Epidemiology Of Oral Diseases Definitions
Epidemiology
- Epidemiology is defined as the study of the distribution and determinants of health-related states or events in specified populations and the application of this study to the control of health problems
Dental caries
- Dental caries is defined as an infectious, microbiologic disease of the teeth that results in localized dissolution and destruction of the calcified tissues
Epidemiology Of Oral Diseases Important Notes
1. Diet studies related to dental caries
- Vipeholm study
- Hopewood House study
- Turku sugar study
- Hereditary fructose intolerance
- Tristan da Cunha’s study
2. Vipeholm study
- Described by Gustaffson et al in 1954 and summarized by Davies in 1955
Read And Learn More: Percentive Communitive Dentistry Question And Answers
Vipeholm Method:
- The institutional diet was nutritious but contained little sugar with no provision for between meals
- 4 meals were eaten daily
- 7 groups were obtained
- Control group
- Sucrose group
- Bread group
- Chocolate Group
- Caramel Group
- 8 toffee group
- 24 toffee group
Vipeholm Conclusion:
- An increase in carbohydrate intake increases dental caries
- Retentive sugar items cause an increase in dental caries
- Sugar consumed in between meals causes dental caries
- Increase in caries activity varies between individuals
- Withdrawal of sugar items causes the disappearance of increased caries activity
- A high concentration of sugar in solution & its prolonged retention leads to increased caries activity
- An increase in clearance time of sugar increases caries activity
Epidemiology Of Oral Diseases Questions And Answers
3. Hopewood house study
- Investigators are Harris and Sullivan
- The dental status of children between 7-14 years of age residing at Hopewood House, Bowral, New South Wales was studied longitudinally for 10 years
- The absence of meat and the rigid restriction of refined carbohydrates are two important features of the study
Hopewood house Result:
- At the end of 10 years
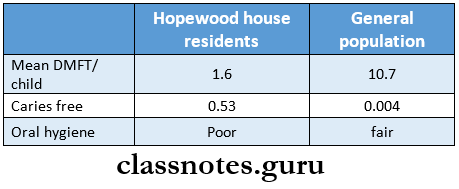
Hopewood House Conclusion:
- In institutionalized children dental caries can be reduced by a restricted carbohydrate diet even in the presence of unfavourable oral hygiene
4. Turku sugar study
- Investigators are Scheinin and Makinen et al
- Investigated the effect of sucrose, fructose and xylitol on caries development
Turku sugar Conclusion:
- Sucrose – highly cariogenic
- Fructose – cariogenic as sucrose for the first 12 hours but less at the end of 24 hours
- Xylitol – anti-cariogenic with 85% reduction in dental caries
5. Tristan
- Investigator is Fisher
- He carried dental examinations in 1932,1937, and 1953 on the island and again in England in 1962 and 1966 in the island when the people of Tristan de Cunha returned to their island from England
Tristan Results:
- In 1932 and 1937 – 0% of caries
- In 1962-50%
- In 1966-80%
6. Hereditary fructose intolerance
- It is due to reduced levels of enzyme fructose-l-phosphate aldolase required for the metabolism of sucrose or fructose
- Persons affected by it avoid food containing fructose or sucrose because ingestion of these foods causes nausea, vomiting, excessive sweating and even coma.
7. Predictors of high caries risk are
- Multiple new lesions
- Multiple restorations
- History of premature extraction for caries
- Anterior teeth caries or restoration
- History of frequent replacement of restoration
8. Frequent intake of sucrose for at least 60-100 minutes/day is associated with the formation of rampant caries
Oral Diseases Epidemiology
Epidemiology Of Oral Diseases Long Essays
Question 1. Define epidemiology. Describe the epidemiological factors of oral cancer.
