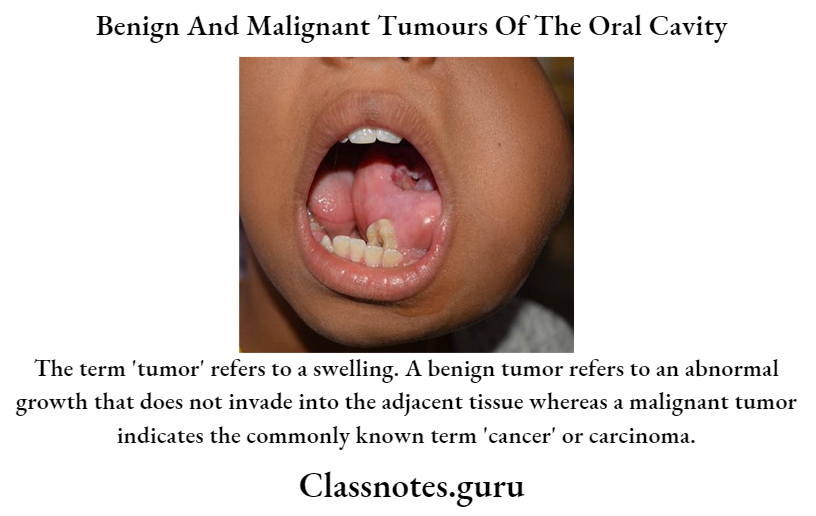
Benign And Malignant Tumours Of The Oral Cavity Important Notes
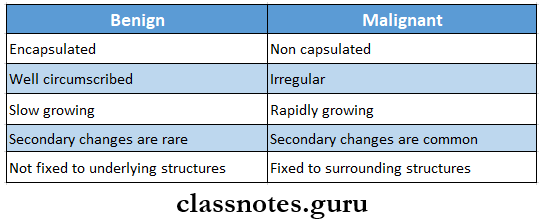
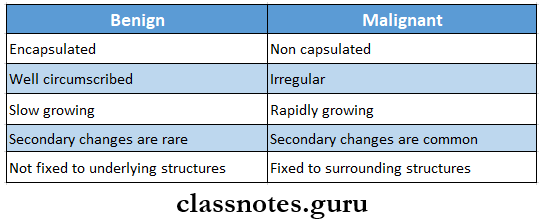
- Differences Between Benign And malignant Neoplasm
- Premalignant Conditions
- Premalignant Conditions is defined as a generalized state or condition associated with a significantly increased risk for cancer development
- Oral submucous fibrosis
- Syphilis
- Sideropenic dysplasia
- Dyskeratosis congenital
- Lupus erthymetosis
- Features of Epithelial Dysplasia
- Loss of polarity of basal cells
- The presence of more than one layer of cells having the basaloid appearance
- Increased nuclear-cytoplasmic ratio
- Drop-shaped rete pegs
- Irregular epithelial stratification
- Increased number of mitotic figures
- Cellular pleomorphism
- Nuclear hyperchromatism
- Enlarged nucleoli
- Reduced cellular cohesion
- Keratinization of single cells or cell groups in the prickle layer
- Leukoplakia
- Leukoplakia is a whitish patch or plaque that cannot be characterized, clinically or pathologically, as any other disease and which is not associated with any other physical or chemical causative agent except the use of tobacco.
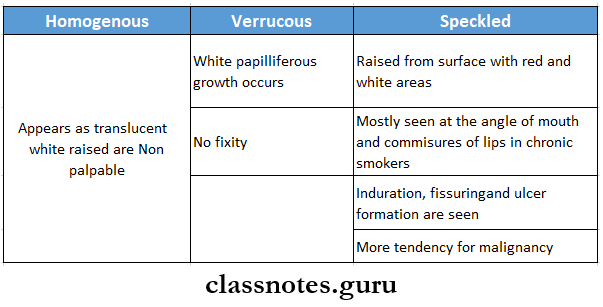
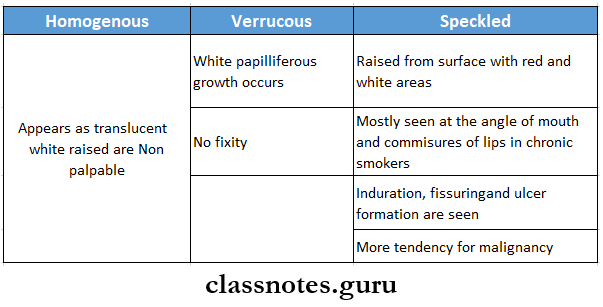
- Types:
- Reduction of basement membrane
- Chronic cell infiltration in connective tissue
- Oral submucous Fibrosis
- An insidious chronic disease affecting any part of the oral cavity and sometimes the pharynx.
- Although occasionally preceded by and /or associated with vesicle formation, it is always associated with juxta epithelial inflammation reaction followed by fibroelastic changes of lamina propria with epithelial atrophy leading to stiffness of oral mucosa and causing trismus and inability to eat
- Histopathological features
- Epithelial atrophy
- Loss of rete pegs – shortening or flattening of recipes
- Epithelial atypia
- Hyalinization of connective tissue
- Classification Of Lymphangioma By Watson And Mccarthy
- Simple Lymphangioma
- Cavernous Lymphangioma
- Cellular/ hypertrophic Lymphangioma
- Diffuse systemic Lymphangioma
- Cystic Lymphangioma or hygroma
- Types Of Kaposi Sarcoma
- Classic variant – associated with altered immune state
- Lymphadenopathic – endemic to young African children
- Transplantation associated – seen in 1-4% of renal transplant patients
- AIDS-related – 40% of homosexual AIDS patients develop it.
- Codman’s Triangle
- Seen in osteosarcoma
- In the long bones affected, the periosteum is elevated over expanding tumor mass in a tent-like fashion
- At the point on the bone where the periosteum begins to merge, an acute angle between the bone surface and the periosteum is created
- This is called Codman’s triangle
- Grinspan syndrome – Consists Of:
- Diabetes mellitus
- Lichen planus
- Hypertension
- Multiple Myeloma
- Dysplastic features in multiple myeloma are:
- Increased abnormal mitoses
- Individual cell keratinization
- Epithelial pearls in the spinous layer
- Alterations in nuclear-cytoplasmic ratio
- Loss of polarity and disorientation of cells
- Hyperchromatism
- Large nucleoli
- Nuclear atypia including giant nuclei
- Division of nuclei without division of cytoplasm
- Radiographic Features Of Osteosarcoma
- Osteolytic type
- Osteosarcoma presents as a large, irregular radiolucent area with a moth-eaten appearance
- Osteoblastic type
- There is the deposition of new bone on the surface in a radiating fashion producing sun ray appearance
- Actinic Cheilitis
- Causes: ultraviolet light
- The lower lip shows epithelial atrophy and focal keratosis
- The upper lip is minimally affected because it is protected from UV light
- The junction of vermillion and skin becomes indistinct
- May progress to squamous cell carcinoma
- Verrucous Carcinoma
- A well-differentiated and slow-growing form of carcinoma
- Etiology: Tobacco and human papillomavirus are the main etiological factors
- Exhibits a broad-based verruciform architecture
- Treated by surgical excision
- Have a good prognosis.
Benign And Malignant Tumours Of The Oral Cavity Long Essays
Question 1. Mention non-odontogenic malignant tumors of epithelial tissue of oral mucosa. Describe clinical and histopathological features of verrucous carcinoma.
