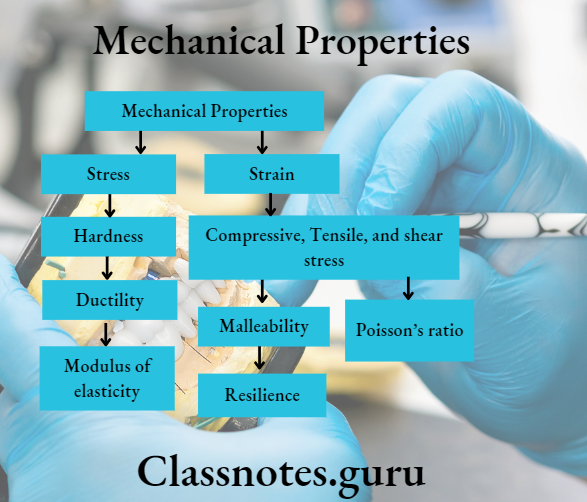
Mechanical Properties Important Notes
1. Stress
- Stress is force per unit area perpendicular to the force direction
- Stress Types:
- Tensile stress
- Shear stress
- Compressive stress
2. Strain
- Strain is the change in length per unit length of an object subjected to stress
- Strain Types:
- Elastic strain
- Plastic strain
Read And Learn More: Dental Materials Question and Answers
3. Hardness
- Hardness is resistance to abrasion and indentation
- Hardness tests
- Macro hardness test – Brinell and Rockwell
- Micro hardness tests – Knoop and Vickers test
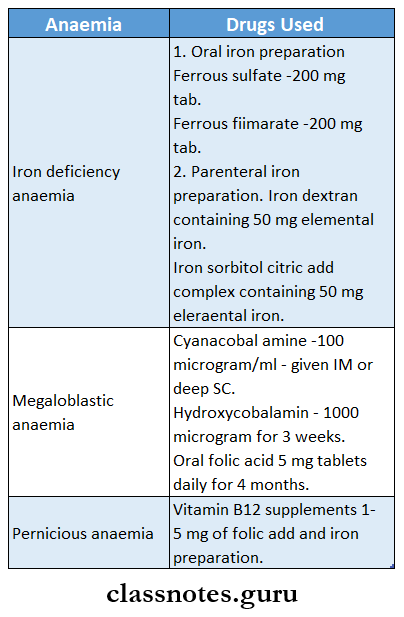
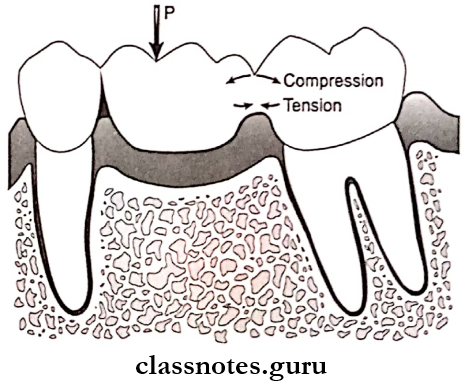
4. Compressive, Tensile, and Shear Stress
5. Ductility
- It is the ability of a metal to be drawn into wire under tensile load without rupture
- It can be measured by percent elongation and cold blend test
6. Malleability
It is the ability of a material to sustain permanent deformation without fracture under compression.
7. Modulus of elasticity
- The stress/ strain ratio within the proportional limit is called the elastic modulus or Young’s modulus
- It measures the relative rigidity or stiffness of the material
8. Resilience
- It is the amount of energy absorbed by a structure when it is stressed to the proportional limit
- The elastic area of the stress-strain graph gives resilience
- It is measured by R
- R= P2/2E
- R = resilience
- P = proportional limit
- E = modulus of elasticity
9. Proportional limit
- It is the maximum stress at which stress is proportional to strain and above which plastic deformation occurs
- It represents the maximum stress above which stress is no longer proportional to strain
10. Poisson’s ratio
Poisson’s ratio = Lateral strain/ Axial strain.
Mechanical Properties Of Dental Materials
Mechanical Properties Short Essays
Question 1. Define stress and strain. Name types of stresses and strains. How are these two properties important in the study of dental materials?