Answer:
Epidemiology Definition:
It is defined as the study of the distribution & determinants of health-related states or events in specified populations and the application of this study to the control of health problems
Epidemiological Factors Of Oral Cancer:
Host:
- Age:
- Older people show an incidence of carcinoma
- Younger people show an incidence of sarcoma
- Race:
- Whites develop lip melanoma more frequently
- Sex
- Carcinoma of the lip common in women
- Cancer of the tongue & buccal mucosa common in males
- Genetic factors
- Oncogenes involved in the initiation & progression of malignancy
- Occupation
- Textile workers show an increased incidence of oral cancer
Read And Learn More: Percentive Communitive Dentistry Question And Answers
- Immunity
- Kaposi sarcoma common in AIDS patient
- Social class
- Low-income group shows an increase in cancer of the oral cavity
- Customs & Habits
- Smoking increases the incidence of cancer
Agent:
- Biological
- Virus
- Fungi
- Chemical
- Arsenic
- Dyes
- Nickel
- Aromatic amines
- Mechanical
- Sharp tooth
- fitting dentures
- Jagged teeth
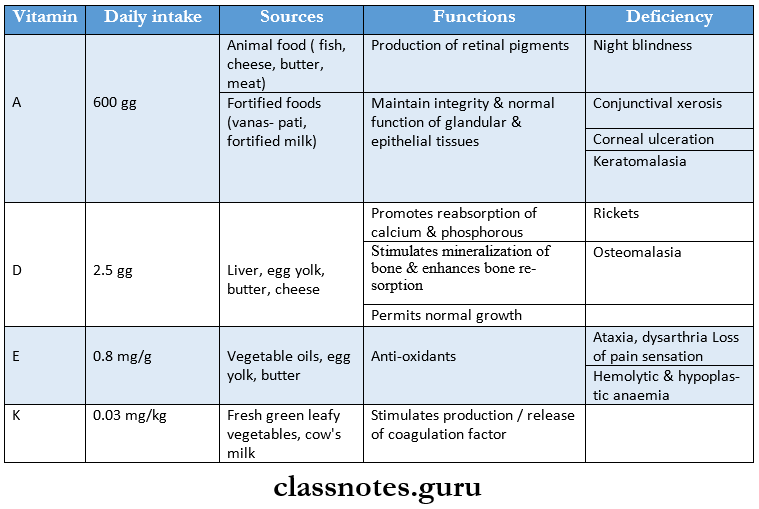
- Nutritional agents
- Precarcinogens
- Increased consumption of fat
- Deficiency of folic acid
- Protein deficiency
- Increased consumption of red chilli powder
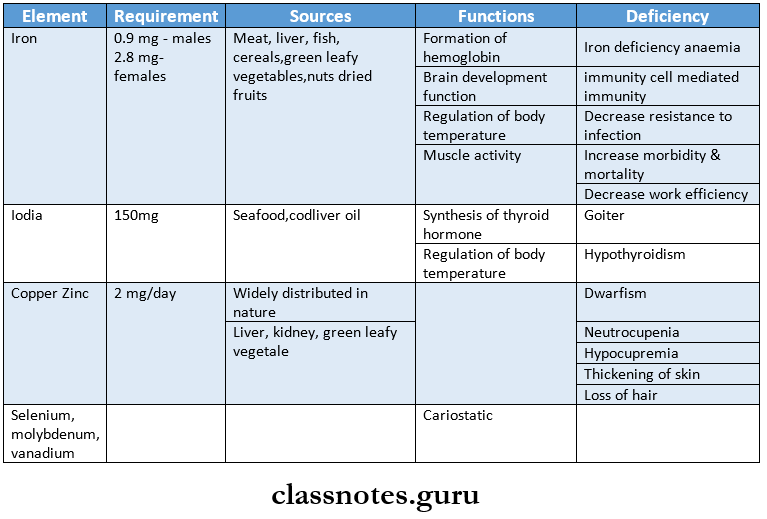
- Decrease in copper, zinc, vegetable, vitamin C, E
Environmental:
- Water contaminants
- Includes some organic pollutants like chloroform
- Air pollution
- Caused by the release of several gases from automobiles & factories
- Geographic variation
- In the Netherlands: buccal mucosa is most affected
- In Switzerland: the lip & tongue are most affected
- In Canadian Eskimos: cancer of the salivary gland is more common
- In Srikakulam & Vishakapatnam: palatal cancer is the most common
- Solar heat
- Prolonged exposure to sunlight causes melanoma
- Industrialization
- The release of various toxins by the industries contaminates water & lead to cancer
Epidemiology Of Dental Caries
Question 2. Epidemiology of periodontal disease.
