Cranial Nerves Introduction
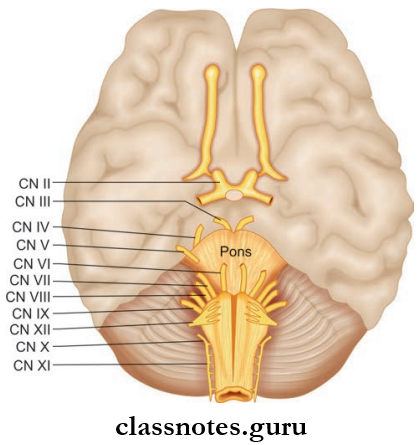
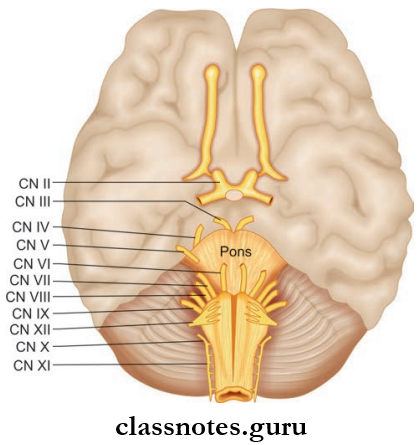
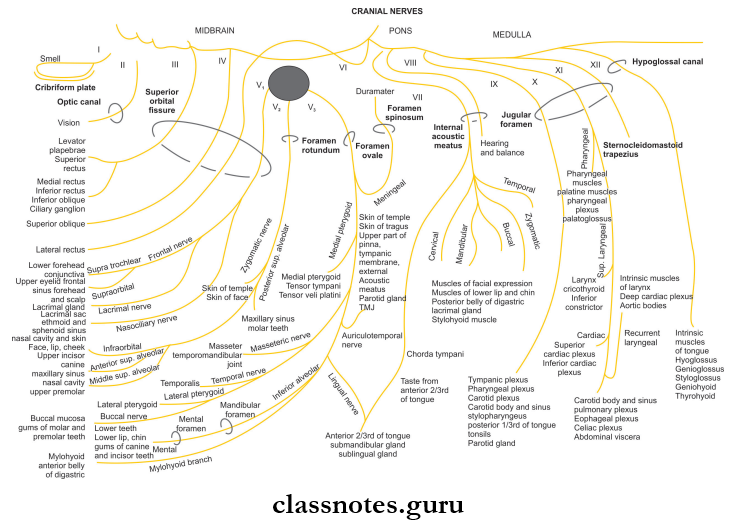
There are twelve pairs of cranial nerves designated by Roman numerals.
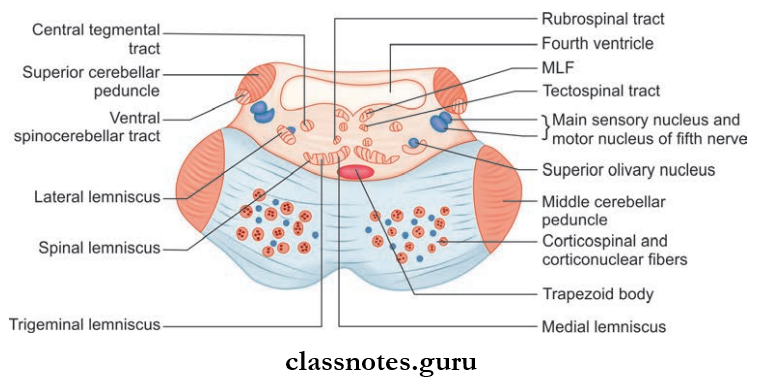
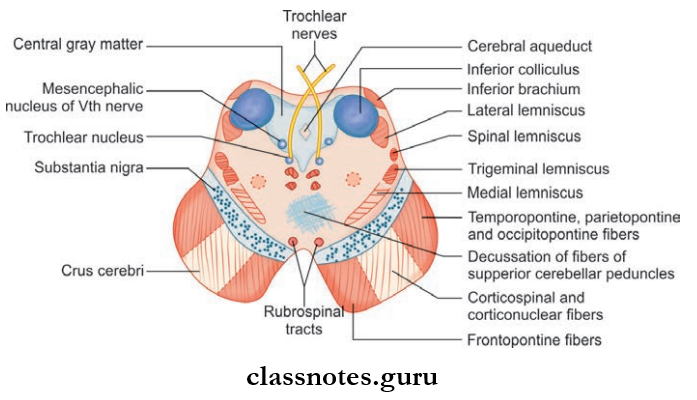
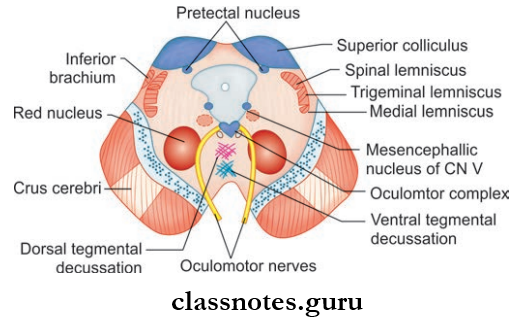
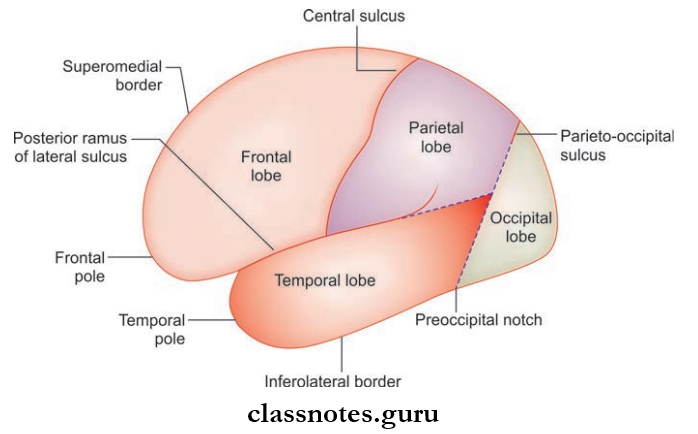
The first two pairs are attached to the forebrain and the next 10 are attached to the brainstem, i.e. 3 and 4 to the midbrain; 5, 6, 7, and 8 to the pons and the 9, 10, 11, and 12 to the medulla.
- They are numbered from 1 to 12 in a craniocaudal sequence of their attachment.
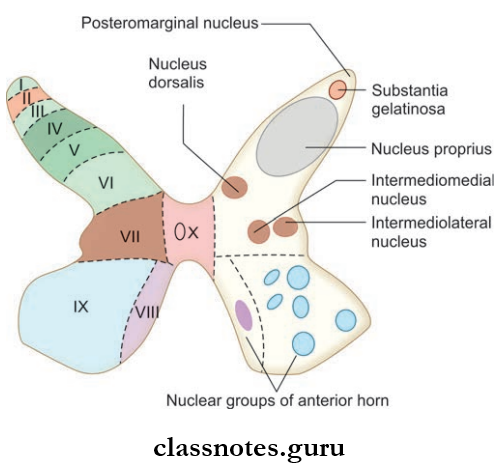
- During development, the middle mantle layer of the neural tube which represents the gray matter differentiated into dorsal alar lamina (sensory) and ventral basal lamina (motor) which are separated by the sulcus limitans.
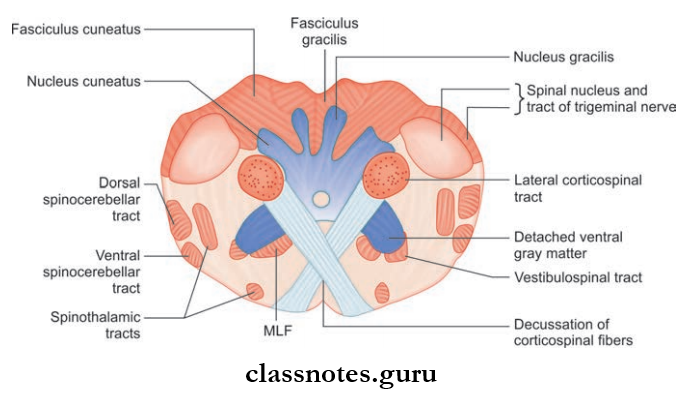
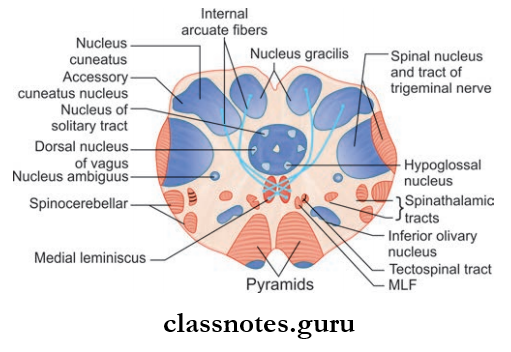
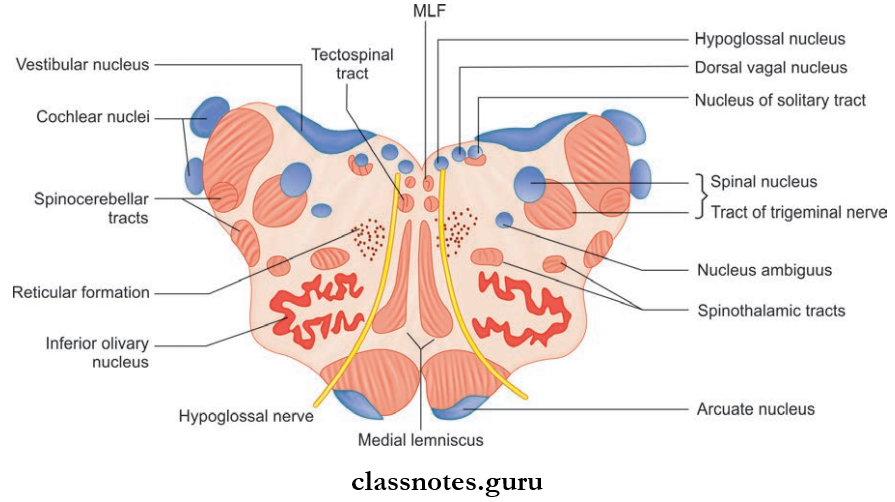
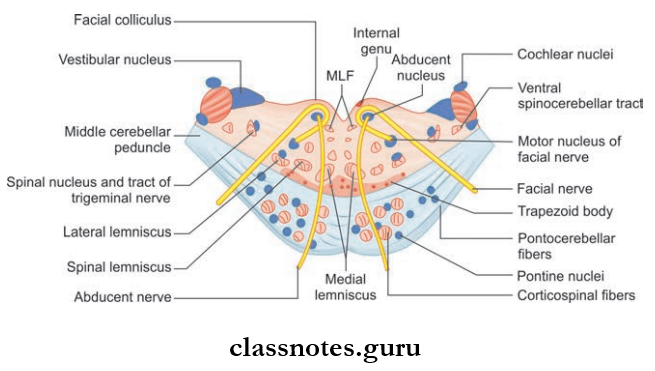
- In the brainstem, the alar and basal lamina lie in the same ventral plane, and the gray matter forms separate longitudinal functional columns. The columns from basal lamina (motor columns) are medial and from alar lamina (sensory) are lateral in position.
- In the spinal cord, the gray matter is differentiated into four functional columns, i.e. two somatic and two visceral functional columns.
- The somatic columns are general somatic efferent (motor or anterior horn) and general somatic afferent (sensory or posterior horn) and they supply the structures derived from somites.
- The visceral columns are general visceral afferent (sensory) and general visceral efferent (motor) and supply the viscera, vessels, and glands.
- In addition to the four functional columns, there are three more columns namely the special visceral efferent (motor) and special visceral afferent (sensory) for the branchial apparatus of the head region and the special somatic afferent (for the special senses).
- Thus a total of seven columns (3 motor and 4 sensory) are formed and each column in turn breaks up into smaller fragments to form nuclei of the cranial nerves.
- A cranial nerve consists of motor fibers (motor nerve) sensory fibers (sensory nerve) or both motor and sensory fibers (mixed nerve).
- The motor fibers arise as outgrowths of axons from motor nuclei situated within the central nervous system (CNS) whereas sensory fibers arise as outgrowths of axons from cells situated within sensory ganglia and terminate in sensory nuclei.
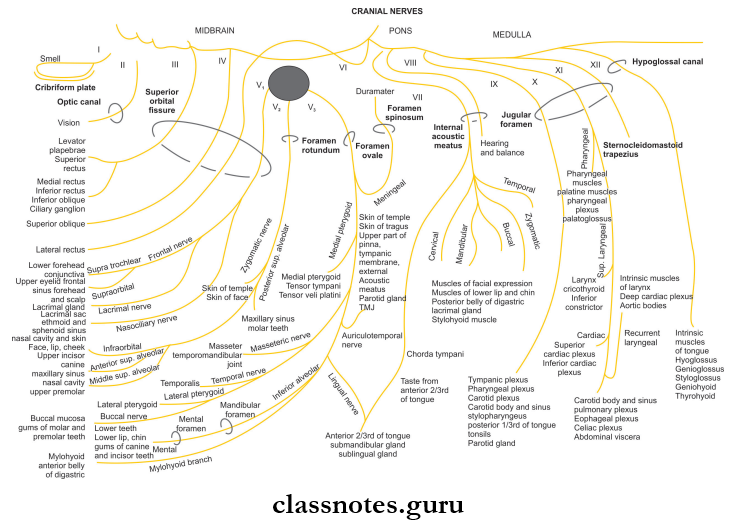
- The Motor Fibers Of The Cranial Nerve Can Be Of The Following Types:
- General somatic efferent (GSE) fiers which supply striated muscles developed from somites.
- Special visceral efferent (SVE) fiers supply muscles developed from mesoderm.
- General visceral efferent (GVE) fibers which are preganglionic parasympathetic fibers and supply glands, smooth muscles of viscera, and blood vessels.
- The Sensory Fibers Of The Cranial Nerve Can Be Of The Following Types:
- General somatic afferent (GSA) fiers carry general sensations of pain, touch, and temperature and proprioceptive sensations of vibration, position, and joint sense.
- General visceral afferent (GVA) fibers carry sensations of distention and ischemic pain from the viscera.
- Special visceral afferent (SVA) fibers carry a special sensation of taste from the tongue.
- Special somatic afferent (SSA) which carries special sensations of smell, hearing, and balance.
Cranial Nerves Question And Answers
Question 1. Write a note on the olfactory nerve.
Answer:
Olfactory Nerve.
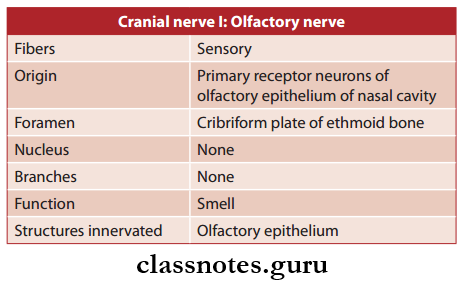
- The Olfactory Nerve is the 1 cranial nerve
- Olfactory Nerve is purely sensory and carries smell from the nasal cavity.
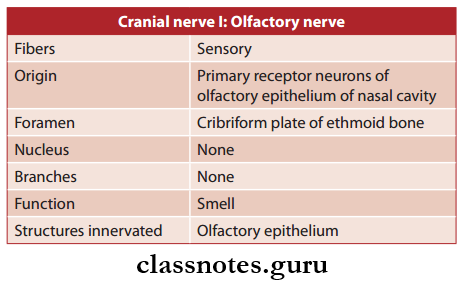
Olfactory Nerve Functional Components: Special somatic afferent fibers carry the special sensation of smell from the olfactory region of the nasal cavity to the olfactory bulb.