Answer:
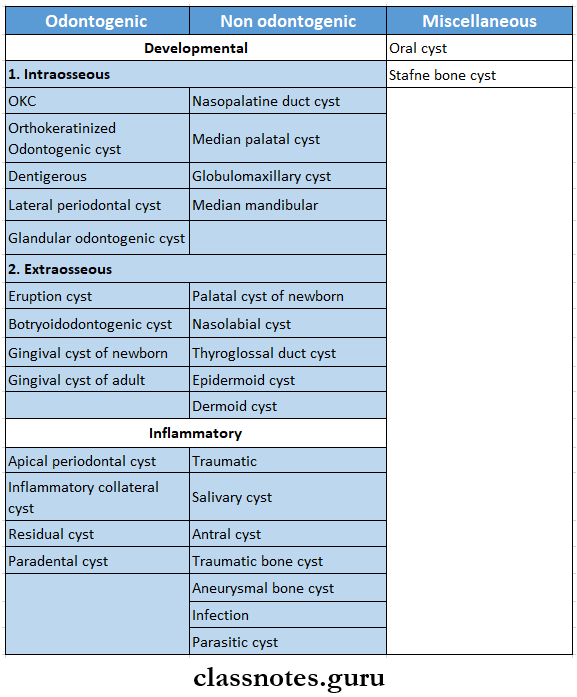
Non-Odontogenic Malignant Tumours Of Epithelial Tissue:
- Basal cell carcinoma
- Squamous cell carcinoma
- Verrucous carcinoma
- Spindle cell carcinoma
- Adenoid squamous cell carcinoma
- Basaloid squamous cell carcinoma
- Lymphoepithelioma
- Nasopharyngeal carcinoma
- Malignant melanoma
Verrucous Carcinoma:
Verrucous Carcinoma is diffused papillary, non-metastasizing well-differentiated malignant neoplasm of oral epithelium
Read And Learn More: Oral Pathology Questions and Answers
Verrucous Carcinoma Clinical Features:
- Age- 50-80 years
- Sex- commonly affects males
- Site Involved
- Buccal mucosa
- Gingiva
- Alveolar mucosa
- Hard palate
- The floor of the mouth
- Present as slow enlarging, soft, exophytic neoplasm
- Consist of closely packed, papillary growth of keratinized epithelium
- Surface
- Raised and plebby
- Warty
- Consist of multiple range-like folds with deep clefts
- Fully developed lesion
- An exophytic, greyish-red, bulky lesion with a rough mating surface
- Resembles papilloma
- Can occur in association with other lesions
- Lesions of buccal mucosa
- Extensive lesion
- Cause pain, tenderness
- Difficulty in taking food
- Lesion of gingiva and alveolar mucosa
- Fixed to the underlying periosteum
- Gradual invasion
- Destruction of jaw bone
- Enlarged and tender lymphadenopathy
Verrucous Carcinoma Histopathology:
- Epithelium
- Hyperplastic
- Covered by a thick layer of parakeratin
- The surface contains broad processes of well-differentiated squamous cells resembling church spires
- Epithelial Cells
- Well-differentiated
- Mitotic activity is less or absent
- Have basilar or parabasal hyperchromatism
- Spread laterally
- Exhibit severe dysplastic changes
- Rete Ridges
- Massively enlarged
- Bulb-like acanthotic
- In vaginates into underlying connective tissue at more or less the same level
- This is known as pushing margins
- Cleft-like spaces formed by it are lined by her tain called parakeratin plugging
- Basement Membrane
- The basement membrane is intact
- Connective Tissue
- Shows chronic cell infiltration
Question 2. Describe clinical features, histopathology,y and radiographic features of central ossifying fibroma
Answer:
Central Ossifying Fibroma: Central ossifying fibroma represents well-demarcated, encapsulated, expansible, central jaw lesion
Central Ossifying Fibroma Clinical Features:
- Age- commonly occurs in children and young adults
- Sex- common in females
- Site- common in the mandible
- Characterised by localized, painless, non-tendered, bony hard swelling in the jaw
- Maybe a single or multiple
- Central Ossifying Fibromais slow growing fibroma
- Expansion and distortion of cortical bones occurs
- Displacement of regional teeth results
- Fast growing lesion produces massive swelling called aggressive ossifying fibroma
Central Ossifying Fibroma Histopathology:
- Consist of delicate collagen fiber arranged in a whorled pattern
- Its veil is demarcated by a thin zone of the fibrous capsule
- There is the presence of numerous blood capillaries
- Initially
- There are multiple small foci of osteoid trabeculae
- Osteoids are poorly calcified
- Later
- Osteoid trabeculae fuse
- They form large irregular calcified masses
- The lesion also contains basophilic spherules with peripheral brush borders
Central Ossifying Fibroma Radiographic Features:
- Well-defined, unilocular or multilocular radiolucent area
- Has well-demarcated border
- Expansion of cortical bones
- Downward bowing expansion of the lower border of the mandible is seen
- Lesion extending between roots of teeth causes root divergence
- In the mature stage, large radiopaque areas lined by radiolucent rims are present
Question 3. Enumerate precancerous lesions, Write In detail about the etiology, dental features, and histopathology of erythroplakia.
Answer:
Precancerous Lesions:
- Precancerous Lesions is defined as morphologically altered tissue in which cancer is more likely to occur than its normal counterparts
- Precancerous Lesions For example,
- Leukoplakia
- Erythroplakia
- Mucosal changes associated with smoking habits
- Carcinoma in situ
- Bowen’s disease
- Actinic keratosis
Erythroplakia:
Erythroplakia is a red patch or plaque in the oral mucosa which cannot be characterized clinically or pathologically as any other condition and which has no apparent cause
Precancerous Lesions Etiology:
- Use of tobacco
- Alcohol
- Candida infection
- Idiopathic
Precancerous Lesions Clinical Features:
- Age: a fifth-seventh decade of life
- Sex: both sexes are equally affected
- Site
- The floor of the mouth
- Reiromolar area
- Buccal mucosa
- Gingiva
- Tongue
- Soft palate
- It appears as a small or extensive red lesion
- It has well-defined borders
Precancerous Lesions Types:
- Homogeneous
- Has uniform red patches all over
- Erythroplakia with interspersed patches of leukoplakia
- Has a few white leukoplakic patches along with a red patch
- Speckled leukoplakia
- Precancerous Lesions is characterized by the presence of soft irregular, raised, erythematous areas with a granular surface
Precancerous Lesions Histopathology:
- The epithelium shows a lack of keratinization
- Precancerous Lesions may be atrophic or hyperplastic
- There is an increase in the vascularity of submucosal connective tissue
- The underlying connective tissue shows chronic inflammatory cell infiltration
Question 4. Classify white lesions. Discuss in detail leukoplakia
Answer:
White Lesions Classification:
- Variation In Structure And Appearance Of Normal Mucosa
- Leukoedema
- Fordyce granules
- Linea alba
- White Lesion With Precancerous potential
- Leukoplakia
- Erythroplakia
- Lupus erythematosus
- Carcinoma in situ
- Lichen planus
- White Lesion without precancerous potential
- Traumatic lesions
- Focal epithelial dysplasia
- White sponge nevus
- Stomatitis nicotine
- Hairy leukoplakia
- Nonkeratotic Lesion
- White hairy tongue
- Burns
- Pemphigus
- Desquamative gingivitis
- Candidiasis
- Koplik’s spots
Leukoplakia Definition:
- It is a whitish patch or plaque that cannot be characterized, clinically or pathologically, as any other disease and which is not associated with any other physical or chemical causative agent except the use of tobacco.
Leukoplakia Etiology:
- Tobacco
- Smokeless tobacco
- Smoking tobacco
- Alcohol
- Chronic irritation
- Candidiasis
- Galvanism
- Vitamin deficiency
- Xerostomia
- Nutritional deficiency
- Hormones: sex hormones
- Drugs: Anticholinergic, antimetabolic
- Virus: herpes simplex and HIV
- Idiopathic
Leukoplakia Clinical Features:
- Age and sex: in older age males it occurs commonly i.e in the age of 35-45 years
- Sites
- Buccal mucosa
- Commissures
- Lip
- Tongue
- Oral leukoplakia often represents solitary or multiple white patches
- They can be nonpalpable, faintly, translucent, white areas over the mucosa
- Many lesions can be thick, fissured, indurated, or, papillomatous
- The size of the lesion varies from a small wall localized patch measuring about a few mm in diameter to diffuse large lesions, covering a wide mucosal surface
- The surface of the lesion is smooth or finely wrinkled or even rough on palpation.
