Etiopathogenesis:
- It is caused by an exotoxin produced by Clostridium tetani bacilli.
- This acts at the synapse of the interneurons of inhibitory pathways and motor neurons to produce a blockade of spinal inhibition.
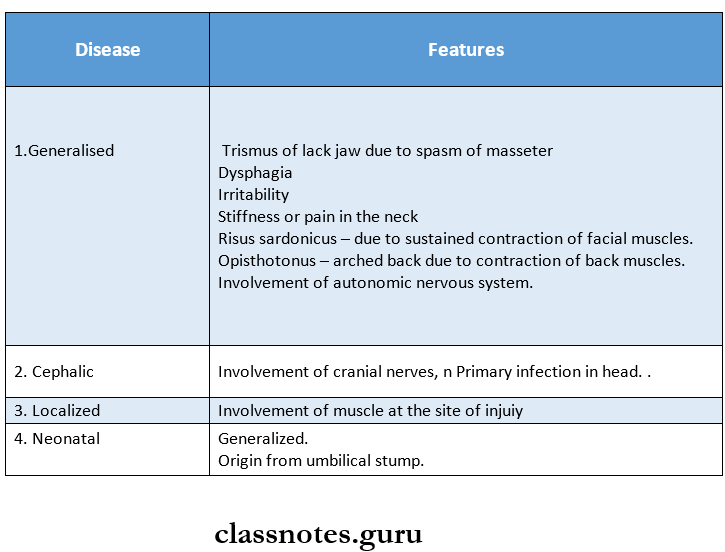
Tetanus Clinical features:
Incubation period – 6 – 10 days.
Tetanus Treatment:
1. General measures.
- Cardiopulmonary monitoring.
- Sedation.
- Airway maintenance.
2. Antibiotics.
- Includes antibiotics like metronidazole.
3. Antitoxin.
- HTIG is given, 3000 – 6000 units 1M
4. Prophylaxis – includes.
- Wound debridement.
- Booster doses of tetanus toxoid.
5. Unimmunised individuals are given.
- ATS – 1500 units or
- HTIG – 250 units.
Clostridium Short Question And Answers
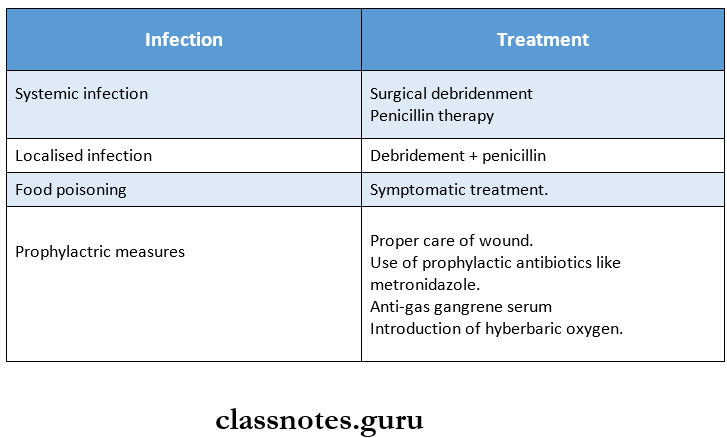
Question 1. Prophylaxis and treatment of gas gangrene.
Answer:
Question 2. Toxins of Cl. Tetani.
Answer:
1. Tetanolysis.
- Heat labile
- Oxygen labile
- Causes hemolysis on blood agar.
- May act as leukotoxin.
2. Tetanospasmin.
- Heat labile.
- Oxygen stable.
- Gets rapidly destroyed by proteolytic enzymes.
- Blocks release of neurotransmitters.
- Neurotoxin.
- Responsible for manifestations of tetanus.
Question 3. Nagler’s reaction.
Answer:
It is a cultural characteristic of C. Welchii.
Nagler’s reaction Method:
- Cl. Welchoi is grown on a media containing.
- 6 % agar.
- 5 % hide’s peptic digest of sheep blood.
- 20% human serum or 5% egg yolk.
- Neomycin sulphate
- It is collected in a plate, half of which contains antitoxin.
- It is incubated at 37oC for 24 hours.
Nagler’s reaction Result:
1. Colonies without antitoxin.
- Surrounded by opacity.
2. Colonies with antitoxin.
- Do not show any opacity.
Nagler’s reaction Mechanism:
- Alpha toxin splits lecithin into phosphorylcholine and diglyceride.
- This lipid deposit results in opacity.
Question 4. Prevention and treatment of botulism.
Answer:
1. Spore germination prevented by
- Maintaining food in an acid pH, by use of fruit preservatives.
- Storage of food at 4°C or colder.
2. Prevention of infant botulism.
- Preventing consumption of honey or food containing it in infants younger than 1 year.
Botulism Treatment:
- Administration of metronidazole or penicillin
- Trivalent botulinium antitoxin.
- Ventilatory support.
