NCERT Class 3 Maths Solutions Chapter 6 House Of Hundreds -1
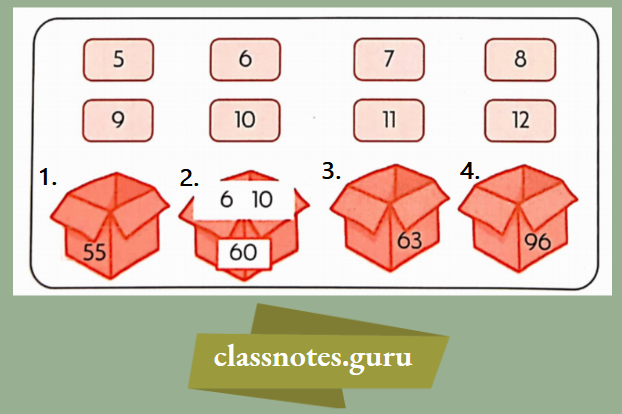
Question 1. Write how many packets of items are given, by using the packets of hundreds, tens, and loose items that are given below. One has been done for you.

Read and Learn More Class 3 Maths Mela Question and Answers
Answer:

NCERT Class 3 Maths Mela Chapter 6 House of Hundreds – I
Question 2. Calculate the sum in the following questions.
1. 200 + 29 =
Answer:
200 + 29 = 229
2. 150 + = 246
Answer:
150 + 96 = 246
3. 250 + 59 =
Answer:
250 + 59 = 309
4. 100 + 100 + 80 = 289
Answer:
100 + 100 + 80 + 9 = 289
5. 200 + 100 + 50 + 15
Answer:
200 + 100 + 50 + 15 = 345
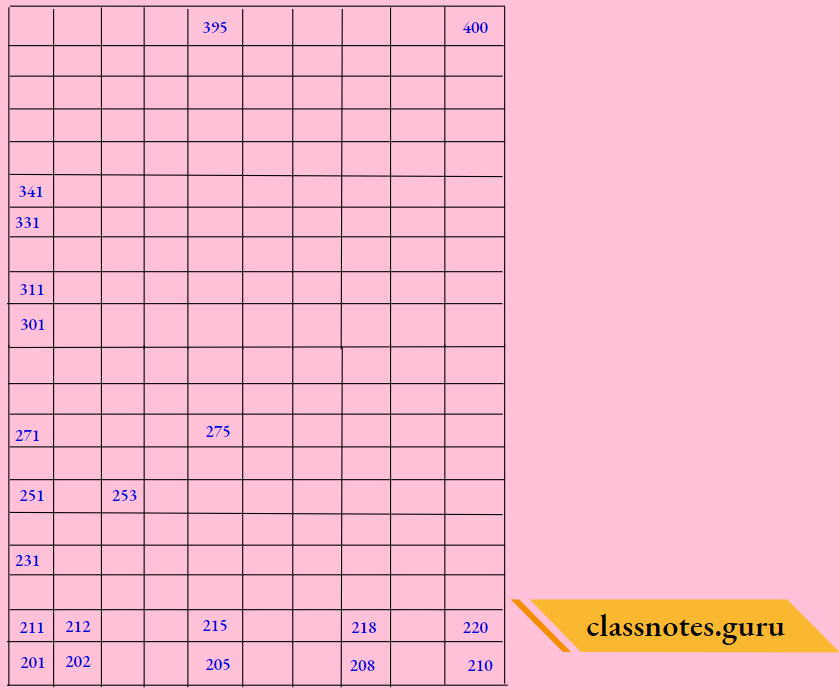
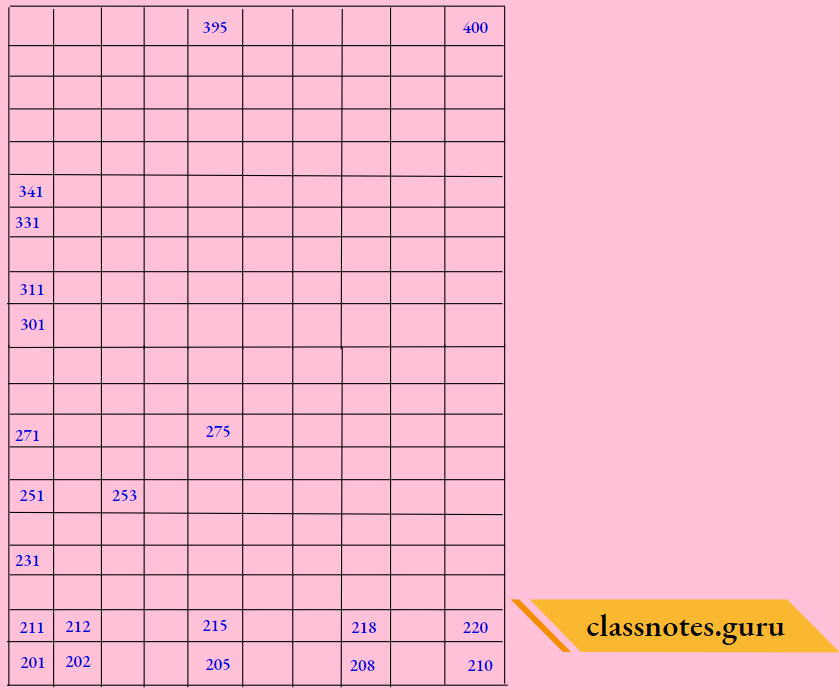
Question 3. Fill the missing numbers

Answer:

Question 4. Answer the following questions given below. One has been done for you
1. 210 decreased by 5, then the number is________
Answer: 205
2. ________ Added to 350 gives 375
Answer: 25
3. 200 increased by 28, then the number is ________
Answer: 228
NCERT Class 3 Maths Mela Chapter 6 House of Hundreds – I
4. 96 increased by ________, then the number is 246.
Answer: 150
5________ + .82 = 415
Answer: 333
Question 5. Fill In the blanks appropriately.

Answer:

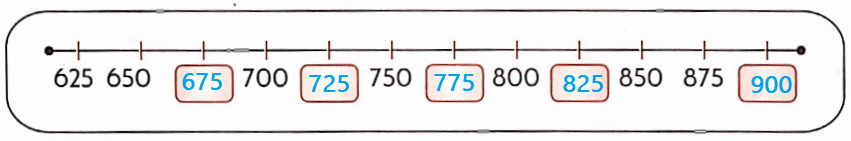
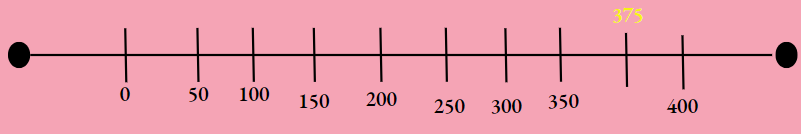
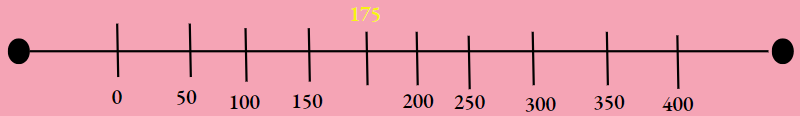
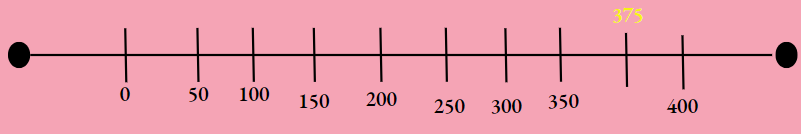
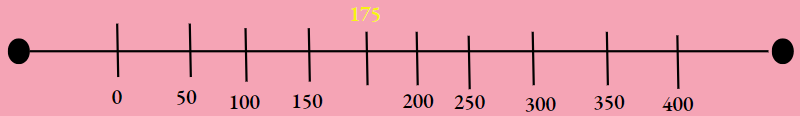
Question 6. Place the numbers on the number line. One has been done for you.
1. 225
Answer:

2. 275
Answer:

3. 325
Answer:

NCERT Class 3 Maths Chapter 6 House of Hundreds
4. 375
Answer:
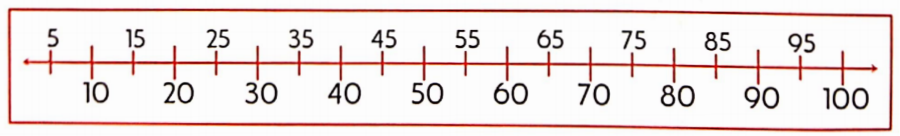
Question 7. Answer the following questions, which are based on the arrangement of numbers.
1. Find the number between 310 and 330
- 315
- 230
- 250
- 335
Answer: 315
2. 243 Is the number between _______ to 395.
- 315
- 230
- 280
- 365
Answer: 2. 230
3. 175 is the number between _____________ to _______ on the number line
Answer: 150 to 200
4. 375 is the number between ___________ to _________ on a number line
Answer: 350 to 400

Question 8. Match the following appropriately. One has been done for you.

Answer:

Maths Mela Class 3 Chapter 6 House of Hundreds – I
Question 9. Fill in the appropriate answer in the blank box. One has been done for you.

Answer:

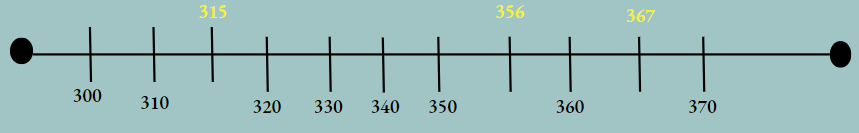
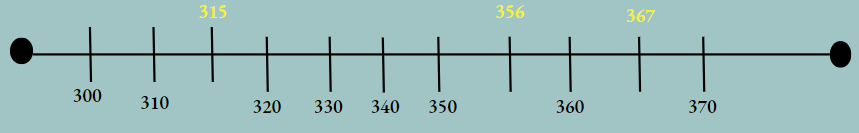
Question 10. Place the appropriate numbers on the number line.
1. Place the numbers 315, 356, and 367 on the number line.
Answer:
2. Place the numbers 255, 257, 268, 279, and 281 on the number line
Answer:

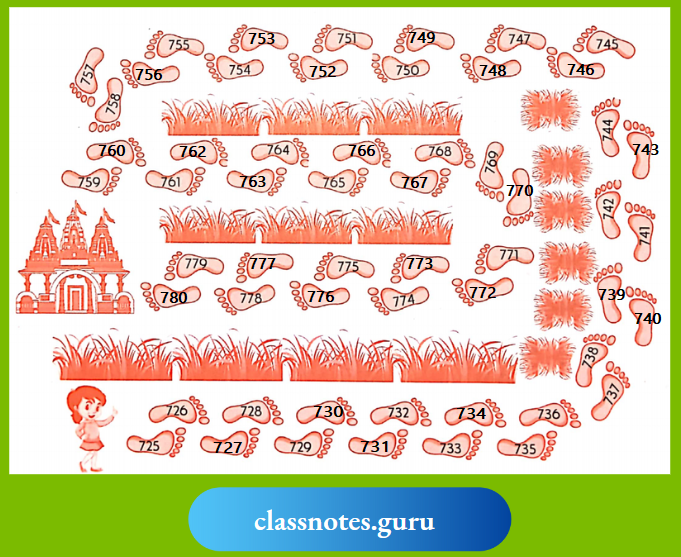
Question 11. Read the following story of jumping animals and answer the given questions.

Monkey, cat, and frog are jumping all the way. Monkey Jumps on every 2nd step, cat Jumps on every 3rd step and frog jumps every 4th step Monkey jumps 3 steps, cat Jumps 2 steps and frog Jumps 2 steps in one jump.
- Monkey starts jumping from step number 210.
- Cat starts jumping from step number 212.
- Frog starts jumping from step number 211.
1. Cat’s 4th jump will be on step number________________
Answer: 229
2. Frog’s 3rd jump will be on step number________________
Answer: 225
3. How many times should a frog jump to reach 231?________________
Answer: 4
Class 3 Maths Mela Chapter 6 House of Hundreds – I Solutions
Question 12. Ludo, Dholuo, Bholu, Sunno, and Golu collected candies from a box. Look at the following pictures and answer the questions given below