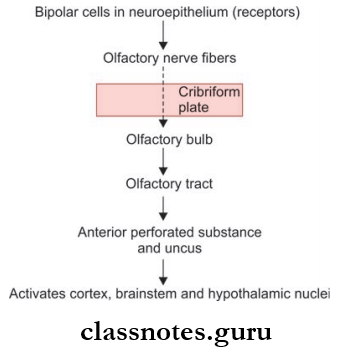
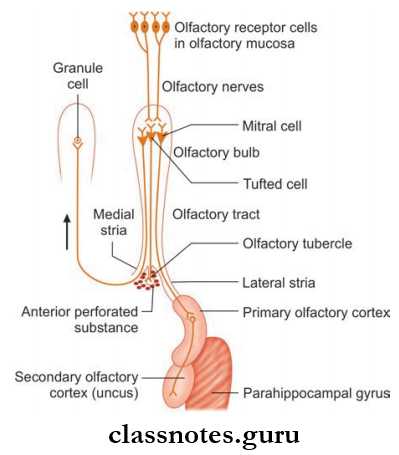
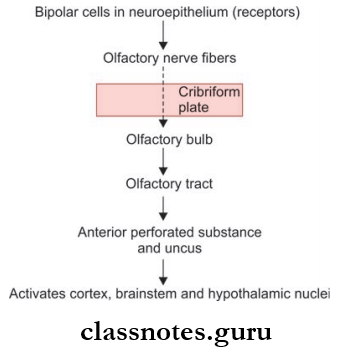
Olfactory Nerve Course And Relations
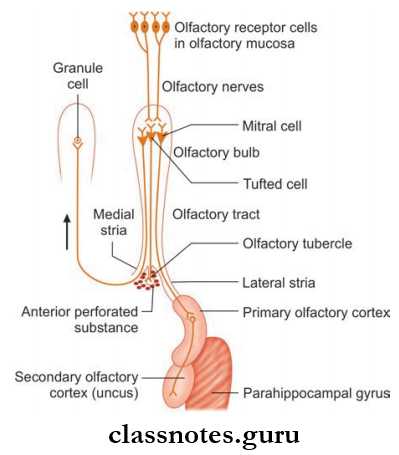
- Olfactory Nerve consists of minute bundles of non-myelinated nerve fibers that arise from the olfactory epithelium of the nasal cavity
- Then it passes through the cribriform plate enters the anterior cranial fossa and terminates in the olfactory bulb
- In the olfactory bulb, they synapse with mitral cells
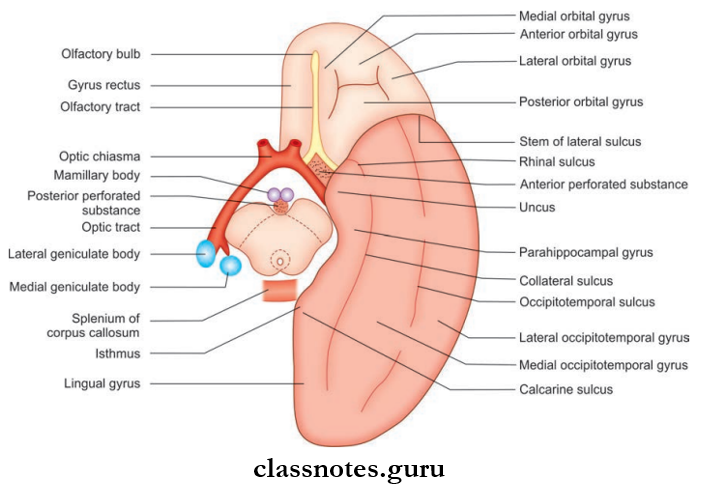
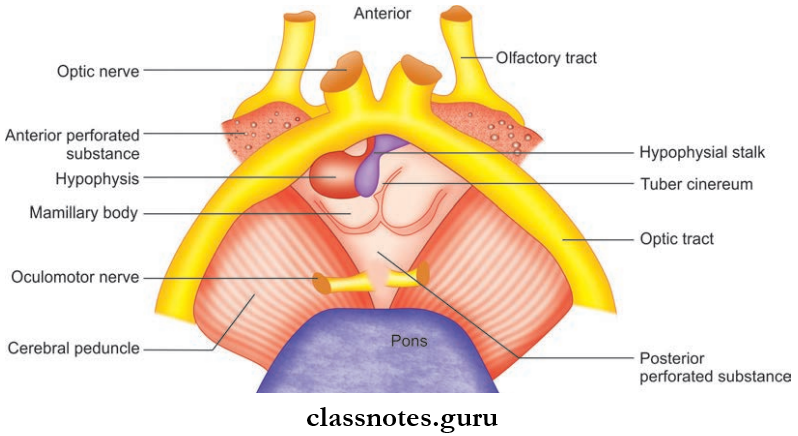
- The neurons from the olfactory bulb form the olfactory tract and widen at the olfactory trigone at the anterior perforated substance
- These neurons are in the form of striae that terminate in the para terminal gyrus and primary olfactory cortex.
Olfactory Nerve Clinical Testing: The olfactory nerve is tested by asking the patient to smell common odors like clove, and peppermint from each side of nose separately with eyes closed.
Olfactory Nerve Applied
- Anosmia refers to the inability to perceive the smell
- Allergic rhinitis can cause temporary olfactory impairment
- In severe head injuries involving the anterior cranial fossa, the olfactory bulb may be separated from olfactory nerves or the nerves may be injured, producing anosmia and cerebrospinal fluid (CSF) leakage.
Question 2. Write a note on the optic nerve.
Answer:
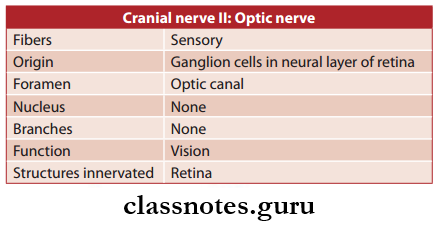
Optic Nerve
- Optic Nerve is the 2 cranial nerve
- Optic Nerve is purely sensory and is responsible for vision.
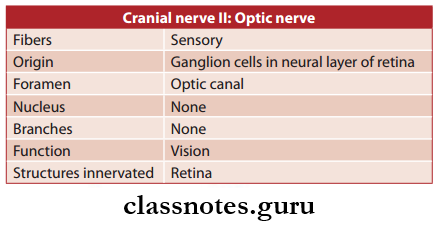
Optic Nerve Functional Components: Special somatic afferent fibers carry a sense of sight from the visual field of the corresponding eye.
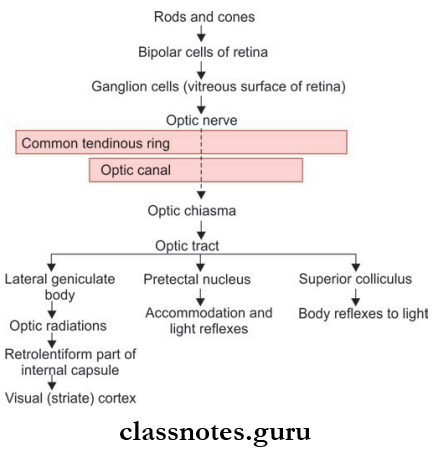
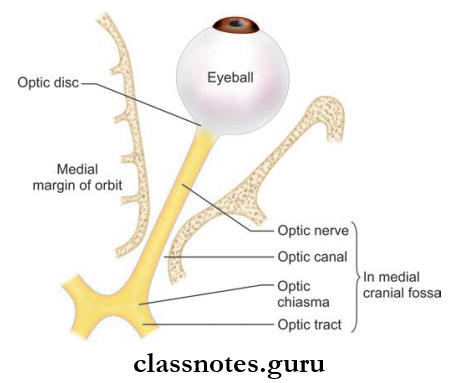
Optic Nerve Course And Relations
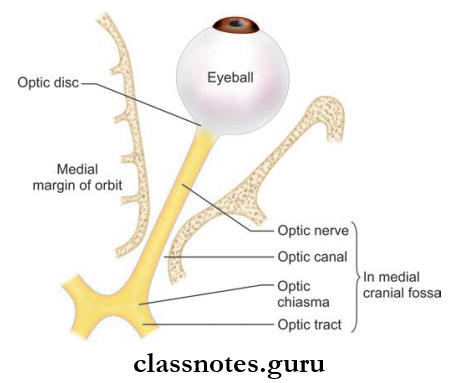
- The fibers of the optic nerve arise from ganglion cells of the retina converge towards the optic disc and pierce the retina, choroid, and sclera to leave the eyeball
- After emerging from the eyeball, fiers unite to form an optic nerve which passes through the orbit and enters into the middle cranial fossa where both optic nerves of two sides unite to form optic chiasma
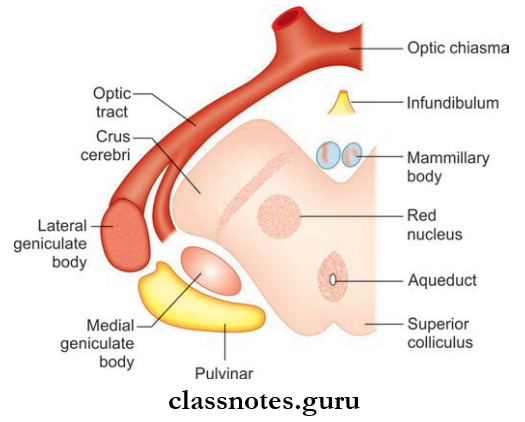
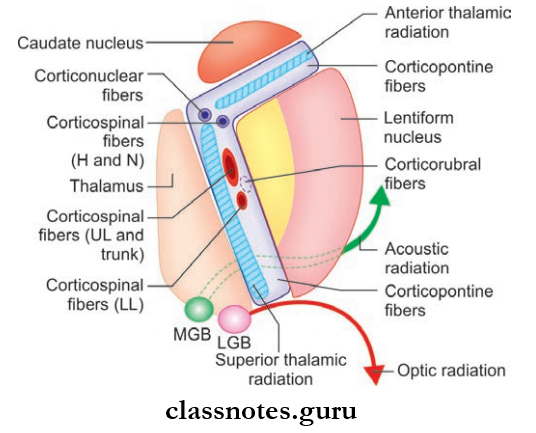
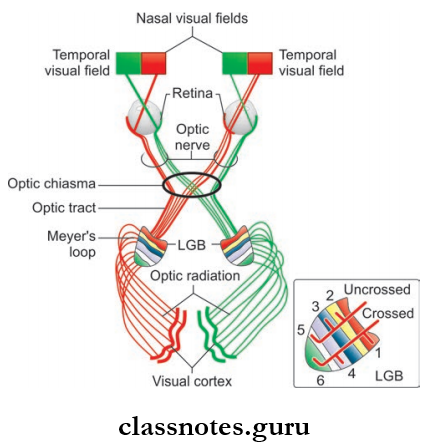
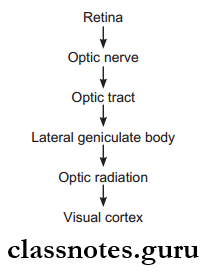
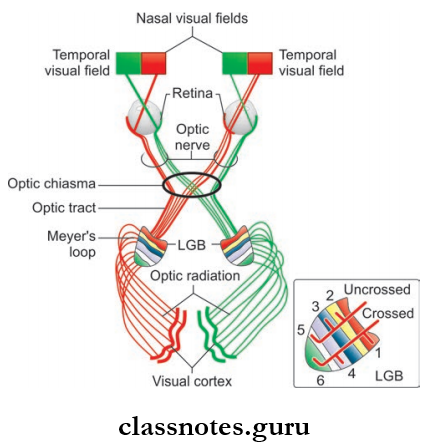
- From the optic chiasma, fibers diverge and are known as optic tracts which relay in lateral geniculate body
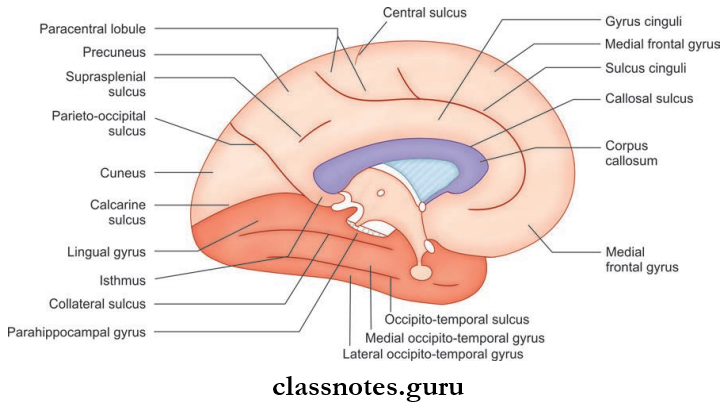
- They run in the retrolenticular part of the internal capsule form optic radiations and terminate in and around the calcarine sulcus of the occipital lobe (visual cortex).
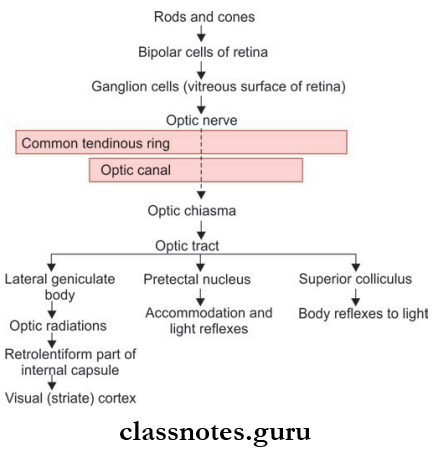
Optic Nerve Visual Pathway
Optic Nerve Parts: Divided into
- Intraorbital part
- Canalicular part
- Intracranial part.
Optic Nerve Clinical Testing
- The nerve is tested by performing tests for:
- Visual acuity of near and distant vision
- Visual field either manually by confrontation method or perimetry
- Color vision by using Ishihara charts
- Light reflexes.
Optic Nerve Applied
- Lesions of the optic pathway may have many pathological causes. Expanding tumors of the brain and the meninges and cerebrovascular accidents are commonly responsible.
- Lesions of the optic nerve may be at different levels with different effects, as follows:
- A complete lesion of the optic nerve on one side leads to complete blindness in the corresponding eye
- Compression of optic chiasma causes bitemporal hemianopia because the nasal fibers from both sides are interrupted
- Lesion of the optic tract and optic radiation of one side each leads to corresponding nasal and contralateral temporal hemianopia
- Circumferential blindness is caused most commonly by optic neuritis.
Question 3. Write a note on the oculomotor nerve, trochlear, and abducens nerve.
Answer:
Oculomotor Nerve, Trochlear, And Abducens Nerve
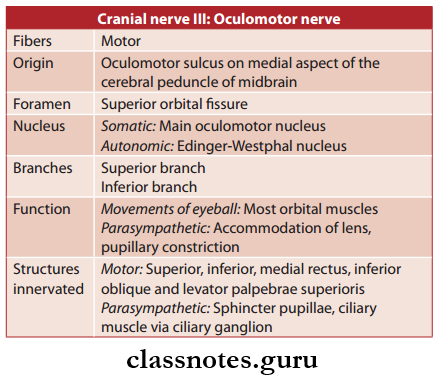
Oculomotor Nerve
- The Oculomotor Nerve is the 3 cranial nerve
- The Oculomotor Nerve is purely motor and supplies most of the muscles of the eye and plays a major role in accommodation.