Answer:
Epidemiology of periodontal disease Agent:
Dental plaque:
- Dental plaque is a primary etiological factor for periodontal disease
- Dental plaque is defined as a structured, resilient, yellow-greyish substance that adheres tenaciously to the intraoral hard surfaces, including removable & fixed restoration
- Dental plaque is composed of bacteria in a matrix of salivary glycoprotein & extracellular polysaccharides
- Dental plaque is because of this matrix, it cannot be removed by rinsing
- Classified into
- Supragingival plaque: at or coronal to marginal gingiva
- It is responsible for gingivitis
- Subgingival plaque: apical to gingival margin
- It is responsible for calculus & root caries
- Accumulation of plaque is found more on the gingival l/3rd of the tooth surfaces, cracks, pits & fissures, overhanging restoration & around malaligned teeth
- Supragingival plaque: at or coronal to marginal gingiva
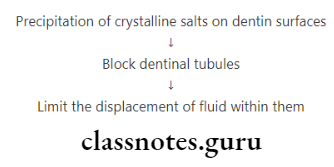
Calculus:
- Calculus is a hard deposit that forms by mineralization of dental plaque & is usually covered by a layer of unmineralized plaque
- Calculus is classified into
- Supragingival calculus
- Located coronal to the gingival margin
- Calculus is white or whitish-yellow
- Calculus has a hard, clay-like consistency
- Calculus can be easily detached from the tooth
- Subgingival calculus
- Subgingival calculus is located below the crest of the marginal gingiva
- Subgingival calculus is a dark brown or greenish black
- Subgingival calculus is hard & dense
- Subgingival calculus is firmly attached to the tooth structure
- Calculus provides a fixed nidus for the continued accumulation of plaque
Host Factors:
- Age
- The prevalence of periodontal disease increases with age due to the cumulative progression of the lesions over time
- Gender
- Based on epidemiological studies, the prevalence & severity is higher in males than in females
- Socio economic status
- Lower socioeconomic status results in poor diet, poor oral hygiene & a general lack of dental awareness
- Whereas those who are well-educated, wealthier & live in better circumstances visit dentists frequently
- Thus periodontal disease prevalence increases in low socioeconomic status
- Diet & Nutrition
- Sticky foods adhere to the teeth & are difficult to remove thus interfering with the natural cleansing mechanism and leading to periodontal disease