Answer:
1. ______________ collected the most number of candies.
Answer: Golu
2. Sunno needs to collect
Answer: 60
3. If Ludo gets 20 more candies, he will have ____________ candles.
Answer: 470
4. Dholuo has 5 candies less than 450 and_______________ has 15 candies more than 450.
Answer: Bholu
5. How many children have less than 450 candies
Answer: 2
Question 13. Geeta Aunty, a popular local florist, has several orders to deliver bouquets across the city. She has a map with various landmarks and houses marked on it. Your task is to help her by coloring the houses where she needs to deliver the flowers
Answer:
Answer:

NCERT Class 3 Maths Mela Chapter 6 House of Hundreds – I
Question 14. Rihanna lives in a 10-story building, in which some grids are coloured and some are not. On that basis, answer the following questions.
Answer:

Answer:

Answer:
1. Find the grid numbers which is grey in colour _______________
Answer: 409,418,427,436,445,454,463,472,481
2. The magenta grid numbers are _______________
Answer: 444,455,466,477,488,499
3. _______________ total coloured grid in a 10-story building.
Answer: 15
4. What pattern do you get, a magenta and grey grid?
Answer:
- Grey patter,2nd rowand 1st column, 3rd rowand 2nd column…10th row and 9th columns
- Magentalgrid pattern 4th columnand 6 th row,5th column and 5 ty row, 9th column and 1st row
Question 15. Mina Aunty loves baking cookies and packs them for her bakery shop. She uses small packets that hold 5 cookies each and packs these small packets into larger boxes that can hold 50 cookies each.
1. How many packets of 5 cookies can she fit in a box of 50? ________________
Answer: 10
2. How many packets of 5 cookies can she fit in two boxes of 50? ________________
Answer: 20
3. How many packets of 5 cookies can she fit in three boxes of 50? ________________
Answer: 30
4. How many packets of 5 cookies will she find if she opens one box of 50? ________________
Answer: 10
Question 16. Solve the following puzzles

Answer:

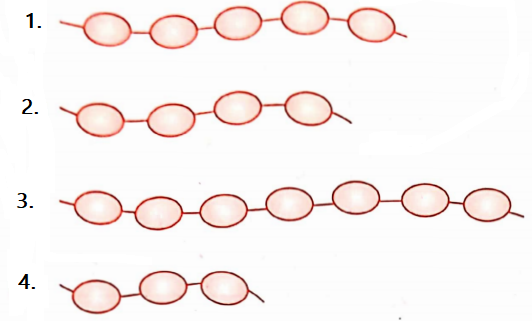
Question 17. Answer the following questions
1. Shikha has a necklace of 226 beads and Shradha has a necklace of 442 beads. Which one has more beads in her necklace?
Answer: Shraddha
2. Rahul has a collection of 368 comic books, while Sunita has 295 comic books. Who has less comic books in their collection?
Answer: Sunita
Question 18. Fill in the blanks with less than < or greater than > signs
Answer:
1. 203__________ 305
Answer: 203 < 305
2. 405_______ 303
Answer: 405 > 303
3. 3 hundred ______ 2 hundred
Answer: 300 > 200
4. 2 tens __________ 3 tens
Answer: 20 > 30
5. 8 ones _______ 2 ones
Answer: 8 > 2
Question 19. Denote the smallest number with the ___________ and the greatest number with _________
1. 274, 373, 247, 337
Answer: Smallest -247, Greatest -373
2. 249, 133, 331, 457
Answer: Smallest – 133, Greatest -457
3. 456, 447, 239, 147, 383
Answer: Smallest – 147, Greatest – 456
4. 364, 287, 223, 246, 548
Answer: Smallest -223, Greatest – 548
Question 20. Arrange the following numbers from Smallest to Biggest – 321,210,432,654,543
Answer:

Question 21. Arrange the following numbers from biggest to smallest – 68,377,295,250,496
Answer:

Question 22.
1. Make 3-digit numbers using 5, 1, and 9 without repeating any digits. Color the greatest number with blue and the smallest number with green.
Answer: 496,377,295,250,68
2. Create 3-digit numbers using 2, 3, and 4, where digits can be repeated. Colour the greatest number with purple and the smallest number with orange
Answer: 222, 223, 224, 232, 233, 234, 242, 243, 244, 322, 323, 324, 332, 333, 334, 342, 343, 344, 422, 423, 424, 432, 433, 434, 442, 443, 444