Tumour Cyst And Neck Swelling Long Essays
Question 1. Describe the various types of cysts of mandible and discuss in detail about their management.
Answer:
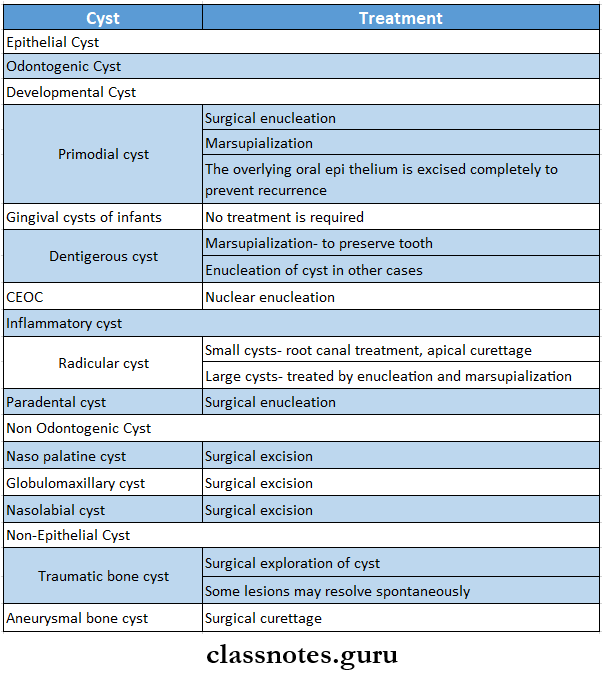
Types Of Cysts Of Mandible Classification:
Epithelial Cyst:
- Odontogenic Cysts
- Developmental cysts
- Primordial cyst
- Gingival cysts of infants
- Dentigerous cyst
- CEOC
- Inflammatory cysts
- Radicular cyst
- Residual cyst
- Paradental cyst
- Developmental cysts
- Nonodontogenic Cysts
- Naso palatine cyst
- Globulomaxillary cyst
- Nasolabial cyst
Non-Epithelial Cyst:
- Simple bone cyst
- Traumatic bone cyst
- Solitary bone cyst
- Aneurysmal bone cyst
Read And Learn More: General Surgery Question and Answers
Tumour cyst and neck swelling Q&A
Question 2. Describe clinical features, diagnosis, and management of the tumor of the maxilla.
Answer:
Tumour Of Maxilla: Tumour of Maxilla is a relatively uncommon, well-circumscribed, odontogenic neoplasm characterized by the formation of multiple duct-like structures by the neoplastic epithelial cells
Tumour Of Maxilla Clinical Features:
- Age- common in young age
- Sex: females are commonly affected
- Site- commonly occurs in the maxillary anterior region
- It is slow enlarging tumour
- Small, bony hard swelling is present in the maxillary anterior region
- Causes elevation of the upper lip on the involved side
- Displacement of regional teeth
- Mild pain and expansion of the cortical plates
- Severe expansion of bone in severe cases
- Associated with unerupted teeth
- It also has extra osseous involvement in the anterior maxillary gingiva
- Produces solitary painless, asymptomatic nodular swelling on the gingiva
Tumour Of Maxilla Diagnosis:
- Clinically- slow enlarging bony hard swelling present in the maxillary anterior region
- Radiographically
- Shows well-circumscribed, unilocular, radiolucent area with few small radiopaque foci
- Microscopically
- Spindle-shaped, neoplastic odontogenic epithelial cells appears to proliferate in multiple duct-like patterns
- These ducts are lined by tall columnar cells
- The central lumen is filled with eosinophilic coagulum
Tumour Of Maxilla Management
- Tumour Of Maxilla is treated by surgical enucleation
- The associated tooth is removed
Question 3. What are the different types of haemangiomas? Describe the treatment of each type.