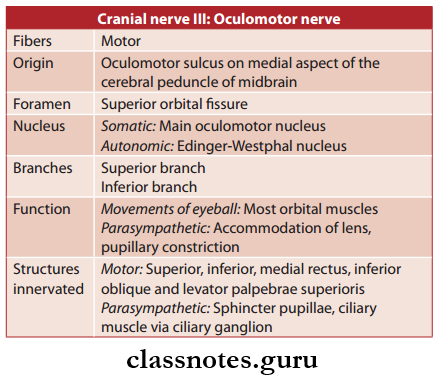
Oculomotor Nerve Functional Components
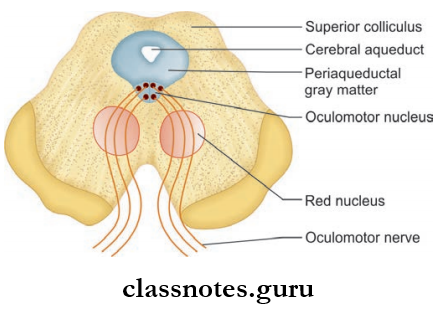
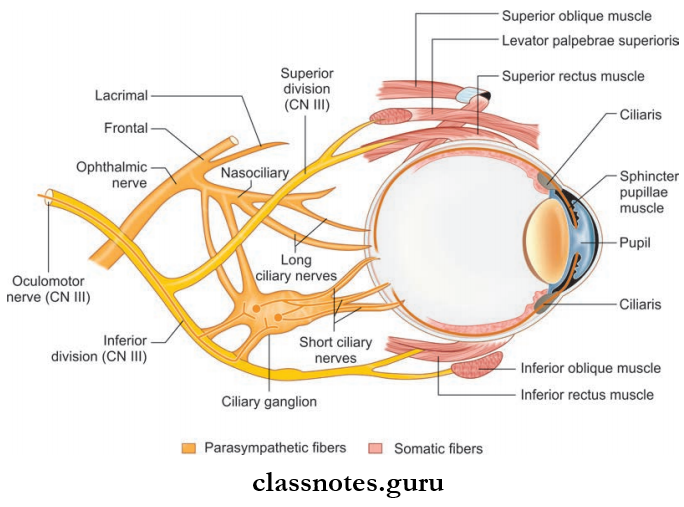
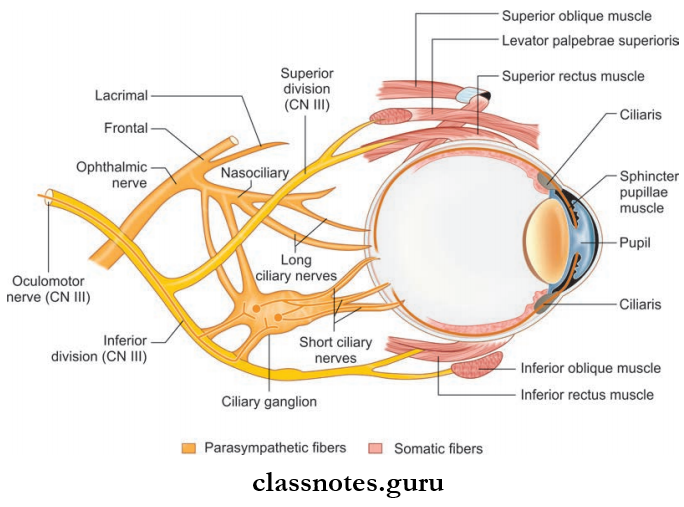
- GSE fibers supply all extraocular muscles except the lateral rectus and superior oblique and they arise from a somatic component of the oculomotor nucleus
- GVE fibers arise from the parasympathetic component of the Edinger-Westphal nucleus and supply sphincter pupillae and ciliary muscle.
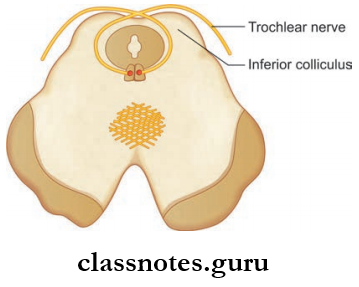
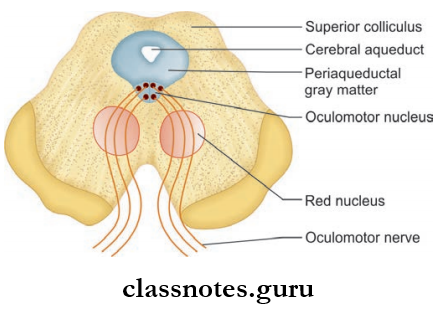
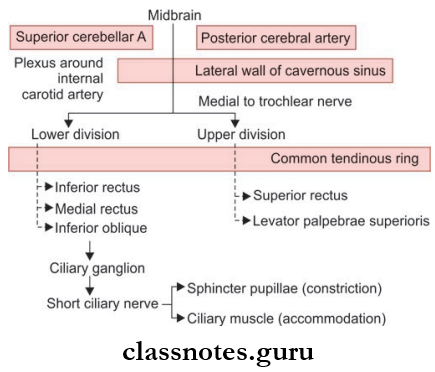
Oculomotor Nerve Course And Relations
- It arises from the oculomotor sulcus on the medial aspect of the cerebral peduncle
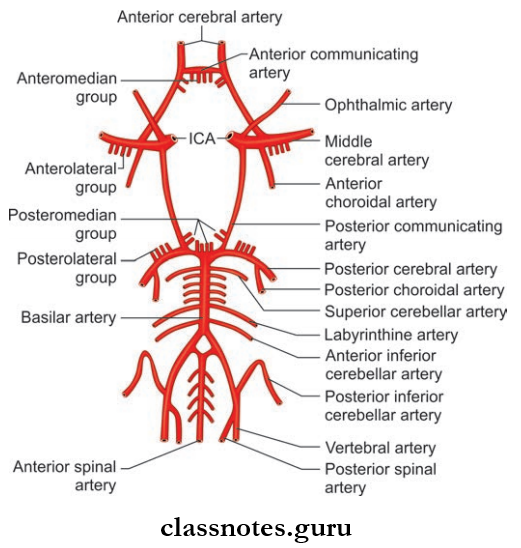
- It runs forward and laterally between posterior cerebral and superior cerebellar arteries passes through tentorium cerebelli and reaches the middle cerebral fossa
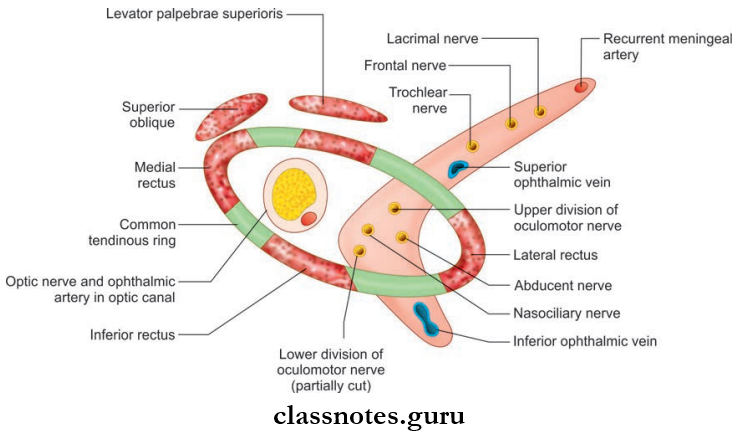
- It then pierces the dura mater in oculomotor triangle enter lateral wall of the cavernous sinus and lies superior to the trochlear, ophthalmic, and maxillary nerve
- It then divides into upper and lower divisions
- These two divisions enter into orbit and the smaller upper division passes above the optic nerve passes through the superior rectus and supply it and then supplies levator palpebrae superioris
- The lower division passes below optic nerve and gives three branches which supply the medial rectus, inferior rectus, and inferior oblique.
Oculomotor Nerve Applied: Oculomotor nerve may undergo complete or incomplete lesions.
- Complete Lesions Of The Oculomotor Nerve Leads To:
- Ptosis: Drooping of the upper eyelid due to paralysis of levator palpebrae
- External Strabismus due to paralysis of the medial rectus and consequent unopposed action of the lateral rectus
- Pupillary Dilatation due to paralysis of sphincter pupillae
- Loss Of Accommodation and of light reflex is due to paralysis of sphincter pupillae and ciliary
- Diplopia: The false image being the higher.
- Incomplete Lesions Of the oculomotor nerve are common and may spare the extraocular or intraocular muscles.
- The condition in which the innervation of extraocular muscles is spared with selective loss of autonomic innervation is called internal ophthalmoplegia.
- The condition in which the intraocular muscles are spared with paralysis of extraocular muscles is called external ophthalmoplegia.
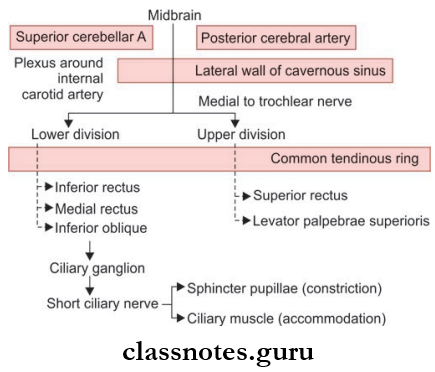
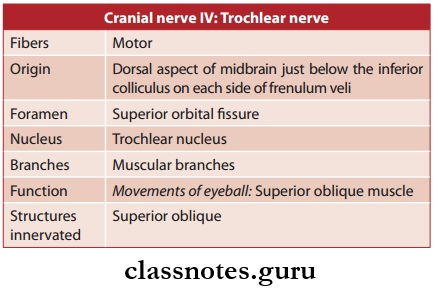
Trochlear Nerve
- Trochlear Nerve is the 4 cranial nerve
- Trochlear Nerve is purely motor and supplies only the superior oblique of the eyeball.
Trochlear Nerve Functional Components: General somatic efferent fibers arise from the trochlear nucleus in the midbrain and supply superior oblique muscle.
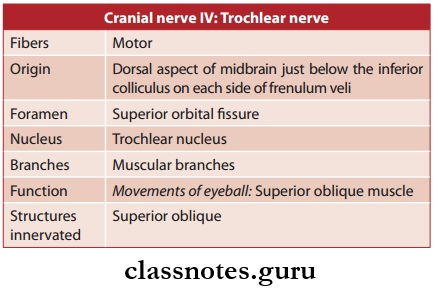
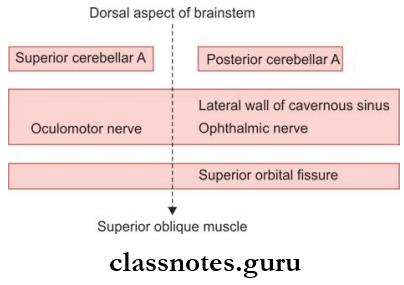
Trochlear Nerve Course And Relations
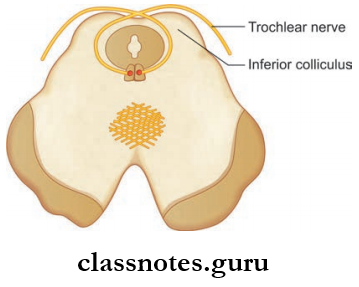
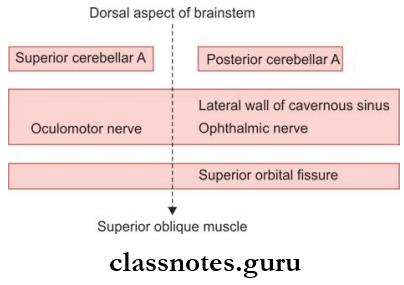
- Trochlear Nerve arises from the dorsal aspect of the midbrain, one on either side of frenulum veli, and wounds around the superior cerebral and superior cerebellar peduncle
- Trochlear Nerve then passes between posterior cerebral and superior cerebellar arteries and lies below the free margins of tentorium cerebelli
- Trochlear Nerve then enters into the cavernous sinus by piercing the roof runs forward in the lateral wall and crosses the oculomotor nerve
- Trochlear Nerve then enters the orbit through the superior orbital fissure runs medially above the levator palpebrae superioris and supplies superior oblique muscle.
Trochlear Nerve Applied
- The conditions most commonly affecting the trochlear nerve include stretching or bruising as a complication of head injuries, cavernous sinus thrombosis, and aneurysm of the internal carotid artery (ICA).
- As a result of such injuries, interruption of the trochlear nerve paralysis of the superior oblique, limiting inferolateral ocular movement; the affected eye rotates medially, producing Diplopia.
- There is also some degree of extorsion, because the superior oblique which normally produces intorsion, is not available.
- To compensate for this, the patient characteristically tilts the head towards the opposite shoulder.
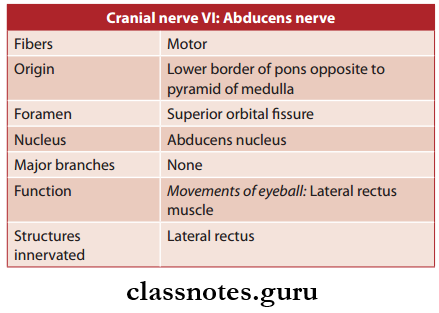
Abducens Nerve
- Abducens Nerve is the 6 cranial nerve
- Abducens Nerve is purely motor and supplies only the lateral rectus muscle and it is called so because it abducts the eyeball.
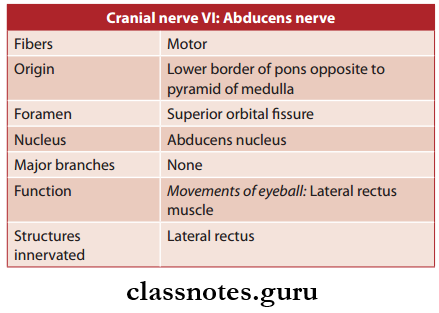
Abducens Nerve Functional Components
- General somatic efferent fibers arise from the abducens nucleus in pons and supply lateral rectus
- General somatic afferent fibers carry proprioceptive sensations from the lateral rectus and terminate in the mesencephalic nucleus of the trigeminal nerve.
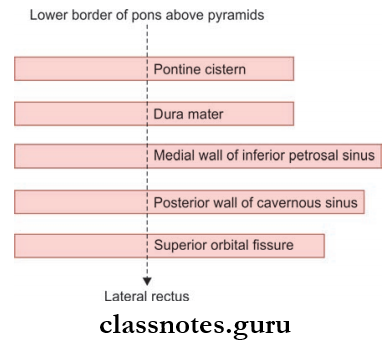
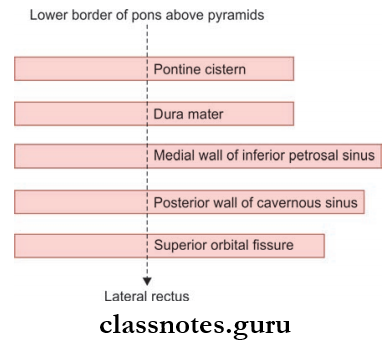
Abducens Nerve Course And Relations
- Abducens Nerve arises from the lower border of pons opposite to the pyramid of the medulla runs upwards and close to the anterior cerebellar artery and pierces the dura mater
- Abducens Nerve then passes through the medial wall of the inferior petrosal sinus arches forward directly over the sharp ridge of the petrous temporal bone and enters into the first-osseous canal
- Abducens Nerve then enters the cavernous sinus by piercing the posterior wall and runs inferolaterally to ICA.
- Abducens Nerve then enters into orbit through a superior orbital fissure runs forward to the lateral side and supply lateral rectus muscle.
Abducens Nerve Applied
- In lesions of the abducens nerve, the patient cannot turn the eye laterally. When the patient is looking ahead, the lateral rectus is paralyzed and the unopposed medial rectus pulls the eyeball medially, causing internal strabismus. There is diplopia.
- The long course of the nerve through the cisterna pontis and its sharp bend over the petrous temporal bone make the nerve liable to damage in conditions producing raised intracranial pressure.
- However, the most common causes of lesions include damage due to head injuries, cavernous sinus thrombosis, or aneurysm of the ICA.
