Cast Metal Restorations Important Notes
1. Pickling
- Pickling is the process of cleaning the gold casting with 50% warm HCl
- Used to remove surface oxides from casting
- Pickling is not a routine procedure
- Used only when indicated
2. Casting Defects
- Distortion
- Surface roughness and irregularities
- Discoloration
- Porosity
- Solidification defects
- Trapped gases
- Residual air
Read And Learn More: Operative Dentistry Question And Answers
3. Types Of Casting Machines
- Centrifugal Casting Machine
- Uses centrifugal force to accelerate the flow of molten metal into the mold space
- Air pressure Casting Machine
- Compressed gas is used to force the molten alloy into the mold
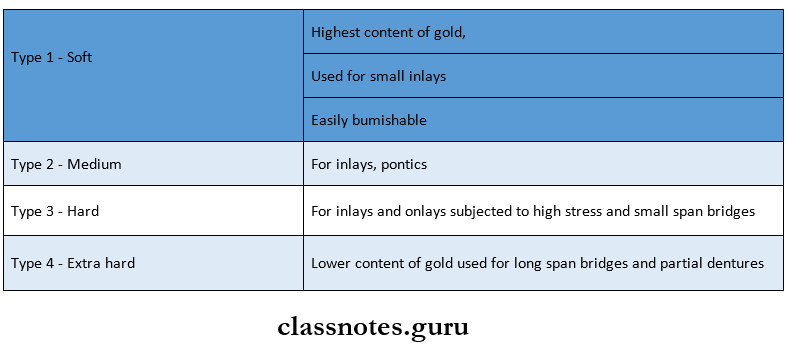
4. Types Of Cast Metal Alloys
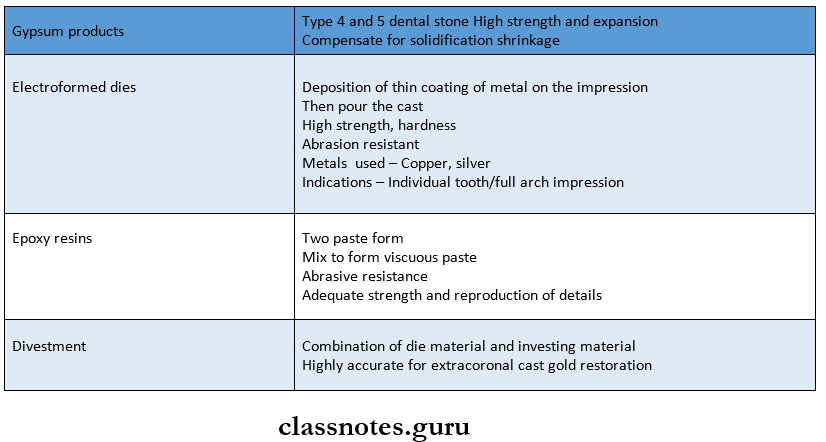
5. Types Of Die Materials Used
- Gypsum products
- Electroformed dies
- Epoxy resins
- Divestment
6. Properties Of Base Metal Alloys
- Low density
- Low percentage elongation
- High fusing temperature
- High hardness
- Tarnish and corrosion resistance
7. Retention Forms In Cast Restorations
- Grooves
- Bevel
- Internal box
- External box
- Pins, slots, skirt, collar
- Cusp capping
- Reciprocal retention
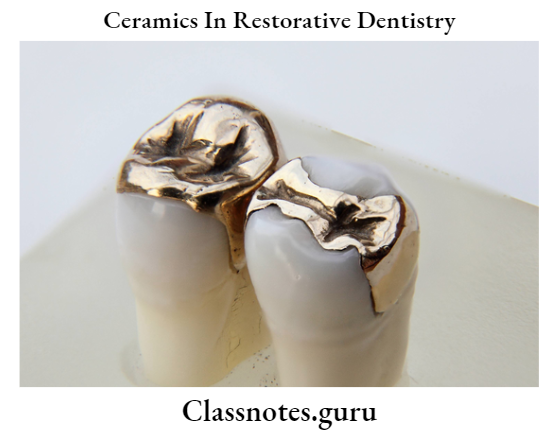
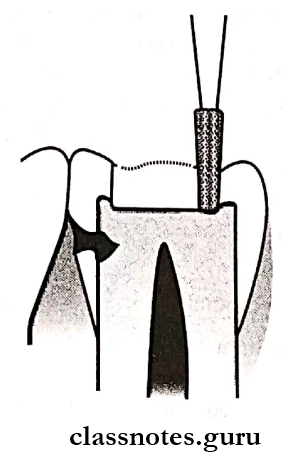
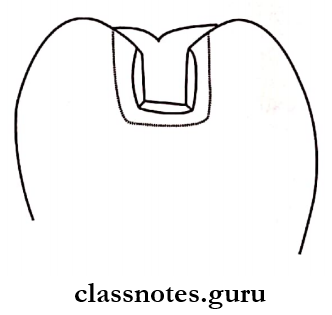
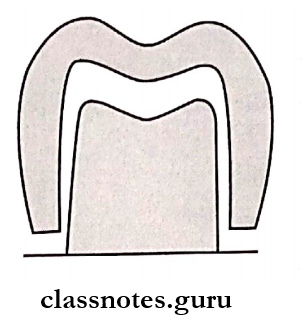
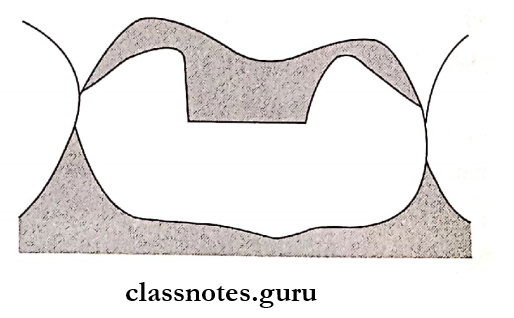
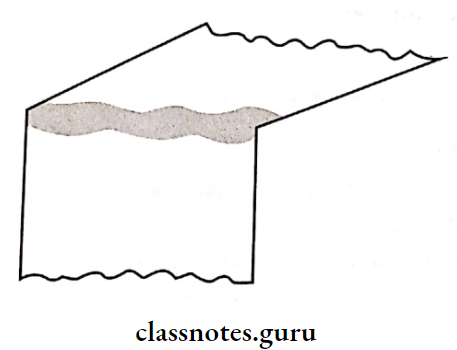
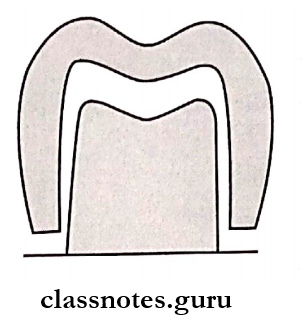
8. Onlay
- They are partly intracoronal and partly extra-coronal types of restoration
- Onlay has cuspal protection
- Onlay is mainly indicated when the width of the lesion exceeds one-third of the intercuspal distance
- Features of cavity preparation:
- Capping of functional cusps
- Cuspal reduction 1.5 mm
- The bevel used is a hollow ground long bevel in the intracoronal portion and a counter bevel in the extra coronal portion
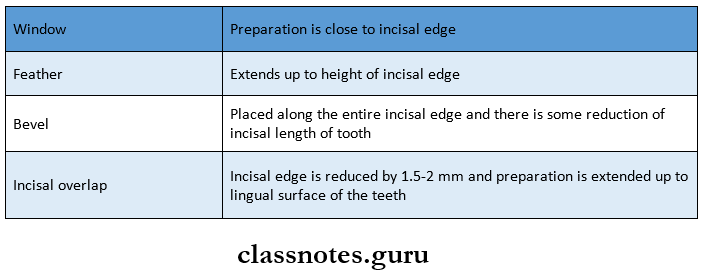
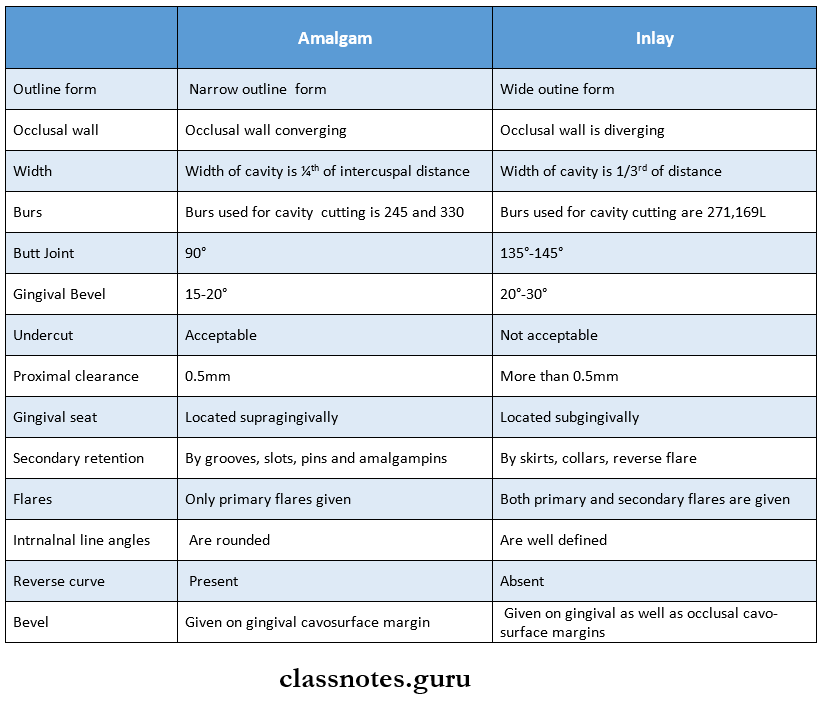
- Table:
- Onlay is a transitional area between the intracoronal and extra-coronal portion