Answer:
Haemangioma is a developmental malformation of blood vessels
Haemangioma Types:
- Capillary haemangioma
- Arises from capillaries
- Mainly there are three varieties of it
- Strawberry angioma
- Port wine stain
- Salmon patch
- Management:
- Most of the lesions disappears on its own
- If it persists following measures are undertaken
- Excision of the lesion with skin grafting
- Carbon dioxide snow application
- Injection of hot water or hypertonic saline
- Radiotherapy
- Injection of steroid
- Venous Haemangioma:
- Also called cavernous haemangioma
- Arises from veins
- Venous Haemangioma consists of multiple dilated venous channels
- Venous Haemangioma is a spongy swelling
- Management:
- Conservative treatment
- Injection of sclerosing agent
- Cautery
- Surgery
- Ligation of feeding vessels
- Excision of the esion
- Diathermy to control hemorrhage
- Conservative treatment
- Arterial Haemangioma:
- Also called plexiform haemangioma
- Arises from arteries
- It is a type of congenital arteriovenous fistula
- There is pulsatile swelling of arteries and the veins become arterialized
- Management:
- Ligation of feeding vessels
- Therapeutic embolization of the feeding arteries
- Excision of lesion with diathermy
- Management:
Question 4. Describe the methods of spread of carcinoma, grading, and staging of carcinoma in general.
Answer:
Spread of Tumours: Spread of Tumours is by 2 ways.
- Local Invasion/Direct Spread:
- Benign Tumors:
- Form encapsulated/circumscribed masses
- These expand and push aside the surrounding normal tissues without actually invading, infiltrating/metastasizing.
- Malignant tumours: They also enlarge by expansion.
- These tumours invade via the route of least resistance
- Often cancers extend through tissue spaces, via lymphatics, blood vessels, and perineural spaces and may penetrate bone.
- More commonly, tumours invade thin-walled capillaries and veins than thick-walled arteries.
- Benign Tumors:
- Metastasis/Distant Spread:
- Metastasis is defined as spread of tumor by invasion in such a way that discontinuous secondary tumour mass/masses are formed at the site of lodgement.
- Benign tumours do not metastasise while all malignant tumours with a few exceptions like gliomas of the CNS and basal cell carcinoma of skin can metastasize.
Routes Of Metastasis:
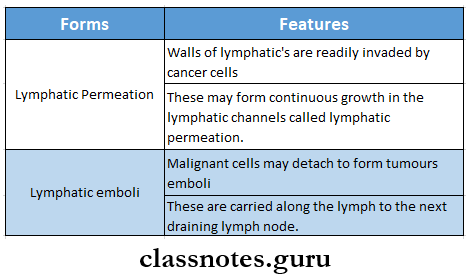
1. Lymphatic Spread: In general, carcinomas metastasise by lymphatic route
- The involvement of lymph nodes by malignant cells may be of two forms.
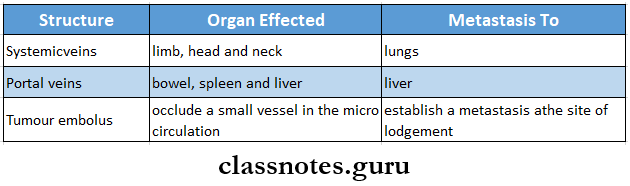
2. Haemategenous Spread:
- Sarcomas spread through hematogenous spread
- Common site for blood borne metastasis are
- Lung,
- Breast,
- Thyroid,
- Kidney,
- Liver
- Prostrate and
- Ovary.
