Viral Infections Of The Oral Cavity Important Notes
- Mumps
- It is an acute viral infection characterized by unilateral or bilateral swelling of the salivary glands
- It is caused by RNA virus
- Incubation period 14-18 days
- Transmitted through the respiratory route
- Complications
- Meningoencephalitis
- Orchitis
- Mastoiditis
- Encephalitis
- Nerve deafness
- Measles
- It is an acute, contagious, hepatotropic viral infection
- Characterized by fever, malaise, Koplik’s spots, cough, maculopapular rash
- Koplik spots are prodromal and disappear after the onset of the rash
- They usually occur on the buccal mucosa as small, irregular bluish-white flecks surrounded by a red margin
- Histologically it shows multinucleated giant cells
- Chickenpox
- It is caused by the Varicella zoster virus
- It rarely occurs second time
- It is an extremely contagious disease usually occurring in children
- Characterized by exanthematous vesicular rashes
- It Is common in the winter and spring months
- the incubation period is 14-21 days
- Maculopapular or vascular eruptions begin on the trunk and spread to involve the face and extremities
- Occasionally secondary infection of the vesicles results in the formation of pustules which may leave small pitting scars upon healing
- AIDS
- Caused by Human Immunodeficiency Virus
- Mode of transmission
- Sexual
- Blood and blood products
- Injected drug users
- Occupational transmission
- Maternal-fetal transmission
- Other – via saliva, milk, and tears
- Oral manifestations
- Candidiasis
- Erythematous
- Hyperplastic
- Pseudomembranous
- Oesophageal
- Herpes Simplex infection
- Herpes Zoster infection
Hairy leukoplakia - Kaposi’s sarcoma
- Angular cheilitis HIV-gingivitis HIV – HIV-periodontitis Necrotizing ulcerative gingivitis Necrotizing stomatitis
- Major aphthae
- Vesiculobullous lesion
- Parotitis
- Toxoplasmosis
- Purpura
- Osteomyelitis
- Diagnosis
- Western blot
- ELISA
- PCR
- Reverse ratio of T helper to T suppressor
- Detection of antibodies in serum
- Detection of virus
- Lymphopenia
- Hypergammaglobulinaemia
- Diagnosis
- Treatment
- Nucleoside reverse transcriptase inhibitor
- Nonnucleoside reverse transcriptase inhibitor
- Protease inhibitor
Viral Infections Of The Oral Cavity Long Essays
Question 1. Enumerate various viral infections affecting the oral cavity, write in detail about clinical features and oral manifestations of herpes simplex virus
Answer:
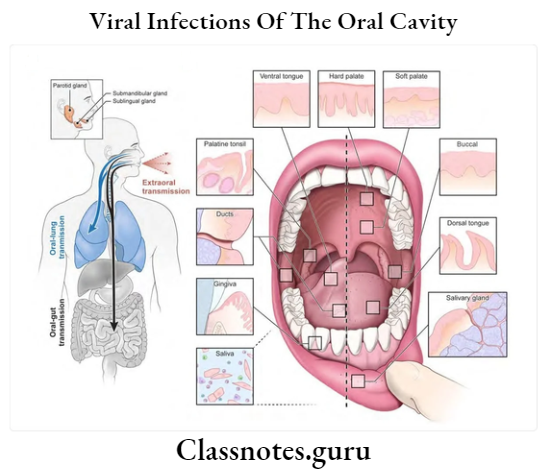
Viral Infections Affecting Oral Cavity:
- RNA Viruses
- Orthomyxovirus
- Influenza
- Paramyxovirus
- Measles
- Mumps
- Rhabdovirus
- Rabies
- Arenavirus
- Lassa fever
- Lymphocytic choriomeningitis
- Calicivirus
- Coronavirus
- Upper respiratory tract infection
- Bunyavirus
- Picornavirus
- Reovirus
- Retrovirus
- Orthomyxovirus
- DNA Viruses
- Herpes virus
- Herpes simplex virus 1 and 2
- Varicella zoster virus
- Cytomegalovirus
- Epstein-Barr virus
- Poxvirus
- Smallpox
- Molluscum contagiosum
- Adenovirus
- Pharyngoconjunctival fever
- Papovavirus
- Human warts or papillomas
- Herpes virus
Read And Learn More: Oral Pathology Questions and Answers
Herpes Simplex Virus:
- Herpes simplex is a DNA virus causing disease in man
Herpes Simplex Virus Types:
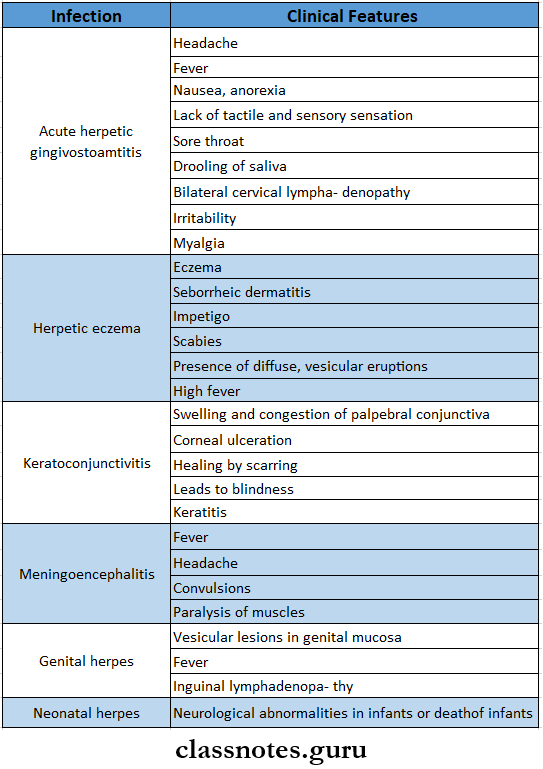
- Herpes simplex virus type-1
- Acute herpetic gingivostomatitis
- Herpetic eczema
- Keratoconjunctivitis
- Meningoencephalitis
- Herpes labialis
- Herpes simplex virus type-2
- Genital herpes
- Neonatal herpes
- Uterocervical cancer
- Oral herpes
Herpes Simplex Virus Clinical Features:
Herpes Simplex Virus Oral Manifestations:
- Site involved
- Gingiva
- Hard palate
- Dorsum of tongue
- Lips
- Vermillion border
- Perioral skin
- Nasopharynx
- Reddening of oral mucosa