- Onlay should be flat
- Relieved from opposing cusps by 1.5 mm
- There should be 3 tables prepared for each cusp in different directions
- Onlay provides retention and resistance form
- Shoeing of nonfunctional cusps
- Provides retention and resistance form over the nonfunctional cusp
9. Composition Of Wax
10. Principles For Correct Spring
- Use of proper gauge of sprue
- Use of proper length of sprue
- Should be attached to the bulkiest portion of the wax pattern
- Attach it to the wax pattern with little heat to avoid distortion
11. Uses Of Casting Ring Liner
- Permits unrestricted expansion of the investment
- Acts as a cushion between rapidly cooling metal ring and the more slowly cooling investment during the casting and crystallization of gold
12. Objectives Of Burnout
- Complete removal of wax pattern
- Elimination of excess water from the investment
- Production of thermal expansion
Cast Metal Restorations Long Essays
Question 1. Classify casting defects describe mesioocclusal cavity preparation for gold inlay on a mandibular first molar.
(or)
Describe class 2 mesioocclusal cavity preparation for gold inlay on mandibular 1 molar tooth.
Answer:
Casting Defects:
- Distortion
- Surface roughness and irregularities
- Discoloration
- Porosity
- Solidification Defects
- Trapped Gases
- Pinhole
- Gas inclusion
- Subsurface
- Residual Air
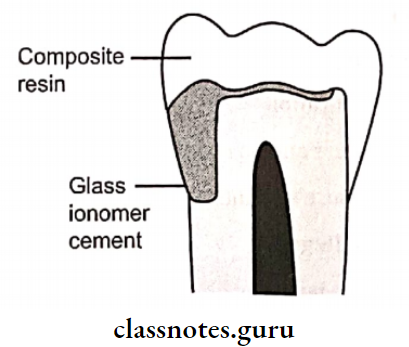
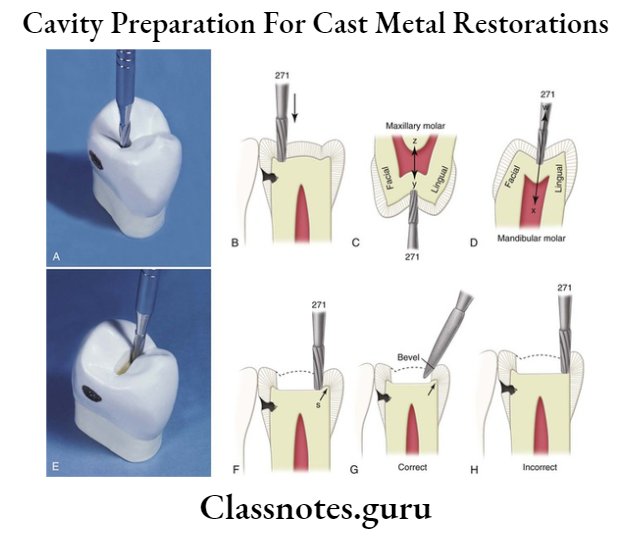
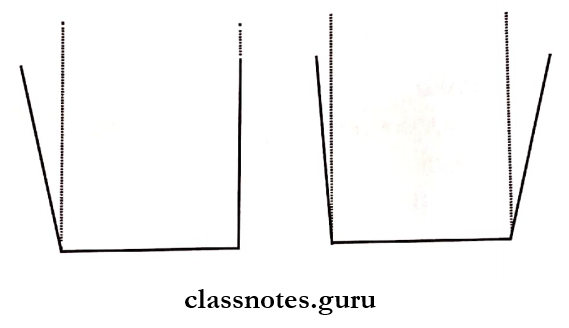
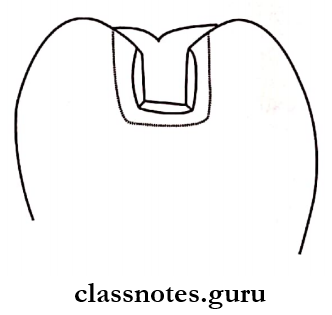
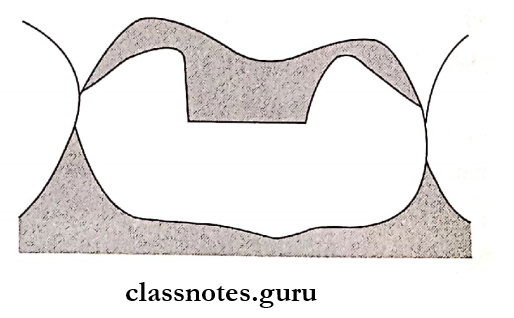
Class 2 Inlay Cavity Preparation
1. Initial Tooth Preparation
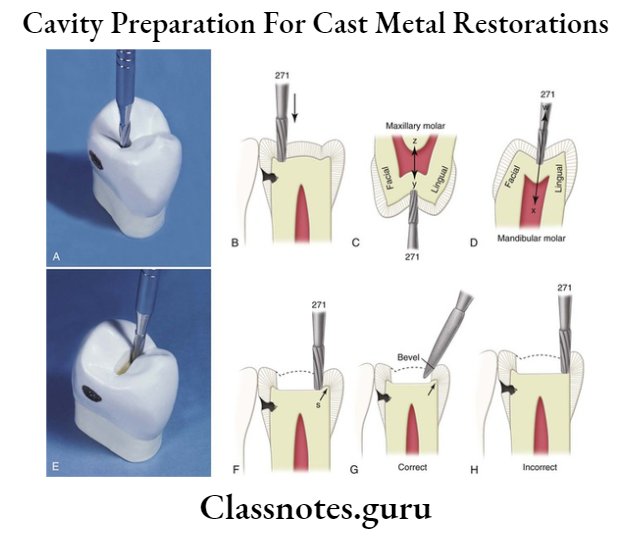
Occlusal Outline Form:
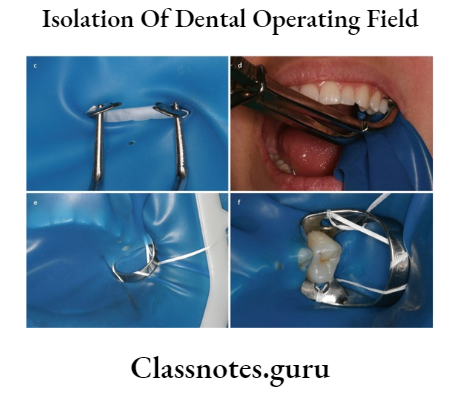
- Anesthetize and isolate the tooth
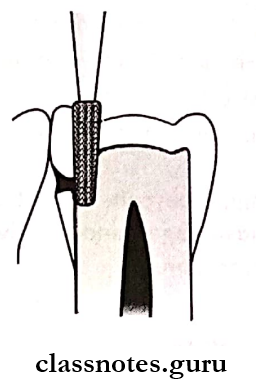
- Penetrate the tooth with no.271 bur from the mesial surface
- Extend upto central fissure to uninvolved marginal ridge
- Maintain a uniform pulpal depth of 1.5mm
- Preserve distal marginal ridge
- Extend up to the smooth areas of the buccal and lingual slopes of the cusps of a tooth.