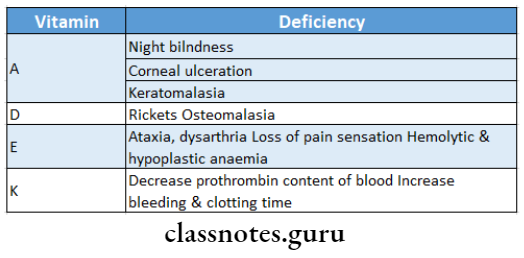
- The nutrients associated with periodontal tissues are vitamin A, B complex, C, D, calcium & phosphorous
- Prevalence & severity of periodontal disease increases in protein malnutrition & vitamin A deficiency
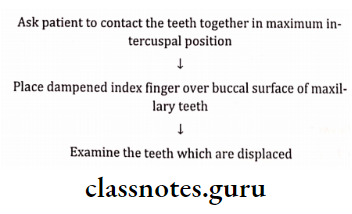
- Anatomy
- The normal contour of the tooth protects the underlying tissues
- Tooth
- Sharp cusps, uneven marginal ridges, lack of contact between teeth & crowding can cause food impaction
- Soft tissue
- When the frenum is inserted close to the marginal gingival, the pull of attachment may cause recession of the papilla along with interfering with the proper use of the toothbrush
- Habits
- Thread biting, holding nails between teeth, bruxism, lip, cheek & nail biting can cause traumatic effects on the periodontium
- Local irritants
- Mechanical
- Faulty tooth brushing causes abrasion or recession of the gingival tissues
- Faulty restoration impinges on gingival & irritates them
- Faulty orthodontic treatment results in root resorption as well as alveolar bone loss & Mobility
- Mechanical
- Chemical
- Alcohol, tobacco & condiments lower tissue resistance & increase susceptibility to gingivitis & periodontitis
- Atmospheric lowers the tissue resistance
- Systemic factors
- Systemic diseases act locally to reduce the resistance to periodontal destruction & the local periodontal pathogens act systemically to produce an impact on the general health
Epidemiology of periodontal disease Environmental Factor
Geographic variation:
- Nutrition:
- Avitaminosis C, Niacin deficiency shows an increased prevalence of periodontal disease
- Increased prevalence of periodontal disease was found in areas with protein malnutrition & vitamin A Deficiency
- Degree of urbanization
- Rural areas may have an increased prevalence than urban areas
- It can be due to oral hygiene practices, diet & socioeconomic status
- Psychological & cultural factors
- Stress predisposes to ANUG
- Certain cultures view dental problems & loss of teeth solely as an ageing process
Periodontal Disease Epidemiology
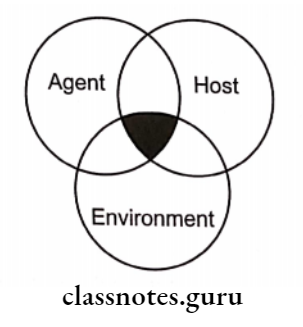
Question 3. What is an epidemiological triad? Discuss the role of components of an epidemiological triad in dental caries.
Answer:
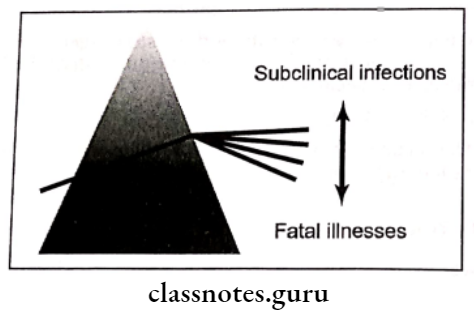
Epidemiological Triad:
- The occurrence of any disease is determined by the interaction between the agent, host and environment constituting an epidemiological triad
Components In Dental Caries:
1. Host factor:
- Tooth
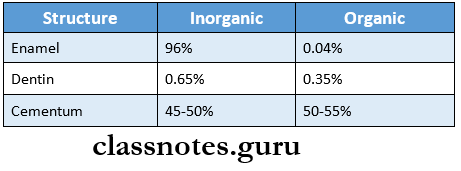
Composition:
Morphology:
- That predisposes to dental caries are deep, narrow, occlusal fissures, buccal & lingual pits
- Disturbed clarification
Position:
- Malaligned & rotated predispose to caries
Saliva:
- Removes bacteria & food debris through its flushing action
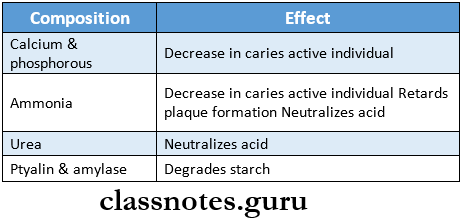
pH:
- Saliva is slightly acidic
- As the flow rate increases pH also increases
Viscosity:
- As viscosity increases caries activity increases
Sex:
- Caries are more common in females
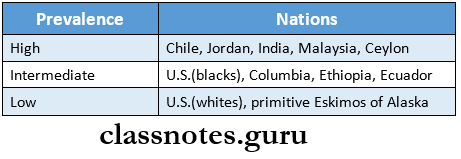
Race:
- Caries are more common in whites
Age:
- Root caries common in older individuals
- Familial hereditary
- Inheritance of a characteristic tooth structure
- Developmental disturbances
- The presence of deep pits and fissures, enamel hypoplasia and enamel defects more prone to caries
- Economic status
- In young individuals, caries decreases with an increase in income
- In adults, as income decreases, dental caries decreases
- Concomitant disease
- Fewer caries in controlled diabetes
- Oral hygiene habits
- Fewer caries in those who maintain good oral hygiene
2. Microflora:
- Streptococcus mutans are responsible for early carious lesions
- Lactobacilli are associated with dentinal caries and
- actinomyces strains with root surface caries
3. Local substrate diet:
- It depends on
- Physical Properties of Food and Cariogenicity
- Physical properties that improve the cleansing action reduce the retention of food within the oral cavity and increase saliva flow are caries-preventive
- Sucrose
- It is responsible for caries development
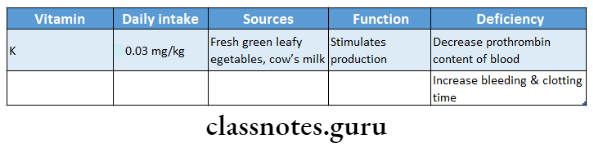
- Vitamin K
- Has the possible anticaries agent
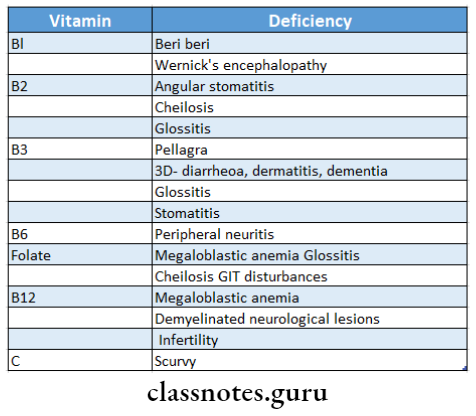
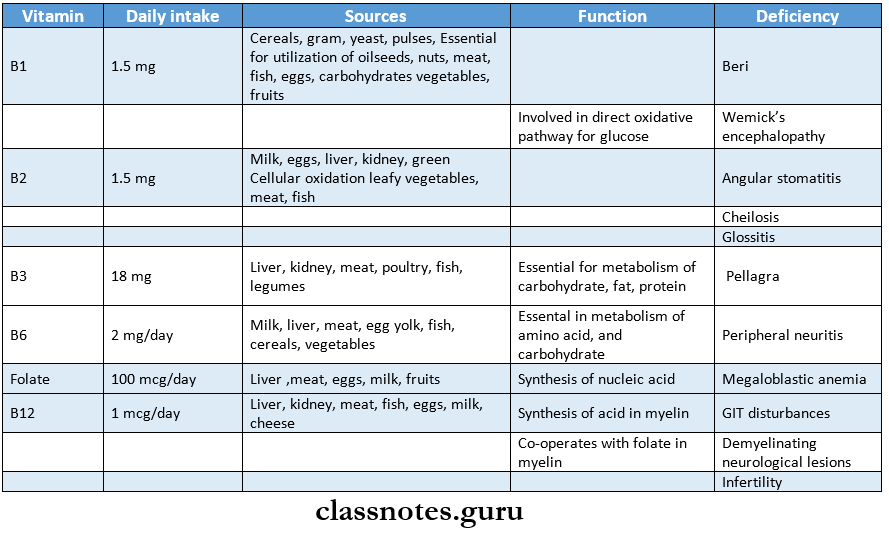
- Vitamin B complex
- Alters oral flora by promoting the growth of non-cariogenic organisms
- Calcium and phosphorous dietary intake
- Disturbance in calcium and phosphorous metabolism during the period of tooth formation may result in severe enamel hypoplasia and defects of the dentin
- Fluoride in diet
- Fluoride prevents dental caries
Oral Cancer Epidemiology
Epidemiology Of Oral Diseases Short Essays
Question 1. Role of tobacco in oral health.