Answer:
Stress And Strain
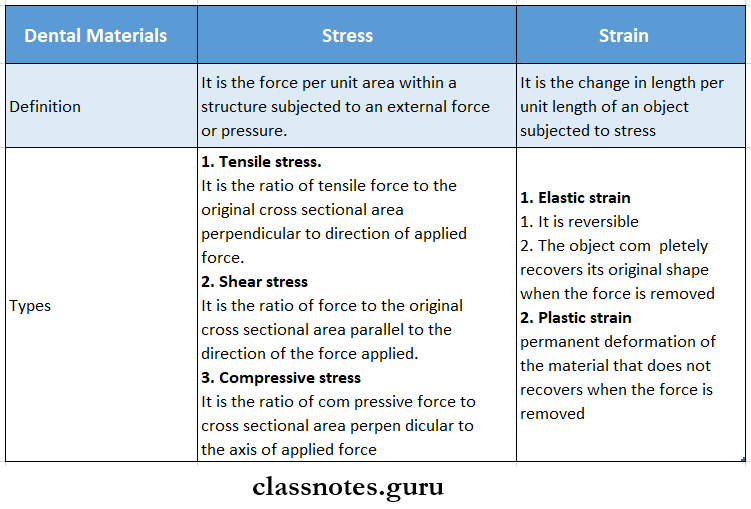
Importance Of Stress And Strain:
- Stress and strain are related to the force applied
- Stress is the displacing force in a given area while strain is the change in dimension
- In the oral cavity, many complex forces exist which tend to deform the material of the restorations
- Thus, it is important to know about the stress and strain of the material to interpret how the material will behave under the effect of such forces
Question 2. Stress and strain relation.
Answer:
Stress And Strain Relation
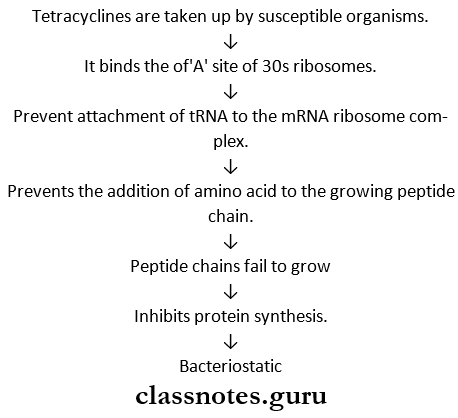
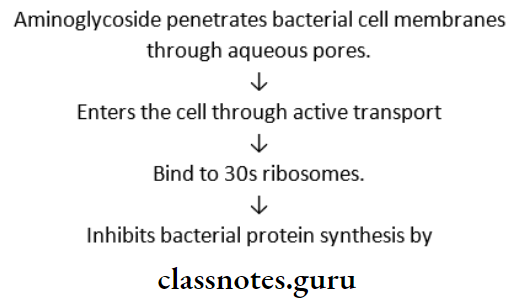
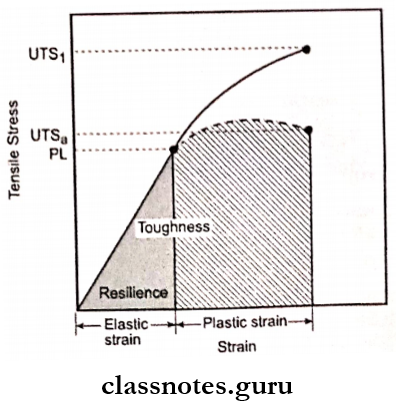
For each material, there is a stress-strain proportional relationship establishing a stress-strain curve
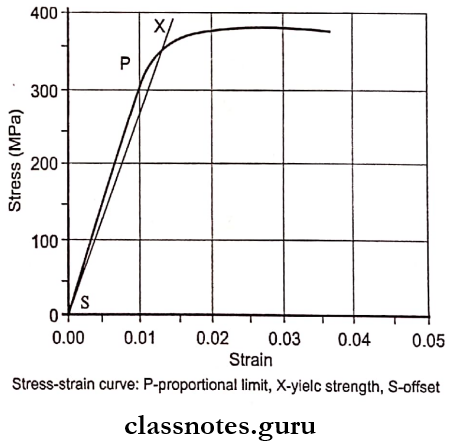
- As shown in a curve, stress is directly proportional to strain up to point P called the proportional limit, and elastic deformation occurs
- At this point, the object will withstand the forces applied without permanent deformation
- It determines the elasticity of a material
- When the applied load exceeds this point, irreversible deformation occurs resulting in plastic deformation
- After this point, stress is no longer proportional to strain
- The area under the elastic portion of the curve represents resilience
- This indicates the amount of energy required to deform the material to its proportional limit
- The area under the elastic and plastic portion of the curve indicates the toughness of a material.
