Nerves Of Head And Neck Question And Answers
Question 1. Write a short note on ansa cervicalis or ansa hypoglossi.
Answer:
Ansa Cervicalis
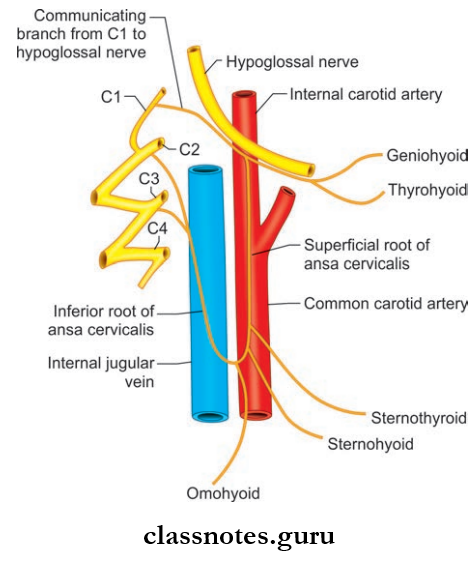
- U-shaped nerve loop present in carotid triangle embedded to the anterior wall of the carotid sheath
- Derived from vertebral rami of C1, C2, and C3 spinal nerves.
Ansa Cervicalis Or Ansa Hypoglossi Formation
- Superior Root (Descendants Hypoglossi)
- Continuation of descending branch of hypoglossal nerve whose fibers are derived from C1 spinal nerve
- It descends over the internal and common carotid artery.
- Inferior Root (Descendens Cervicalis)
- Derived from C2 and C3 spinal nerves
- It winds around the internal jugular vein and continues anteroinferior (takes a U-turn) to join the superior root in front of the common carotid artery.
Ansa Cervicalis Or Ansa Hypoglossi Distribution
- Supplies all infrahyoid muscle except thyrohyoid
- Throhyoid and geniohyoid are supplied by branches from C1 spinal nerve through the hypoglossal nerve
- Superior root supplies superior belly of omohyoid.
Ansa Cervicalis Or Ansa Hypoglossi Applied: In case of paralysis of recurrent laryngeal nerve as in complicated esophageal carcinoma, nerve transplantation is being done by using ansa cervicalis after resection of recurrent laryngeal nerve.
Mnemonics: Ansa cervicalis nerve supply:
Question 2. Write a short note on the cervical part of the sympathetic trunk.
Answer:
Cervical Part Of The Sympathetic Trunk
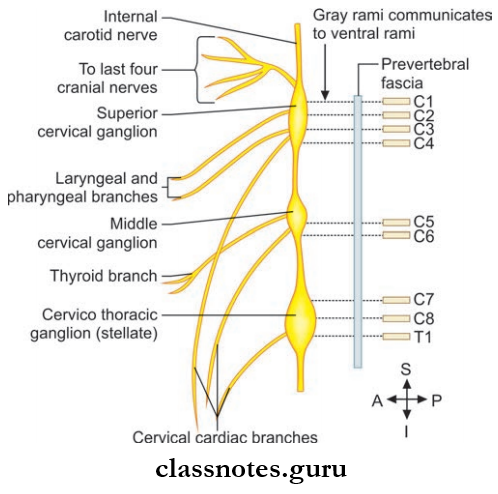
The cervical part of the sympathetic trunk is situated on each side of the vertebral column.
Sympathetic Trunk Formation: Formed by nerves that emerge from T1 to T4 segments of the spinal cord which ascends to the neck.
Sympathetic Trunk Relations
- Anterior
- Carotid sheath and contents
- Inferior thyroid artery.
- Posterior
- Prevertebral fascia
- Longus capitis and cervicis muscles
- Transverse process of C2–C7 vertebrae.
Ganglia: Due to the fusion of cervical nerves three ganglions are formed.
- Superior Cervical Ganglion
- Lies at the level of C2, and C3 vertebrae formed by fusion of upper four cervical connections
- It communicates with 9, 10, and 12 cranial nerves and with external and recurrent laryngeal nerve
- It gives internal carotid and external carotid branches to form plexus around them and also pharyngeal branches and superior cardiac branches to form pharyngeal and cardiac plexus respectively.
- Middle Cervical Ganglion
- Lies at the level of C6 vertebrae formed by fusion of 5th and 6th cervical ganglia connections
- It gives grey rami communicans to C5 and C6 ventral rami and branches to thyroid, parathyroid gland, trachea, and esophagus, and also gives branches to the cardiac plexus.
- Inferior Cervical Ganglion (Stellate Ganglion)
- Lies at the level of C7 vertebrae
- Formed by the fusion of 7th and 8th cervical ganglia connections
- It gives grey rami communicans to C7 and C8 ventral rami, branches to the vertebral artery and subclavian artery to form plexus around them
- It also give a cardiac branch to the deep cardiac plexus.