- Color white or grayish or yellowish whiter in color in some cases, due to the heavy use of tobacco, they may take a brownish-yellow color,
- Some lesions may exhibit a pumice-like surface which waits due to the preserve of multiple discrete keratehestrlae on the surface of these lesions
- Leukoplakia of the floor of the mouth sometimes has an ebbing tide pattern of appearance
- The thickness of the patch may vary from one faint to considerably thick
- In roost of cases, these lesions are asymptomatic, however, in some cases, they may cause pain, a feel- hag of thickness and a burning sensation, etc
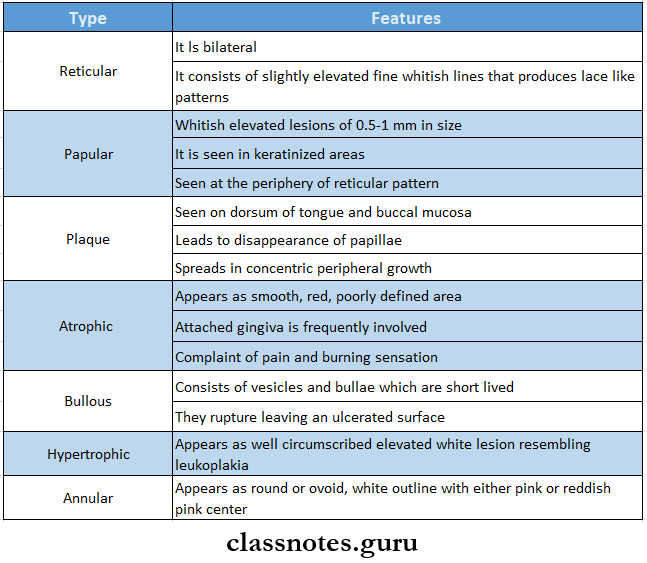
Leukoplakia Types
- Homogenous leukoplakia
- Ulcerative leukoplakia
- Nodular or speckled leukoplakia
Leukoplakia Histopathological Features
- Changes in Epithelium
- Hyper ortho keratinization or hyper para keratinization of the epithelium
- Epithelial dysplasia
- Acanthosis of epithelium is present
- Cellular Change
- Nuclear hyperchromatism
- Cellular pleomorphism
- Irregular epithelial stratification
- Increased nuclear-cytoplasmic ratio
- Poikilocytosis
- Loss of polarity of basal cells
- Increased number of mitotic figures
- Individual cell keratinization
- Dyskeratosis
- Absence of intercellular adhesions
- Enlarged nucleoli
- Drop-shaped rote pegs
- Basement Membrane
- Gradual reduction of basement membrane
- Connective Tissue
- Destruction of collagen fibers
- Presence of chronic cell infiltration
Leukoplakia Management:
- Elimination of etiological factor
- Conservative treatment
- Vitamin therapy:
- Lingual tablets and oral sprays may be used against glossitis and glossodynia
Leukoplakia Estrogen:
- Surgical management:
- Conventional surgery
- Cryosurgery
- Fulguration
Leukoplakia Laser: Radiation therapy is only used in neoplastic tissues
Chemotherapeutic Agents: Bleomycin and human fibroblast interferon are used
Question 5. Write about giant cell lesions of the oral cavity. Describe central giant cell granuloma
Answer:
Giant Cell Lesions Of Oral Cavity:
- Neoplasm
- Giant cell tumor of bone
- Central and peripheral giant cell granuloma
- Giant cell epulis
- Giant cell tumor of hyperthyroidism
- Giant cell fibroma
- Malignant fibrous histiocvtoma
- Other Lesions
- Osteoblastoma
- Chondroblastoma
- Fibrous dysplasia
- Hodgkin’s disease
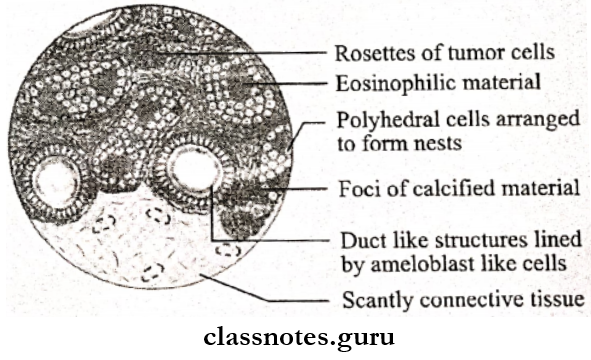
- CEOT
- Sarcoidosis
Central Giant Cell Granuloma: It is a common benign intraosseous destructive giant cell lesion of the oral cavity
Central Giant Cell Granuloma Clinical Features:
- Age- below 30 years of age
- Sex- common in females
- Site
- Body of mandible in anterior to first molar area
- In tooth-bearing jaws
- Palate
- Mandibular condylar- area
- Present as small, slow enlarging and bony hard swelling of the jaw
- Produces pain and paraesthesia of the jaw
- Expansion and distortion of buccal and lingual cortical plates
- The lesion may protrude outside the jawbone as a flat-base, dome-shaped, soft, purplish nodule over the alveolar ridge
- Loosening and displacement of teeth occurs
- Ulceration of surface epithelium
- Involved teeth are vital
Central Giant Cell Granuloma Radiographic Features:
- Lesion produces a well-delineated, multi-locular radiolucent area in the jaw producing a soap-bubble appearance
- Margin is scalloping and well-demarcated
- Some lesions are unilocular and produce drop-shaped radiolucency in the jaw
- Expansion and distortion of cortical bones
- Displacement of teeth
Central Giant Cell Granuloma Histopathological Features:
- Presence of lobulated mass of fibrovascular tissue
- Cells present are
- Giant cells
- Found around blood capillaries
- Contains 5-20 nuclei
- Dispersed throughout fibrous tissue stroma
- Stroma cells
- Plump and spindle-shaped
- Exhibit frequent mitosis
- Hemosiderin pigments are present
- Presence of chronic cell infiltration in connective tissue stroma
Question 6. Describe the clinical features and histopathology of epidermoid carcinoma of the oral cavity
(or)
Enumerate malignant nonodontogenic tumors of epithelial origin. Write in detail about the most common malignant neoplasm of the oral cavity
(or)
Describe the etiology, clinical features, and histopathology of oral squamous cell carcinoma
Answer:
Malignant Nonodontogenic Tumours of Oral Cavity:
- Basal cell carcinoma
- Squamous cell carcinoma
- Verrucous carcinoma
- Spindle cell carcinoma
- Adenoid squamous cell carcinoma
- Basaloid squamous cell carcinoma
- Lymphoepithelioma
- Nasopharyngeal carcinoma
- Malignant melanoma
Squamous Cell Carcinoma/Epidermoid Carcinoma:
Epidermoid Carcinoma is the most common malignant epithelial tissue neoplasm of the oral cavity derived from stratified squamous epithelium
Epidermoid Carcinoma Etiology:
- Tobacco
- Alcohol
- Nutritional deficiency
- Chronic irritation
- Radiation
- Viral infection
- Immunosuppression
- Chronic infections
- Genetic factors
- Pre-existing oral diseases
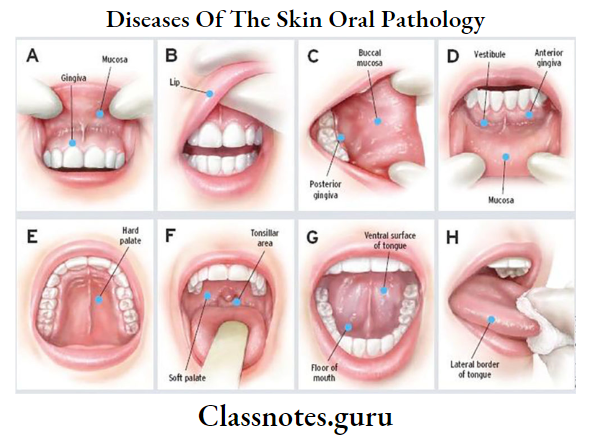
Epidermoid Carcinoma Clinical Features:
- Age and sex: it is common in older men
- Sites: sites involved in their order are
- Lower lip
- Lateral tongue
- The floor of the mouth
- Soft palate
- Gingiva
- Alveolar ridge
- Buccal mucosa
- Initially, it is an asymptomatic lesion
- Epidermoid Carcinoma may resemble leukoplakia or erythroplakia
- Epidermoid Carcinoma appears as a white or red nodule or fissure over the mucosa
- The advanced lesappeareara s is a rapidly enlarging exophytic growth or ulcer or tumor-like mass
- The ulcer has persistent induration around the periphery with elevated and everted margins
- Epidermoid Carcinomamay predispose to candidal infections
- Epidermoid Carcinoma may be secondarily infected
- There is a presence of regional lymphadenopathy
- Pathological fractures of jawbones may sometimes occur
- Maxillary lesions may lead to nasal bleeding and pressure sensation over the eyeball
- Involvement of the inferior alveolar nerve leads to paraesthesia of lower teeth and lip
- Excessive salivation
- Hoarseness of voice
- Foetor oris
- Sore throat
- Immobility of tongue
- Dysphagia
- Presence of extraoral discharging sinuses
Histopathological Features:
- It exhibits excessive proliferation of malignant squamous epithelial cells
- Cellular changes are
- Abnormal mitosis
- Cellular pleomorphism
- Nuclear hyperchromatism
- Increased nuclear-cytoplasmic ratio
- Individual cell keratinization
- Loss of polarity of the cell
- They invade underlying connective tissue by destroying the basement membrane
- Connective tissue consists of chronic cell infiltration, especially lymphocytes and plasma cells
- Based on histological features squamous cell carcinoma is graded into
- Well-differentiated squamous cell carcinoma
- Moderately differentiated squamous cell carcinoma
- Poorly differentiated squamous cell carcinoma
Question 7. Describe the clinical features and radiological features of osteosarcoma and write in detail about histological variants of osteosarcoma.
Answer:
Osteosarcoma Clinical Features
- Can occur in any bone
- Common sites
- Long bones – femur, tibia, humerus
- Skull, pelvis
- Sex/age
- Higher incidence in males
- Common in age between 10-25 years
- Pain and swelling of the involved bone
- Patients may complain of sprain or arthritis
- In extremity, pain may result in limp
- Regional lymphadenopathy is unusual
Osteosarcoma Oral Manifestations
- Pain and swelling of the involved area
- Causes facial deformity
- Loose teeth, toothache
- Paraesthesia
- Bleeding, nasal obstruction
Osteosarcoma Radiological Features Types:
- Osteolytic type
- Osteosarcoma presents as a large, irregular radiolucent area with a moth-eaten appearance
- Osteoblastic type
- There is the deposition of new bone on the surface in a radiating fashion producing sun ray appearance
Osteosarcoma Features
- Small streaks of bone radiating outwards produce a sunray pattern
- Tumors growing with periodontal membrane space cause resorption of bone and widening of periodontal space
- In long bones, the periosteum is elevated over expanding tumor mass in a tent-like fashion
- At the point of bone where the periosteum begin to merge, an acute angle between the bone surface and periosteum is formed
- This is called Codman’s triangle
Histopathological Variant
- Osteoblastic type
- Contains atypical neoplastic osteoblasts of varying size and shape
- Arranged in a disorderly fashion
- Fibroblastic type
- Shows varying degrees of proliferation of anaplastic fibroblasts
- ChondmhJaslic type
- Shows aims of neoplastic myxomatous list end cartilage
Benign And Malignant Tumours Of The Oral Cavity Short Essays
Question 1. Tori
Answer:
Tori
- Tori is an exostosis or outgrowth of hone
- Tori consists primarily of compact bone
Tori Site:
- In maxilla- in the midline of the palate
- In mandible- in premolar region on lingual aspect
Tori Features:
- Seen In middle-aged patients
- Tori may occur singly, multiply, unilateral, or bilateral
- Large torus filling the palatal vault
- Ulceration of overlying mucosa
- Deep undercuts
- Interference In functions
- Psychological disturbances
- Food lodgement
Tori Radiographic Features:
- Margins are sharply demarcated anteriorly and less dense and less well defined posteriorly
- Shape-oval in posteroanterior direction
- Tori represents radiopaque, homogenous, knobby protuberances
Question 2. Leukoedema
Answer:
Leukoedema
Leukoedema is an alteration of the oral epithelium characterized by Intra-cellular accumulation of fluid within the spiral cell layer
Leukoedema Clinical Features:
- Age- around 45 years
- Asymptomatic condition
- Mucosa exhibits diffuse, translucent, greyish-while area with a filmy appearance
- Site Involved
- Buccal mucosa near occlusal plane
- The lateral border of the tongue
- The inner surface of the lips
- Affected mucosa may be wrinkled or corrugated
- When stretched the lesion disappears
Leukoedema Histopathological Features:
- Characterized by the thickening of epithelium with parakeratosis and acanthosis
- The spinus cell layer consists of a large amount of intricacy- cytoplasmic fluid and glycogen
- Spinus cells are enlarged with pyknotic nuclei and clear cytoplasm
- Rete pegs are broad
- Connective tissue is normal
Question 3. Carcinoma in situ
Answer:
Carcinoma In Situ
Carcinoma In Situ is the most severe stage of epithelial dysplasia, which involves the entire thickness of the epithelium with the basement membrane intact
Carcinoma In Situ Clinical Features:
- Age: elderly patients
- Sex: common in males
- Carcinoma In Situ Presentation:
- Appears as white plaques or ulcerated areas
- Site: floor of the mouth, tongue, lip, etc
- Appears as leukoplakia or erythroplakia
Carcinoma In Situ Treatment:
- Surgery
- Radiotherapy
- Electrocautery
Question 4. Epithelial dysplasia
Answer:
Epithelial Dysplasia
- Dysplasia means disordered cellular development
- Epithelial dysplasia is characterized by cellular proliferation and cytological changes
Epithelial Dysplasia Features:
- Nuclear hyperchromatic
- Cellular pleomorphism
- Irregular epithelial stratification
- Increased nuclear-cytoplasmic ratio
- Poikilocylosis
- Loss of polarity of basal cells
- Increased number of mitotic figures
- Individual cell keratinization
- Dyskeratosis
- Absence of intercellular adhesions
- Enlarged nucleoli
- Drop-shaped rete pegs
Question 5. Papilloma
Answer:
Papilloma
- Papilloma is a common benign neoplasm of the oral cavity arising from epithelial tissue
- Papilloma is characterized by exophytic growth with a typical cauliflower-like appearance