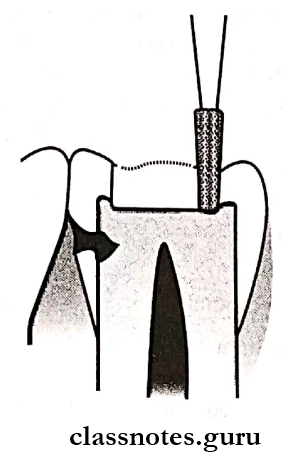
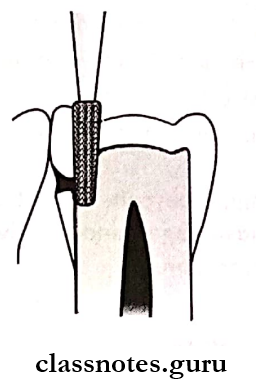
Proximal Box Preparation:
- Mesial ditch cut is given using the same bur
- Width of cut 0.8mm, 0.5 mm in dentin, and 0.3 mm in enamel
- Extend it faciolingually
- Extend gingivally
- Provide 0.5mm of clearance
- Break the contact using cuts over facial and lingual walls using No.271 bur
Resistance And Retention Form:
- Flat pulpal floor
- Box-shaped preparation
- The extra thickness of gold
- Occlusal step
- Dovetail
2. Final Preparation:
1. Removal Of Remaining Caries, Old Restorative Material
- Removal of soft caries and infected dentin with a spoon excavator
2. Pulp Protection
- Use of pulp protective materials
3. Secondary Resistance And retention Forms
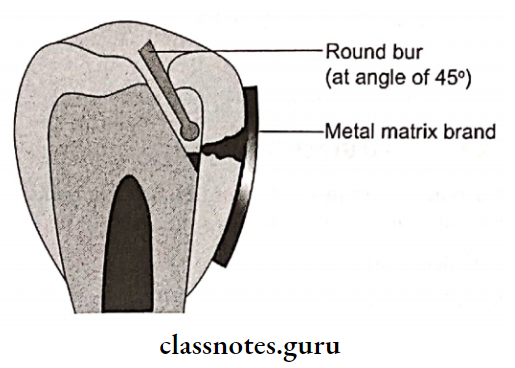
- Retention grooves were placed in the facial axial and in coaxial line angles using 169L carbide bur
- Bevels
- Gingival bevel 45° to the preparation
- Include one-half the width of the gingival wall
- Occlusal bevel At occlusal 1/3rd of adjacent occlusal wall
- Removes unsupported enamel
4. Inspecting, Cleaning, And Rinsing
- Clean the prepared tooth with air/water spray
- Dry it with a cotton pellet
- Inspect the angles and margins
Question 3. Define Inlay Describe the Indications, Contraindications, advantages, and disadvantages of cast gold restoration.
Answer:
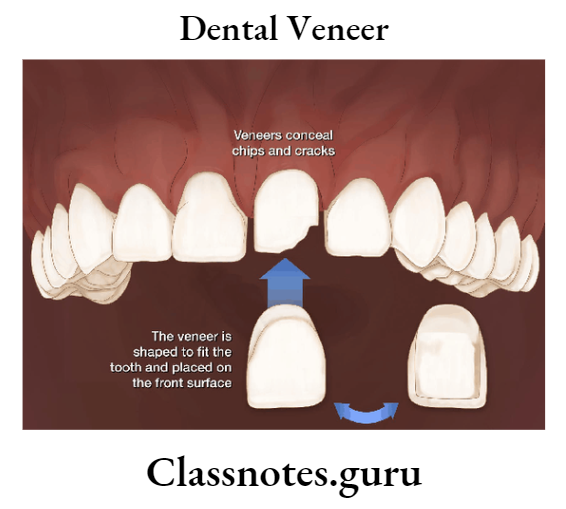
Definition Of Inlay:
- An inlay is an indirect intracoronal restoration which is fabricated extra orally and cemented in the prepared tooth
Inlay Indications:
- Extensive proximal caries
- Patients with good oral hygiene and low caries index
- Postendodontic restoration
- Teeth with extensive restoration
- To maintain proper tooth contact and contour
- Presence of cast metal restoration
- Abutment teeth
- Teeth with heavy occlusal forces and attrition
Inlay Contraindications:
- Aesthetic consideration
- Patients with high caries index
- Young patients
- Periodontally weak teeth
- Extensive caries involving facial and lingual and multiple surfaces
- Low economic status
- Presence of dissimilar restoration
- Extensive occlusal wear facets
Inlay Advantages:
- Better reproduction of details
- Better wear resistant
- Biocompatible
- Strengthens remaining tooth structure
- Fewer chances of voids
- Easy to polish
- Less chair time
Inlay Disadvantages:
- Need of temporary restoration
- Expensive
- Technique sensitive
- Difficult to repair
- Weak tooth bonding
- Unesthetic
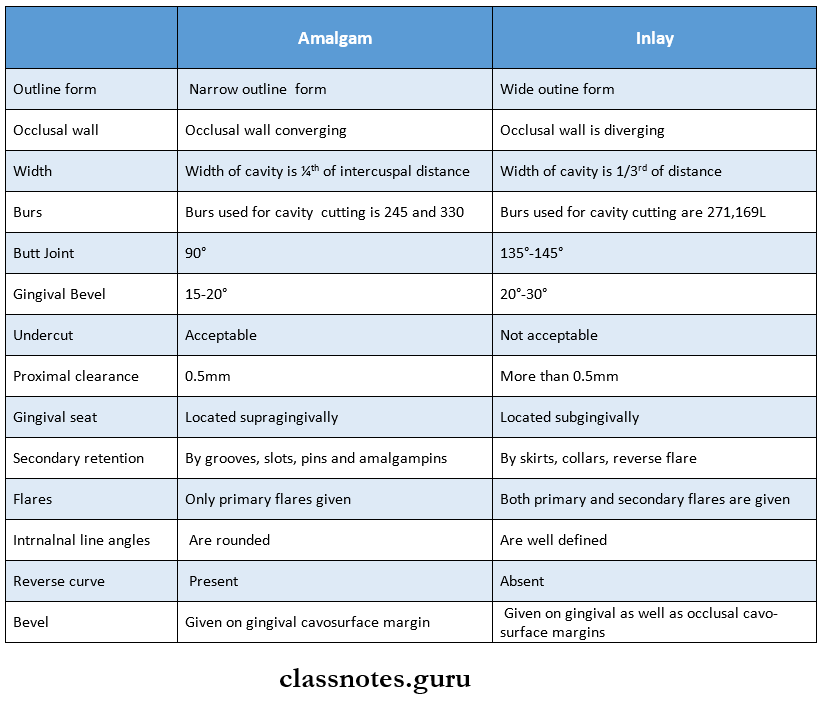
Question 4. Give the difference in cavity preparation between amalgam and gold inlay.