Abducens Nerve Clinical Testing
- The clinical testing of the third, fourth, and sixth nerves is usually done together. These include:
- On inspection look for ptosis, lid retraction, and squint
- Testing for movements of extraocular muscles, ask for diplopia and look for nystagmus
- Eliciting direct and consensual reflex.
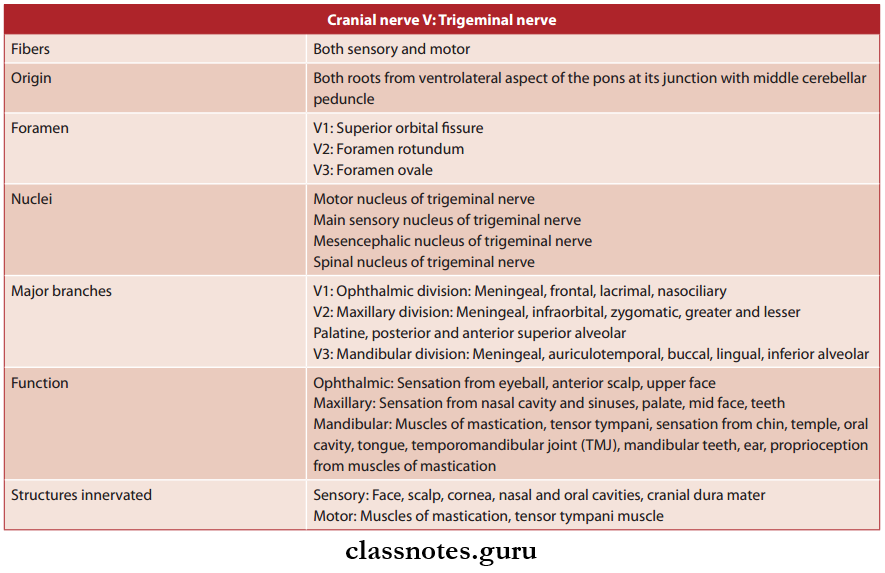
Question 4. Write a note on the trigeminal nerve.
Answer:
Trigeminal Nerve
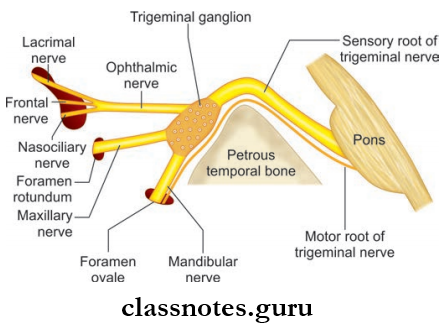
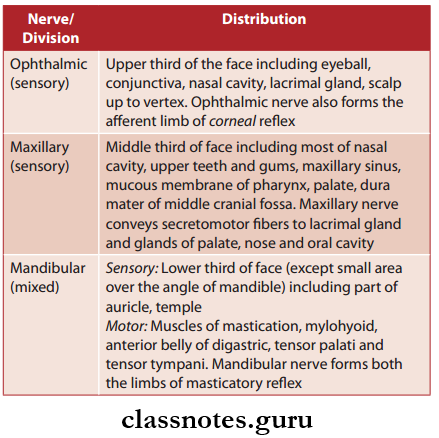
- Trigeminal Nerve is the V cranial nerve
- Trigeminal Nerve is the largest cranial nerve
- Trigeminal Nerve is a mixed nerve carrying both sensory and motor fibers but predominantly it is sensory.
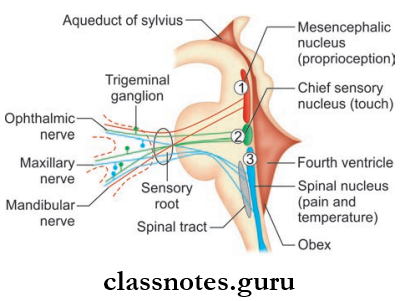
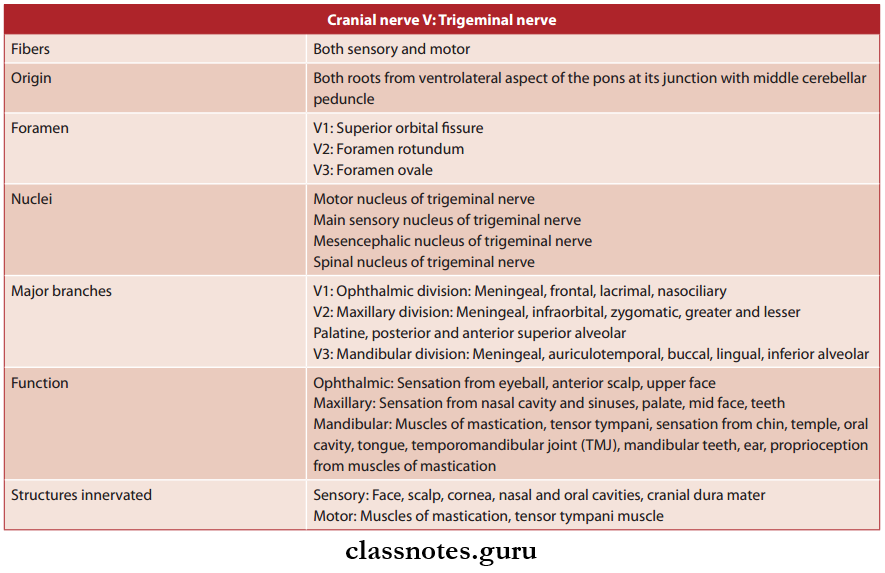
Trigeminal Nerve Functional Components
- General somatic affrent (GSA) fiers carry
- Exteroceptive sensations (pain, touch, and temperature) from the skin of the head and face, mucous membrane of the mouth, nasal cavity, meninges, etc., and terminate in the main sensory nucleus and spinal nucleus of the trigeminal nerve
- Proprioceptive sensations from muscles of mastication, temporomandibular joint, and teeth terminate in the mesencephalic nucleus of the trigeminal nerve and reticular formation of the brainstem.
- Special visceral efferent (SVE) fibers arise from the motor nucleus of the trigeminal nerve and supply muscles derived from the 1st pharyngeal arch, viz muscles of mastication, mylohyoid, anterior belly of digastric, tensor palati and tensor tympani.
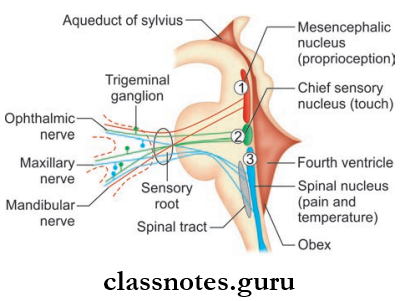
Trigeminal Nerve Nuclei
- Spinal Nucleus Of 5th Nerve: It takes pain and temperature sensations from most of the face area which relays here.
- The Superior Sensory Nucleus Of 5th Nerve: The fiers carrying touch and pressure relay here.
- Mesencephalic Nucleus: It receives proprioceptive impulses from muscles of mastication, and temporomandibular joint.
- Motor Nucleus Of 5th Nerve: The fibers from the nucleus supply eight muscles derived from the 1st branchial arch.
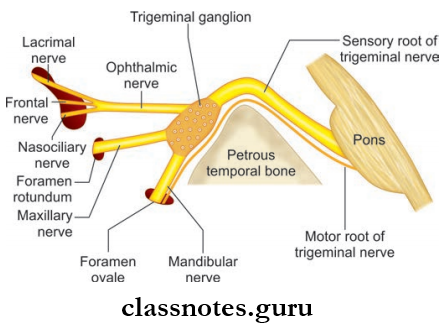
Trigeminal Nerve Course And Relations
- The nerve arises by two roots, a small medial motor root and a large lateral sensory root from the ventrolateral aspect of pons at its junction with the middle cerebellar peduncle.
- The sensory root passes forward and laterally over the apex of the petrous temporal bone to enter the middle cranial fossa.
- Here the nerve presents a dilatation called the trigeminal ganglion and it occupies the dural cave known as the Meckel’s cave.
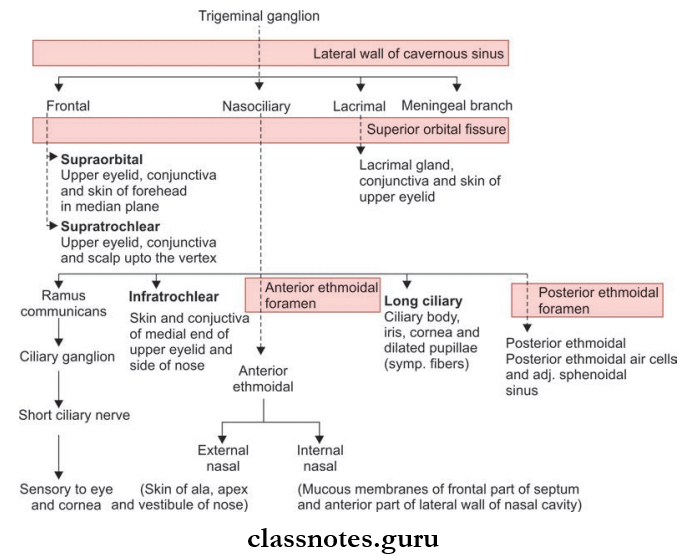
The Convex Surface Of The Ganglion Gives Of Three Divisions:
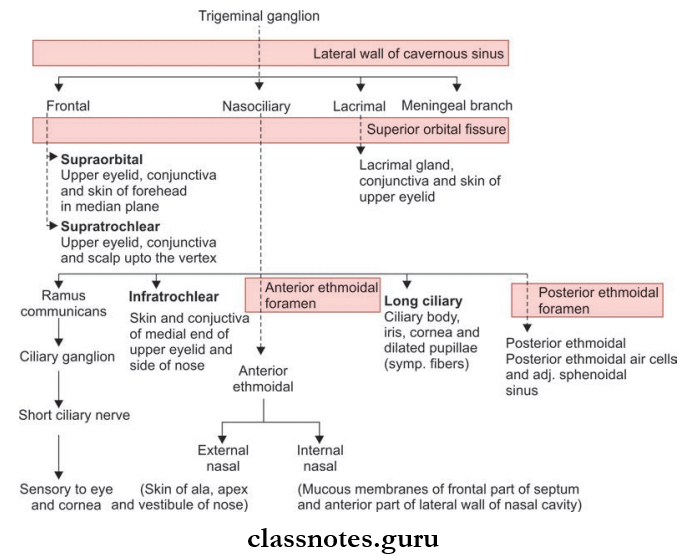
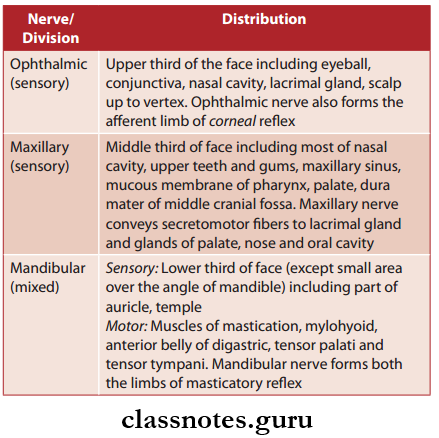
1. Ophthalmic Nerve: It arises from the anterolateral aspect of the ganglion enters the lateral wall of the cavernous sinus and lies below the trochlear nerve.
- The cavernous sinus, divides into three branches nasociliary nerve, lacrimal nerve, and frontal nerve.
- All these enter the orbit through the superior orbital fissure.
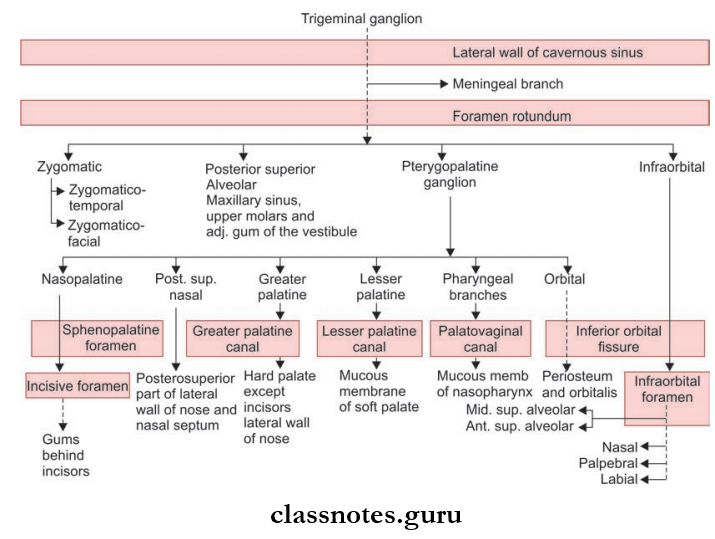
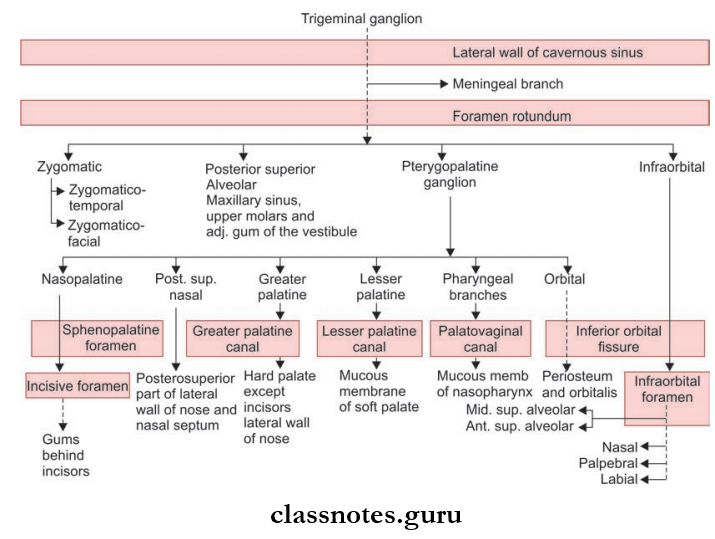
2. Maxillary Nerve: It arises from the ganglion and enters the lateral wall of the cavernous sinus it occupies the lowest position and leaves the sinus to enter the pterygopalatine fossa through the foramen rotundum.
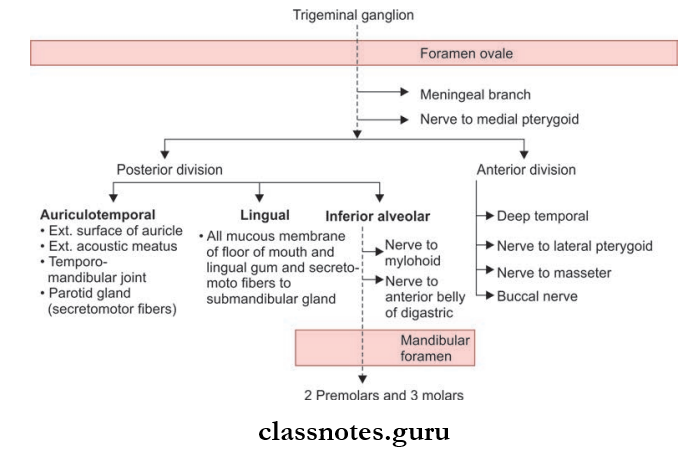
3. Mandibular Nerve: After arising from the ganglion it immediately enters the infratemporal fossa through the foramen ovale.