Papilloma Clinical Features:
- Age- third, fourth, and fifth decade of life
- Sex– both sexes are equally affected
- Site involved
- Tongue
- Lips
- Buccal mucosa
- Gingiva
- Hard and soft palate
- Present as slow growth, exophytic, soft, pedunculated, painless, nodular growth with a cauliflower-like appearance
- Have numerous finger-Iike projections over the surface
- Papilloma appears as ovoid swelling with a corrugated surface
- Size- a few mm to 1 cm in diameter
- The base of the lesion may be pedunculated or sessile
- Color- White
- Surface- highly keratinized
- Superficial ulceration and secondary infection occur
- Rarely papilloma grows inward
Papilloma Histopathological Features:
- Characterized by multiple, long finger-like projections
- There is the presence of koilocytes and virus-altered epithelial clear cells in the Spinus cell layer of epithelium
- There is increased mitotic activity in the basal layer of epithelium
- Little cellular atypia is seen
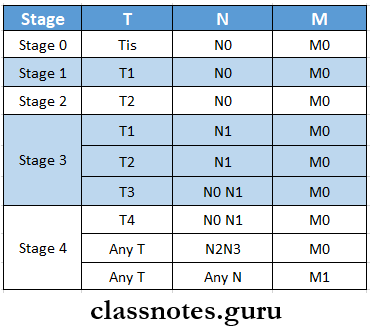
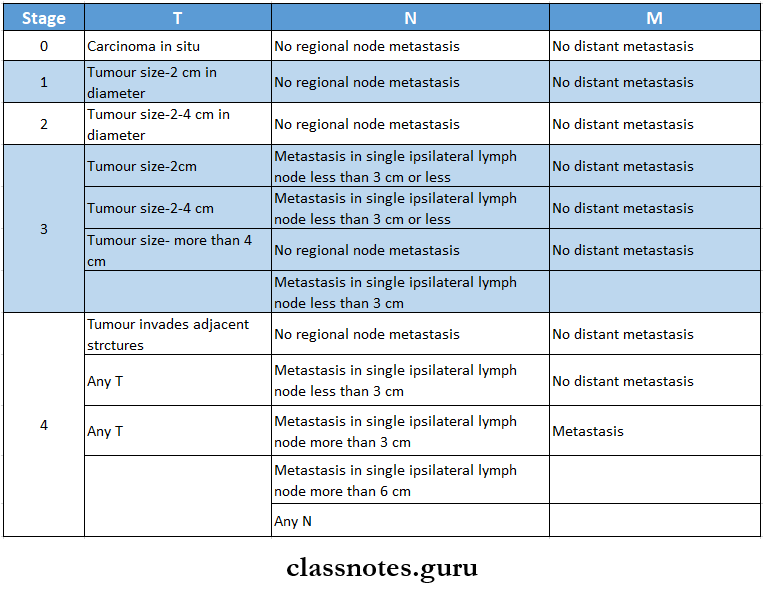
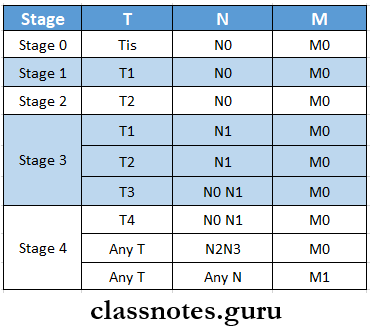
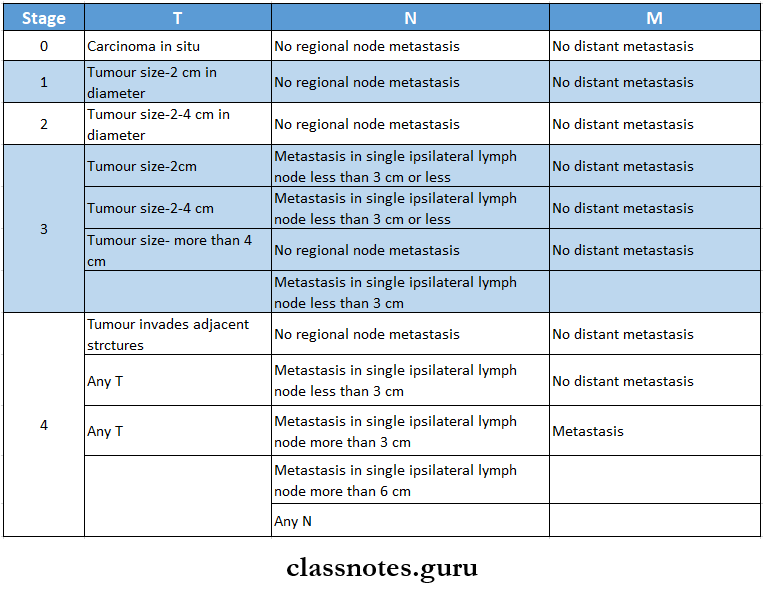
Question 6. TNM Classification
Answer:
TNM Classification
- TNM is the staging of malignancy which measures 3 major parameters of cancer
- T- the size of the tumor
- N- lymph node involvement
- M- distant metastasis
- T- Primary tumor
- Tx- Primary tumor cannot be assessed
- T0- No evidence of primary tumor
- This- carcinoma in situ
- T1- Tumour size- 2 cm or less in diameter
- T2- Tumour size- 2-4 cm in diameter
- T3- Tumour size- more than 4 cm in diameter
- T4- Tumour invades adjacent structures
- N- Regional lymph node
- Nx- Regional lymph node cannot be assessed
- N0- No regional lymph node metastasis
- N1- Metastasis in single ipsilateral lymph node, 3 cm or less in dimension
- N2- Metastasis in single ipsilateral lymph node, more than 3 cm but less than 6 cm
- N2a- Metastasis in single ipsilateral lymph node, 3-6 cm in dimension
- N2b- Metastasis in multiple ipsilateral lymph nodes, not more than 6 cm
- N2c- Metastasis in bilateral or contralateral lymph nodes, not more than 6 cm
- N3- Metastasis in lymph node, more than 6 cm in dimension
- M- Distant metastasis
- Mx- The presence of distant metastasis cannot be assessed
- M0- No distant metastasis
- Ml- Presence of metastasis
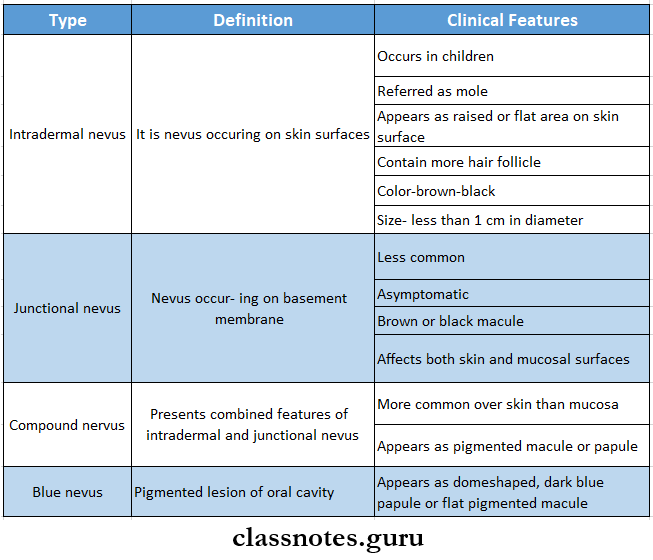
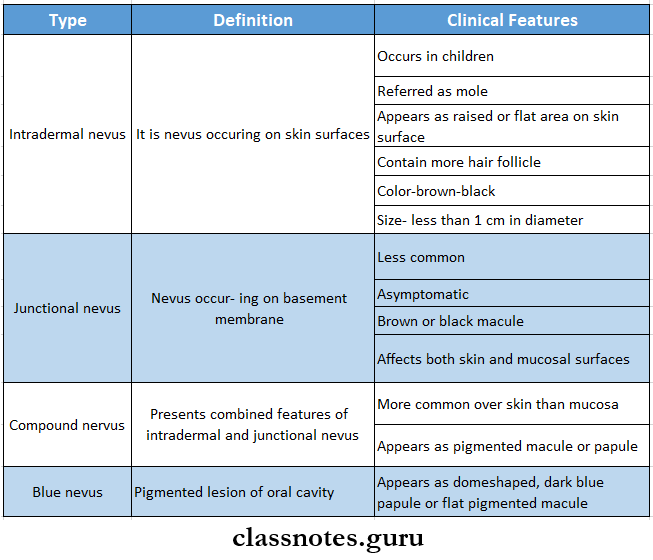
Question 7. Nevus
Answer:
Nevus Definition: It is defined as congenital, developmental, tumourlike malformation of the skin or mucous membrane
Nevus Types:
Question 8. Hemangioma
Answer:
Hemangioma
They are relatively common benign proliferative lesions of vascular tissue origin
Hemangioma Clinical Features:
- Age and sex: early-females are commonly affected
- Site: intraorally over
- Tongue
- Lip
- Buccal mucosa
- Palate
- Within jaw bones
- Within salivary gland
- They are usually raised, multinodular, red or purple lesions
- When a hemangioma is compressed with the help of a slide it blanches
- Once the pressure is released, its reddish appearance returns due to the refilling of the tumor cells with blood
- Hemangioma is soft and compressible
- The size of the lesion varies from time to time
- Port wine stain is often seen over the face
- Jawbones involvement
- Mandible is more commonly affected
- Hemangioma produces slow enlarging, painful, expansile jaw swelling
- Hemangioma may cause erosion of the bone
- Loosening of the teeth
- Anesthesia or paraesthesia of the skin and oral mucosa
Hemangioma Differential Diagnosis:
- Pyogenic granuloma
- Mucoceles
- Kaposi’s sarcoma
- Salivary gland neoplasm
Hemangioma Management:
- Local excision for smaller lesions
- Larger lesions are treated by excision after pretreatment of the lesion with, sclerosing agents to reduce the size of the lesion
Question 9. Blue Nevus
Answer:
Blue Nevus
Blue nevus is a common pigmented lesion of the oral cavity
Blue Nevus Clinical Features:
- Blue Nevus appears as a dome-shaped, dark blue papule or flat-pigmented macule
- Appears over skin as well as oral mucosa
- Intraorally seen over hard palate
Blue Nevus Histopathology:
- Melanin-producing cells are elongated, bipolar and spindle-shaped
- Blue Nevus are oriented parallel to the overlying epithelium
- Presence of fusiform dendritic cells
- Few pigmented macrophages called melanophages are present
Question 10. Histopathology Of Verrucous Carcinoma
Answer:
Histopathology Of Verrucous Carcinoma
- Epithelium is well-differentiated
- Marked epithelium proliferation with down growth of epithelium into connective tissue is seen