Sympathetic Trunk Applied
- The head and neck region is supplied by sympathetic fiers arising from upper four thoracic spinal segments.
- The preganglionic fibers pass though the stellate ganglion to relay in the superior cervical ganglion and the postganglionic fibers arise from the stellate ganglion and supply structures in the head and neck.
- An injury to the cervical part of the sympathetic trunk produces a clinical condition known as Horner’s syndrome.
- Horner’s Syndrome Is Characterized By The Following:
- Partial ptosis (drooping of upper eyelid) due to paralysis of smooth part levator palpebrae superioris.
- Miosis (constriction of pupil) due to paralysis of dilator pupillae
- Anhydrosis (loss of sweating on that side of face) due to vasomotor denervation
- Loss of ciliospinal reflux (pinching of the skin of neck produces dilation of pupil)
- Enophthalmos (sunken eyeball).
- Horner’s syndrome also can be caused due to lesion within the central nervous system anywhere at or above the 1st thoracic spinal segment.
Question 3. Write a short note on the cervical plexus.
Answer:
Cervical Plexus
Cervical Plexus Formation
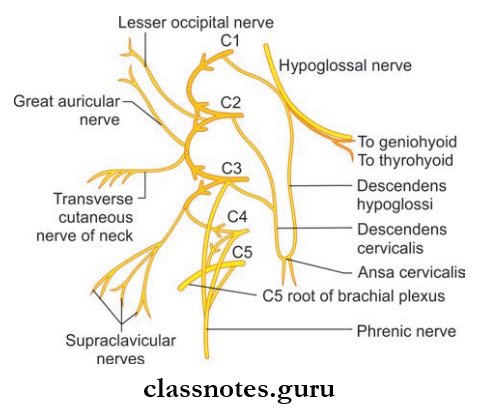
- Formed by ventral rami of upper four cervical nerves(C1–C4)
- The ventral rami of C2–C4 divide to form upper and lower branches
- The ventral ramus of C1 and branches of C2–C4 are connected with one another to form three loops
- The first loop is directed forwards in front of the transverse process of atlas and others two loops are directed backward.
Cervical Plexus Position And Relations
- Anteriorly
- Prevertebral fascia
- Internal jugular vein
- Sternocleidomastoid.
- Posteriorly
- Levator scapulae
- Scalenus medius.
Cervical Plexus Branches
- Superficial Branches
- Lesser occipital
- Greater auricular
- The transverse cutaneous nerve of neck
- Supraclavicular.
- Deep Branches
- Communicating Branches
- Grey rami from superior cervical ganglion to C1–C4 nerve roots
- Branch from C1 join the hypoglossal nerve and take part in ansa cervicalis
- Branch from C2 to sternocleidomastoid and branches from C3 and C4 to trapezius.
- Muscular Branches
- Muscles supplied only by the cervical plexus
- Rectus capitis anterior from C1
- Rectus capitis lateralis from C1 and C2
- Longus capitis from C1–C3
- Lower root of ansa cervicalis from C2, C3 to sternohyoid, sternothyroid, inferior belly of omohyoid.
- Muscles are supplied by cervical plexus along with the brachial plexus or spinal accessory.
- Sternocleidomastoid from C2 and spinal accessory
- Trapezius from C3, C4 and spinal accessory
- Levator scapulae from C3, C4 and C5
- Phrenic nerve from C3, C4, C5
- Longus colli C3–C8
- Scalenus medius C3–C8
- Scalenus anterior C4–C6
- Scalenus posterior C6–C8.
- Muscles supplied only by the cervical plexus
- Communicating Branches
Mnemonics: Branches of cervical plexus
‘GLAST’: Four compass points—clockwise from north on the right side of neck
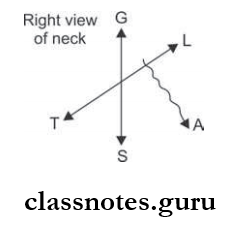
- Great auricular
- Lesser occipital
- Accessory nerve pops out between
- L and S
- Supraclavicular
- Transverse cervical.
Question 4. Write a short note on phrenic nerve.
Answer:
Phrenic Nerve
Mixed nerve-carrying motor fibers to the diaphragm and sensory fibers from pleura and pericardium, diaphragm, and peritoneum (some part).
Phrenic Nerve Origin: Arises chiefly from ventral rami of the C4 nerve and receives a contribution from C3 and C5 nerves.