Answer:
Role of tobacco in oral health
- Tobacco is a major contributor to oral disease
- Tobacco use
- Slows wound healing after dental surgery
- It promotes periodontal disease
- Halitosis
- Oral infections
- Causes cancer of the oral cavity & tongue, larynx, pharynx, oesophagus, stomach, lung
- Smokeless tobacco causes oral cancer
- Chewing of paan is a major cause of oral & oesophageal cancer
- Smoking is a known cause of cardiovascular disease
- Exposure to non-smokers causes respiratory disease, worsening of asthma
- Tuberculosis is more common in smokers
- Mortality increases
- Pregnant women exposed to passive smoking may deliver lower birth-weight babies
- Its consequence may be babies with cleft lip & palate
- Men who smoke or use smokeless tobacco may develop reduced fertility & sexual impotence
Question 2. Prevention of oral cancer.
Answer:
Prevention of oral cancer
- Prevention of oral cancer mainly focuses on modifying habits associated with the use of tobacco
- There are 3 well-known approaches
- Regulatory approach
- Print warning on cigarette packets
- In 2003, prohibition was made on advertisement of & to provide for the regulation of production, supply & distribution of cigarettes & other tobacco production
- Regulatory approach
- Service approach
- The active search for disease among apparently healthy people
- Educational approach
- Dentists help patients to quit tobacco by promoting tobacco prevention & control strategies
Counselling For Tobacco Cessation (5a’s):
- Ask:
- Ask the patient about tobacco use at every visit
- Advice
- Non-smokers to never use tobacco smokers to quit
- Assess
- The level of dependence
- Assist
- Quitting by setting a firm quit date
- Arrange
- For follow-up/recall visits
Use Of Pharmacotherapy:
- Nicotine replacement therapies
- Nicotine gum
- Nicotine patch
- Nicotine inhaler
- Nicotine nasal spray
- Nicotine lozenges
- Anti .depressants
- First line therapies
- Buproprion SR
- Selegiline
- Second line therapies
- Clonidine
- Nortriptyline
Counselling Those Unwilling To Quit (5r’s):
- Relevance of quitting
- Risks of continuing tobacco use
- Rewards of quitting
- Roadbacks to quitting
- Repeat these at each level
Common Oral Diseases And Prevention
Question 3. Oral submucous fibrosis.
Answer:
Oral submucous fibrosis
- Oral submucous fibrosis is a pre-cancerous condition
- Oral submucous fibrosis is characterized by juxta epithelial inflammatory reaction in the oral mucosa followed by a fibro elastic transformation of the lamina propria leading to mucosal atrophy, rigidity & trismus
Aetiology:
- Consumption of red chillies
- Consumption of areca nuts
- Nutritional deficiencies
- Immunological factors
- Genetic factors
Features:
- Burning sensation
- Difficulty in mastication
- Referred pain in the ear
- Depapillation of tongue
- Restricted movement of the floor of the mouth
- Shrunken uvula
- Fibrous bands
- Restricted mouth opening
- Stiffness of buccal mucosa
Management:
- Quit the habit
- Antioxidant- Oxyace-1 capsule/ day
- Multivitamin therapy
- Steroid- Betnovate 0.12%
- Tumeric application
- Intralesional injection of Hyaluronidase- 1500 U
- Physiotherapy
- Splitting of fibrous bands
- Laser
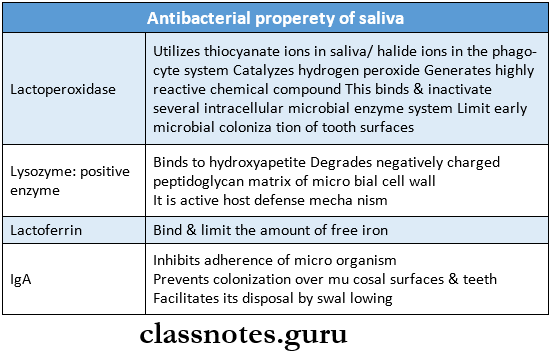
Question 4. Antibacterial property of saliva.