- spread
3. Various Other Routes:
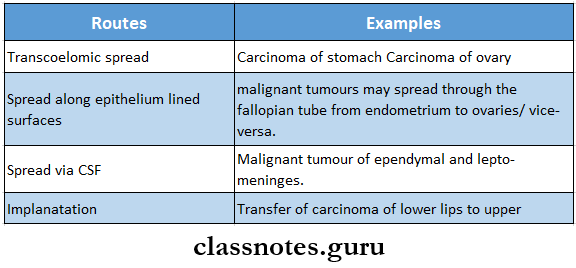
- TNM STAGING:
- T- size of tumour
- N- lymph node involvement
- M- distant metastasis
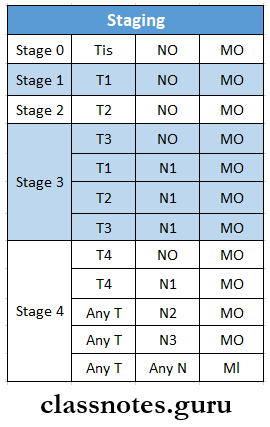
- T0- No tumour present
- Tis- Carcinoma in situ
- T1 – Tumour 2 cm or less
- T2- Tumour between 2-4 cm
- T3- Tumour more than 4 cm
- T4- Tumour invading adjacent structures
- NO- No node involvement
- Nl- ipsilateral lymph node involvement of 3 cm or less
- N2- ipsilateral lymph node involvement of more than 3 cm or less than 6 cm
- N3- Contralateral node involvement
- MO- no metastasis
- Ml- metastasis present
Questions on neck swellings and tumors
Question 5. What are the epidermal malignant lesions of skin? Describe the clinical features and outline management of squamous cell cacinoma What are the premalignant conditions of the skin?
Answer:
Epidermal Malignant Lesions Of Skin?
- Epidermal malignant lesions of skin are
- Basal cell carcinoma
- Squamous cell carcinoma
- Verrucous carcinoma
- Malignant melanoma
- Spindle cell carcinoma
- Primary intra-alveolar carcinoma
Squamous Cell Carcinoma:
Squamous Cell Carcinoma is the most common epidermal malignant neoplasm derived from the stratified squamous epithelium
Squamous Cell Carcinoma Clinical Features:
- Age: common in old age
- Sex: Common in males
- Sites involved are:
- Lower lip
- Lateral border of tongue
- Floor of the mouth
- Soft palate
- Gingiva or alveolar ridge
- Buccal mucosa
- Associated with oral leukoplakia and erythroplakia
- Initial Symptoms Are
- Asymptomatic
- White or red, varigated patch
- Nodule or fissure over oral mucosa
- Painless
- Later Symptoms
- Fast enlarging
- Exophytic or invasive ulcer
- Persistent induration around periphery
- Presence of superadded candidal infections
- Painful lesions due to secondary infections
- Fixation to the underlying tissues
- Trismus
- Invasion of the alveolar bone
- Enlarged regional lymph nodes
- Pathological fractures of the jaw bone
Squamous Cell Carcinoma Management:
- Surgical excision
- Radiotherapy
- Chemotherapy
Premalignant Conditions:
- Premalignant Conditions is defined as the generalized state of the body which is associated with a significantly increased risk of cancer
- They are
- Oral submucous fibrosis
- Sideropenic dysphagia
- Syphilis
- Oral lichen planus
Question 6. Discuss in detail about etiology, pathology, clinical features, investigations, and management of basal cell carcinoma.
Answer:
Basal cell carcinoma
- Also called as rodent ulcer. Most common tumor.
- Basal cell carcinoma is locally invasive, slow-growing tumor of middle-aged individuals which rarely metastasizes.
Basal Cell Carcinoma Etiology:
- Prolonged exposure to strong sunlight
- UV rays
- Arsenic used in skin ointments.
- Dysregulation of PTCH pathway.
- Inherited effects of PTCH gene causing BCC, Gorlin syndrome.
Basal Cell Carcinoma Pathology:
- It is characterized by neoplastic proliferation of basaloid epithelial cells in the form of multiple solid islands or strands
- These cells arises from the basal cell layer of the epidermis
- Cells in the periphery are columnar in shape
- Central cells may be polyhedral, oval, round, or even spindle-shaped
- Fibrous connective tissue contains large number of elastic fibres
Basal Cell Carcinoma Clinical Features:
- