Osseous Surgery Definition
Respective Osseous Surgery
- Respective Osseous Surgery is defined as a procedure by which changes in the alveolar bone can be accomplished to rid it of deformities induced by the periodontal disease process or other related factors such as exostosis and tooth supra eruption.
Osteoplasty
- Osteoplasty is the reshaping of bone without removing tooth-supporting bone
Ostectomy
- Ostectomy is the removal of tooth-supporting bone
Read And Learn More: Periodontics Question and Answers
Osseous Surgery Definition Important Notes
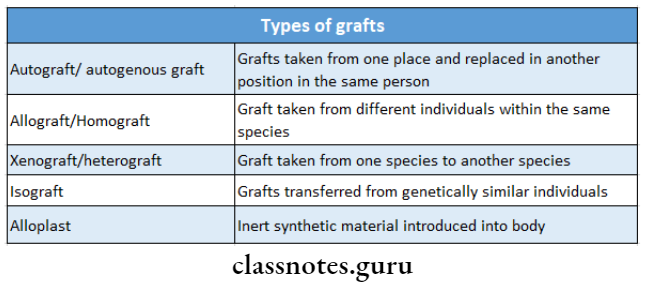
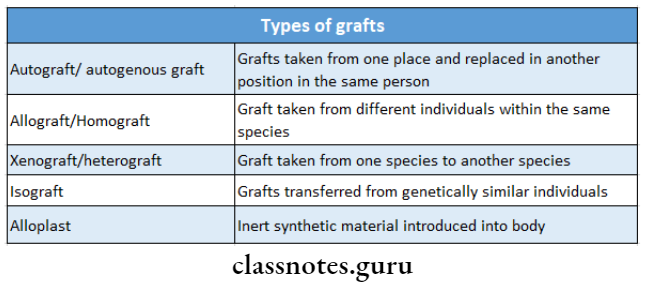
1. Types of grafts
2. Indications for resection osseous surgery
- Interdental craters
- One wall osseous defects
- Wide shallow two-wall defects
- Exostosis
- Supra erupted teeth
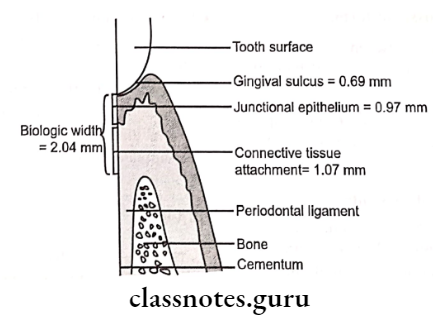
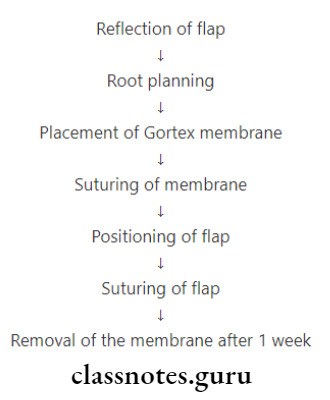
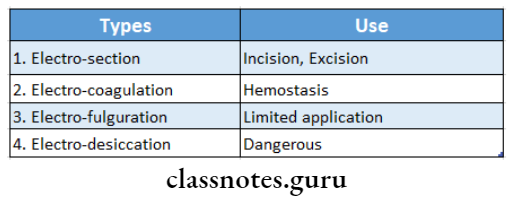
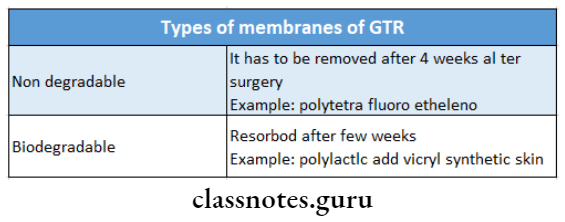
3. Guided tissue regeneration, GTR
- It is based on the assumption that only the periodontal ligament cells have the potential for regeneration of the attachment apparatus of the tooth
- The technique consists of placing barriers of different types to cover the bone and periodontal ligament to prevent the migration of epithelium
4. Bioglass
- It is an alloplastic or non-graft material
- It consists of sodium and calcium salts, phosphates and silicon dioxide
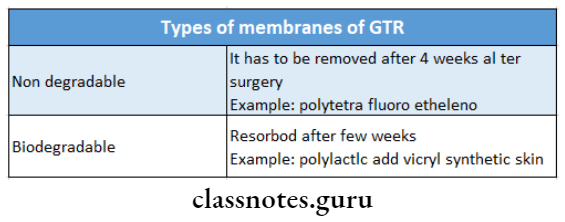
5. Types of membranes of GTR
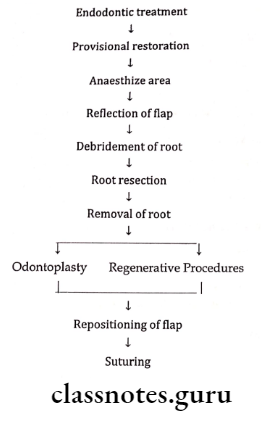
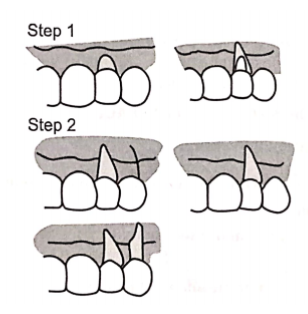
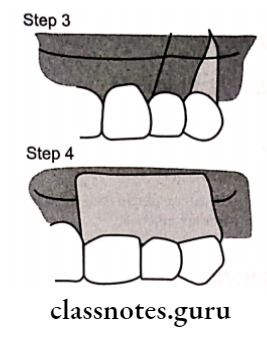
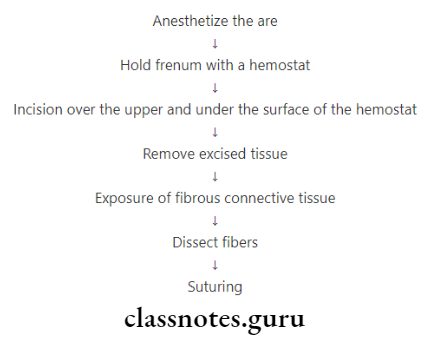
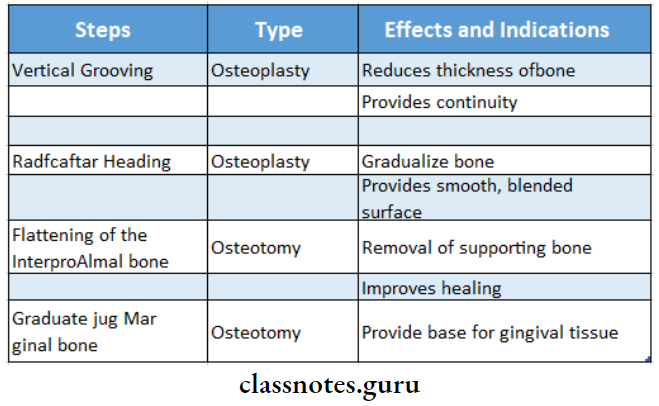
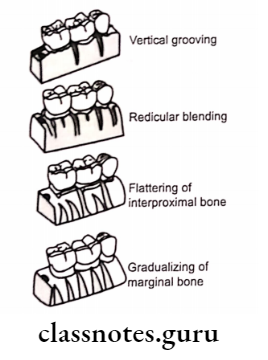
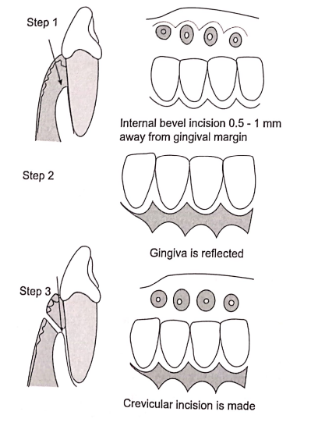
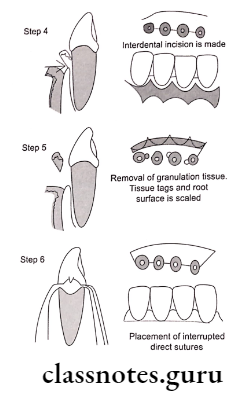
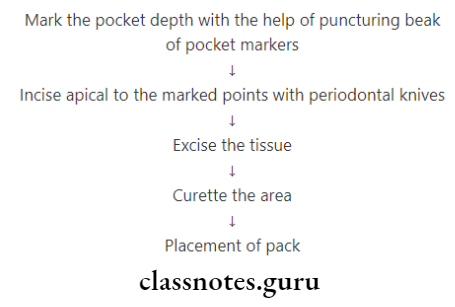
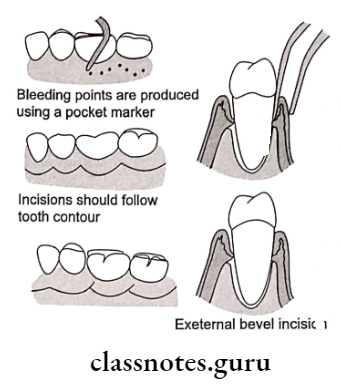
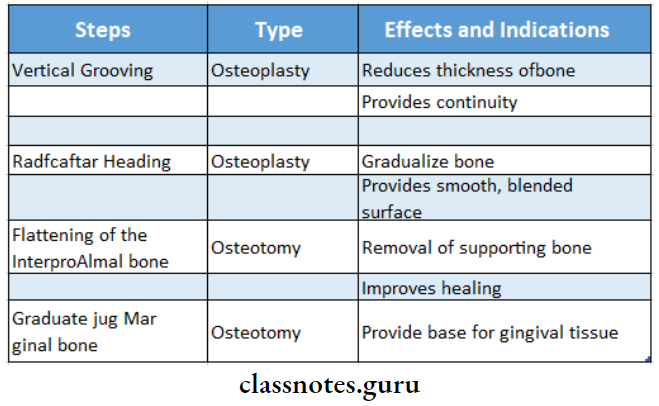
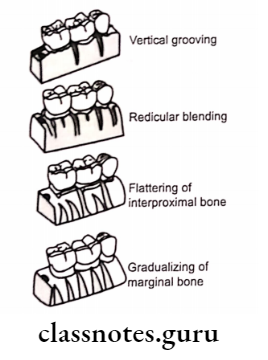
6. Steps in osseous resection surgery
- Vertical grooving
- Radicular blending
- Flattening interproximal bone
- Gradualizing marginal bone
Osseous Surgery Long Essay
Question 1. Define Respective Osseous Surgery. Mention its indication, contraindications and steps involved in it.
Answer:
Respective Osseous Surgery Definition:
- Respective Osseous Surgery is defined as a procedure by which changes in the alveolar bone can be accomplished to rid it of deformities in- duced by the periodontal disease process or other related as exostosis and tooth supra eruption.
Respective Osseous Surgery Indications:
- One wall defect
- Thick bony margins
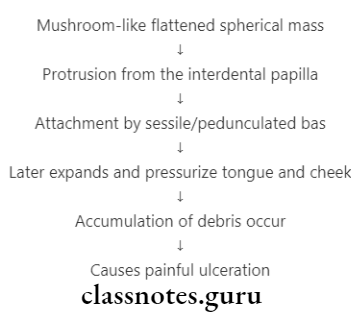
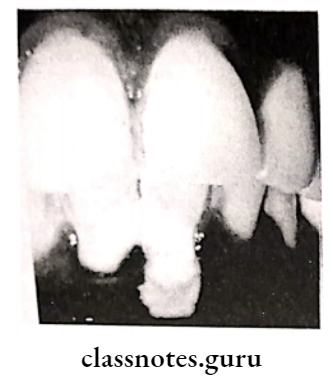
Respective Osseous Surgery Shallow Crater:
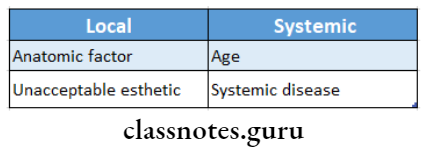
Contraindication:
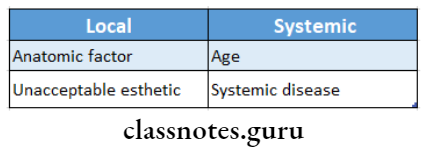
Respective Osseous Surgery Orally:
- Improper oral hygiene
- High DMFT
- Dentinal Hypersensitivity
- Advanced Periodontitis
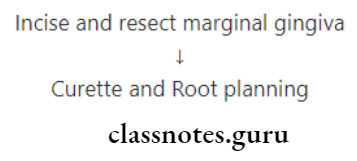
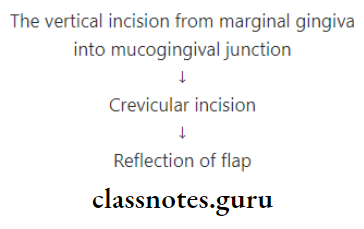
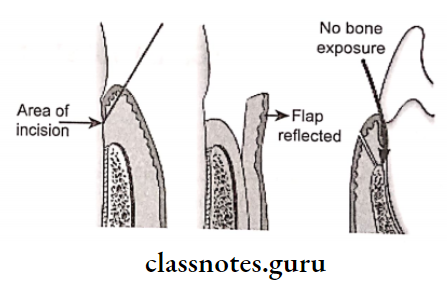
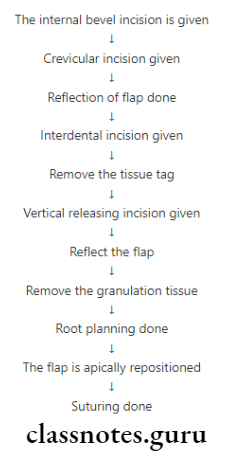
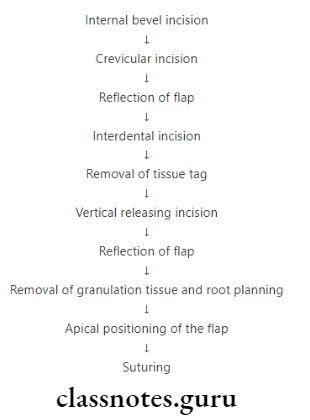
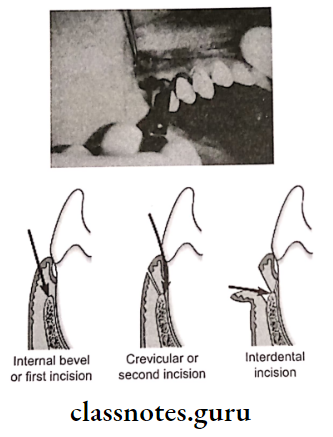
Respective Osseous Surgery Steps:
- Vertical Grooving
- Radicular blending
- Flattening of interproximal bone
4. Gradualizing marginal bone
Following these steps
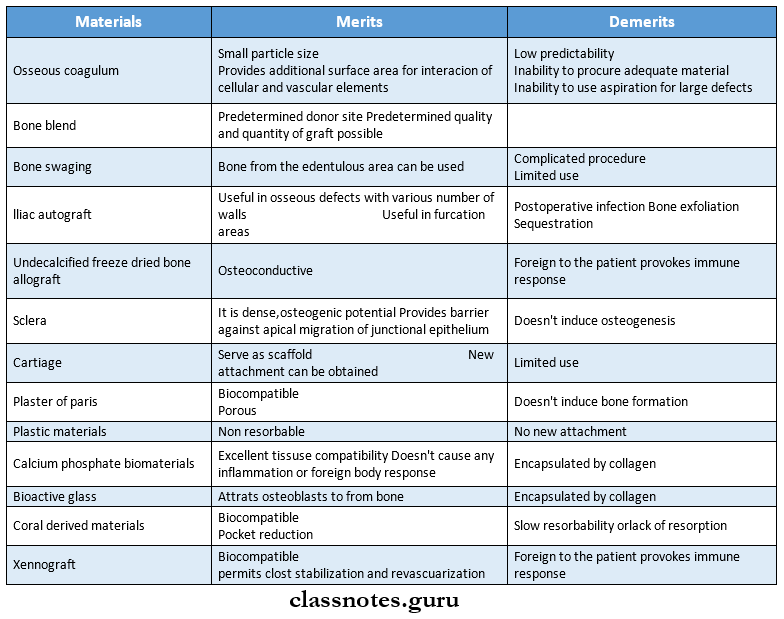
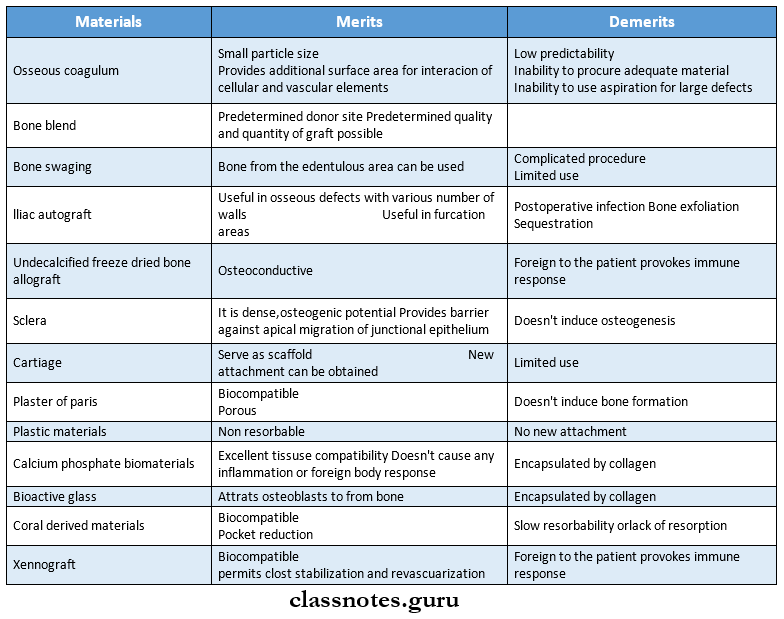
Question 2. Classify bone replacement grafts and describe the merits and demerits of each type
Answer:
Classification of replacement grafts:
Replacement grafts Autogenous bone grafts:
1. Bone from intraoral sites:
- Osseous coagulum
- Bone blend
- Intraoral cancellous bone marrow transplants
- Bone swaging
2. Bone from extraoral sites:
Replacement grafts Allografts:
- Undecalcified freeze-dried bone allograft
- Demineralized freeze-dried bone allograft
replacement grafts Xenografts:
Non-bone graft materials:
- Sclera
- Cartilage
- Plaster of Paris
- Plastic materials
- Calcium phosphate biomaterials
- Bioactive glass
- Coral derived materials
- Bioactive glass
Question 3. Define osseous surgery. Discuss various osseous grafting procedures.
Answer:
Osseous grafting Definition:
- Osseous Grafting is defined as a procedure by which changes in the alveolar bone can be accomplished to rid it of deformities induced by the periodontal disease process or other related factors such as exostosis and tooth supra eruption
Osseous grafting Procedures:
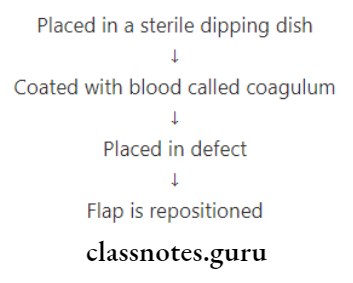
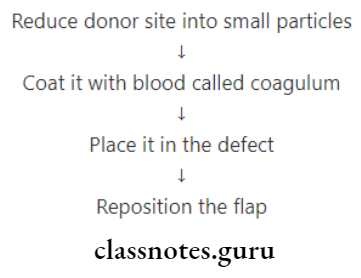
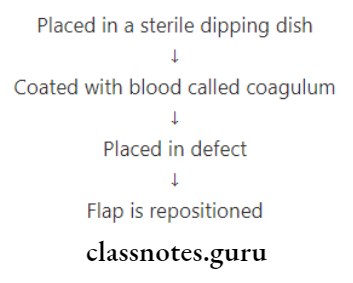
1. Osseous coagulum:
- Donor Sites:
- Lingual ridge
- Exostoses
- Edentulous ridges
- Bone distal to terminal tooth
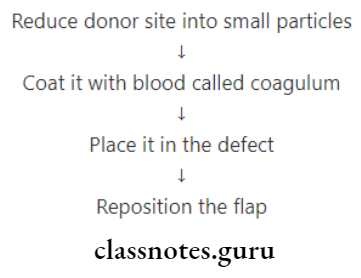
Osseous grafting Technique:
Bone is removed from the donor site by carbide bur
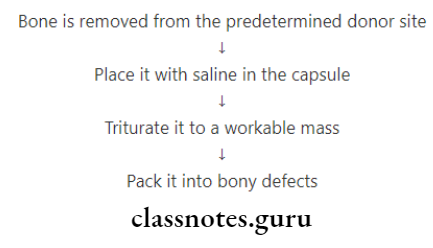
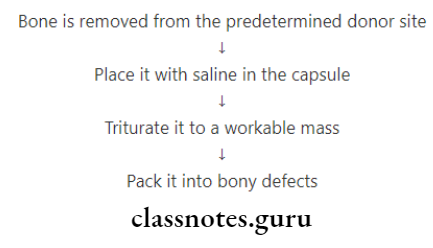
2. Bone blend:
3. Cancellous bone marrow transplants:
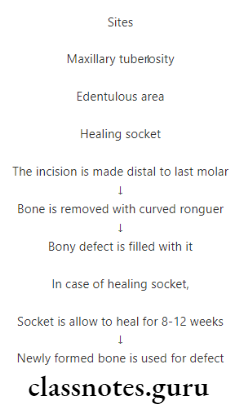
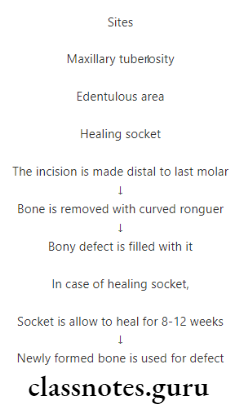
4. Bone swaging:
- Bone from an edentulous area adjacent to the defect is pushed into contact with the root surface without fracturing the bone at its base
5. Allografts:
Question 4. Describe in brief various reconstructive Osseous techniques.