Phrenic Nerve Course:
- Forms at the lateral border of scalenus anterior at the level of upper border of thyroid cartilage opposite to middle of the sternocleidomastoid
- Then it runs vertically downwards on the anterior surface of scalenus anterior (oblique, so the nerve appears crossing obliquely from lateral border to medial border)
- Then it runs downwards on the cervical pleura behind the brachiocephalic vein to enter thorax behind the fist costal cartilage.
Phrenic Nerve Distribution
- Phrenic Nerve provides sensory innervation to the diaphragm, pleura, pericardium, and subdiaphragmatic pleura.
- Phrenic Nerve provides motor supply to the diaphragm.
Phrenic Nerve Applied
- Accessory phrenic nerve is a branch from nerve to the subclavius having C5 fiers and lies lateral to the phrenic nerve and usually join the main nerve near 1st rib
- Pain arising from structures supplied by the phrenic nerve is referred regions supplied by spinal nerves C3–C5
- A subphrenic abscess beneath the right diaphragm can cause pain in the right shoulder
- Irritation of the phrenic nerve (or the tissues supplied by it) leads to the hiccup reflex. A hiccup is a spasmodic contraction of the diaphragm, which pulls air against the closed folds of the larynx.
Question 5. Write a short note on the greater occipital nerve.
Answer:
Greater Occipital Nerve
- Large medial branch of dorsal ramus of C2 nerve
- Thickest cutaneous nerve in the body.
Greater Occipital Nerve Course
- Winds around the middle of the lower border of inferior oblique muscle and passes upwards and medially
- Greater Occipital Nerve Course then crosses suboccipital triangle and pierces semispinalis capitis and trapezius.
Greater Occipital Nerve Areas Supplied: Semispinalis capitis and scalp.
Question 6. Write a short note on submandibular ganglion.
Answer:
Submandibular Ganglion
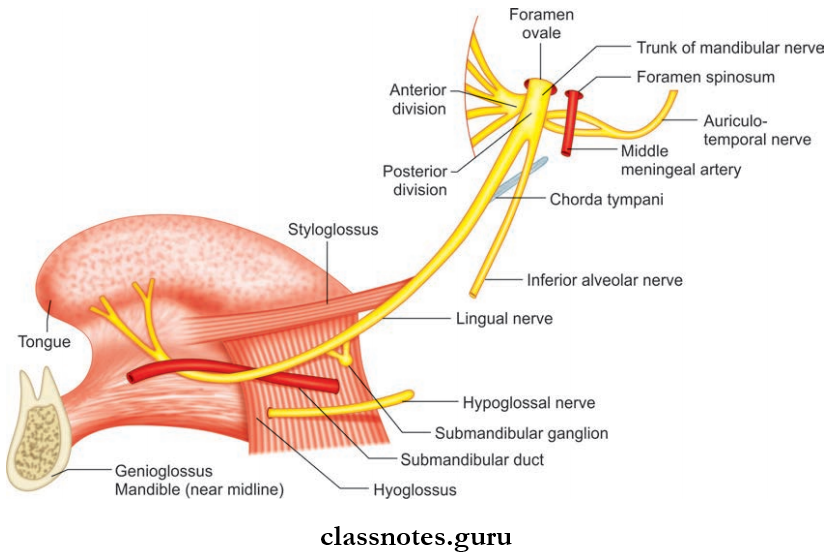
- Peripheral parasympathetic ganglion
- Relay station for secretomotor fiers to submandibular and sublingual glands
- Topographically it is related to lingual nerve but functionally connected to chorda tympani nerve.
Submandibular Ganglion Situation: Lies on the hyoglossus muscle just above deep part of submandibular gland.
Submandibular Ganglion Relation:
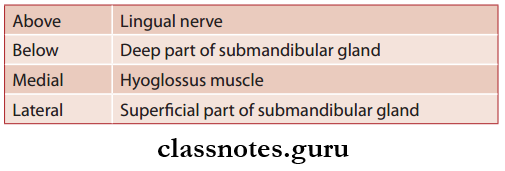
Submandibular Ganglion Connections
- Sensory fibers are through lingual nerve
- Sympathetic Fibers: Derived from the sympathetic plexus around facial artery and contain postganglionic fibers from the superior cervical ganglion
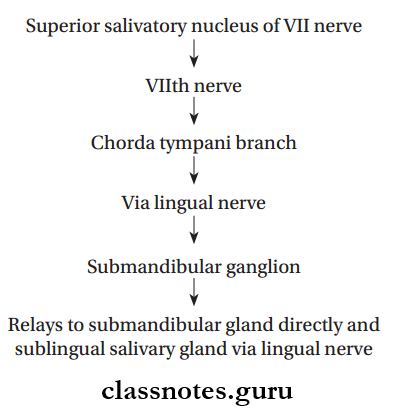
- Secretomotor Fibers: Though posterior root from lingual nerve and contain preganglionic fibers from the superior salivatory nucleus through nervus intermedius via chorda tympani and lingual nerve and relay in the ganglion.
Submandibular Ganglion Branches
- Six branches which supply submandibular gland
- Other fires join lingual nerve to supply the sublingual and anterior lingual nerve.
Submandibular Ganglion Secretomotor Fibers
Question 7. Write a short note on mandibular nerve.
Answer:
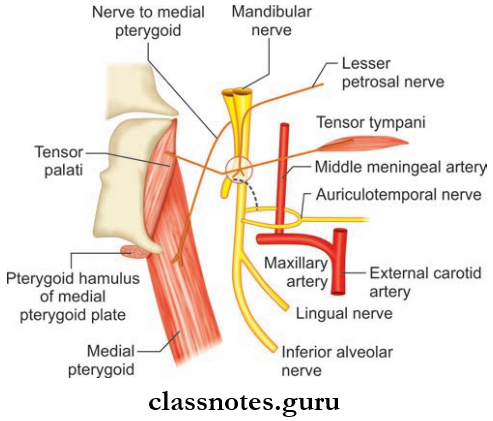
Mandibular Nerve
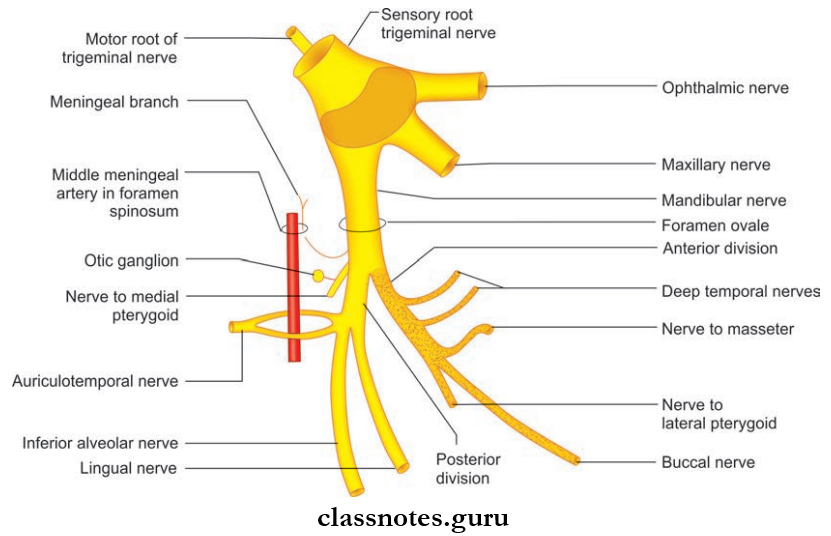
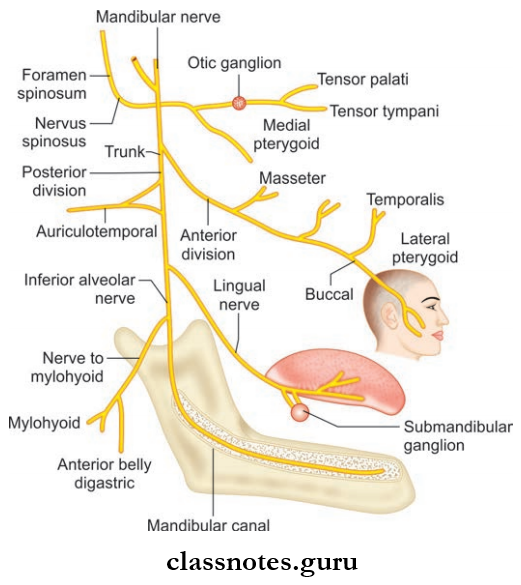
- Largest division of trigeminal nerve
- Mixed nerve having both sensory and motor fibers
- Nerve of fist pharyngeal arch and supply all structures derived from this arch.
Mandibular Nerve Course
- Mandibular Nerve Course begins in the middle cranial fossa from a large sensory root and a small motor root
- Sensory root arises from the lateral convex part of trigeminal ganglion whereas small motor root arises from the pons
- Both roots pass through the foramen ovale and join in the infratemporal fossa and form main trunk
- The trunk is short and soon divides to anterior (small) and posterior (large) division.
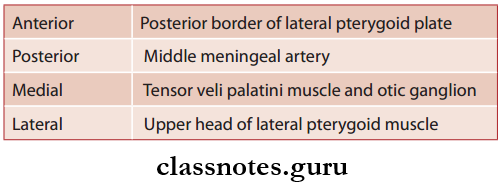
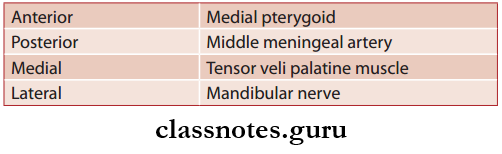
Relations In Infratemporal Fossa
Mandibular Nerve Branches
- From Main Trunk
- Nervus spinosus which supplies the dura of middle cranial fossa
- Nerve to medial pterygoid which supplies medial pterygoid, tensor veli palatine and tensor tympani muscles.
- From Anterior Division
- Masseteric nerve which supplies masseter and temporomandibular nerve
- Deep temporal nerve which supplies the temporalis muscle
- Nerve to lateral pterygoid which supplies lateral pterygoid muscle
- Buccal nerve which supplies the mucous membrane of the cheek and gum of lower jaw opposite to the molars and 2nd premolar.
- From The Posterior Division
- The auriculotemporal nerve which supplies skin of the tragus, upper part of the pinna external auditory meatus, temporomandibular joint, the skin of the temple, secretomotor fibers to the parotid gland
- The lingual nerve which supplies sensory supply to floor of mouth, lingual surface of the gum, anterior 2/3rd of tongue, carries secretomotor fibers to submandibular and sublingual glands
- Inferior alveolar nerve which supplies mylohyoid, nanterior belly of digastric, molar and premolar teeth, skin of chin and lower lip, canine and incisor teeth.
Question 8. Write a short note on the maxillary nerve.
Answer:
Maxillary Nerve
Arises from trigeminal ganglion.
Maxillary Nerve Course
- It then runs forwards in the lateral wall of cavernous sinus just below the ophthalmic nerve
- It then leaves the middle cranial fossa by passing through foramen rotundum and crosses upper part of the pterygopalatine fossa
- Then it passes straight in the upper part of the fossa and enter the orbit through the inferior orbital fissure and continues as the infraorbital nerve
- In the pterygopalatine fossa, it is related to pterygopalatine ganglion and gives ganglionic fibers, posterior superior alveolar nerves, and zygomatic nerves.
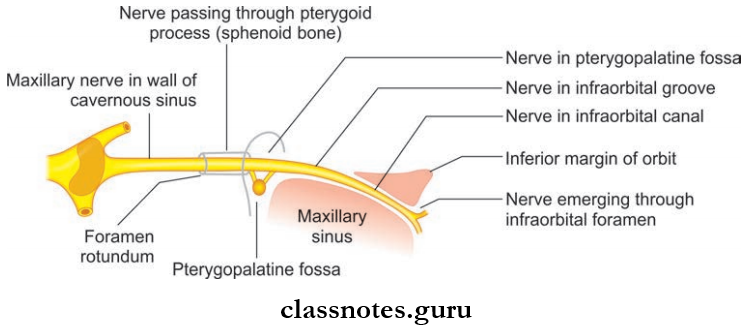
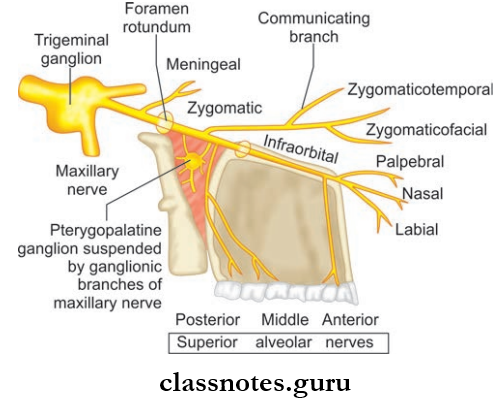
Zygomatic Nerve
- Enters orbit through inferior orbital fissure and enters zygomatic bone and divides to
- Zygomaticotemporal nerve
- Zygomaticofacial nerve.
- These supply skin of face and anterior part of the temple.
Posterior Superior Alveolar Nerve
- Posterior Superior Alveolar Nerve supplies the upper molar of the same side.
Infraorbital Nerve
- Continuation of the maxillary nerve
- Enters orbit through the inferior orbital foramen
- It has a common course in the orbit and then emerges on the face through the infraorbital foramen and divides into palpebral, nasal, and labial branches.
- Infraorbital Nerve Branches
- Middle superior alveolar nerve
- Anterior superior alveolar nerve
- Terminal branches
- Palpebral
- Nasal
- Labial.
Maxillary Nerve Branches
- In Middle Cranial Fossa
- The meningeal branch which supplies dura mater of the middle cranial fossa.
- In Pterygopalatine Fossa
- Ganglionic branches to pterygopalatine ganglion.
- Zygomatic nerve
- The zygomaticotemporal branch which supplies the skin of temple
- The zygomaticofacial branch which supplies skin of face.