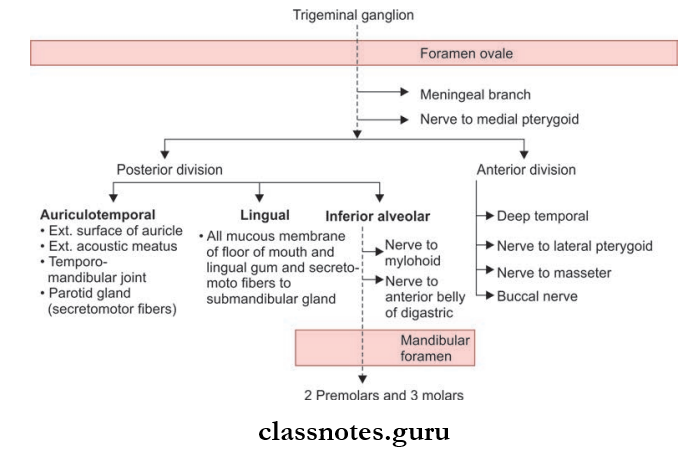
- The motor root passes forwards and laterally deep to the sensory root and enters the infratemporal fossa through the foramen ovale and after passing through the foramen ovale it joins the mandibular nerve.
Trigeminal Nerve Distribution
Trigeminal Nerve Clinical Testing
- The motor part is tested by testing the temporalis, a masseter, and pterygoids
- The masseter and temporalis is palpated after clenching the teeth
- Opening the mouth against resistance is used to test the pterygoid
- The sensory part is tested by testing the seven areas on each side of the face away (from midline) for pain, touch, and temperature.
- The corneal reflex, conjunctival reflex, and jaw jerk is also elicited.
Trigeminal Nerve Applied
- Lesion of the whole trigeminal nerve causes anesthesia of the anterior half of the scalp, of the face (except a small area near the angle of the mandible), of the cornea and conjunctiva, the mucosa of the nose, mouth, and sulcal part of the tongue. Paralysis and atrophy occur in the muscles supplied by the nerve.
- Trigeminal Neuralgia characterized by pain in the distribution of branches of the trigeminal nerve, is the most common condition affecting the sensory part of the nerve.
- With the maxillary nerve affected, the pain is usually felt deeply in the face and nose between the mouth and orbit. The cause of maxillary neuralgia is often neoplasms and empyema of the maxillary sinus.
- With the mandibular nerve affected, the pain is usually felt from the mouth up to the ear and the temporal region.
- The most common cause is a carious mandibular tooth or an ulcer and carcinoma of the tongue.
- With the ophthalmic nerve affected, the pain is usually felt in the supraorbital region and is often associated with glaucoma or with frontal or ethmoidal sinusitis.
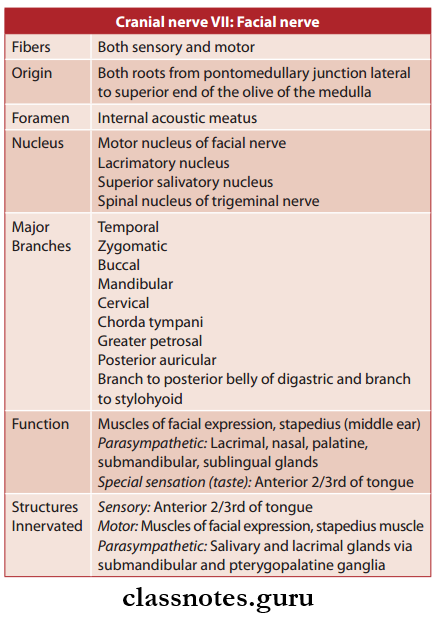
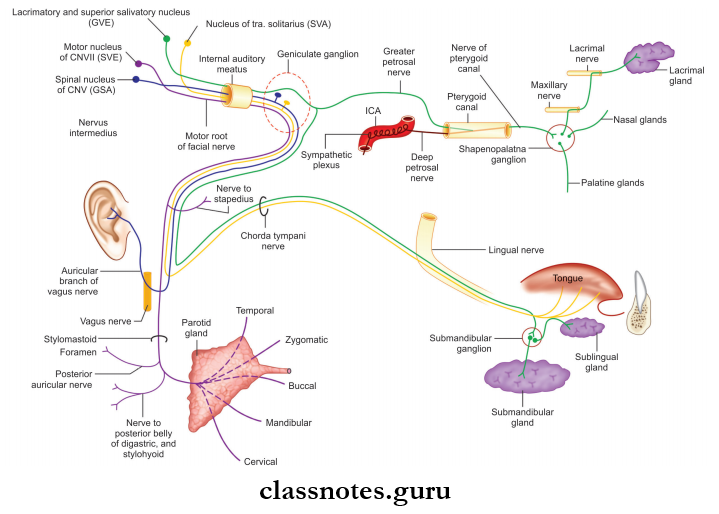
Question 5. Write a short note on the facial nerve.
Answer:
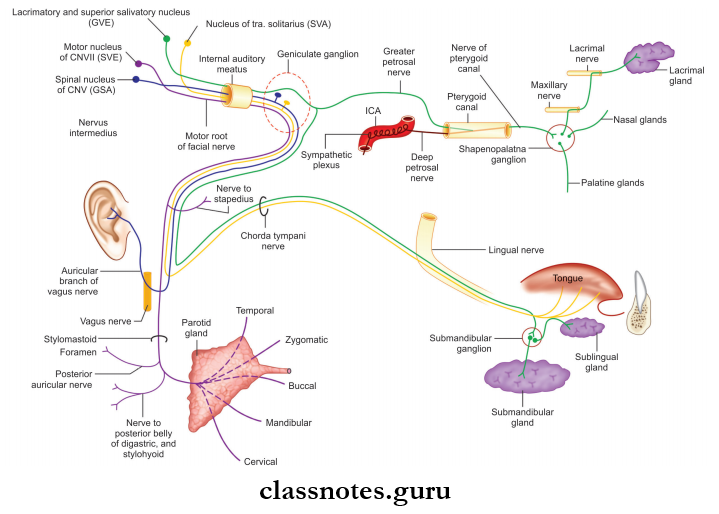
Facial Nerve
- Facial Nerve is the 7 cranial nerve.
- Facial Nerve is a mixed nerve but is predominantly a motor nerve.
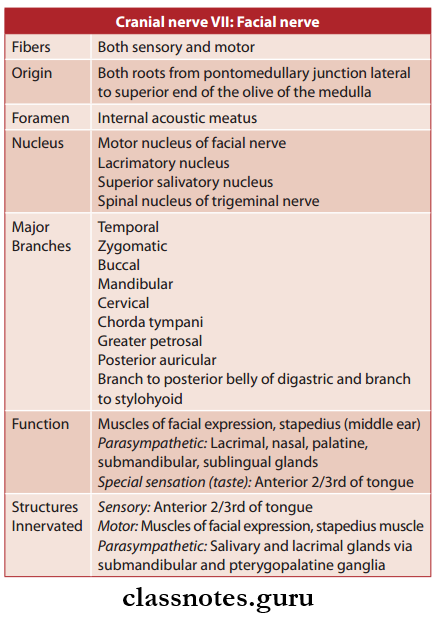
Facial Nerve Functional Components
- General somatic afferent (GSA) fiers carry general sensations from the skin of the auricle and terminate in the spinal nucleus of the trigeminal nerve
- General visceral efferent (GVE) fibers arise from lacrimatory and superior salivatory nuclei and supply secretomotor fibers to lacrimal, submandibular, and sublingual glands
- Special visceral afferent (SVA) fibers carry special sensations of taste from the anterior 2/3rd of the tongue except vallate papillae and terminate in the nucleus of tractus solitarius
- Special visceral efferent (SVE) fibers arise from the motor nucleus of the facial nerve and supply the muscles of facial expression.
Facial Nerve Nuclei: The fibers are connected to four nuclei situated in the lower pons.
- Motor nucleus (branchiomotor)
- Superior salivatory nucleus (parasympathetic)
- Lacrimatory nucleus (parasympathetic)
- Nucleus of tractus solitarius (gustatory).
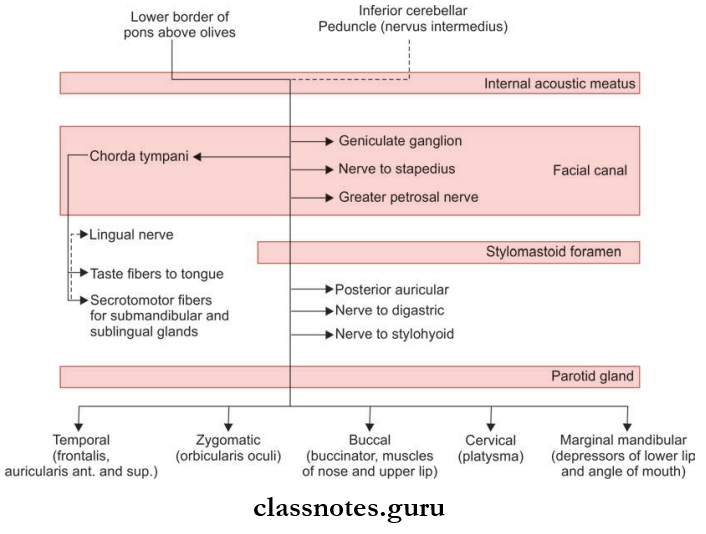
Facial Nerve Course And Relations
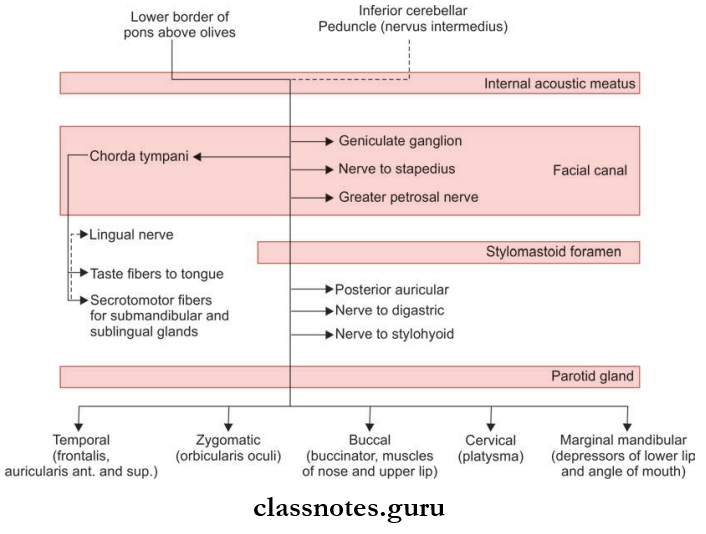
- The nerve consists of two distinct roots, a large medial motor root (facial nerve proper) and a small lateral sensory root (the nervus intermedius)
- Both roots arise from the pontomedullary junction lateral to the superior end of the olive of the medulla
- The sensory root lies in between the motor root medially and the vestibulocochlear nerve laterally
- After emerging from the brainstem both the roots pass laterally and forwards in the cerebellopontine angle along with the vestibulocochlear nerve and labyrinthine artery
- These structures then enter the internal acoustic meatus
- In the meatus, the motor root is lodged in a groove on the vestibulocochlear nerve and the sensory root remains separate
- At the lateral end of the internal acoustic meatus, the two roots unite to form the trunk of the facial nerve and enter the facial canal in the petrous temporal bone
- The course in facial canal can be divided into three parts by two bends
- The first part is directed laterally above the vestibule, the second part runs backward in relation to the medial wall of the middle ear above the promontory, and the third part is directed vertically downwards behind the promontory
- The first bend at the junction of the first and second part is sharp and it lies over the anterosuperior part of the promontory and is also called the genu and possesses geniculate ganglion
- The second bend is gradual and lies between the promontory and the aditus to the mastoid antrum
- The facial nerve leaves the cranial cavity through the stylomastoid foramen
- After coming out through the stylomastoid foramen the facial nerve crosses the lateral side of the base of the styloid process
- It then enters the posteromedial surface of the parotid gland and runs forward through the gland crossing the retromandibular vein and the external carotid artery
- Behind the neck of the mandible, it divides into its fie terminal branches which emerge along the anterior border of the parotid gland.
Facial Nerve Branches And Distribution
- Within The Facial Canal:
- Greater Petrosal Nerve:
- Greater Petrosal Nerve arises from the geniculate ganglion and consists of the preganglionic parasympathetic fibers which relay in pterygopalatine ganglion
- The Greater Petrosal Nerve then supplies the secretomotor fibers to the lacrimal gland and mucous glands of the nasal cavity and palate.
- The Nerve To Stapedius
- The Nerve To Stapedius arises from the vertical part of the facial nerve opposite to the pyramidal eminence and runs through a short canal to reach the stapedius to supply it
- The muscle damps the excessive vibration of the stapes caused by high-pitched sounds. Paralysis of this muscle causes even the normal sounds to appear too loud.
- The Chorda Tympani Nerve
- The Chorda Tympani Nerve arises from the vertical part of the facial nerve and enters the middle ear through the posterior canaliculus then runs in close relation to the tympanic membrane and then passes between the long process of incus and handle of the malleus and leaves the middle ear by entering the anterior canaliculus
- The Chorda Tympani Nerve then traverses through the bony canaliculus and enters the infratemporal fossa through the medial end of the petrotympanic fissure
- The Chorda Tympani Nerve then passes medial to the spine of the sphenoid and enters the infratemporal fossa
- In The Infratemporal Fossa, It Joins The Lingual Nerve And Carries:
- Preganglionic secretomotor fibers to the submandibular ganglion to supply the submandibular and sublingual glands
- Taste fibers from the anterior 2/3rd of the tongue except the circumvallate papillae.
- At its exit from the stylomastoid foramen
- Posterior Auricular Nerve
- Arises just below the stylomastoid foramen
- It supplies the auricularis posterior, occipital belly of occipitofrontalis, and intrinsic muscles on the back of the auricle.
- Nerve To The Posterior Belly Of The Digastric: It is a short branch and supplies the posterior belly of the digastric muscle.
- Nerve To Stylohyoid: Arises with the stylohyoid muscle and supplies the stylohyoid muscle.
- Communicating branches with adjacent cranial and spinal nerves
- Six Terminal Branches That Supply The Muscles Of Facial Expression Include:
- Temporal
- Zygomatic
- Buccal
- Marginal
- Mandibular
- Cervical.
Facial Nerve Clinical Testing: The testing of the facial nerve is done by carrying out the following:
- Check for wrinkling of the forehead by asking the patient to look upwards. On the affected side the wrinkling will be reduced in the LMN type of facial paralysis
- Forced eye closure is tested by asking the patient to tightly close the eyelid and the examiner tries to open the eyes with fingers. Normally examiner is unable to overcome the closure but in the case of LMN facial palsy the eye closure will be defective
- On asking the patient to show the teeth, the angle of the mouth will deviate to the opposite side of the lesion
- The examiner asks the patient to blow the cheeks and the symmetry on both sides is looked for and tries to expel the air by pressing on either side of the cheeks
- Ask for hyperacusis or subjective assessment to be done
- Taste sensation in the anterior 2/3rd of the tongue is tested by using solutions of sugar or salt.
Facial Nerve Applied
- The facial nerve may be injured or become dysfunctional anywhere along its course from the brainstem to the face. The paralysis may be supranuclear or intranuclear
- Supranuclear facial paralysis, involving the upper motor neuron pathway is usually a part of hemiplegia. It involves paralysis of the lower part of the face but not the upper (forehead and orbicularis oculi) because the facial nerve nucleus innervating the upper part of the face receives fiers from the cerebral cortex of both sides whereas the lower part innervating the lower part of the face receives contralateral fiers.
- However, emotional movements of the lower face, as in smiling and laughing, are still possible (presumably there is an alternative pathway from the cerebrum)
- Infranuclear lesions vary in their effects depending on the site of the lesion. Due to the anatomical location of the facial nerve, neighboring structures are inevitably involved
- If the facial nucleus or facial pontine fibers are involved, there may be damage to the abducens nucleus (paralysis of lateral rectus), motor trigeminal nucleus may be involved (paralysis of masticatory muscles), and principal sensory nucleus and spinal trigeminal nucleus may also be involved (sensory loss of face)
- Lesions in the posterior cranial fossa or internal acoustic meatus may involve the vestibulocochlear nerve, resulting in loss of taste from the anterior part of tongue with ipsilateral deafness and facial paralysis
- Lesions of the facial nerve in the facial canal may involve the nerve to stapedius causing excessive sensitivity to sound in one ear (hyperacusis)
- When damage is in the petrous temporal bone, the chorda tympani nerve is usually involved resulting in loss of taste from the anterior two-thirds of the tongue
- Bell’s Palsy: It is caused due to inflammation of facial nerve near the stylomastoid foramen or compression of its fibers near the facial canal or stylomastoid foramen.