Answer:
Differences In Cavity Preparation Between Amalgam And Gold Inlay:
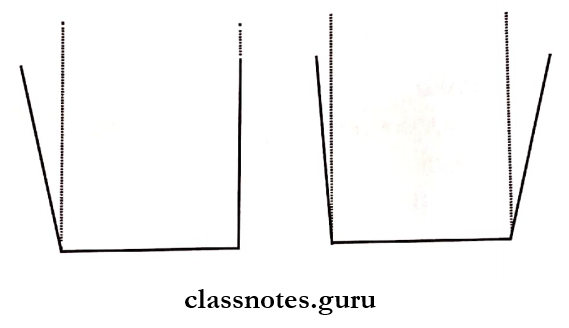
Question 5 Define retention form. How it is achieved in cast restoration.
Answer:
Retention Form:
- Retention Form is that form of cavity that resists the displacement of restoration from tipping and lifting forces
Retention In Cast Restorations:
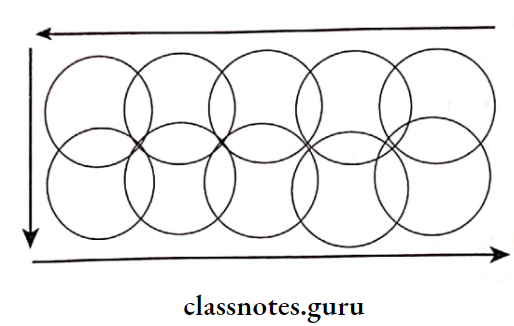
1. Grooves:
Resist lateral displacement of restoration
- Internal Grooves
- Indicated in a shallow and small cavity
- Contraindicated in a deep cavity
- External Grooves
- Indicated in extra coronal preparation
- Prevents dislocation
- May be prepared in stepped form
2. Reverse Bevel:
- Indication Class 1, 2, 3 restoration
- Presence of sufficient gingival floor
- Placed over the gingival floor with an incline gingivally and axially
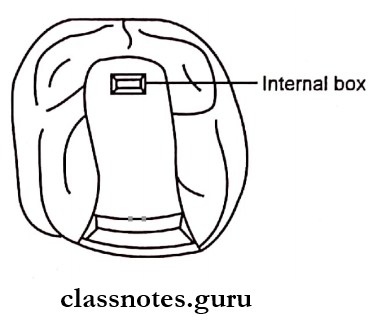
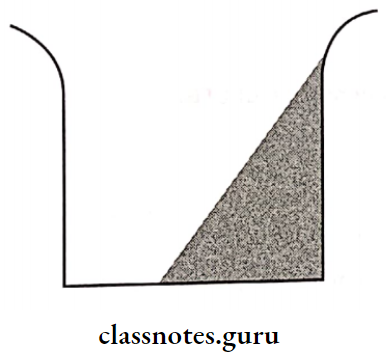
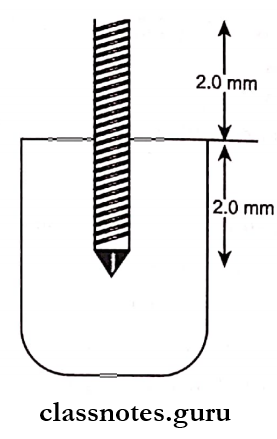
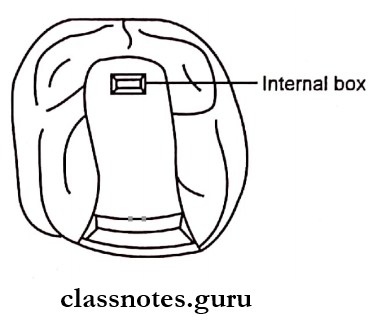
3. Internal Box:
- Indicated in the presence of sufficient dentin
- Contraindicated in class IV and V preparation