- Formation of numerous small, dome-shaped, or pinhead-type vesicle
- Size-2-3 mm in diameter
- Vesicles contain clear fluid and rupture to form ulcers
- Ulcers are multiple, small, circular, punctuate, shallow, and painful
- Have red margins and yellowish or greyish floor
- Small ulcers fuse to form diffuse, large, whitish ulcers
- They are surrounded by a red halo
- Gingival margins are red, swollen, and painful and have punched-out erosions
- Difficulty in taking food
- Difficulty in mastication
- Difficulty in swallowing
- Numerous vesicle formations over the tonsillar area and posterior pharynx
Question 2. Describe in detail histological features, and lab investigations of primary herpetic gingivostomatitis
Answer:
Primary Herpetic Gingivostomatitis:
- Primary Herpetic Gingivostomatitis is an acute infection of the oral cavity caused by the herpes simplex type-I virus
Primary Herpetic Gingivostomatitis Histological Features:
- Formation of sharply defined vesicles in the superficial part of keratinized epithelium
- Ballooning degeneration of prickle cells with intranuclear inclusion body and marginated chromatin
- Presence of multiple multinucleated giant cells
Primary Herpetic Gingivostomatitis Lab Investigations:
- Cytologic smear
- The presence of inclusion bodies and ballooning degeneration of infected cells
- Culture
- Produces change In culture cells
- Serology
- Detects HSV-specific antibodies
Viral Infections Of The Oral Cavity Short Essays
Question 1. Herpangina
Answer:
Herpangina Clinical Features:
- Age- young age
- Incubation period-2-10 days
- Site- Posterior pharynx, tonsil, faucial pillars, and- soft palate
Herpangina Prodromal Symptoms:
- Fever, chills
- Headache
- Anorexia, vomiting
- Abdominal pain
- Sore throat
- Dysphagia
- Laceration
- The lesion initially appears as a punctuate macule
- This turns into papules and vesicles
- Within 24-48 hours, vesicles rupture to form a 1-2 mm ulcer
- They show a grey base
- They generally heal without treatment
Herpangina Differential Diagnosis:
- Primary herpes simplex infection
- Herpes zoster
Herpangina Treatment:
- Palliative treatment is done
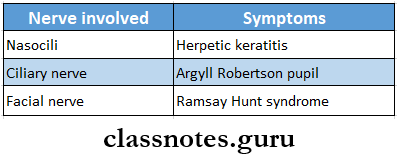
Question 2. Herpes zoster
Answer:
Herpes Zoster
- Herpes Zoster is a recurrent regional infection caused by the Herpes Zoster virus
Herpes Zoster Clinical Features:
- Age- 5th, 6th and 7th decade of life
- Prodromal symptoms
- Fever, malaise
- Headache
- Painful lymphadenopathy
- Severe pain, irritation or burning sensation develops in the dermatome of the involved nerve
- Affects the first branch of the trigeminal nerve
- Later symptoms
- Intense pain
- Formation of clusters of vesicles over skin and oral mucosa unilaterally
- Vesicles develop over buccal mucosa, soft palate, and tongue
- Causes stinging pain, paraesthesia, and severe stomatitis
- Vesicles rupture to form crateriform ulcers
- Ulcers heal without scar formation
- Stimulates toothache
Herpes Zoster Histopathology:
- Presents as swelling of infected epithelial cell cytoplasm called ballooning degeneration
- Margination of nuclear chromatin
- Formation of intranuclear inclusion bodies
- Reticular degeneration of epithelial cells
- The presence of multinucleated giant cells and polymorphonuclear neutrophilic infiltration in connective tissue
Question 3. Lipschutz bodies
Answer:
Lipschutz Bodies
- Lipschutz bodies are characteristic histologic features seen in primary herpetic stomatitis
- It is intranuclear inclusion present in herpetic vesicle
- These are eosinophilic, ovoid homogenous structures within the nucleus that tend to displace the nucleolus and nuclear chromatin peripherally
- This displacement of chromatin produces a perinuclear halo
Question 4. Oral manifestations of AIDS
Answer:
Oral Manifestations Of AIDS
- Bacterial infections
- Tuberculosis
- M. avium complex
- Salmonellosis
- Viral infection
- Herpes simplex
- Varicella zoster
- Epstein Barr virus
- Mycotic infections
- Pneumocystis pneumonia
- Candidiasis
- Aspergillosis
- Cryptococcosis
- Parasitic infection
- Toxoplasmosis
- Cryptosporidiosis
- Malignancies
- Kaposi’s sarcoma
- B cell lymphoma
Question 5. Measles
Answer:
Measles Clinical Features:
- Insidious in onset
- Moderate fever
- Tachycardia
- Sore throat
- Formation of greyish-greenish pseudomembrane on tonsils
- Associated nausea and vomiting
- Bull neck- swollen neck
- Tender lymphadenopathy
- Nasal infection
- Hoarseness of voice
- Cough
- Respiratory obstruction
- Toxaemia
- Acute peripheral circulatory failure
- Nerve paralysis
- Dysphagia
- Dysphonia
- Paraesthesia
Question 6. Reiter’s syndrome
Answer:
Reiter’s Syndrome
- Reiter’s Syndrome consists of a triad of non-gonococcal urethritis, arthritis, and conjunctivitis
Reiter’s Syndrome Clinical Features:
- Genital lesions
- Balanitis circinata over glans penis
- Genital ulcers
- Oral lesions
- Seen over buccal mucosa, palate, and gingiva
- Present as painless, aphthous-like ulcers
- Geographic tongue
- The presence of few elevated areas of erythema on oral mucosa
- Pruritic spots on the palate
- Skin lesions
- Well-circumscribed erythematous erosions with irregular white border
Question 7. Infectious mononucleosis
Answer:
Infectious Mononucleosis
- Infectious Mononucleosis is a benign acute infectious disease caused by to Epstein-Barr virus affecting B-lymphocytes
Infectious Mononucleosis Clinical Features:
- Incubation period-10-40 days
- Age-young age individuals
- Sore throat
- Fever-101-103 degrees – F
- Headache
- Photophobia
- Nausea, vomiting, diarrhea
- Erythematous macular rash
- Splenomegaly, hepatomegaly
- Lymphadenopathy
- Myalgia, arthralgia
- Depression and cognitive defect
Infectious Mononucleosis Oral Manifestations:
- Petechiae over soft palate
- Ulcerative gingivitis, periodontitis
- Stomatitis
- Inflamed and enlarged tonsils
- Tonsils are covered by pseudomembrane
- Sore throat
- Dysphagia
- Bleeding from the oro-nasopharyngeal region and gingiva
Infectious Mononucleosis Complications:
- Airway obstruction
- Splenic rupture
- Neurological involvement
- Hemolytic anemia
Question 8. Herpes labialis
Answer:
Herpes Labialis
- Herpes Labialis occurs in patients with no prior infection with Herpes Simplex Virus-1
Herpes Labialis Clinical Features:
- Age- children and young adults
- Incubation period-5-7 days
- Prodromal generalized symptoms
- Fever
- Malaise
- Headache
- Nausea, vomiting
- Painful mouth
- Sore throat
- Irritability
- Excessive drooling of saliva
- Lack of tactile sensation
- Cervical lymphadenopathy
- Later symptoms
- Numerous vesicle formations over keratinized mucosa
- Vesicles are thin-walled
- They contain clear fluid
- They rupture leaving multiple, small, punctuate shallow painful ulcers of 2-6 mm
- Ulcers are surrounded by a red ring of inflammation
- Ulcers may become secondarily infected
- Healing starts in about 3 days and is completed within 7-14 days
Herpes Labialis Treatment:
- To prevent secondary infection- antibiotics are used
- To control fever- Antipyretics are given
Question 9. Ramsay Hunt syndrome
Answer:
Ramsay Hunt Syndrome
- Ramsay Hunt is a zoster infection of the geniculate ganglion with involvement of external ear and oral mucosa
Ramsay Hunt Syndrome Features:
- Facial paralysis
- The pain of the external auditory meatus and pinna of the ear
- Vesicular eruption in oral cavity and oropharynx
- Hoarseness of voice
- Tinnitus
- Vertigo
Question 10. Chickenpox
Answer:
Chickenpox
- Chickenpox is caused by Varicella zoster virus
- Chickenpox seldom occurs a second time