Answer:
Osseous Techniques Reconstructive Osseous Surgery:
Osseous techniques Non-Graft associated new attachment.
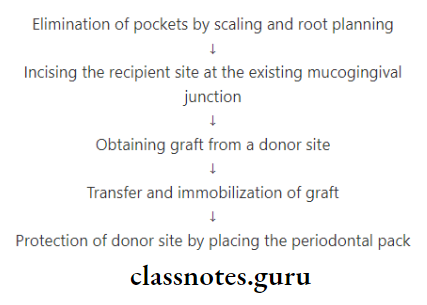
1. Removal of Junctional/Pocket Epithelium through the following
- Curettage
- Chemical agents
- Sodium sulfide
- Phenol
- Camphor
- Antiform
- Ultrasonic methods- Lacks tactile sensation
- Surgical methods
- ENAP
- Gingivectomy
- Widman flap
- Coronally displaced flap
2. Prevention of Epithelial Migration.
- GTR
- Degradable – Collagen
- Non-degradable – Millipore
- Clot stabilization, wound protection and space creation by
- Coronally displaced flap
- Root conditioners
- Citric acid
- Fibronectin
- Tetracycline
3. Growth Factors (GF)
- Regulates events in wound healing
- Example: Platelet-derived GF
4. Enamel Matrix Proteins
- Favours periodontal regeneration
Osseous techniques Graft-associated new attachment
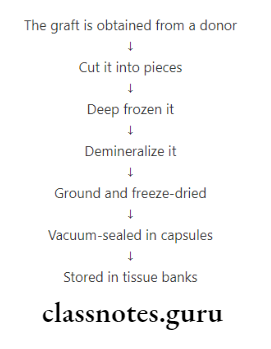
1. Allografts:
- Tissue transfer between individuals of the same species
2. Xenografts:
- Grafts from different species
- Causes severe allergic reactions
3. Alloplasts:
- For restoration of the periodontium
- Example: Sclera, dura, Cartilage
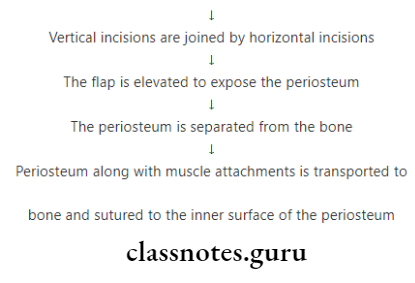
Osseous techniques Combined techniques
- Combination of both graft and non-graft-associated methods
Osseous Surgery Short Essays
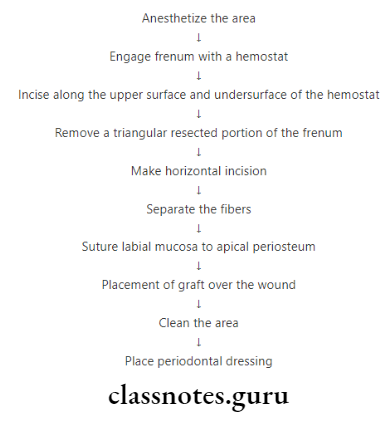
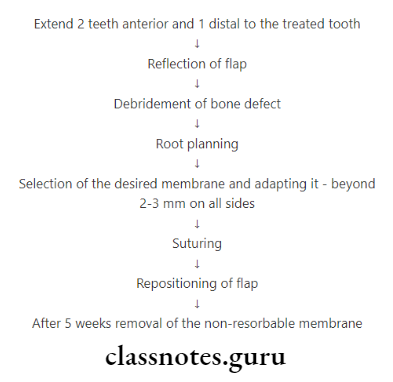
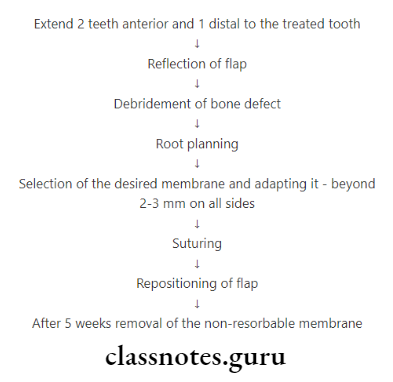
Question 1. GTR (Guided Tissue Regeneration).
Answer:
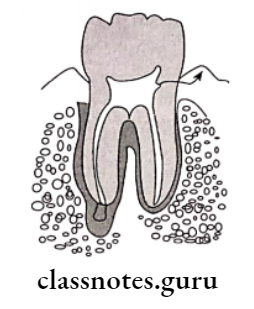
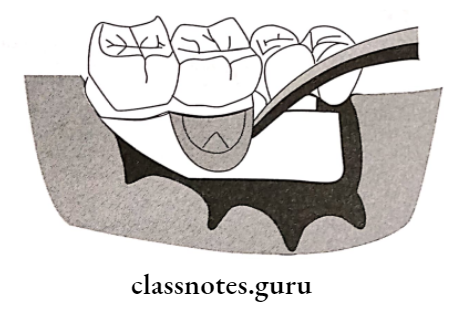
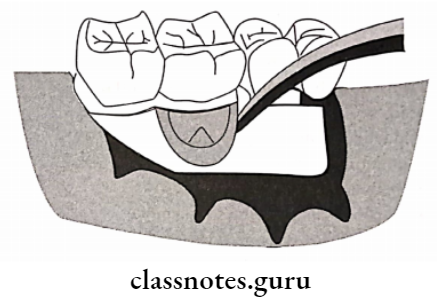
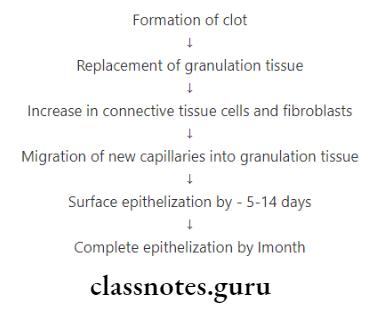
- After the flap surgery, epithelium from the excised margin may proliferate apically.