- Have vertical walls prepared in dentin
- Increases retention
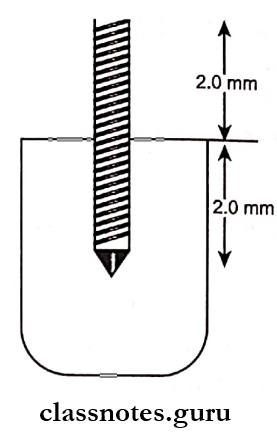
- It should be 2 mm in dimension
4. External box:
- Box with an opening to the axial surface of the tooth
- The peripheral portion can be flared/beveled
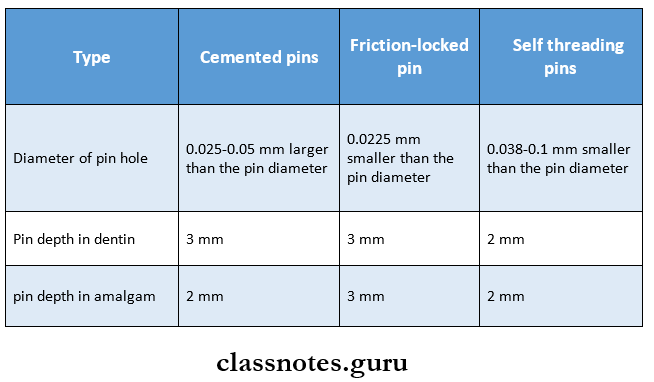
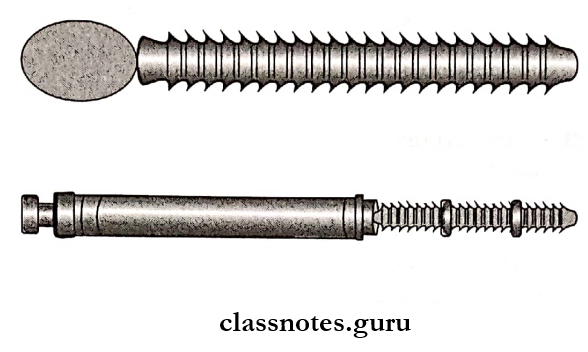
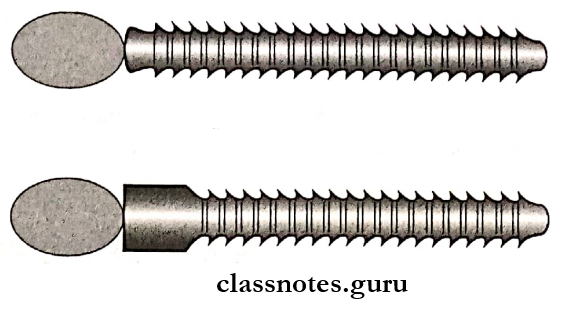
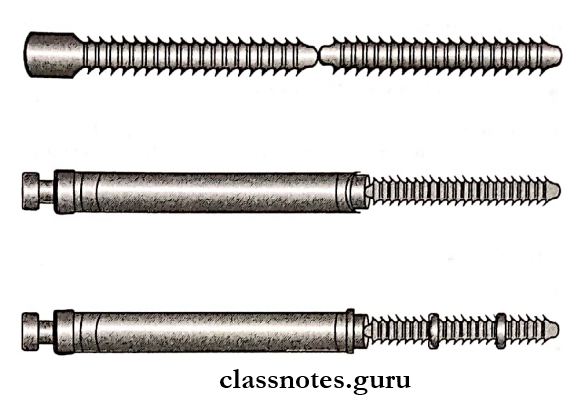
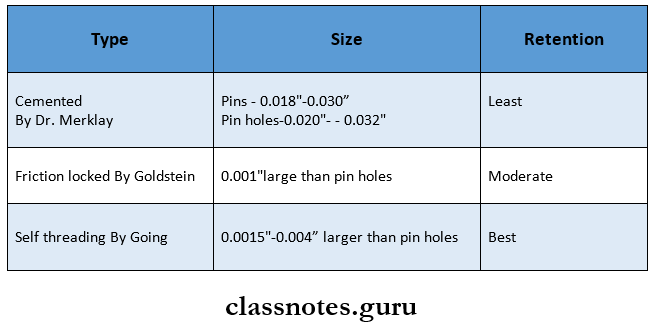
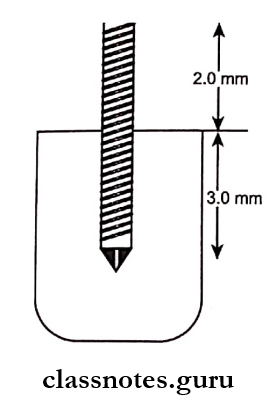
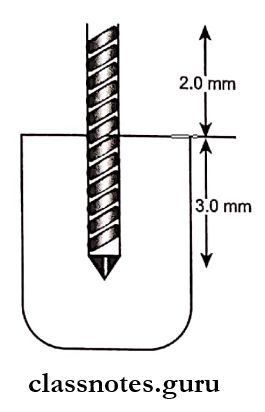
5. Pins:
- Types of pins used Cemented, threaded, parallel, cast, and wrought
6. Slot:
- Indicated in the shallow cavity, restricted occlusal anatomy
- Have a depth of 23mm
7. Skirt:
- Indicated in missing wall
8. Collar:
- Depth 1.52mm, surface extension
- Indication Grossly carious teeth
- Short teeth
9. Cusp Capping:
- Provide sufficient height of cusp
10. Reciprocal Retention:
- Placement of retention made at every end of the preparation
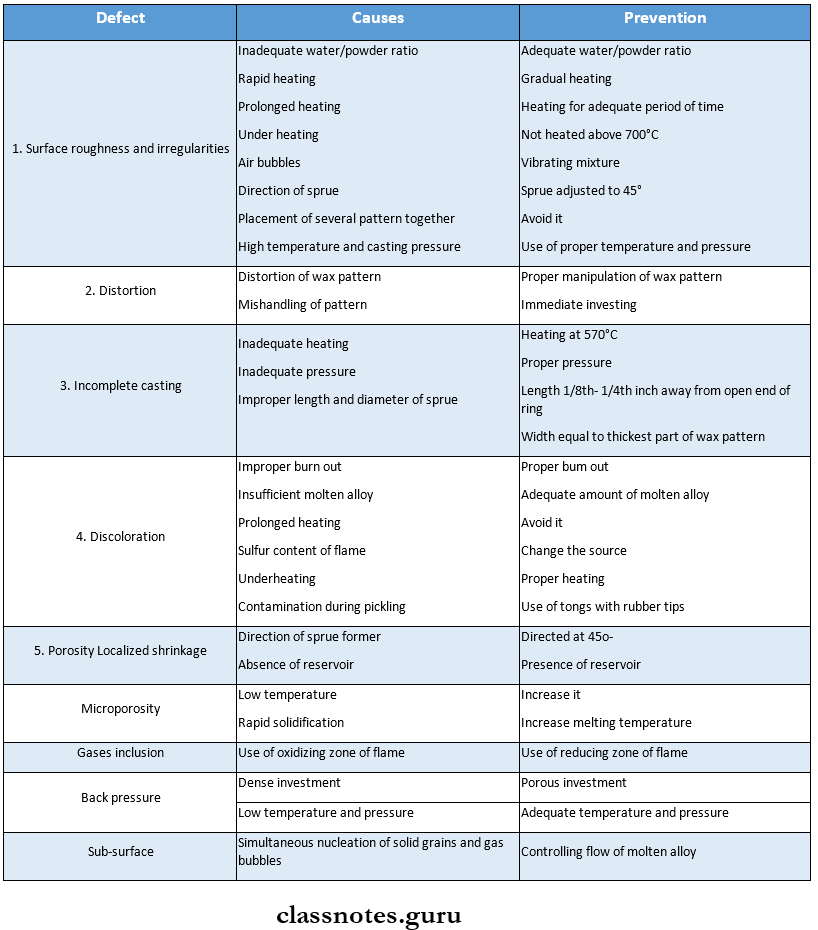
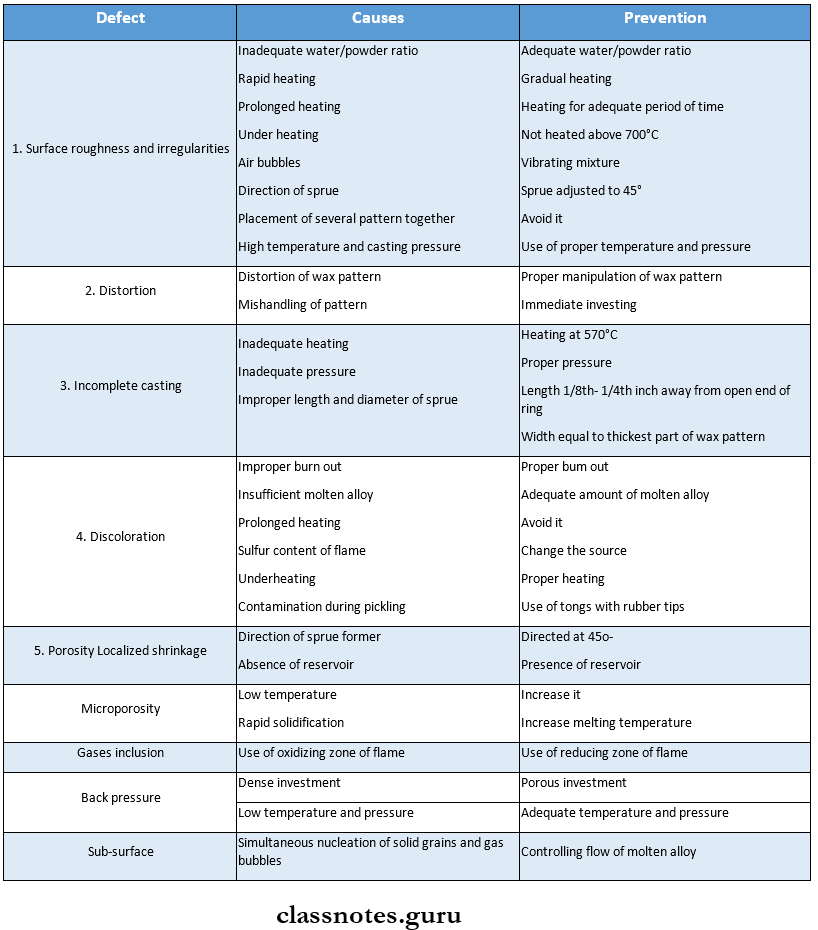
Question 6. Discuss the causes of casting defects and their prevention.