- The virus enters the mucosa of the upper respiratory tract and spreads by droplets from the throat
Chickenpox Clinical Features:
- It involves young children and adults
- The incubation period is 14-21 days
- Malaise
- Low-grade fever followed by a rash
- Rash is maculopapular
- Heals by scabs formation
- Sites Involved:
- Skin lesions- over trunk and face then spread to peripheral parts of the body
- Mucosal lesions- affects the mucosa of the pharynx and vagina
Chickenpox Complications:
- Superinfection of skin due to frequent scratching
- Encephalitis
- Cerebellar ataxia
- Myocarditis
- Osteomyelitis
- Septic arthritis
- Septicaemia
- Hepatitis
- Pneumonia
Question 11. Rubella
Answer:
Rubella
- Rubella is a mild childhood disease
- Rubella may be acquired, congenital, or postnatally
Rubella Features:
- Infection is acquired by inhalation
- Incubation period-2-3 weeks
- Fever, malaise
- Headache
- Mild conjunctivitis
- Lymphadenopathy
- Rash develops on the forehead and face
- It spreads downward to the trunk and extremities
- It lasts for 1-5 days
Rubella Prevention: It is prevented by MMR vaccine
Question 12. Koplik’s spots
Answer:
Koplik’s Spots
- Koplik’s spot is an important clinical feature of measles
- Appears over buccal mucosa
- The mucosa becomes inflamed
- They appear as small, irregularly shaped flecks surrounded by a bright red margin
- Over it, there is the presence of white or white-yellow pinpoint papules
- Koplik’s Spots is followed by red maculopapular rashes on the skin
Question 13. Behcet’s syndrome
Answer:
Koplik’s Spots
- Koplik’s Spots is a triad of recurring oral ulcers, recurring genital ulcers, and eye lesions
Behcet’s Syndrome Clinical Features:
- Genital lesions
- Consist of recurrent aphthae
- Larger than mucosal lesions
- Site
- In males- penis, inner thigh, scrotum
- In females- vulva
- It is painful in females
- Healing of these lesions leads to severe scarring
- Oral lesions
- Recurrent aphthae ulcers develop
- Size- varies from several mm to cm
- They are painful lesions
- They have erythematous borders and are covered by exudate
- Can occur anywhere in the oral mucosa
- Eye lesions
- Initially, ocular lesions develop
- Consist of conjunctivitis, keratitis, uveitis, optic trophy and, and retinal this may
- May lead to visual damage and eventually blindness
- Photophobia
- Other features
- Skin lesions- Small pustules or papules develop on the trunk or limbs
- Neurological degeneration
- Intestinal ulceration
- Arthralgia
- Visceral involvement
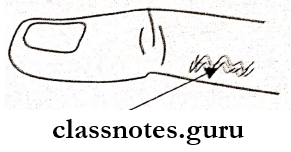
Question 14. Herpetic whitlow
Answer:
Herpetic whitlow
- Herpetic whitlow is caused by Herpes Simplex Virus
- Herpetic whitlow is the infection of the finger by a virus through the break in the skin
- Dentists may experience it through contact with lesions of the mouth or saliva of patients who are asymptomatic carriers of HSV
- The lesions are usually preceded by prodromal symptoms of burning or tingling sensation
Viral Infections Of The Oral Cavity Viva Voce
- Infectious mononucleosis is caused in the oral cavity by Ebstein-Burr most common malignancy in AIDS is Kaposi’s sarcoma
- Lipschutz bodies is seen in primary herpetic stomatitis
- Herpes simplex virus causes oral ulcerations in immunocompromised patients
- Herpes virus shows prodromal symptoms preceding local lesions
- Reiter’s syndrome is a triad of non-gonococcal urethritis, arthritis, and conjunctivitis
- Ramsay Hunt syndrome is a zoster infection of the geniculate ganglion with involvement of external ear and oral mucosa
- Behcet’s syndrome is a triad of recurring oral ulcers, recurring genital ulcers, and eye lesions
- Koplik’s spot is an important clinical feature of measles
- Ballooning degeneration is seen in herpes zoster infection.