- If the lesion is complete, the facial muscles are all equally affected, with the following complications:
- There is facial asymmetry and the affected side is immobile.
- The eyebrows are drooped, wrinkles are smoothed out and the palpebral fissure is widened by the unopposed action of levator palpebrae.
- The lips remain in contact and cannot be pursued; in attempting to smile the angle of the mouth is not drawn up on the affected side, the lips remaining nearly closed.
- Food accumulates in the cheek, from the paralysis of the buccinator and dribbles, or is pushed out between the paralyzed lips.
- Platysma and the auricular muscles are paralyzed.
- Tears will fly over the lower eyelid and saliva will dribble from the corner of the mouth.
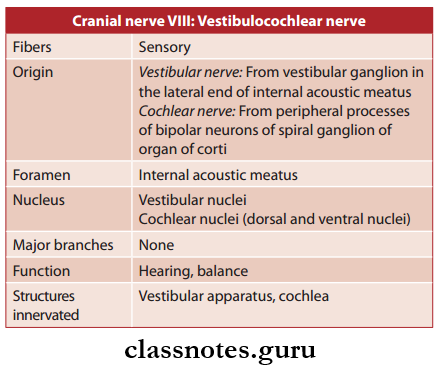
Question 6. Write a note on the vestibulocochlear nerve.
Answer:
Vestibulocochlear Nerve
- Vestibulocochlear Nerve is the 8 cranial nerve.
- Vestibulocochlear Nerve consists Of Two Parts:
- Vestibular part called the vestibular nerve
- The cochlear part called the cochlear nerve.
- The vestibular nerve is concerned with the maintenance of equilibrium while the cochlear nerve is concerned with hearing.
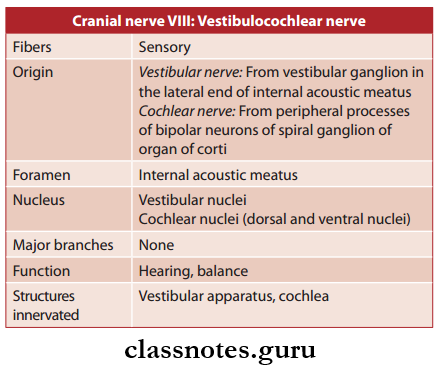
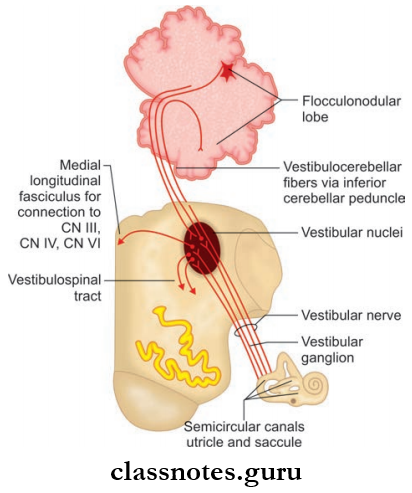
Vestibulocochlear Nerve Functional Components
- Special somatic afferent (SSA) fibers carry sensory information necessary for maintenance of equilibrium and hearing from the membranous labyrinth of the internal ear
- The fibers carrying sensory information for equilibrium terminate in the vestibular nuclei
- The fibers carrying sensory information for hearing terminate in the dorsal and ventral cochlear nuclei.
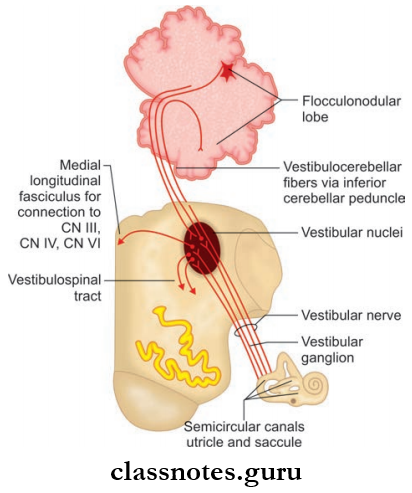
Vestibulocochlear Nerve Nuclei
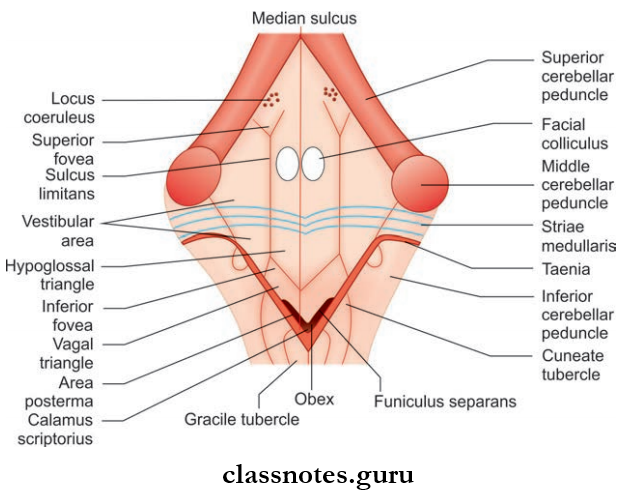
- The vestibular nuclei occupy the vestibular area in the lateral part of the floor of the fourth ventricle
- It consists of superior, inferior, lateral, and medial subdivisions
- The nucleus receives the vestibular nerve, cerebella vestibular fiers from floccus and nodule, spinovestibular fibers, and reticulovestibular fibers
- The Connections Of Nuclei Include The Following:
- Fibers to the archicerebellum through the inferior cerebellar peduncle (vestibulocerebellar tract)
- Fibers to motor nuclei of the brainstem (3, 4, and 6 nerves) through the medial longitudinal bundle.
- These regulate the vestibulocochlear reflexes.
- Fibers to anterior horn cells of the spinal cord through the vestibulospinal tract and help in the coordination of head, neck, and eye muscles.
- The Cochlear Nuclei Consist Of Two: the ventral and dorsal nuclei and lie on the floor of the fourth ventricle.
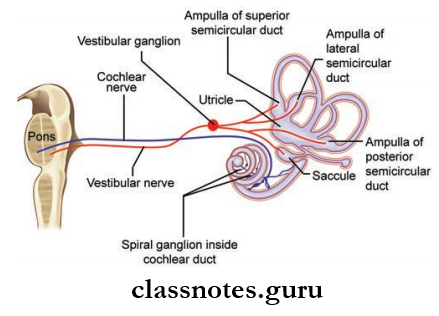
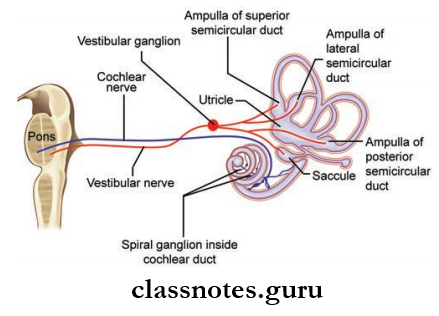
Vestibulocochlear Nerve Course And Relations
- The vestibular nerve begins in the vestibular ganglion (Scarpa’s ganglion) located at the lateral end of the internal acoustic meatus
- The peripheral processes change the origin of the neurons pass through the foramina in the lateral end of the internal acoustic meatus and supply the ampullary crista and the maculae
- The central processes of the ganglion cells unite to form the trunk of vestibular nerve
- The nerve then enters the posterior cranial fossa and passes through the cerebellopontine angle to reach the brainstem
- It enters the brainstem at the pontomedullary junction slightly lateral and posterior to the facial nerve
- The peripheral processes of the bipolar neurons of the spiral ganglion (present in modiolus) innervate the hair cells in the organ of Corti
- The central processes of the bipolar neurons pass through the tractus spiralis foraminous at the medial end of the internal acoustic meatus and assemble to form the cochlear nerve
- The cochlear nerve passes through the pontocerebellar angle to reach the lateral aspect of the pontomedullary junction
- It enters the pons and divides into ascending and descending fibers, which terminate in ventral and dorsal nuclei in the floor of the fourth ventricle.
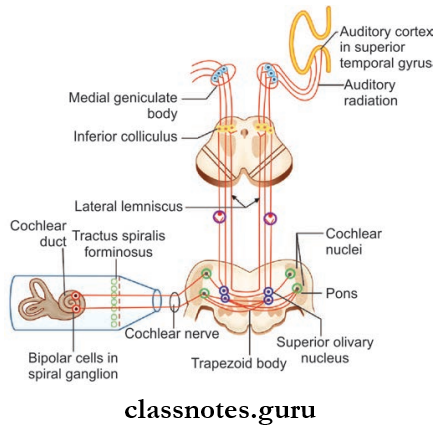
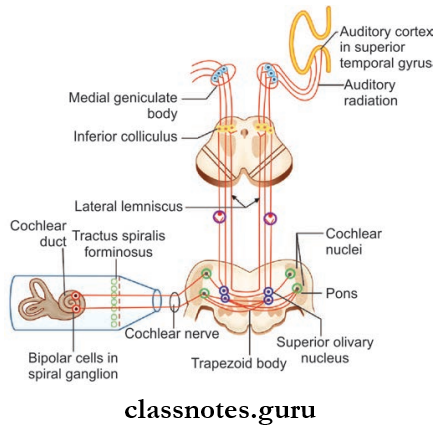
Vestibulocochlear Nerve Auditory Pathway
- The hair cells are innervated by the dendrites of bipolar cells of the spiral ganglion and the axons of this form the cochlear part of the VIII cranial nerve and end in cochlear nuclei.
- From the cochlear nuclei the main nuclei in the auditory pathways, from below upwards are:
- Superior olivary complex
- Lateral lemniscus
- Inferior colliculus
- Medial geniculate body
- Auditory cortex.
- The auditory fibers travel via the ipsilateral and contralateral routes and have multiple decussation points and as a result, each ear is represented in both cerebral hemispheres
- The auditory cortex concerned with hearing is situated in the superior temporal gyrus (Brodmann’s area 41).
Vestibulocochlear Nerve Clinical Testing
- The vestibular part is clinically examined by asking for tinnitus and vertigo and look for nystagmus
- The cochlear part is tested by Rinne’s test, Weber’s test, and Absolute bone conduction test.
Vestibulocochlear Nerve Applied
- Disturbances of vestibular nerve function include giddiness (Vertigo) and Nystagmus
- Vestibular nystagmus is an uncontrollable rhythmic oscillation of the eyes
- This form of nystagmus is essentially a disturbance in the reflex control of the extraocular muscles, which is one of the functions of the semicircular canals
- The causes of vertigo include diseases of the labyrinth, lesions of the vestibular nerve and the cerebellum, multiple sclerosis, tumors, and vascular lesions of the brainstem
- Disturbances of the cochlear nerve function produce deafness and tinnitus
- Loss of hearing may be due to a defect of the auditory conducting mechanism in the middle ear, damage to the receptor cells in the spiral organ of Corti in the= cochlea, lesions of the cochlear nerve due to acoustic neuroma and trauma, or lesion of the cerebral cortex of temporal lobe due to multiple sclerosis.
Question 7. Write a note on the glossopharyngeal nerve.
Answer:
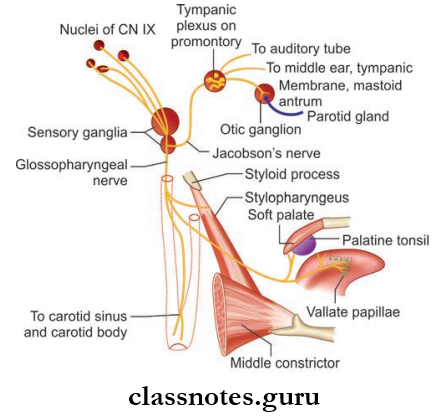
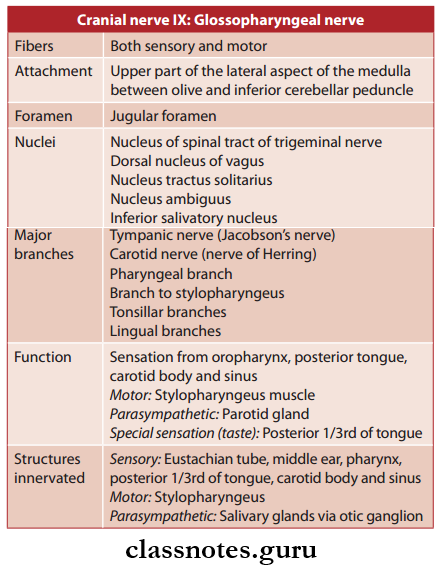
Glossopharyngeal Nerve
- Glossopharyngeal Nerve is the 9-nerve
- It is a mixed nerve and consists of both sensory and motor fibers but predominantly it is sensory.
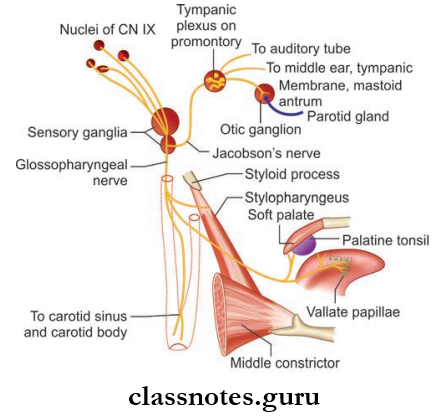
Glossopharyngeal Nerve Functional Components
- General somatic afferent (GSA) fiers carry proprioceptive sensations from the stylopharyngeus and skin of auricle and terminate in nucleus of spinal tract of the nerve
- General visceral afferent (GVA) fibers carry general sensations of pain, touch, and temperature from the mucous membrane of pharynx, tonsil, soft palate, and posterior 1/3rd of tongue and terminate in dorsal nucleus of vagus
- General visceral efferent (GVE) fibers (preganglionic parasympathetic) arise from the inferior salivatory nucleus and they supply secretomotor fibers to parotid gland
- Special visceral afferent (SVA) fibers carry taste sensations from posterior 1/3rd of tongue including vallate papillae and terminate in nucleus tractus solitarius
- Special visceral effrent (SVE) fibers arise from nucleus ambiguus and supply stylopharyngeus muscle.
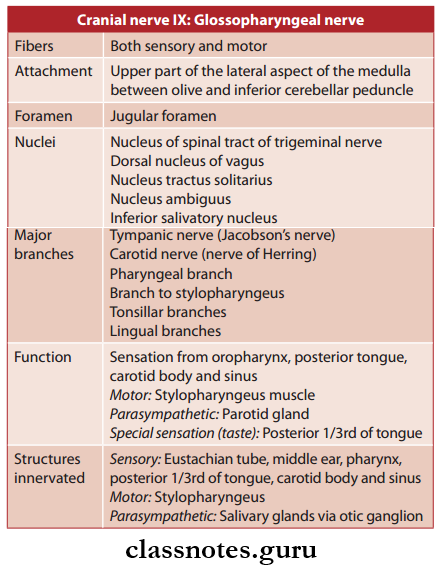
Glossopharyngeal Nerve Nuclei: The nuclei includes the following
- Nucleus ambiguus (branchiomotor)
- Inferior salivatory nucleus (parasympathetic)
- Nucleus of tractus solitaries (gustatory).