Answer:
The Causes Of Casting Defects And Their Prevention:
- Casting defects can be prevented by following various steps systematically
- Types of casting defects along with their causes and prevention are as follows
Cast Metal Restorations Short Essays
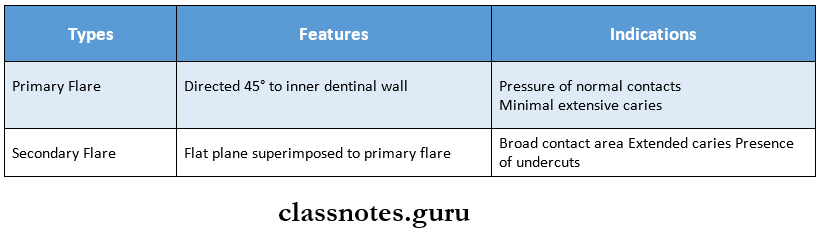
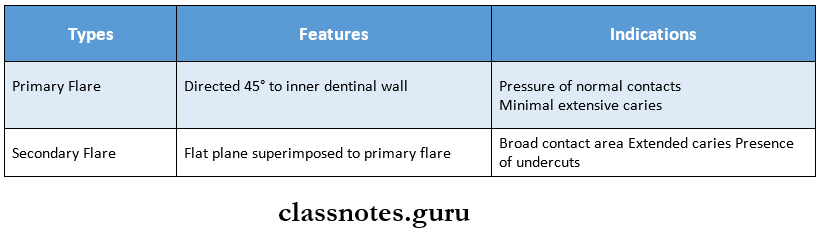
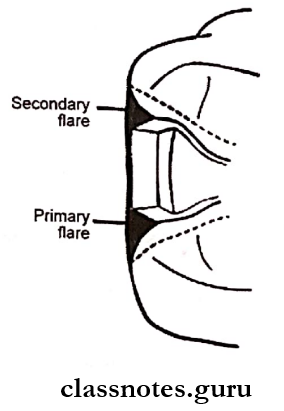
Question 1. Bevel and flares.
or
Circumferential Tie.
Answer:
Circumferential Tie:
- Circumferential Tie refers to the design of the cavosurface margin of an inlay tooth preparation
Significance:
- The cavosurface margin is the weakest part of the restoration
- To strengthen it, it is designed by incorporating bevels and flares
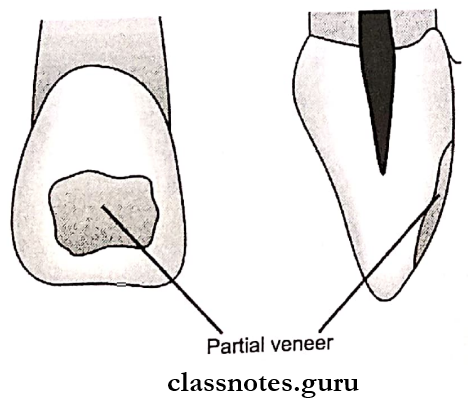
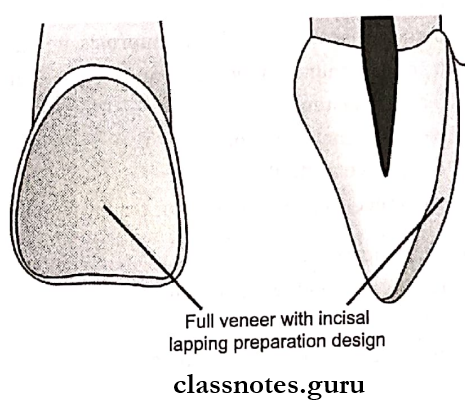
1. Bevels:
- Bevels is the inclination that one surface makes with another when not at right angles
Bevels Types:
- Partial Bevel
- Involving less than 2/3rd of enamel
- Use of type 1 casting alloys
- Short Bevel
- Involves full thickness of enamel
- Use of type 1 and 2 alloys
- Long Bevel
- Involves full enamel and half dentin
- Use in type 1, 2, and 2 alloys
- Full Bevel
- Involves complete enamel and dentin
- Hollow ground Bevel
- Concave in shape
- Counter Bevel
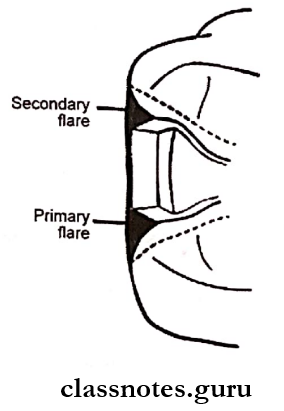
1. Flares: They are concave/flat peripheral portions of the facial/lingual proximal walls
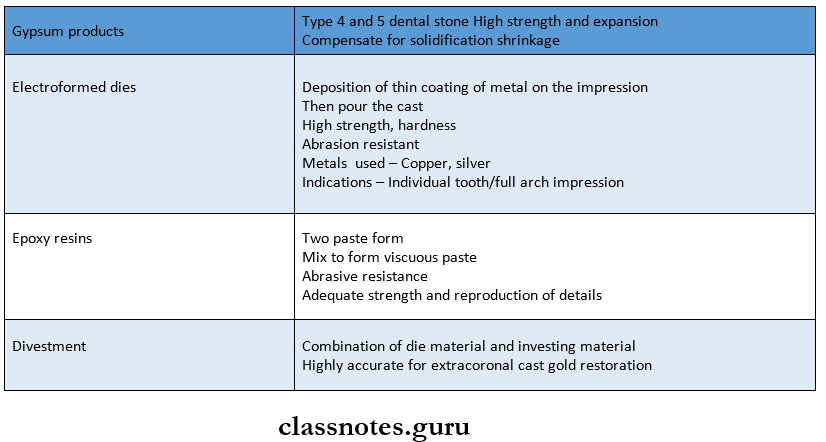
Question 2. Die materials.
Answer:
Die materials Properties:
- Compatible with impression materials
- Have smooth surface
- Have adequate strength
- Easy to fabricate
- Have contrasting color
- Reproduce accurate details
Die materials Materials:
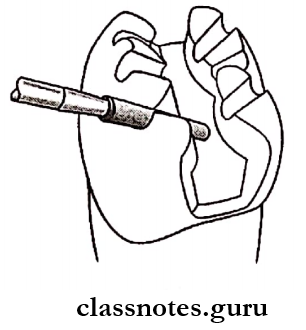
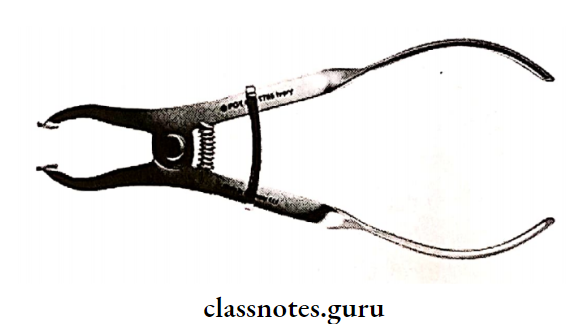
Question 3. Direct Wax Pattern.