Answer:
Antibacterial properties of saliva
Epidemiology Of Oral Diseases Short Question And Answers
Question 1. Stephen’s curve.
Answer:
Stephen’s curve
- Stephan showed that within 2-4 minutes of rinsing with a solution of glucose/ sucrose, plaque pH is reduced from 6.5-5
- Stephen’s curve gradually returns to the original value within approximately 40 minutes
- Graphical presentation of it gives Stephan a curve
Epidemiology Of Oral Health
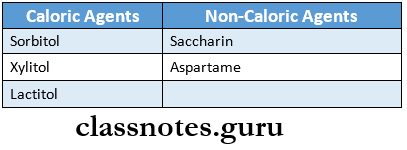
Question 2. Sugar substitutes.
Answer:
Sugar substitutes
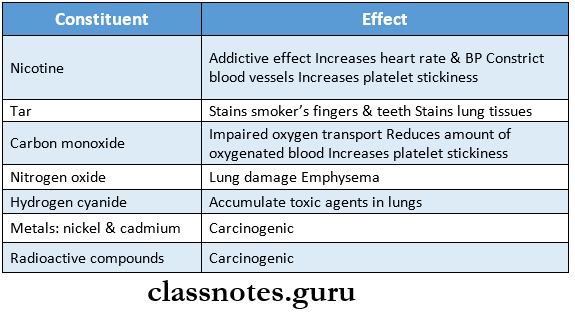
Question 3. Constituents of Cigarette smoke
Answer:
Constituents of Cigarette smoke
Question 4. Reverse smoking.
Answer:
Reverse smoking.
Cigarette
- Tobacco is smoked with a lighted end inside the mouth
- Air reaches the burning side through the unlighted end
- Smoke is expelled through the cigarette/ mouth
Chutta
- The smoker lights the chute
- Draws a few puffs conventionally
- Chutta is rarely taken out
Places
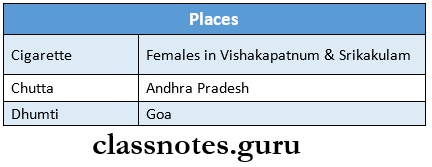
Side Effects:
- The temperature of the palatal mucosa increases to 58 degrees C
- Palatal patches exhibiting malignancy
Question 5. Smoking form of tobacco.
Answer:
Smoking form of tobacco
1. Bidis
- About 0.2-0.3 gms of sundried tobacco flakes are hand-rolled in a rectangular piece of tempura or tendu leaf and tied with a thread
2. Chillum
- It is a straight, 10-14 cm long conical clay pipe
3. Chutta
- It is a cylindrical coarsely prepared cheroot
4. Cigarettes
- About 1 gm of tobacco cured in the sun or artificial heat is covered with papers
5. Dhumti – conical carrots
- Hookah – water pipe
- Hookli
- Clay pipe of about 7-10 cm with mouthpiece and bowl
Risk Factors For Oral Diseases
Epidemiology Of Oral Diseases Viva Voce
- Miller proposed the chemical-parasitic theory of dental caries
- Clark observed a higher number of Streptococcus mu- tans are found at various site
- The two most important risk factors associated with oral cancer are tobacco and alcohol
- Hookah is also called water pipe or hubble-bubble
- No tobacco day is observed on 31st May.
- Anticancer drug busulfan is an alkylating agent
- Dhumti is used for reverse smoking in women
- Masheri is used to clean the teeth