- Posterior superior alveolar nerve.
- Supplies mucous membrane of the maxillary sinus, molar teeth, and adjoining part of gum.
- In The Orbit
- Middle superior alveolar nerve which supplies premolar teeth
- Anterior superior alveolar nerve supplies canine and incisor teeth, the mucous membrane of the lateral wall, and floor of nasal cavity.
- On Face
- Palpebral branch which supplies the skin of lower eyelid
- Nasal branch which supplies the skin of side of nose and mobile part of the nasal septum
- Superior labial branch which supplies the skin and mucous membrane of upper lip.
Question 9. Write a short note on optic ganglion.
Answer:
Optic Ganglion
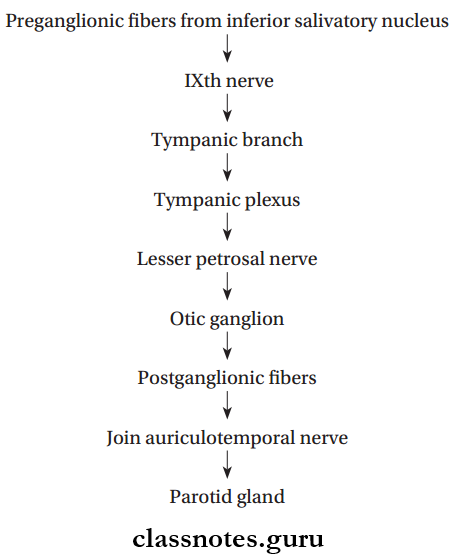
Peripheral parasympathetic ganglion which relays secretomotor fibers to the parotid gland.
Optic Ganglion Size And Situation
- 2–3 mm in size
- Situated in infratemporal fossa below foramen ovale
- Lies medial to mandibular nerve lateral to tensor veli palatine.
Optic Ganglion Relations
Optic Ganglion Connections And Branches
- Motor root is formed by lesser petrosal nerve
- The sympathetic root is derived from the plexus in the middle meningeal artery and contain postganglionic fibers arising in superior cervical ganglion and fiers pass without relay in the ganglion and reach parotid gland through the auriculotemporal nerve
- Sensory root is from the auriculotemporal nerve
- Other Fibers
- Nerve to medial pterygoid: Gives a motor root to ganglion and do not relay and supplies tensor veli palatini and tensor tympani muscles
- Chorda tympani nerve: Connected to otic ganglion and nerve of pterygoid canal and forms alternate taste pathway from anterior 2/3rd of tongue.
Secretomotor Fibers To Parotid Gland
Question 10. Write a short note on pterygopalatine ganglion.
Answer:
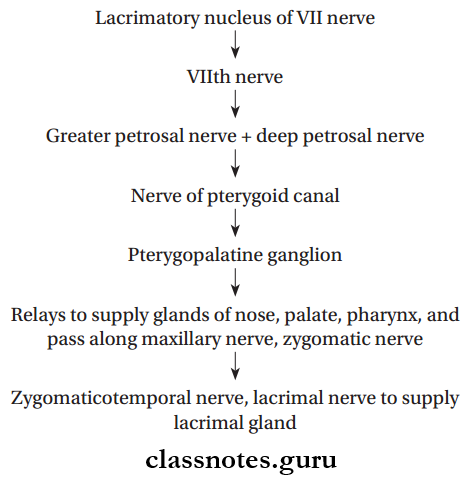
Pterygopalatine Ganglion
- Largest parasympathetic peripheral ganglion
- Act as a relay station for secretomotor fibers to the lacrimal gland and to the mucous gland of nose, paranasal sinuses, palate, and pharynx
- Topographically related to the maxillary nerve and functionally connected to the facial nerve through the greater petrosal branch.
Pterygopalatine Ganglion Location: Lies in the pterygopalatine fossa.