- Shows little mitotic activity, pleomorphism, and hyperchromatism
- Cleft-like spaces lined by thick layers of parakeratin extend from the surface deep into the lesion
- Parakeratin plugging also extends into the epithelium
- Parakeratin lines the clefts with the parakeratin plugging
- The basement membrane is intact
- Chronic inflammatory cell infiltration in connective tissue may appear
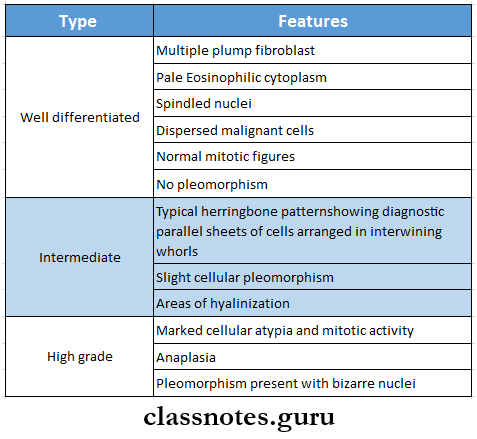
Question 11. Fibrosarcoma
Answer:
Fibrosarcoma
Fibrosarcoma is a tumor of mesenchymal cell origin composed of malignant fibroblast in a collagenous background
Fibrosarcoma Types:
- Primary
- Malignant fibroblastic producing variable amount of collagen
- Central fibrosarcoma – arises from the medullary canal
- Peripheral fibrosarcoma – arises from periosteum
- Secondary
- Arises from pre-existing lesions or after radiotherapy
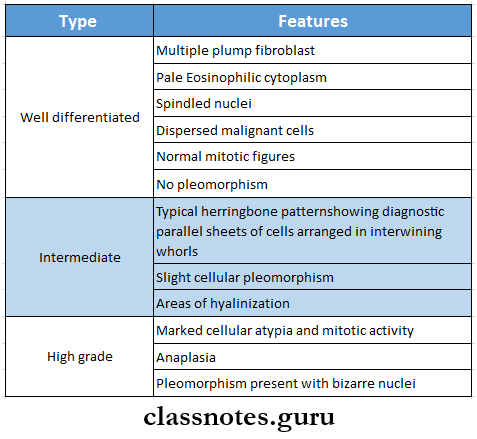
Fibrosarcoma Histopathology
Benign And Malignant Tumours Of The Oral Cavity Short Question And Answers
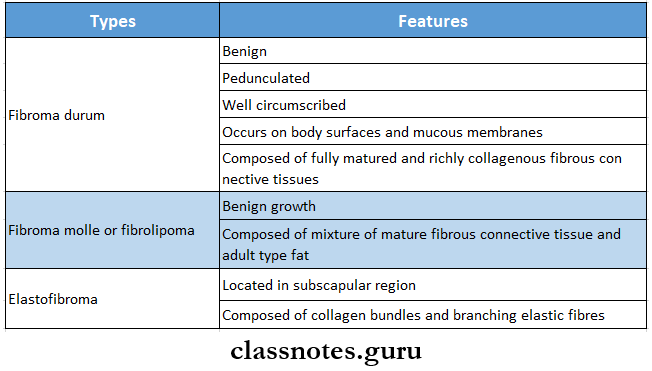
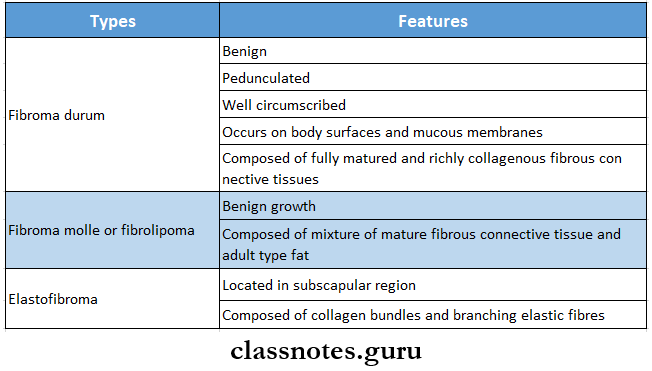
Question 1. Fibroma
Answer:
Fibroma
Fibroma are uncommon tumors of soft tissues
Fibroma Types: Based on microscopic appearance, fibroma are of three types
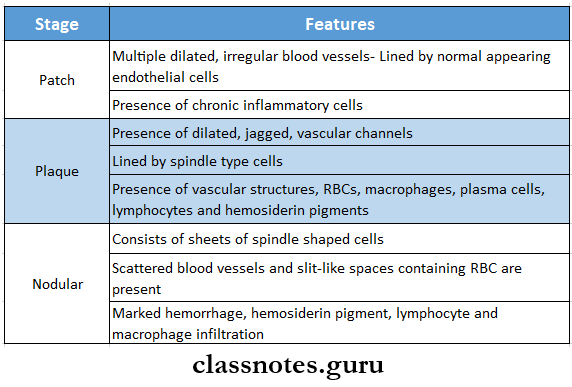
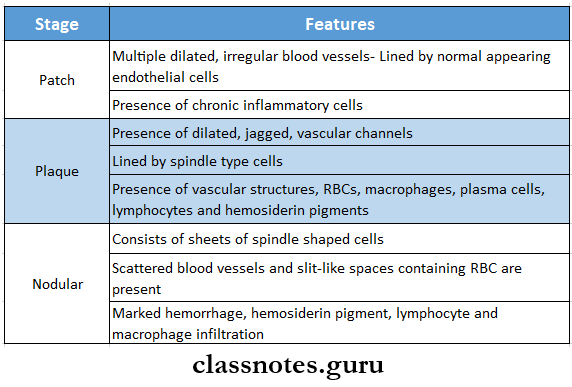
Question 2. Histology of Kaposi’s sarcoma
Answer:
Histology of Kaposi’s Sarcoma
Question 3. Histology of Burkitt’s lymphoma
Answer:
Histology Of Burkitt’s Lymphoma
- Burkitt’s lymphoma consists of proliferation of small B-lymphocytes
- Burkitt’s Lymphoma Cells Have
- Large round nuclei
- Prominent nuclear membrane
- Stippled nucleoplasm
- Prominent nucleoli
- Minimal cytoplasm
- Abundant mitotic activity
- Numerous macrophages are scattered throughout the tumour giving a starry sky appearance
- The malignant cells invade the periodontal ligament and dental pulp
- Presence of multinucleated giant cells
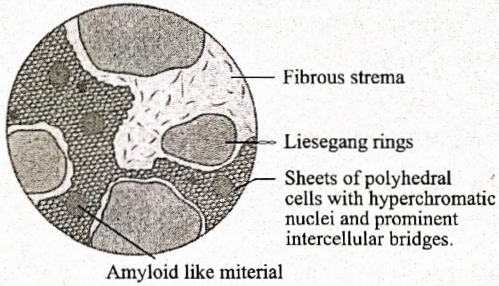
Question 4. Histopathology of well-differentiated squamous cell carcinoma
Answer:
Histopathology Of well-Differentiated Squamous Cell Carcinoma
- In it, the malignant tumor epithelial cells resemble cells of squamous epithelium
- They produce large amounts of keratin in the form of keratin pearls
- These cells invade underlying connective tissue and form epithelial islands
- These islands are bordered at the periphery by basal cells
- Dysplastic features are
- Cellular pleomorphism
- Nuclear hyperchromatism
- Individual cell keratinization
- Altered nuclear-cytoplasmic ratio
- Presence of epithelial maturation, keratinization, stratification, and existence of intracellular bridges
Question 5. Hairy Leukoplakia
Answer:
Hairy Leukoplakia
Hairy Leukoplakia is an HTV-associated mucosal disorder
Hairy leukoplakia Clinical Features:
- Site Involved
- Lateral and ventral surface of the tongue
- Floor of mouth
- Buccal or labial mucosa
- Palate
- Present as slightly raised, white plaque with vertically corrugated, irregular surface
- The surface contains numerous projections resembling hairs
- Size- a few millimeters to 3 cm in diameter
- Asymptomatic
- Colonizes Candida albicans
Hairy Leukoplakia Histopathology:
- Consists of a parakeratin layer containing the candidal organism
- Presence of sub-corneal upper spinous layer zone of keratinocytes
- Balloon cells are present which are large, pale staining epithelial cells
- They exhibit clear cytoplasm and vesicular nuclei with margination of chromatin
Question 6. Erythroplakia Speckled
Answer:
Erythroplakia Speckled
- Erythroplakia is also known as granular erythroplakia
- Erythroplakia is a type of erythroplakia classified based on appearance
- Characterized by the presence of soft, irregular, raised, erythematous areas in epithelium with a granular surface
- Erythroplakia is soft on palpation with a velvety feel
- There are some tiny, focal white plaques distributed all over the red surface
Question 7. Traumatic Neuroma
Answer:
Traumatic Neuroma
Traumatic Neuroma is also known as amputation neuroma
Traumatic neuroma Etiology: Due to injury to the nerve
Traumatic neuroma Clinical Features:
- Appear as a small nodule or swelling of mucosa near the mental foramen, alveolar ridge, lips, or tongue
- Pain occurs on pressing the tire involving the nerve
- Pain refers to the face, eyes, throat, head
Traumatic neuroma Histopathology:
- Consists of nerve bundles
- Presence of fibrous septa
Question 8. Basal cell carcinoma (or) Rodent ulcer
Answer:
Basal Cell Carcinoma
- Also called a rodent ulcer.