Glossopharyngeal Nerve Course And Relations
- The nerve arises from the upper part of the posterolateral sulcus of medulla between olive and inferior cerebellar peduncle as 3–4 rootlets just above rootlets of vagus nerve
- The rootlets unite to form a single trunk which passes forwards and laterally cross the jugular tubercle and reaches the jugular foramen
- It leaves the cranial cavity through middle part of jugular foramen enclosed in a separate dural sheath
- The nerve consists of a small superior ganglion and a larger inferior ganglion
- The superior ganglion lies within the jugular foramen and the inferior ganglion lies just below the jugular foramen
- In the jugular foramen the nerve lies in a deep groove leading to the cochlear canaliculus and is separated from the 10th and 11th cranial nerves by inferior petrosal sinus
- After emerging through the jugular foramen the nerve passes downwards and forwards between internal carotid artery and internal jugular vein. It then descends anterior to internal carotid artery and styloid process to reach the lower border of stylopharyngeus and it pass along with the stylopharyngeus through the gap between superior and middle constrictors
- It then curves around the lateral border of stylopharyngeus and supplies it and gives of the pharyngeal branches and then passes deep to the stylohyoid ligament and posterior end of hyoglossus and divide into terminal branches tonsillar and lingual branches which supply the mucous membrane of tonsil, pharynx, and tongue.
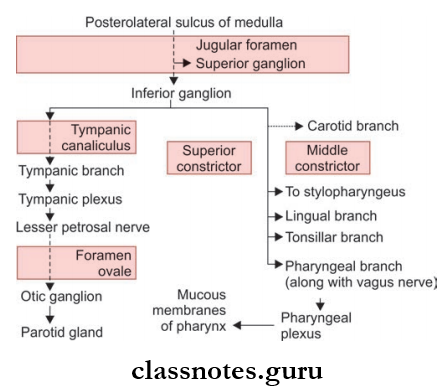
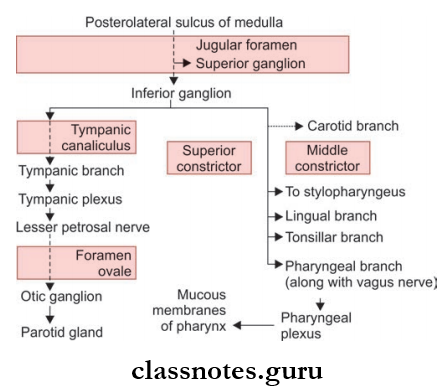
Glossopharyngeal Nerve Branches and Distribution: T branches include
- Tympanic branch: It arises from the inferior ganglion and enters the middle ear through the tympanic canaliculus and takes part in the tympanic plexus and gives of the following branches:
- Lesser petrosal nerve which carries the preganglionic fibers to the otic ganglion
- To supply middle ear, mastoid antrum, and auditory tube.
- Carotid nerve: It is a branch to carotid body and sinus
- Pharyngeal branches: They take part in the pharyngeal plexus along with the pharyngeal branches of vagus and cervical sympathetic chain
- Branch to stylopharyngeus: It is the only muscular branch of the glossopharyngeal nerve and supply the stylopharyngeus muscle
- Tonsillar branches: Supplies the tonsil, fauces, and palate
- Lingual branches: Supplies the posterior 1/3rd of the tongue and vallate papillae and carries the taste and general sensations.
Glossopharyngeal Nerve Clinical Testing: The nerve is clinically tested by
- Eliciting the gag reflex: On stroking the posterior wall of pharynx there is a reflex contraction of pharyngeal muscles causing gagging
- Testing the taste sensations in the posterior 1/3rd of tongue.
Glossopharyngeal Nerve Applied
- Isolated glossopharyngeal nerve lesions are extremely rare, as the last four cranial nerves are not often damaged and even if they are, they are commonly affected together, for example by a tumor in posterior cranial fossa.
- Complete lesion of glossopharyngeal nerve can result in:
- Loss of taste and general sensations over posterior
- 1/3rd of tongue
- Difficulty in swallowing
- Loss of salivation from parotid gland.
Question 8. Write a note on vagus nerve.
Answer:
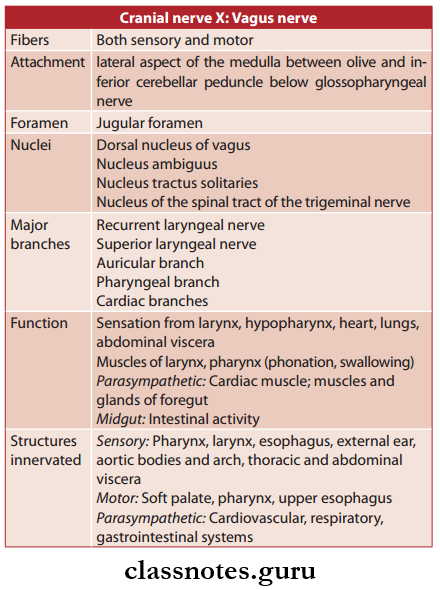
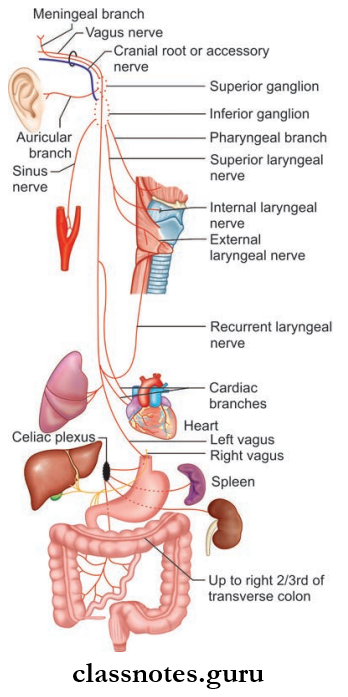
Vagus nerve
- It is the 10 cranial nerve
- It is called so because of the extensive or vague course through the head, neck, thorax, and abdomen.
- It is a mixed nerve consisting of both sensory and motor fibers but predominantly it is motor.
- The fibers of the cranial root of the accessory nerve are also distributed through vagus nerve.
- The nerve bears two ganglia: superior and inferior.
- The superior ganglion is round and lies in the jugular foramen whereas the inferior is cylindrical and lies near base of skull.
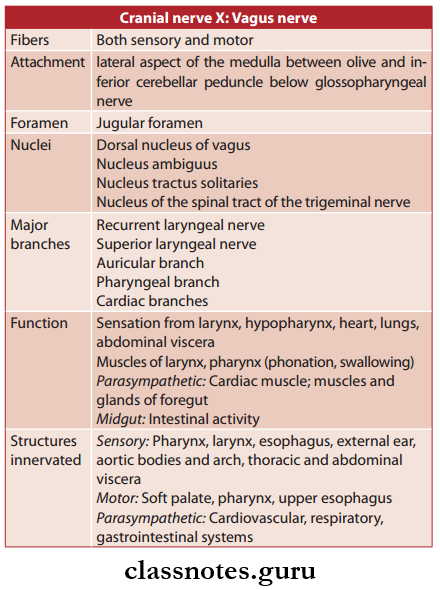
Abbreviations: GSA = General somatic affrent; SVA = Special visceral affrent; GVE = General visceral effrent; SVE = Special visceral effrent
Vagus Nerve Functional Components:
- General somatic afferent (GSA) fiers (peripheral processes of neurons of superior ganglion) carry general sensations from skin of the auricle and terminate in the nucleus of the spinal tract of the trigeminal nerve
- General visceral afferent (GVA) fiers (peripheral processes of neurons of inferior ganglion) carry general sensations from mucous membrane of the pharynx, larynx, trachea, esophagus, and thoracic and abdominal viscera and terminate in the nucleus tractus solitarius, and some in the dorsal nucleus of the vagus
- General visceral efferent (GVE) fibers arise from dorsal motor nucleus of vagus and provide parasympathetic innervation to thoracic and abdominal viscera
- Special visceral afferent (SVA) fibers carry taste sensations from posterior 1/3rd of tongue and epiglottis and terminate in the nucleus tractus solitarius
- Special visceral efferent (SVE) fibers arise from nucleus ambiguus and supply muscles of the palate, pharynx, and larynx.
Vagus Nerve Nuclei
- The nuclei associated with vagus nerve include the following:
- The nucleus of spinal tract of trigeminal
- Nucleus tractus solitarius (gustatory) is distributed through internal laryngeal nerve to taste buds of epiglottis and vallecula
- Dorsal nucleus of vagus (parasympathetic) is a mixed nucleus and its fibers form the main bulk of the nerve
- Nucleus ambiguus (branchiomotor) is mainly a part of cranial root of the accessory nerve.
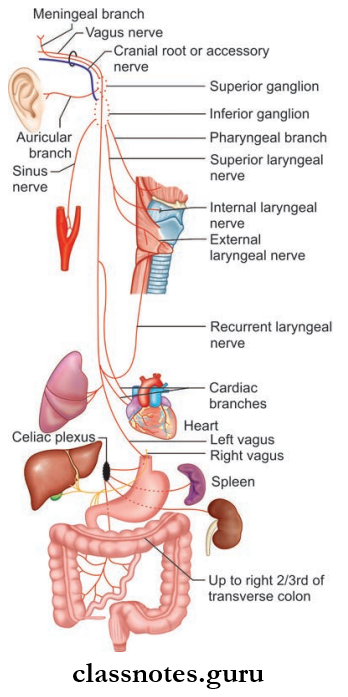
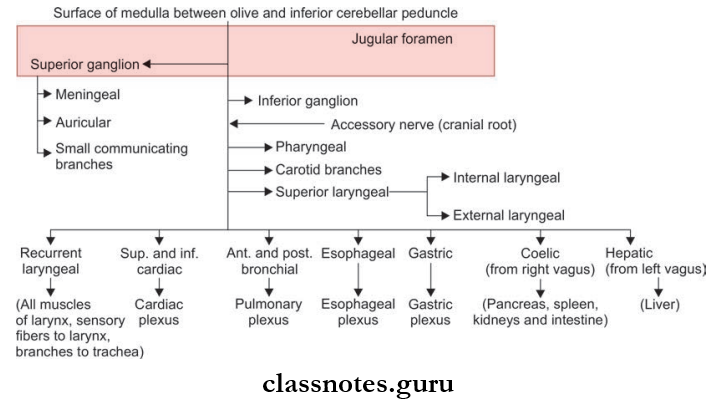
Vagus Nerve Course and Relations
- It arises from the posterolateral sulcus of the medulla between the olive and inferior cerebellar peduncle as 5–10 rootlets below and in line of the rootlets of the glossopharyngeal nerve
- The rootlets unite to form a large trunk that passes laterally and cross the jugular tubercle and reaches the jugular foramen
- It then leaves the cranial cavity by passing through middle part of the jugular foramen along with 11th nerve as enclosed within common dural sheath
- The superior and inferior ganglia are located on the nerve as it passes through the jugular foramen
- The superior ganglion which is small and round lies within the foramen and the large cylindrical inferior ganglion lies just below the jugular foramen
- After coming out through jugular foramen the nerve runs vertically downwards within the carotid sheath and lies first between internal jugular vein and internal carotid artery and then between internal jugular vein and common carotid artery
- At the root of the neck, the nerve enters the thorax
- The right vagus enters by crossing the first part of the subclavian artery and then inclines medially behind brachiocephalic vessels and reaches the right side of trachea which separates it from the right pleura
- It then inclines behind the hilum of the right lung and courses medially toward the esophagus to form the esophageal plexus with the left vagus nerve
- The left vagus enters thorax by passing between the left common carotid and left subclavian arteries
- It descends on the left side of the aortic arch, which separates it from the left pleura, and travels behind the phrenic nerve
- It then courses behind the root of the left lung and then deviates medially and downwards to reach the esophagus and form the esophageal plexus by joining the right vagus nerve
- The anterior and posterior gastric nerves are then formed from the esophageal plexus
- The gastric nerves supply all abdominal organs and the gastrointestinal tract ending just before the left colonic (splenic) flexure.
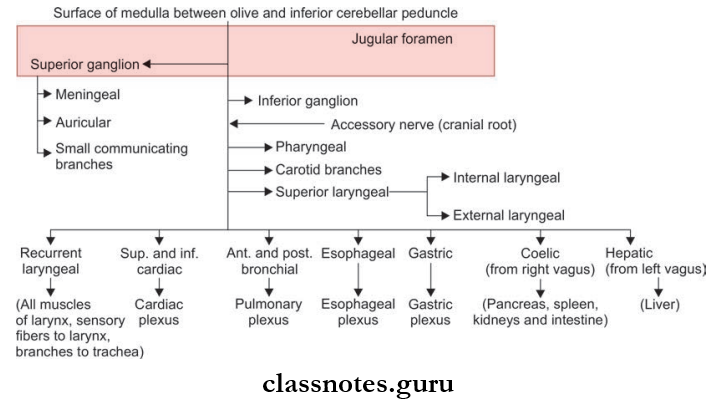
Vagus Nerve Branches and Distribution
- The branches of the vagus nerve in head and neck region is as follows:
- In the jugular foramen the superior ganglion gives of the following branches:
- Meningeal Branch: This supplies the dura of posterior cranial fossa after taking a recurrent course to enter the cranial cavity
- Auricular Branch (Alderman’s nerve): It enters the mastoid canaliculus and emerges through tympanomastoid fissure behind the external auditory meatus to supply the skin on the back of the meatus and adjoining part of auricle. It then enters the meatus between the bony and cartilaginous part to supply the flor and the tympanic membrane
- Communicating branches to glossopharyngeal and cranial root of accessory nerves and superior cervical ganglion.
- In the neck it gives of the following branches:
- The pharyngeal branch arises from the lower part of the inferior ganglion and chiefly contains fibers of the accessory nerve. It passes between external and internal carotid arteries and reaches near the middle constrictor of pharynx and takes part in formation of the pharyngeal plexus. It supplies:
- All muscles of pharynx except the stylopharyngeus (supplied by glossopharyngeal nerve)
- All muscles of soft palate except tensor palati (supplied by mandibular nerve).
- Superior laryngeal nerve arises from the inferior ganglion and runs downwards and forwards on the superior constrictor and reaches the middle constrictor to divide into external and internal laryngeal nerves.
- The external laryngeal nerve (motor) is a thin nerve that accompanies the superior thyroid artery and pierces the inferior constrictor and supplies the cricothyroid muscle. It also gives branches to the inferior constrictor and pharyngeal plexus
- The internal laryngeal nerve (sensory) is a thick nerve it passes downwards and forwards and pierces the thyrohyoid membrane and enters larynx and supplies:
- Mucous membrane of pharynx, epiglottis, vallecula
- Mucous membrane of larynx up to the level of vocal cords.
- Carotid branches supply the carotid body and sinus
- Right recurrent laryngeal nerve arises from the vagus in front of the right subclavian artery and winds around the first part of subclavian artery and then ascends up in the tracheoesophageal groove.
- Here it is related to inferior thyroid artery. It then passes deep to the inferior constrictor and enters larynx behind the cricothyroid joint and supplies:
- All intrinsic muscles of larynx except cricothyroid muscle
- Sensory supply to larynx below vocal cords
- Branches to trachea and esophagus
- Inferior constrictor
- Cardiac branches to the deep cardiac plexus.
- Cardiac branches: Superior and inferior. They enter thorax through thoracic inlet. Out of the four cardiac branches the left inferior goes to the superficial cardiac plexus and other three go to the deep cardiac plexus.
- In thorax the left recurrent laryngeal arises in the superior mediastinum and crosses the arch of aorta and hooks below the arch of the aorta on left side of ligamentum arteriosum and reaches tracheoesophageal groove and supplies structures similar to right recurrent laryngeal nerve.
Vagus Nerve Clinical Testing
- The nerve is tested by asking the patient to open his mouth and say ‘Ah’ and the palatal arches of two sides are compared
- In normal cases the soft palate rises in the midline
- In bilateral lesions the soft palate droops
- In unilateral lesions there is drooping of soft palate on one side and uvula deviates to the normal side.