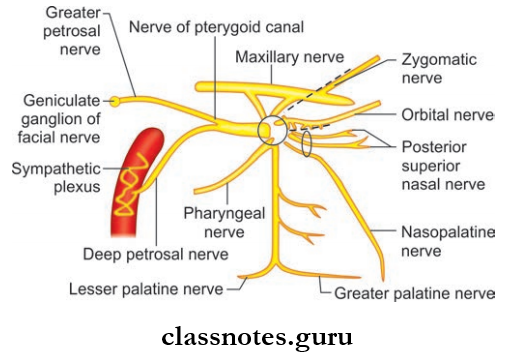
Pterygopalatine Ganglion Relations
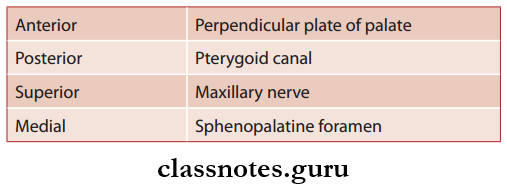
Pterygopalatine Ganglion Connections
- The sensory root arises from the maxillary nerves and fibers do not relay in the ganglion
- The fibers emerge as the branches of ganglion
- The sympathetic root is derived from sympathetic plexus around internal carotid artery through nerve of pterygoid canal and contains postganglionic fibers from the superior cervical sympathetic ganglion
- These fibers also do not rely in the ganglion and supply mucous membranes of nose, paranasal sinuses, nasopharynx, and palate
- The motor root is formed by nerve of the pterygoid canal and contains preganglionic fibers from neurons present near the superior salivatory nucleus and lacrimatory nucleus
- The fibers relay in the ganglion and postganglionic fibers supply secretomotor nerves to the lacrimal gland, mucous glands of nose, nasopharynx, paranasal sinuses, and palate.
Pterygopalatine Ganglion Branches
- These are actually branches of the maxillary nerve which forms the sensory root
- The Branches Include:
- Orbital Branches: These supplies the periosteum of orbit, orbitalis muscle, ethmoid sinus, and secretomotor fibers to lacrimal gland
- Palatine Branches: Th greater and lesser palatine nerve.
- The greater palatine nerve supplies hard palate and lateral wall of nose while lesser palatine nerve supplies the soft palate and tonsil.
- Nasal Branches: Supply posterior part of superior and middle conchae, roof of nose, nasal septum
- Pharyngeal Branches: Supply part of nasopharynx behind auditory tube
- Lacrimal Branches: Supply secretomotor fiers to lacrimal gland.
Secretomotor Fibers
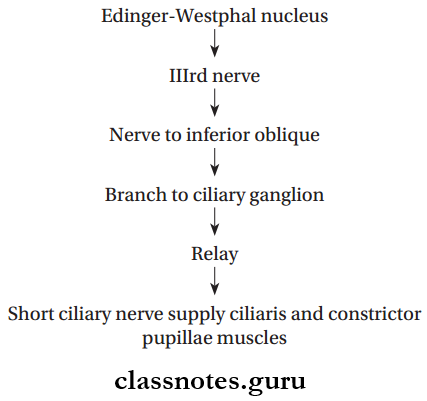
Question 11. Write a short note on ciliary ganglion.
Answer:
Ciliary Ganglion
- Ciliary Ganglion is a peripheral parasympathetic ganglion
- Topographically, it is connected to the nasociliary nerve which is branch of ophthalmic division of the trigeminal nerve but functionally it is connected to the oculomotor nerve.
Ciliary Ganglion Situation: It is a small structure measuring about 2 mm in diameter near the apex of orbit between the optic nerve and lateral rectus muscle.
Ciliary Ganglion Connections: Three roots enter the ganglion through the posterior end.
- Sensory root: Derived from nasociliary nerve and consist of sensory fibers from eyeball and do not relay here.
- Sympathetic root: Derived from the sympathetic plexus around the internal carotid artery and consist of postganglionic fibers from superior cervical ganglion and do not relay and pass through short ciliary nerve to supply dilator pupillae and blood vessels.
- Motor root: Derived from nerve to inferior oblique and contain preganglionic fibers from Edinger-Westphal nucleus and fiers relay here and postganglionic fibers pass through short ciliary nerve to supply ciliary muscle and sphincter pupillae.
Ciliary Ganglion Branches: Branches are short ciliary nerves about 8–10 in number.
Secretomotor Fibers
Question 12. Write a short note on the nasociliary nerve.
Answer:
Nasociliary Nerve
One of the terminal branches of the ophthalmic division of trigeminal nerve.
Nasociliary Nerve Course
- Begins in the lateral wall of anterior part of the cavernous sinus and enters orbit through middle part of superior orbital fissure
- Nasociliary Nerve Course cross the optic nerve lateral to medially and runs along medial wall of orbit between the medial rectus and superior oblique
- Nasociliary Nerve Course ends by dividing into infratrochlear and anterior ethmoidal nerves at the anterior ethmoidal foramen.
Nasociliary Nerve Branches
- Anterior ethmoidal nerve: Large terminal branch and supplies the nose and nasal septum
- Posterior ethmoidal nerve: Supply ethmoidal and sphenoidal air sinuses
- Infratrochlear nerve: Small terminal branch and supply conjunctiva, lacrimal sac and caruncle, medial end of eyelid, and upper half of external nose
- Long ciliary nerves: Supply cornea, iris, and ciliary body
- A communicating branch to the ciliary ganglion.
Question 13. Write a note on trigeminal ganglion.