- This results in the formation of long Junctional epithelium
- Thus this should be prevented
- To prevent this, a membrane is placed between healing connective tissue and cementum
- Such a membrane is (GTR)
GTR Types:
- Degradable – Collagen, Guidor membrane
- Nondegradable – Millipore, Teflon membrane
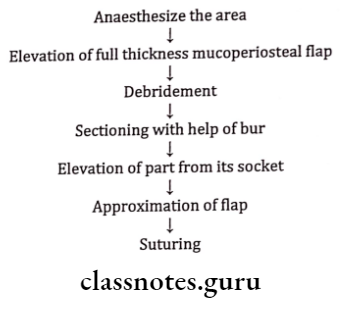
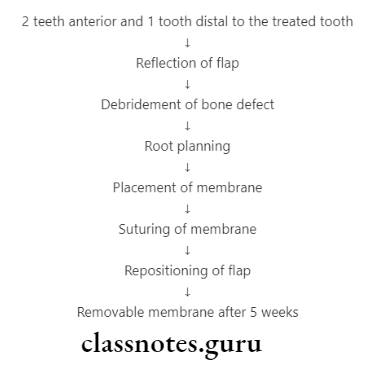
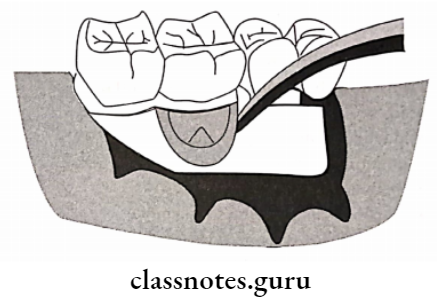
GTR Procedure:
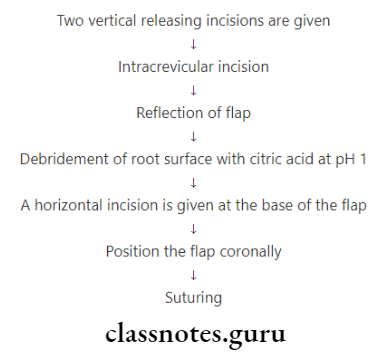
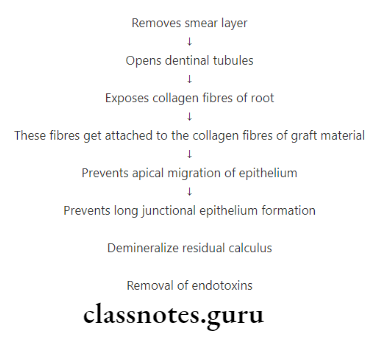
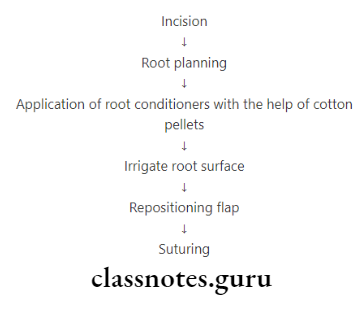
Question 3. Root conditioners/Root Biomodification effects.
Answer:
Root Conditioners Effects:
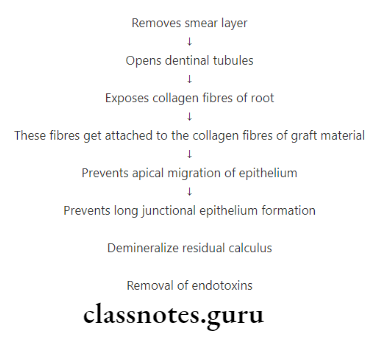
Root Conditioners Examples:
- Citric acid at pH 1
- Fibronectin
- Tetracycline
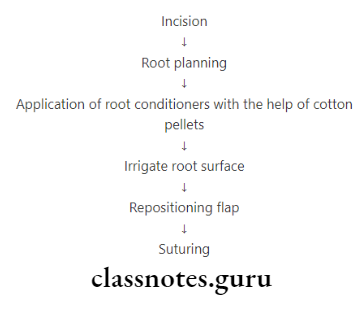
Root Conditioners Procedure:
Question 3. Non-bone graft materials
Answer:
Non-Bone Graft Materials:
- Sclera
- Cartilage
- Plaster of Paris
- Plastic materials
- Calcium phosphate biomaterials
- Hydroxyapatite
- Tricalcium phosphate
- Calcitite
- Bioactive glass-consists of
- Sodium and calcium
- Phosphates
- Silicon dioxide
- Coral derived materials
- Natural coral material
- Coral derived porous hydroxyapatite
Question 4. Define osteotomy and osteoplasty. Explain how they differ from each other.