- Carcinoma is the most common tumor.
- Carcinoma is a locally invasive, slow-growing tumor of middle-aged individuals that rarely metastasizes.
Rodent Ulcer Etiology:
- Prolonged exposure to strong sunlight
- UV rays
- Arsenic is used in skin ointments.
Rodent ulcer Clinical Features:
- The majority of lesions occur on the face, usually above a line joining the lobe of the ear and the angle of the mouth.
- Common sites are the inner and outer canthus of the eye, the eyelids bridge of the nose, and around the nasolabial fold.
- The most common pattern is a nodule-ulcerative lesion a slow-growing small nodule that undergoes central with pearly, rolled margins.
- Tumour enlarges in size by burrowing and by destroying the tissues locally like a rodent hence the name rodent ulcer.
Question 9. Junctional Nevus
Answer:
Junctional Nevus Clinical Features:
- Asymptomatic lesion
- Appears as brown or black macule over the skin or oral mucosa
- Intraorally it is seen over the hard palate and gingiva
Junctional Nevus Histopathology:
- Consist of proliferating nevus cells at the basement membrane zone of epithelium
- They form clusters, especially at the apex of epithelial rete pegs
- These cells may undergo malignant transformation and result in malignant melanoma
Junctional Nevus Treatment: Surgical excision
Question 10. Neurofibroma
Answer:
Neurofibroma
- Also known as neurofibromatosis or von Recklinghausen’s disease
- Arises from connective tissue sheath of Schwann cells
Neurofibroma Features:
- Occurs at any age and in any sex
- Site involved- tongue, buccal mucosa, vestibule, lips, jaws
- Present as small, asymptomatic, soft to firm, submucosal mass
- Well-demarcated, freely movable mass
- Produces slow-growing, expansile swelling of jaw bones
- Pain and paraesthesia if it involves nerve
- Diffuse lesions producing massive flabby soft masses over oral mucosa
- Cafe-au-lait spots
- Macrognathia
- Macroglossia
- Deformity of bone
Question 11. Exostoses
Answer:
Exostoses
- Exostoses is also known as hyperostosis
- Found on the buccal surface of the maxilla below the mesiobuccal fold in the molar region
- They appear as small nodular protuberances
- The overlying mucosa is blanched
- They interfere with the preparation and insertion of prosthetic appliance
- Its etiology is unknown
Question 12. Torus palatinus
Answer:
Torus palatinus
- Torus palatinus is slow growing, flat-based bony protuberance occurring in the midline of the palate
- Torus palatinus is a hereditary condition
- Common in females
- Shape- flat, spindle, nodular or lobular
- Mucosa may be intact or ulcerated
- Torus palatinus is composed of dense compact bone with the center of cancellous bone
Question 13. Keratoacanthoma
Answer:
Keratoacanthoma
Keratoacanthoma is a benign endophytic epithelial tissue neoplasm, which commonly occurs in the sun-exposed skin of the face and it usually appears as a circumscribed keratin-filled crater
Keratoacanthoma Features:
- Keratoacanthoma appears as a small, well-circumscribed, elevated, and crater-like lesion with a central depression
- Keratoacanthoma initiates as a small lump or bud-like growth on the sun-exposed skin surface of the face
- Keratoacanthoma grows rapidly and achieves the maximum size over about 4-8 weeks
- Keratoacanthoma reveals a well-circumscribed, elevated nodule that has a sharply delineated, rolled margin and a central keratotic core
- Keratoacanthoma is often painful
- Keratoacanthoma may have associated lymphadenopathy
Keratoacanthoma Treatment: Surgical excision of the lesion is done
Question 14. Reed Sternberg Cells
Answer:
Reed Sternberg Cells
- Reed Sternberg cells are characterized as malignant cells of Hodgkin’s disease
- They are large cells
- Size- 20-50 micrometers in diameter
- Contains abundant, amphophilic, finely granular, or homogenous cytoplasm
- Nuclei show mirror image with eosinophilic nucleolus and thick nuclear membrane- They give owl eye appearance
Question 15. Bence Jones proteins
Answer:
Bence Jones Proteins
- Bence-jones proteins are light chain proteins produced by tumor cells
- Due to this serum protein levels raises
- Bence Jones Proteinspresence in urine detects multiple myeloma
- Serum and urinal protein Immunoelectrophoresis is done to detect it
- Bence-Jones protein coagulates when the urine is heated to 42 degrees C to 60 degrees C
- Bence Jones Proteinsdisappears when the urine is boiled and finally reappears again as the urine is cooled
- Bence Jones Proteins is also present in patients with polycythemia or leukemia
Question 16. Kaposi sarcoma
Answer:
Kaposi Sarcoma
Kaposi Sarcoma is a malignant neoplasm arising from the endothelial cells of the blood capillaries
Kaposi Sarcoma Etiology:
- Genetic predisposition HIV
- Immunosuppression
- Environmental factors
Kaposi Sarcoma Clinical Features:
- Sites: maxillary gingiva, tongue
- Kaposi Sarcoma Clinical Stages:
- Patch stage:
- Patch stage is the initial stage of the disease and during this, a pink, red, or purple macule appears over the oral mucosa
- Plaque Stage
- Plaque stage continued into the plaque stage with time and during this stage, the lesion appears as a large, raised plaque
- Nodular Stage:
- Nodular stage is the last stage of the disease
- Nodular stage is characterized by the occurrence of multiple nodular lesions on the skin or the mucosa
Kaposi Sarcoma Management:
Question 17. Staging and grading of squamous cell carcinoma
Answer:
Staging Of Squamous Cell Carcinoma:
Grading Of Squamous Cell Carcinoma:
- Squamous cell carcinoma is graded into three types according to histological features
- Well-differentiated squamous cell carcinoma
- Moderately differentiated squamous cell carcinoma
- Poorly differentiated squamous cell carcinoma
Question 18. Peripheral giant Cell carcinoma
Answer:
Peripheral Giant Cell Carcinoma
Peripheral Giant Cell Carcinoma is common giant cell lesions arising from tooth-bearing areas of the jaw
Peripheral Giant Cell Carcinoma Clinical Features:
- Age- during the mixed dentition period
- Sex- common in females
- Site- interdental papilla
- Appears as a small, exophytic, well-circumscribed, pedunculated lesion on the gingival surface
- Peripheral Giant Cell Carcinoma is painless, firm, and lobulated
- Surface- smooth or granular
- Size-less than 2 cm in diameter
- Color-purplish-red to dark-red in color
- The overlying epithelium is ulcerated
- Consistency- firm
- Bleeding occurs spontaneously
- Some lesions may develop with hour-glass shapes located between teeth and lobulated extremities projecting both buccally and lingually
Question 19. Radiological and biological findings of multiple myeloma
Answer:
Radiological Features:
- Seen bilaterally and in mandibular posterior region and ramus
- Appears as sharply punched-out radiolucency
- Size- varies from a few millimeters to centimeters in diameter
- The tooth may appear radiopaque due to mineral loss
- Diffuse destructive lesions of bone occurs
Histopathological Features:
- Characterized by diffuse sheets of closely packed, monotonous, round, or oval cells resembling typical plasma cells
- Cells consist of eccentrically placed nuclei and exhibit chromatin clumping in a typical “cart-wheel” or ‘checkerboard’ pattern
- The presence of high mitotic figures and binucleated or multinucleated cells
- Neoplastic plasma cells invade and destroy normal tissues of the body
- Deposition of amyloids beneath plasma cells
- Amyloids appear as homogenous, eosinophilic acellular areas
Question 20. Lymphangiomas
Answer:
Lymphangiomas
Lymphangiomas are benign hematogenous neoplasms characterized by excessive proliferation of the lymphatic vessels
Lymphangiomas Types:
- Capillary lymphangioma- contains numerous small lymphatic capillaries
- Cavernous lymphangioma- contains large dilated lymphatic vessels
- Cystic hygroma- It is a massive diffuse lesion of the neck
Lymphangiomas Clinical Features:
- Age- Present at birth or during childhood
- Site- head and neck region
- Intraoral lesions are painless, flat or nodular, or vesicle-like translucent swelling
- Surface- pebbly resembling frog-eggs
- Regress spontaneously
- Some lesions may produce diffuse, soft, painless, submucosal lumps
- Color- pale or red-blue
- The secondary hemorrhage causes the purple color of the lesion
- Palpitation produces crepitate sound
- Diffuse and extensive lesions over the tongue produce macroglossia
- Cervical lymphangiomas produce respiratory distress
- Cystic hygroma is present as massive, pendulous, fluctuant swelling on the lateral neck
Question 21. Leukocytosis
Answer:
Leukocytosis
- Leukocytosis is an increase in the number of white cells and is common in a variety of reactive inflammatory states caused by microbial and non-microbial stimuli.