Vagus Nerve Applied
- Various branches of the vagus nerve are affected due to lesions
- Recurrent laryngeal nerve palsies are most common due to malignant disease (25%) and surgical damage (20%) during operations of thyroid gland, neck, esophagus, heart, and lung
- Because of its longer course, lesions of left are more frequent than those of right
- High lesions of the vagus nerve, which affect the pharyngeal and superior laryngeal branches, cause difficulty in swallowing as well as vocal cords defects
- The Bilateral Lesions Can Cause:
- Nasal regurgitation of liquids while swallowing
- Nasal twang of voice
- Hoarseness of voice
- Flattening of palatal arches
- Cadaveric position of vocal cords
- Dysphagia.
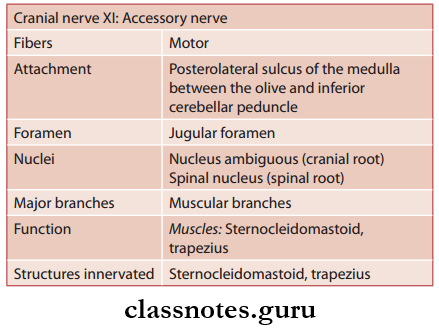
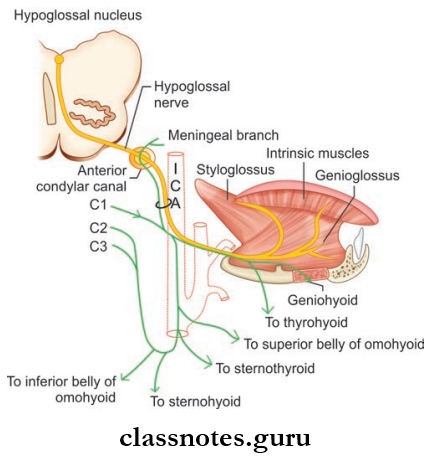
Question 9. Write a note on an accessory nerve.
Answer:
Accessory Nerve
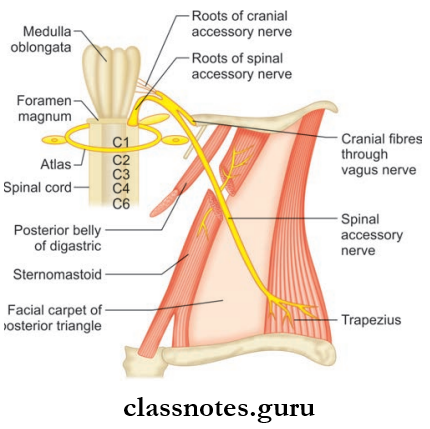
- Accessory Nerve is the 11 cranial nerve
- Accessory Nerve Is A Purely Motor Nerve And Has Two Roots: Cranial and spinal
- The cranial root is an accessory to vagus and its fibers are distributed through the vagus nerve
- The spinal root has an independent course and is regarded as an accessory nerve.
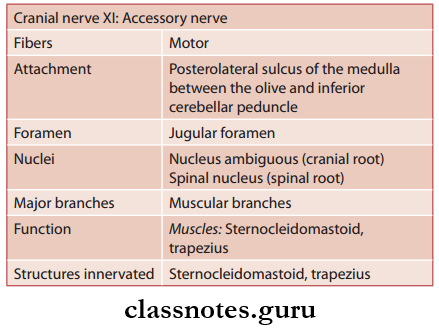
Accessory Nerve Functional Components
- General somatic efferent (GSE) fibers arise from the long spinal nucleus of the accessory nerve and provide motor supply to sternocleidomastoid and trapezius muscles
- Special visceral efferent (SVE) fibers arise from the nucleus ambiguus and provide motor supply to muscles of the soft palate, pharynx, and larynx.
Accessory Nerve Nuclei
- The cranial root arises from the lower part of the nucleus ambiguus
- The spinal root arises from a long spinal nucleus situated on the lateral part of the anterior grey column of the spinal cord of upper fie spinal segments.
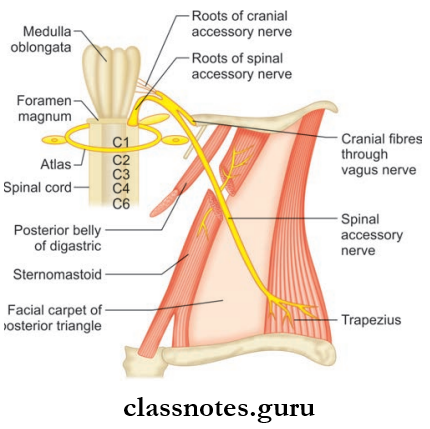
Accessory Nerve Course and Relations
- The Cranial Root
- It arises as 4–5 rootlets from the posterolateral sulcus of the medulla between the olive and inferior cerebellar peduncle
- These rootlets join to form a trunk and then run laterally to the 9th, 10th cranial nerves and spinal root and reach the jugular foramen and joins with the spinal root
- It then gets separated from the spinal root as it emerges from the jugular foramen and finally fuses with the vagus nerve at the inferior ganglion and gets distributed through branches of the vagus.
- The Spinal Root
- The Spinal Root arises from the upper fie spinal segments as a row of rootlets between the ventral and dorsal roots
- These rootlets unite to form a trunk
- The Spinal Root then ascends upwards to the vertebral canal and enters the cranial cavity through foramen magnum behind the vertebral artery
- The Spinal Root then reaches the jugular foramen and unites with the cranial root comes out through the middle part of the jugular foramen and separates from the cranial root after coming out
- The Spinal Root then descends vertically downwards between internal jugular vein and the internal carotid artery
- The Spinal Root then turns downwards and backwards at the midway between the mastoid process and the angle of the mandible and crosses the internal jugular vein
- The Spinal Root is crossed by occipital artery and is accompanied by the sternocleidomastoid branch of the occipital artery and is surrounded by lymph nodes
- The Spinal Root then pierces the sternocleidomastoid muscle at the junction of upper one-fourth and lower three-fourths communicates with C2 and C3 nerves and supplies the muscle
- The nerve then enters the posterior triangle after emerging through the posterior border of the sternocleidomastoid and then runs downwards and backward to get embedded in the fascial roof and lies over levator scapulae
- The nerve leaves the posterior triangle by passing deep to the anterior border of the trapezius 5 cm above the clavicle and communicates with the C3 and C4 nerves and ends by supplying trapezius.
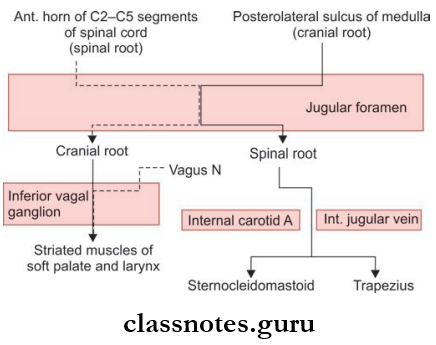
Accessory Nerve Distribution
- The Cranial Root (via vagus and pharyngeal plexus) supplies:
- All muscles of palate except tensor palatine and tensor tympani
- All muscles of pharynx except stylopharyngeus
- All intrinsic muscles of the larynx.
- The Spinal Root Supplies:
- Sternocleidomastoid along with C2 and C3 nerves
- Trapezius along with C3 and C4 nerves.
Accessory Nerve Clinical Testing
- The sternocleidomastoid muscle is tested by asking the patient to turn his face to the opposite against the resistance offered by the examiner’s hand. In normal conditions, a person can do it and sternocleidomastoid stands out prominently
- The trapezius is tested by asking the patient to shrug his shoulder against resistance.
Accessory Nerve Applied
- Lesions of the spinal part of accessory nerve will result in paralysis of the sternocleidomastoid and trapezius muscles
- The sternocleidomastoid will atrophy and there will be a weakness in turning the head to the opposite side
- The trapezius muscle will also atrophy and the shoulder will droop on that side, there will also be weakness and difficulty in raising the arm above the horizontal
- Lesions of the spinal part of the nerve may occur anywhere along its course and mostly result from tumors or trauma from stab or gunshot wounds in the neck.
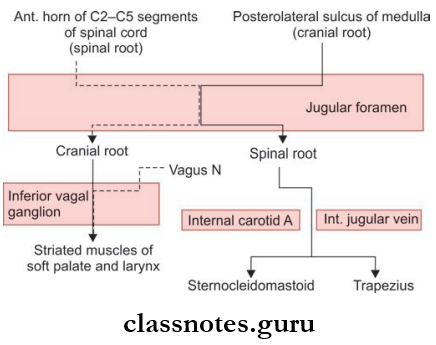
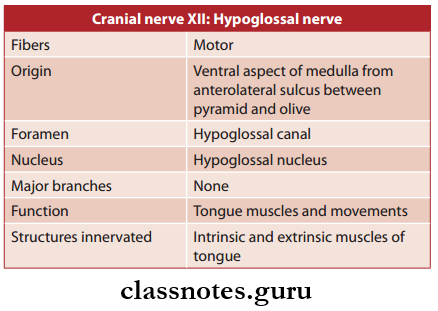
Question 10. Write a note on hypoglossal nerve.
Answer:
Hypoglossal Nerve
- It is the 12 cranial nerve
- It is purely a motor nerve.
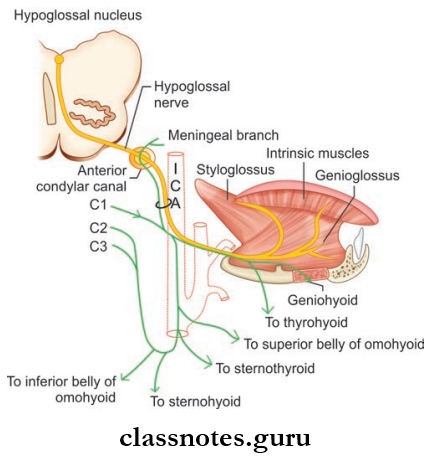
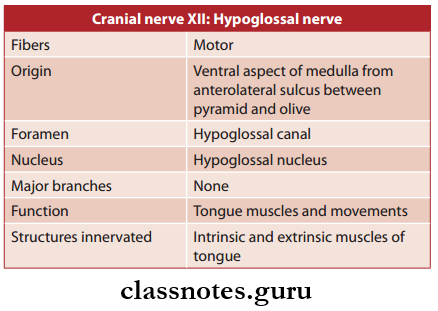
Hypoglossal Nerve Functional Components: General somatic efferent (GSE) fibers arise from the hypoglossal nucleus and supply all the muscles of the tongue.
Hypoglossal Nerve Nucleus: It is a 2 cm long structure that lies at the floor of the fourth ventricle beneath the hypoglossal triangle.
Hypoglossal Nerve Course and Relations
- Hypoglossal Nerve arises from the ventral aspect of the medulla from the anterolateral sulcus between the pyramid and olive as 10–15 rootlets
- The rootlets are attached in line with the rootlets of ventral root of 1st cervical spinal nerve
- The rootlets run laterally and pass behind the vertebral artery to form two roots which pierce the dura mater near the hypoglossal canal and enter the hypoglossal canal
- In the canal the two roots unite to form a single trunk and come out of the cranial cavity
- Hypoglossal Nerve then lies deep to the internal carotid artery and the 10th cranial nerve passes downwards and laterally and reaches the interval between internal carotid artery and internal jugular vein
- Hypoglossal Nerve then descends vertically up to the level of the angle of the mandible
- Hypoglossal Nerve then curves forwards and crosses the internal and external carotid arteries and a loop of lingual artery reach the posterior margin of hyoglossus muscle and runs on its superficial surface below the deep part of the submandibular gland
- At the anterior margin of the hyoglossus muscle, it lies on the genioglossus and then runs forward and upwards up to tip of the tongue to supply the muscles.
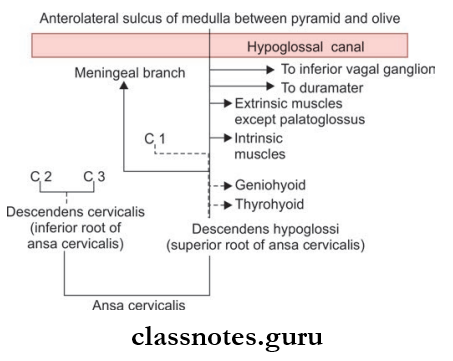
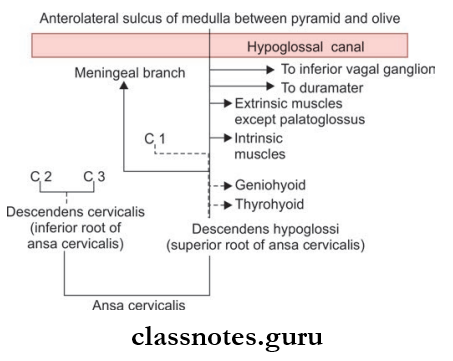
Hypoglossal Nerve Branches And Distribution: The nerve has the following branches:
- Branches of the hypoglossal proper supply all muscles of the tongue except palatoglossus which is supplied by the cranial root of the accessory nerve
- Branches of the hypoglossal nerve containing C1 fiers which include:
- Meningeal branch: After coming through the hypoglossal canal it takes the recurrent course enters the cranial cavity and supplies the dura of the posterior cranial fossa
- Descendants hypoglossal Or Upper Root Of Ansa Cervicalis: It arises while crossing the internal carotid artery and runs downwards to join the inferior root of ansa cervicalis
- Nerve To Thyrohyoid: It crosses the greater cornu of the hyoid bone to reach the muscle
- Nerve To Geniohyoid: It arises from above the hyoid bone.
Hypoglossal Nerve Clinical Testing
- To assess the hypoglossal nerve, the genioglossus muscles are assessed
- The patient is asked to protrude the tongue
- If the nerve of both sides is intact the tongue lies in the midline
- If the hypoglossal nerve of one side is damaged the tongue deviates to the side of the lesion due to the unopposed action of muscles of normal side
- If nerves of both sides are affected the patient is unable to protrude the tongue.
Hypoglossal Nerve Applied
- Infranuclear hypoglossal nerve lesion causes unilateral lingual paralysis and hemiatrophy. The protruded tongue deviates to the paralyzed side on retraction.
- The wasted and paralyzed side also rises higher than the unaffected side. Lesions of the hypoglossal nerve may occur anywhere along its course and may result from tumor, demyelinating diseases, syringomyelia, and vascular accidents
- In case of supranuclear lesions there is paralysis without wasting. The tongue moves sluggishly resulting in defective speech and on protrusion, the tongue deviates to opposite side. Fasciculation can also be present.
Cranial Nerves Multiple Choice Question And Answers
Question 1. All of the following structures pass through the jugular foramen except:
- Glossopharyngeal nerve
- Vagus nerve
- Inferior petrosal sinus
- Hypoglossal nerve
Answer: 4. Hypoglossal nerve
Question 2. All of the following are muscle not supplied by glossopharyngeus except:
- Palatopharyngeus
- Salpingopharyngeus
- Stylopharyngeus
- Superior constrictor of pharynx
Answer: 3. Stylopharyngeus
Question 3. All of the following branches of left vagus arise in neck except:
- Pharyngeal branch
- Branch to carotid body
- Recurrent laryngeal
- Cardiac branches
Answer: 3. Recurrent laryngeal
Question 4. In lesions of right hypoglossal nerve:
- Tongue deviates to right side on protrusion
- Tongue deviated to left side on protrusion
- Tongue fails to protrude at all
- None of the above
Answer: 1. Tongue deviates to right side on protrusion
Question 5. The incorrect statement about accessory nerve is:
- Its both roots arise from the medulla
- Its cranial root is distributed through vagus nerve
- Its spinal root supplies sternocleidomastoid and trapezius
- It exits skull through jugular foramen
Answer: 1. Its both roots arise from the medulla