Answer:
Trigeminal Ganglion
- Trigeminal Ganglion is the sensory ganglion of 5th cranial nerve
- Trigeminal Ganglion is semilunar in shape with convexity directed anterolaterally.
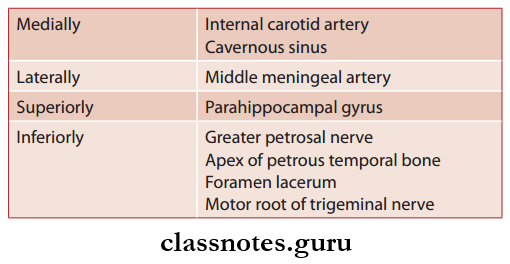
Trigeminal Ganglion Situation And Extent
- Trigeminal Ganglion lies in the impression on the anterior surface of petrous temporal bone near its apex
- Trigeminal Ganglion occupies a special space of Dura called Meckel’s cave.
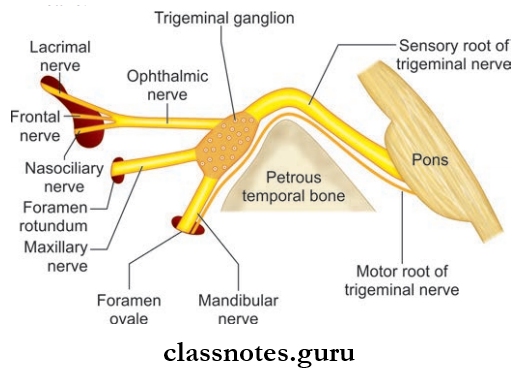
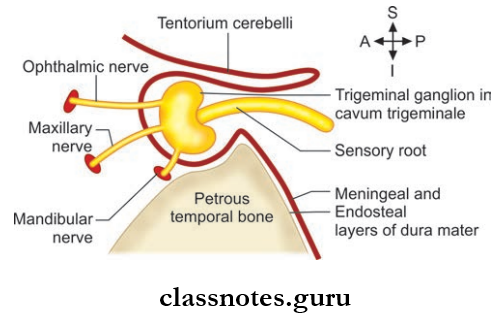
Trigeminal Ganglion Relations
Trigeminal Ganglion Roots And Branches
- The central process of the ganglion forms the large sensory root which is attached to the pons
- The peripheral processes of ganglion cells form the three divisions of the trigeminal nerve—ophthalmic, maxillary, and mandibular.
- The three divisions of trigeminal nerve originate from the convex distal surface of the ganglion.
- The small motor root is attached to pons superomedial to the sensory root.
Trigeminal Ganglion Blood Supply: Supplied by branches of internal carotid, middle meningeal, accessory meningeal and meningeal branch of ascending pharyngeal artery.
Trigeminal Ganglion Applied
- Trigeminal neuralgia is a paroxysmal severe pain of sudden onset and short duration in area of distribution of three divisions of trigeminal nerve
- The sensory root of the trigeminal nerve is cut in the
- Meckel’s cave in order to relieve the pain of trigeminal neuralgia.
Nerves Of Head And Neck Mulltiple Choice Question And Answers
Question 1. Select the incorrect statement about the inferior cervical ganglion:
- It is formed by the fusion of 7th and 8th cervical sympathetic ganglia
- It lies in front of transverse process of the C6 vertebra
- It is also called stellate ganglion
- It is connected to middle cervical sympathetic ganglia by ansa cervicalis
Answer: 2. It lies in front of the transverse process of the C6 vertebra
Question 2. Select the incorrect statement about the cervical plexus:
- It is formed of the ventral rami of C1 to C4 cervical spinal nerves
- It is called the plexus of loops
- It lies superfiial to prevertebral fascia
- Its superficial branches are cutaneous in nature
Answer: 3. It lies superficial to the prevertebral fascia
Question 3. A correct statement about the submandibular ganglion is:
- It is functionally related to the facial nerve
- It is situated on the inner surface of the hyoglossus muscle
- It lies above the lingual nerve
- It supplies preganglionic parasympathetic fibers to the submandibular gland
Answer: 1. It is functionally related to the facial nerve
Question 4. All of the following statements are true about the ansa cervicalis except:
- It is present in the region of the carotid triangle
- It is formed by the ventral rami of C1, C2, and C3 spinal nerves
- It supplies all the infrahyoid muscles
- It is embedded in the anterior wall of the carotid sheath
Answer: 3. It supplies all the infrahyoid muscles
Question 5. All of the following nerves derived from anterior division of the mandibular nerve are motor except:
- Masseteric nerve
- Buccal nerve
- Nerve to lateral pterygoid
- Deep temporal nerve
Answer: 2. Buccal nerve