- Causes of Leukocytosis: Leukocytosis is relatively nonspecific and can be classified based on particular white cell series affected as follows:
- Neutrophilic leucocytosis.
- Acute bacterial infections especially those caused by pyogenic organisms.
- Sterile inflammation caused by tissue necrosis (myocardial infarction, bums)
- Eosinophilic leucocytosis (eosinophilia)
- allergic disorders such as asthma, hay fever
- Allergic skin diseases, for example, pemphigus, and dermatitis herpetiform.
- Parasitic infestations
- Drug reactions
- Certain malignancies, for example’ ‘s disease, and some non-Hodking’ s lymphomas.
- Collagen vascular disorders and some vasculitis.
- Basophilic leucocytosis (basophilia): Rare and often indicates CML.
- Monocytosis
- Chronic infections, for example tuberculosis
- Bacterial endocarditis
- Rickettsiosis and malaria
- Collagen vascular diseases, for example, systemic lupus erythematosus (SLE)
- Inflammatory bowel diseases, for example, ulcerative colitis
- Lymphocytosis: Usually accompanies monocytosis in many disorders associated with it.
- Chronic immunologic stimulation, for example, tuberculosis, brucellosis and
- Viral infections, for example, hepatitis A, cytomegalic- virus, Epstein-Barr virus, and Bordetella pertussis infections.
Question 22. Veracay Bodies
Answer:
Veracay Bodies
- They are groups of uniform, fusiform cells arranged in whorls, herringbones, or palisades
- These are histologic features of Schwann cell tumors
- There is a peculiar arrangement of nuclei in transverse bands
- These bands of fusiform nuclei have alternate clear zones devoid of nuclei
- Typically found in the more densely packed Antoni A regions rather than in the loose or microcystic Antoni B areas
Question 23. Hamartoma
Answer:
Hamartoma
- Hamartoma is a benign, focal malformation that resembles a neoplasm in the tissue of its origin
- Hamartoma is not a malignant tumor but grows at the same rate as the surrounding tissues
- Hamartoma is composed of tissue elements normally found at that site but in disorganized mass
- Occur in many different parts of the body
- They are asymptomatic
Question 24. Plasmacytoid Cell
Answer:
Plasmacytoid Cell
- A characteristic feature of myoepithelioma
- They are round cells with eccentric nuclei and Eosinophilic cytoplasm
- The neoplastic cells proliferate either as
- Closely packed sheets of round cells or
- Group of cells separated by loose myxoid stroma
Question 25. Histopathology of fibroma
Answer:
Histopathology Of Fibroma
- Fibroma consists of bundles of interlacing collagen fibers interspersed with varying numbers of fibroblasts and small blood vessels
- The epithelium is stratified squamous epithelium
- Shortening and flattening of rete pegs occurs
- Areas of diffuse or focal calcification are found
- In presence of trauma, vasodilatation, edema, and inflammatory cell infiltration are present
Question 26. Four dysplastic features
Answer:
Four Dysplastic Features
- Loss of polarity of basal cells
- The presence of more than one layer of cells having a solid appearance
- Increased nuclear-cytoplasmic ratio
- Drop-shaped rete pegs
- Irregular epithelial stratification
- Increased number of mitotic figures
- Cellular pleomorphism
- Nuclear hyperchromatism
- Enlarged nucleoli
- Reduced cellular cohesion
- Keratinization of single cells or cell groups in the prickle layer
Benign And Malignant Tumours Of The Oral Cavity Viva Voce
- Papilloma is exophytic growth made up of numerous small finger-like projection
- Keratoacanthoma occurs in sun-exposed areas
- Fibroma is the most common benign soft tissue neoplasm occurring in the oral cavity
- Lipoma is composed of mature fat cells or adipocytes
- A cirsoid aneurysm is a tortuous mass of small arteries and veins linking a larger artery and vein
- Varicose aneurysm consists of an endothelium-lined sac connecting the artery and vein
- Aneurysmal varix represents a direct connection between an artery and a dilated vein
- Central hemangioma presents a honeycomb appearance
- Arteriovenous aneurysm represents a direct communication between artery and vein through which blood bypasses the capillary circulation
- An immature capillary hemangioma that is highly cellular with poorly canalized vessels occurring very early in life is referred to as juvenile hemangioendothelioma
- Torus platinum is a bony protuberance occurring in the midline of the hard palate
- The torus mandibularis is an outgrowth of bone found on the lingual surface of the mandible
- Cartwheel or checkerboard cell pattern is seen in multiple myeloma
- Neurofibromatosis is also known as Von Recklinghausen disease
- The most common site of basal cell carcinoma is the lower lip
- Phaeochromocytoma is a tumour of the adrenal medulla
- Sarcoma of soft tissues spread by blood vessels
- Abtropfung effect is seen in junctional nerves in nevus
- Central giant cell granuloma gives a whorled appearance to cells
- Multiple myeloma gives cartwheel or checkerboard pattern
- Multiple oral papillomas are present in focal dermal hypoplasia syndrome
- The histological feature of oral papilloma is the proliferation of the spinous layer
- Burkitt’s lymphoma originates from T lymphocytes
- Burkitt’s lymphoma is caused by to Epstein-Burr virus
- Kaposi sarcoma is due to cytomegalovirus
- Reed Sternberg giant cells are found in Hodgkin’s disease
- Burkitt’s lymphoma gives a starry sky appearance
- Osteosarcoma gives sunray burst appearance in radiograph
- Punched-out areas are seen in multiple myeloma
- The most common benign bone tumor is Osteochondroma
- The most common malignant bone tumor in children is osteosarcoma
- Mostly lip cancers occur over the lower lip
- Sarcomas metastasizes through the bloodstream
- Sarcoma that spreads through lymphatics is Rhabdomyosarcoma
- Carcinomas Spread through lymph nodes.
- The presence of epithelial pearls in spinous layers of epithelium is characteristic of carcinoma.