Answer:
Direct Wax Pattern:
- Prepared in the oral cavity
- Done using matrix band or without it
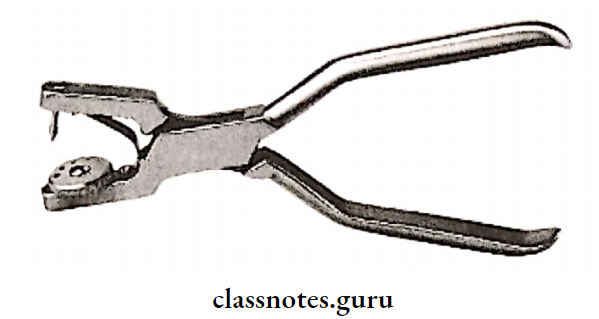
Direct Wax Pattern Technique:
Isolate the tooth
↓
Apply band and retainer
↓
Soften inlay wax
↓
Compress over the prepared tooth
↓
Hold it with finger pressure til it sets
↓
Burnish it
↓
Remove band and retainer
↓
Check for centric occlusion
↓
Check for high points
↓
Smoothen it
↓
Attach sprue former and reservoir
↓
Remove the wax pattern
Direct Wax Pattern Advantages:
- Fewer discrepancies
- Less laboratory work
Direct Wax Pattern Disadvantages:
- Require more skill
- Requires more chair side time
Question 4. Indirect Wax Pattern.
Answer:
Indirect Wax Pattern:
- Prepared outside the oral cavity
- Use of type 11 inlay wax
Indirect Wax Pattern Steps:
Lubricate the die
↓
Adapt inlay wax over it
↓
Carve the wax
↓
Attach sprue former
↓
Remove the wax pattern
Indirect Wax Pattern Advantages:
- Less chair time
- Finishing and polishing
- This can be done on a die
Indirect Wax Pattern Disadvantages:
- More laboratory work
- Errors due to inadequate casting
Question 5. Sprue.
Answer:
Sprue:
- Provides a channel so that molten metal flows into mold space after the wax pattern has been eliminated.
Sprue Types:
Sprue Functions:
- Provides a channel for the flow of molten alloy
- Provides reservoir to compensate for shrinkage
- Provides a channel for wax elimination
Sprue Requirements:
- Diameter Greater than the thickest part of the wax pattern
- Attachment to the thickest part of the wax pattern
- Sprue length such that the end of the wax pattern is l/8th to l/4th inch away from the open end of the casting ring
- Direction 45 to the bulkiest portion of the wax
- ReservoirTo compensate shrinkage
Question 6. Casting machines.
Answer:
Casting machines Types:
1. Centrifugal Casting Machine:
- Cheapest
- Used for small casting
- Uses centrifugal force to accelerate the flow of mol¬ten metal into the mold space
Casting Machines Steps:
Heat the ring at 1200°F for 15 minutes
↓
Move the arm of casting machine 23 turns clockwise and
lock it
↓
Heat the gold alloy
↓
Place the ring in the casting machine
↓
Release the lock of the arm
↓
This forces molten gold into a mold
↓
Recover the ring from the casting machine and cool it
↓
Removes the casting and cleans it
2. Air pressure Casting Machine:
- Compressed air/gases like carbon dioxide or nitrogen are used to force the molten alloy into the mold.
Question 7. CADCAM for Inlay.
Answer:
CADCAM For Inlay:
- CADCAM indicates Computer Aided Design Computer Aided Machine
- In it, the whole casting design is fabricated
- This design is fed up with the computer
- The whole design is scanned
- It is then fabricated into the final prosthesis
- The computer is connected to a machine that processes the prosthesis
- Thus, the machining process of the prosthesis according to the design fabricated by the computer
Question 8. Types of Cast Gold Alloys.
Answer:
Types of Cast Gold Alloys:
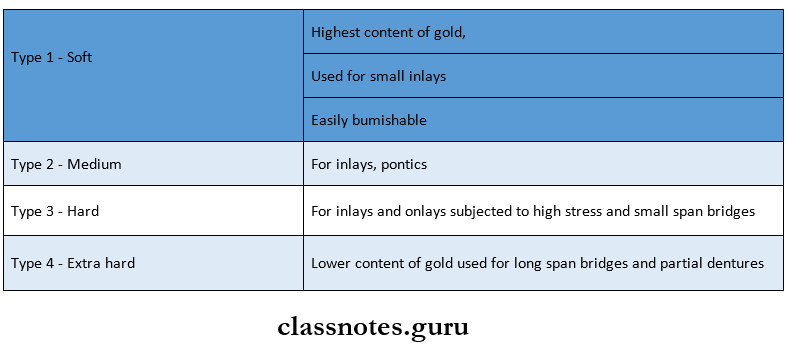
Type 1 Soft
- Used for fabrication of small inlays
- Low strength
- Easily burnished
- Gold content7583%
Type 2 Medium
- Used for fabrication of inlays and onlays subjected to moderate stresses
- Cannot be heat treated
- Gold content7075%
Type 3Hard
- Used for high-stresses
- High strength
- Can be heat-treated
- Gold content6570%
Type 4 Extra Hard:
- Used for crowns, bridges, and removable partial dentures
- Increased hardness
- Can be heat-treated
- Gold content 60%
Question 9. Indications and contraindications of Onlay
Answer:
Indications And Contraindications Of Onlay:
Only:
- Indications And Contraindications Of Onlay is a combination of intracoronal and extra-coronal cast restoration which covers one or more cusps
Indications And Contraindications Of Onlay Indications:
- Extensive weakened tooth due to caries or large restoration
- As post-endodontic restoration
- Presence of other cast restorations in adjacent or opposing teeth
- When the mesiodistal diameter of the tooth needs to be extended
- To correct the occlusal plane
- As an abutment for RPD
Indications And Contraindications Of Onlay Contraindications:
- Patients with high caries rate
- Young patients
- Short clinical crown height
Cast Metal Restorations Short Answers
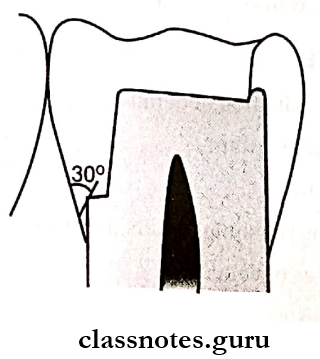
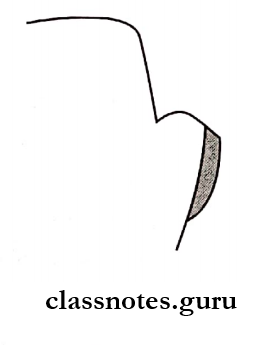
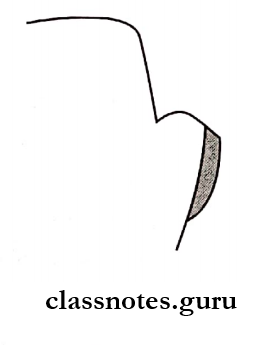
Question 1. Reverse bevel.
Answer:
Reverse Bevel:
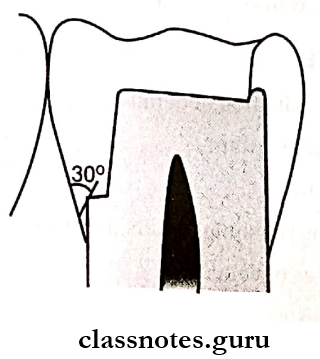
- A reverse bevel is a bevel of generous width that is prepared on the facial margin of a reduced cusp with a flame-shaped, fine grit diamond instrument
- Reverse Bevel width should extend beyond any occlusal contact with opposing teeth
- Reverse Bevel should be at an angle that results in a 30-degree marginal metal
- Reverse Bevel should be wide enough so that the cave surface margin is beyond any contact with the opposing dentition
Question 2. Sprue former.
Answer:
Sprue Former:
- A sprue former is made of wax, plastic, or metal
- Thickness is in proportion to the wax pattern
Sprue Former Functions:
- To form a mount for the wax pattern
- To create a channel for the elimination of wax during burnout
- Forms channel for entry of metal which compensates for allo£ shrinkage during solidification
Question 3. Porosities in casting.
Answer:
Porosities In Casting:
Porosities In Casting Types:
1. Caused By Solidification Shrinkage
- Localized shrinkage porosity
- Suck back porosity
- Microporosity
2. Caused By Gas
- Pinhole porosity
- Gas inclusion
- Subsurface porosity
3. Caused By Air Entrapment:
Porosities In Casting Prevention:
- Use of correct sprue thickness
- Correct placement of sprue
- Use of reservoir
- Use of adequate casting forces
- Use of porous investment and proper vents
- Place the pattern away from the end of the ring
Question 4. Inlay Taper.
Answer:
Inlay Taper:
- Ideally, a tooth preparation should have slight diverg¬ing walls from gingival to occlusal surface
Inlay Taper Value:
- Optimal taper25° per wall
- For short longitudinal walls 2° taper
- For high longitudinal walls Increased but not more than 10°
- Preparation should never have one side with more taper than the other
- For shallow preparation Axis of the taper is parallel to the long axis of the tooth
- For class 5 Axis of the taper is perpendicular to the long axis of the tooth.
Question 5. Hot spot porosity.
Answer:
Hot Spot Porosity:
- Hot Spot Porosity is localized shrinkage porosity
- Occurs due to shrinkage of molten alloy when alloy solidifies from a molten state
- Cause Sprue former directed at 90°
- Prevention Direct the sprue former at 45°
Question 6. Back pressure porosity.
Answer:
Back Pressure Porosity:
- This is caused by inadequate venting of the mold
- If the bulk of the investment is too great the escape of air becomes difficult causing increased pressure in the mold
- The gold will solidify before the mold is filled resulting in a porous casting with rounded short margins
- Avoided by
- Using adequate casting forces
- Use of investment of adequate porosity
- Place the pattern not more than 68 mm from the end of the ring
Question 7. Subsurface porosity.
Answer:
Subsurface Porosity:
- Subsurface Porosity is porosity caused by gas
Subsurface Porosity Cause:
- Simultaneous nucleation of solid grains and gas bubbles
Subsurface Porosity Prevention:
- Controlling the flow of molten alloy
Question 8. Electroformed dies.
Answer:
Electroformed Dies:
Subsurface Porosity Advantages:
- Dimensional accurate
- Hard, abrasion-resistant
- Imparts a smooth surface
- Cheap
- Better marginal definition
- Does not absorb oil or water
- Prevent cuspal wear
Subsurface Porosity Disadvantages:
- Difficult to trim
- Silver bath health hazard
- Noncompatible with impression material
- Color contrast is not good
- or adaptation to wax
- The pattern tends to lift from margins
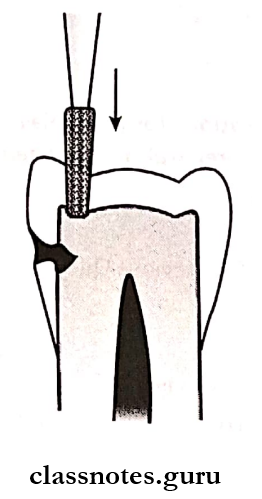
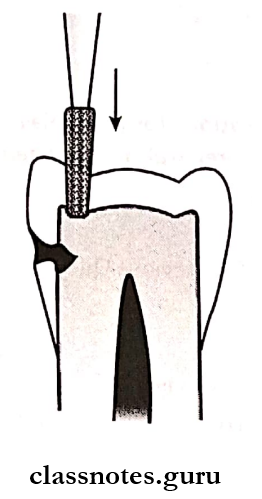
Question 9. Onlay.
Answer:
Onlay:
- Onlay It is a combination of intracoronal and extra-coronal cast restoration which covers one or more cusp
Tooth Preparation:
- Occlusal Outline Form:
- Isolate the tooth
- Start preparation with 271 bur
- Maintain a pulpal depth of 2 mm
- Reduce the cusps
- Occlusal divergence 3°-5°
Proximal Box Preparation:
- Extend the preparation both mesially and distally
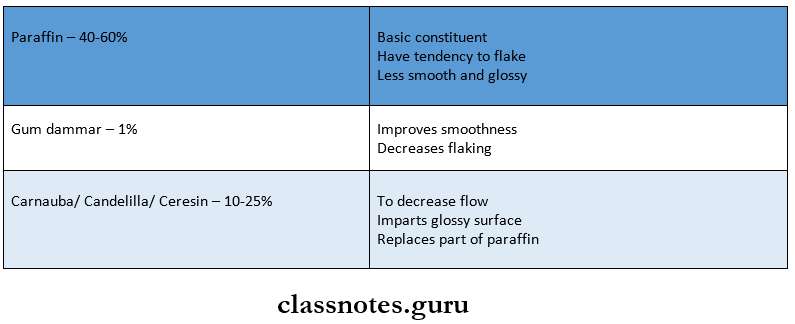
Question 10. Inlay Wax.
Answer:
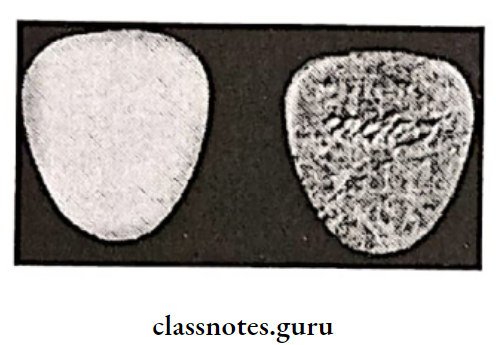
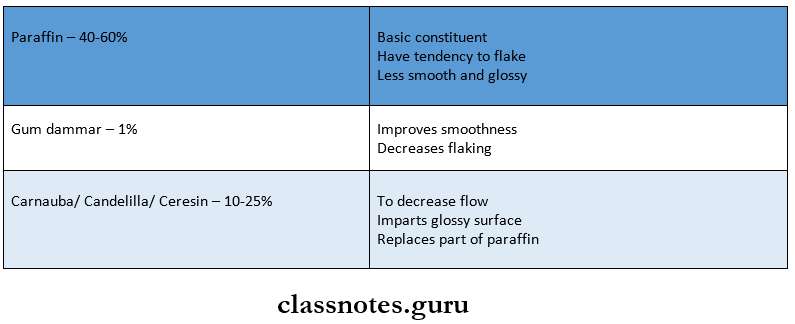
Inlay Wax:
Inlay Wax Properties:
- Plasticity
- Solid below approximately 40°C
Inlay Wax Types:
Inlay Wax Composition:
- Paraffin wax- 40 60%
- Ceresin -10%
- Gum dammar- 1%
- Carnauba- 25%
- Coloring agents
Question 11. Localized shrinkage porosity
Answer:
Localized Shrinkage Porosity:
- Occurs when cooling is incorrect
- The sprue freezes before the rest of the casting
- It results in large irregular voids near the sprue casting interface
Localized Shrinkage Porosity Prevention:
- Sprue former should be directed at 45 degrees
- Placement of reservoir
Cast Metal Restorations Viva Voce
- Sprue former diameter is between 8018 gauge
- Types of sprue former wax, metal, and resin
- Occlusal bevel in inlay3045°
- Gingival bevel in inlay 30°
- The sprue is placed at a 45° angle to the wax pattern
- Wax interocclusal records help check occlusal clearance
- Binder present in investment provides strength
- Casting ring liner helps in permitting the expansion of mold
- Sprue should be positioned in the thickest portion of the wax pattern
- There should be a minimum gap of 1/8 1/4th inch between the ends of the casting ring and wax pattern
- Back pressure porosity is caused by the entrapped air in the mold that does not escape through the pores of the investment
- Type 1 or type B wax is used for the direct technique of wax pattern construction
- Type C is used for indirect technique