Answer:
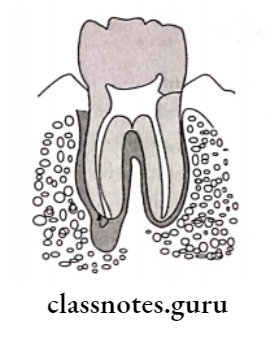
Ostectomy:
- It is a procedure of radicular and inter-radicular removal of supporting bone to eliminate osseous deformities
- It is done by a technique which involves the removal of supporting bone to produce a positive gingival and osseous architecture
Ostectomy Indications:
- To reduce hemisepta-like defects and shallow intrabony defects
- To correct reverse architecture induces by periodontal disease
- Moderate to advanced furcation involvements
- Elimination of interdental craters
- Intrabony defects not amenable to regeneration
Ostectomy Contraindications:
- Anatomic limitations like prominent external oblique ridge or zygomatic arch, etc
- Esthetic limitations like high smile line anteriorly
- Availability of effective alternative treatment
- Areas of insufficient remaining attachment
Ostectomy Advantages:
- Pocket elimination
- Establishment of physiologic gingival and osseous architecture
- Establishment of favourable prosthetic environment Loss of attachment
- Increased root sensitivity
- Esthetic compromise
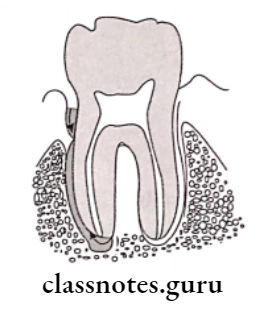
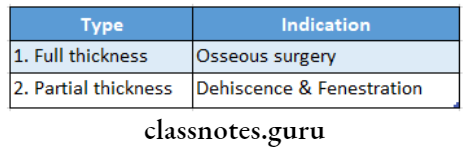
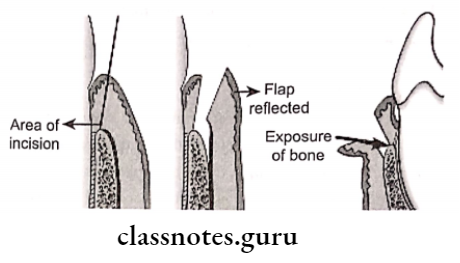
Ostectomy Osteoplasty:
- It is described by Friedman in 1955
- It is a procedure of reshaping the alveolar process to achieve a more physiological form without the removal of supporting bone
Ostectomy Indications:
- Removal of buccal and lingual bony ledges or tori
- Pocket elimination
- Shallow intrabony defects
- Shallow craters
- Thick interproximal areas
- Incipient furcation defects that do not necessitate re-moving supporting bone
- Buttressing bone formation or lipping
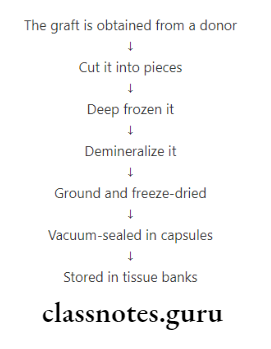
Question 5. Allograft
Answer:
Allografts are tissue transfer between individuals of the same species but with different genetic composition
Allograft Commercial products
- FDBA (Freeze Dried Bone Allograft)-osteoconductive
- DFDBA (Demineralized Freeze-Dried Bone Allograft)
Allograft Disadvantages:
- Foreign to the patient
- Provokes immune response
Osseous Surgery Short Question And Answers
Question 1. Types of Osseous Surgery.
Answer:
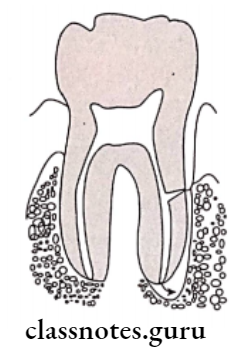
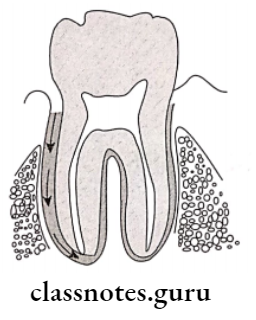
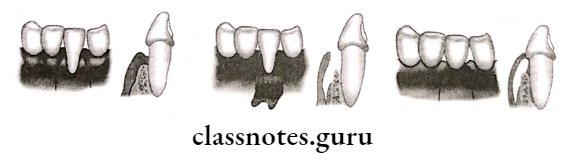
1. Depending on the relative position of interdental to radicular bone
- Positive Architecture
- Radicular bone apical to interdental bone.
- Negative Architecture
- Interdental bone apical to radicular bone.
- Flat Architecture
- Interdental & radicular bone reduced up to the same height.
- Ideal
- Interproximal bone is coronal to that of facial/lingual surfaces.
2. Depending on the thoroughness of the techniques
- Definitive osseous reshaping
- Further reshaping would not improve the overall result.
- Compromise osseous reshaping
- Requires osteotomy procedures.
3. Additive-Restores bone to original levels
- Subtractive Restores bone to the level existing at the time of surgery or apical to it.
Question 2. Instruments of Osseous Surgery.
Answer:
Osseous Surgery Hand Instruments:
- Ronguers Freidman & Blumental
- Interproximal files – Schluger & Sugarman
- Back action chisels
- Oschsenbein chisels
Osseous Surgery Rotary:
- Carbide round burs
- Slow-speed handpiece
- Diamond burs
Question 3. Growth Factors.
Answer:
Growth Factors are polypeptide molecules released by the cells in osteoinductive the inflamed area
Growth Factors Secreted
- Macrophages
- Endothelial cells
- Fibroblasts
- Platelets
Growth Factors Effects:
- Regulates events in wound healing
- Promotes proliferation of fibroblasts
- Favours bone formation
Growth Factors Examples:
- Platelet-derived growth factors (PDGF)
- Insulin-like growth factor (IGF)
- Fibroblast growth factor (FGF)
Question 4. Enamel Matrix Proteins.