Types Of Dental Materials And Their Properties
Question 3. Types of stresses
Answer:
Types of Stresses Are:
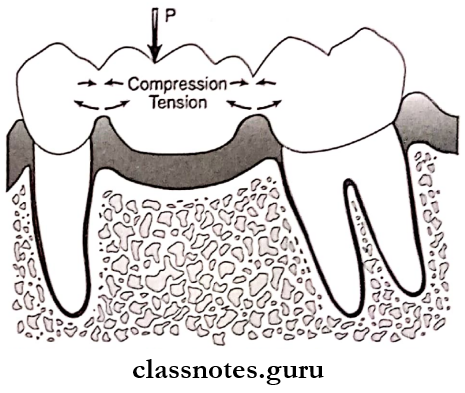
1. Tensile Stress:
Tensile Stress is the ratio of tensile force to the original cross-sectional area perpendicular to the direction of the applied force
Tensile Stress Direction Offered:
The two forces acting are directed away from each other in the same straight line
Tensile Stress Effect:
The load tends to stretch or elongate a body
2. Shear Stress:
Shear Stress is the ratio of force to the original cross-sectional area parallel to the direction of the force applied
Shear Stress Direction of Forces:
The two forces are directed parallel to each other
Shear Stress Effect:
Shear Stress resists sliding one portion of a body over another
3. Compressive Stress:
Compressive Stress is the ratio of compressive force to cross-sectional area perpendicular to the axis of applied force
Compressive Stress Direction of Forces:
The forces are directed toward each other in the same line
Compressive Stress Effect:
The load tends to shorten a body
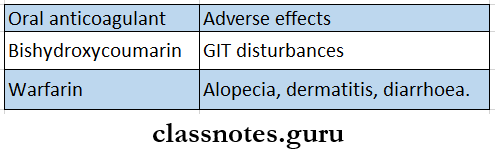
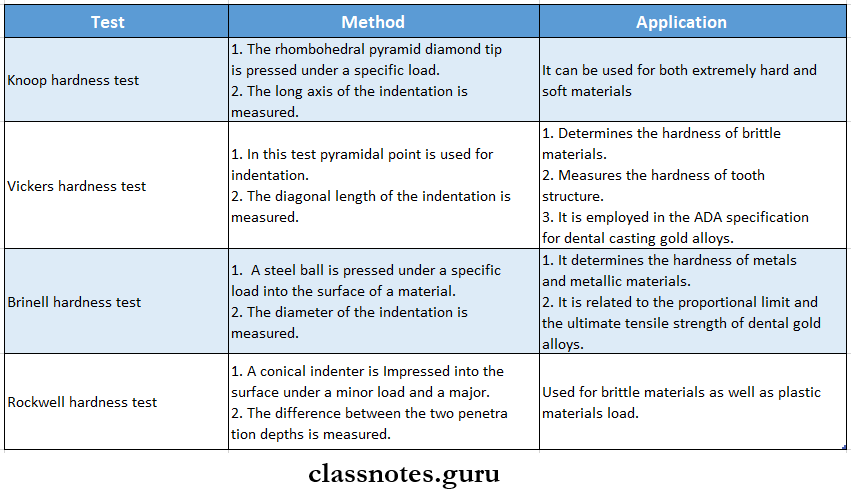
Question 4. Hardness (or) Hardness tests
Answer:
Hardness Definition:
Hardness is the resistance of a material to plastic deformation measured under an indentation load
Factors Affecting Hardness:
- The following factors influence the hardness of a material:
- Strength
- Proportional limit
- Ductility
- Malleability
Hardness Tests:
- Microhardness Tests:
- Knoop hardness test
- Vickers hardness test
- Macrohardness Tests:
- Brinell Hardness test
- Rockwell hardness test
Stress And Strain In Dental Materials
Question 5. Ductility and malleability
Answer:
1. Ductility Definition:
It is the ability of a material to withstand large permanent deformation under a tensile load before it fractures
Ductility Factors Affecting It
- Ductility is dependent on tensile strength
- Ductility decreases as the temperature raises
Ductility Measurements: Ductility is measured by three methods
- By measuring the percentage elongation after fracture
- It is a common method
- The initial length of the wire is measured before the fracture
- This is compared with that of an increase in length after fracture
- Measuring reduction in cross-sectional area of fractured ends
The percentage of decrease in the cross-sectional area of the fractured end is calculated and compared to that of the cross-sectional area before the fracture
- Cold bend test
- The material is clamped in a vise and bent around a mandrel of a specified radius
- The number of bends to fracture is counted
2. Malleability Definition:
Malleability is the ability of a material to sustain permanent deformation without fracture under compression
Malleability Importance: Metals according to their ductility and malleability are
- First is gold- It is the most ductile and malleable
- Second is silver
- Third in ductility is platinum and in malleability is copper
- The ductility is assessed by the stress-strain curve
- After fracture, the stress reduces to zero.
Mechanical Properties Short Question And Answers
Question 1. Name types of strength. Discuss the importance of strength in the study of dental materials
Answer:
Strength Definition:
Strength is the stress necessary to cause either fracture or a specified amount of plastic deformation.