Answer:
Namely, amelogenin is secreted by Hertwigs Epithelial root sheath during tooth development and induces accel-cellular cementum formation.
Matrix Proteins Actions:
- Enhance periodontal regeneration
- Promote bone cell attachment
- Increases proliferation of more immature bone cells
- It is not osteoinductive, but it is osteopromotive in that it stimulates bone formation when combined with demineralized freeze-dried bone allograft.
Question 5. Osseous Coagulum.
Answer:
Osseous Coagulum Technique:
Osseous Coagulum Donor Site:
- Lingual ridge on mandible
- Exostosis or tori
- Edentulous ridges
- Bone distal to the terminal tooth.
Osseous Coagulum Advantages:
- Better resorbed
- Provides additional surface area
Osseous Coagulum Disadvantages:
- Low predictability
- Poor visibility
Question 6. Bone Swaging.
Answer:
Bone Swaging Requirement:
- An edentulous area adjacent to the defect
Bone Swaging Procedure:
- Push the bone of the edentulous area into the defect
- Avoid fracture of basal bone
Bone Swaging Disadvantage:
- Complicated procedure
- Limited use
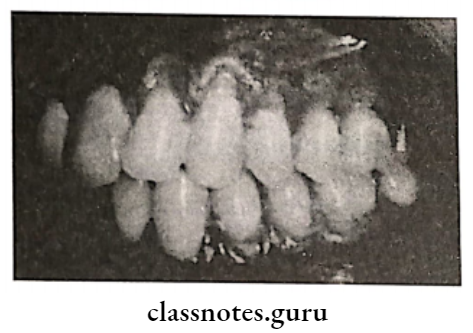
Question 7. Positive architecture
Answer:
When Radicular bone is present apical to interdental bone it is called positive architecture
Question 8. Define root planning.
Answer:
Root planning is a process by which residual embedded calculus and a portion of cementum are removed from the roots to produce a smooth, hard and clean surface
Question 9. Reversed architecture.
Answer:
- The loss of interdental bone produces these defects including the facial and lingual plates without concomitant loss of radicular bone, thereby reversing normal architecture
- Normally interproximal bone is coronal to facial and lingual plates forming a scalloped osseous margin
- When the loss of interdental bone occurs without significant loss of radicular bone, normal scalloping gets reversed
- It is more common in the maxilla
Question 10. Osteoplasty
Answer:
- Osteoplasty is described by Friedman in 1955
- Osteoplasty is a procedure of reshaping the alveolar process to achieve a more physiological form without the removal of supporting bone
Osteoplasty Indications:
- Removal of buccal and lingual bony ledges or tori
- Pocket elimination
- Shallow intrabony defects
- Shallow craters
- Thick interproximal areas
- Incipient furcation defects that do not necessitate re-moving supporting bone
- Buttressing bone formation or lipping
Question 11. Ostectomy
Answer:
- Ostectomy is a procedure of radicular and inter-radicular removal of supporting bone to eliminate osseous deformities
- Ostectomy is done by a technique which involves the removal of supporting bone to produce a positive gingival and osseous architecture
Ostectomy Indications:
- To reduce hemisepta-like defects and shallow intrabony defects
- To correct reverse architecture induces by periodontal disease
- Moderate to advanced furcation involvements
- Elimination of interdental craters
- Intrabony defects not amenable to regeneration
Question 12. Allografts.
Answer:
Tissue transfer between individuals of the same species but with different genetic composition
Allografts Commercial Products
Allografts Name – Effect
1. FDBA [Freeze-dried Bone allograft]
- Osteoconductive
- 50% bone file
2. DFDBA [Demineralized Freeze-dried bone allograft]
Question 13. Define osteoconduction and osteoinduction.
Answer:
Osteoconduction: It is an effect by which the matrix of the graft forms a scaffold that favours outside cells to penetrate the graft and form new bone
Osteoinduction: A process by which graft material is capable of promoting cementogenesis, osteogenesis and new periodontal ligament.
Osseous Surgery Definition Viva Voce
- The goal of osseous therapy is to reshape marginal bone
- Respective osseous surgery is performed in combination with apically displaced flap
- Interproximal bone normally is pyramidal in shape
- The level of interdental bone is the same as that of radicular bone in a flat architecture
- The buccolingual contour of the interdental bone in the pose- ous crater appears as that of the opposite of CEJ
- Gore-tex is a PTFE membrane
- Biobrane is a synthetic skin
- Emdogain is an enamel matrix protein
- Graft from different individuals from the same species is called allograft
- Enamel matrix protein is osteoconductive
- Boplant is xenograft
- The osseous coagulum is a mixture of bone dust and blood
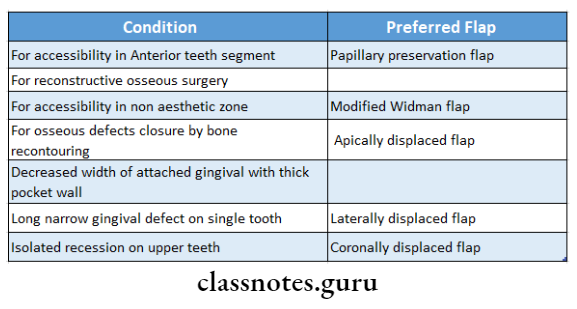
- Flap best suited for grafting is the papilla preservation flap
- Plaster of Paris resorbs completely in 1-2