Strength Types:
- Tensile Strength Or Ultimate Tensile Strength: It is the maximal stress the structure will withstand before the rupture
- Shear Strength: It is the maximal shear stress at the point of fracture of a test specimen
- Compressive Strength: It is the compressive stress within a compression test specimen at the point of fracture
- Flexural Strength: It is the force per unit area at the point of fracture of a test specimen subjected to flexural loading
- Impact Strength: It is the energy required to fracture a material under an impact force
Importance Of Strength:
- Strength describes the types of deformation that can occur
- It measures the interatomic forces over the stressed structure
- Shear strength is used to study the interface between two materials
- Transverse strength is used to test denture base resins and long-span bridges
Question 2. Modulus of elasticity
Answer:
Modulus Of Elasticity Synonyms:
- Young’s modulus
- Elastic modulus
Modulus Of Elasticity Definition:
Modulus Of Elasticity is the relative stiffness or rigidity of material within the elastic range.
Modulus Of Elasticity Measurement:
- It is the ratio of stress to strain and is described as E.
- E= Stress / Strain
Modulus Of Elasticity Importance:
- It indicates that the less the strain, the greater will be the stiffness
- Elastic modulus has a constant value
- It is not affected by the amount of plastic and elastic stress that is induced in the material
- It is independent of the ductility of the material
- By determining Young’s modulus of enamel and dentin, it describes that
- Enamel is stiffer and more brittle
- Dentin is more flexible and tougher
Modulus Of Elasticity Unit:
Ciiganewtons per square meter ( GN/ m²)
Elasticity Of Dental Materials
Question 3. Proportional limit
Answer:
Proportional Limit Definition:
Proportional Limit is the maximum stress at which stress is proportional to strain and above which plastic deformation occurs
Proportional Limit Importance:
- The proportional Limit is the greatest elastic stress possible in accordance with Hooke’s law
- Proportional Limit represents the maximum stress above which stress is no longer proportional to strain
Question 4. Resilience
Answer:
Resilience Definition: Resilience is a relative amount of elastic energy’ absorbed within a unit volume of a structure when it is stressed to its proportional limit.
Resilience Measurement: It is measured in terms of the modulus of resilience, R.
- R = P2/2E where,
- R- Modulus of resilience
- P- Proportional limit
- E- Modulus of elasticity
- Resilience can be illustrated by the stress-strain curve
- The area bounded by the elastic region is a measure of resilience
Question 5. Elastic limit
Answer:
Elastic Limit Definition:
Elastic Limit is defined as the greatest stress to which a material can be subjected such that it returns to its original dimensions when the force is released
Elastic Limit Importance:
- Elastic Limit describes the elastic behavior of the material
- Elastic Limit can measure any type of stress
Mechanical Testing Of Dental Materials
Question 6. Poisson’s Ratio
Answer:
Poisson’s Ratio
- When a tensile force is applied along one axis to produce elongation, compressive strain is produced at right angles proportionately.
- It is related to the nature and symmetry of the interatomic bonding forces
- For an ideal isotropic material of constant volume, the ratio is 0.5
- Poisson’s ratio = Lateral strain / Axial strain
Question 6. Strain hardening
Answer:
Strain Hardening Synonyms:
- Cold working
- Work hardening
Strain Hardening Features:
- The process of plastically deforming a metal usually at room temperature is called cold-working
- When a metal is stressed beyond its proportional limit, the hardness, and strength of the metal increase but the ductility decreases
- Repeated plastic deformation of the metal leads to the brittleness of the wire and it will fracture
- In the stress-strain curve, as the elastic modulus remains constant, the plastic deformation part of the curve would be decreased.
Question 7. Define: Elasticity and stiffness
Answer:
Elasticity: Elasticity is the tendency of solid materials to return to their original shape after being deformed.
Stiffness:
- Stiffness is the ratio of the force required to create a specified deflection
- Stiffness is the ability of a material to resist bending or stretching
- A stiff material has a high Young’s modulus.
Question 8. Yield strength
Answer:
Yield Strength
- Yield Strength is the stress at which a test specimen exhibits a specific amount of plastic strain.
- Yield strength is greater than the proportional limit
- If it exceeds the masticatory stresses, the restorations may not function any longer.
Question 9. Toughness
Answer:
Toughness
- Toughness is the ability of a material to absorb elastic energy and to deform plastically before fracture
- Toughness increases with increases in strength and ductility
- The greater the strength and the higher the ductility, the greater the toughness
- Tough material is generally strong.
Compressive Strength Of Dental Materials
Question 10. Ductility and malleability
Answer:
Ductility:
- Ductility is the ability of a material to withstand large permanent deformation under a tensile load before it fractures
- Factors affecting it are:
- It is dependent on tensile strength
- It decreases as the temperature raises
Malleability:
Malleability is the ability of a material to sustain permanent deformation without fracture under compression.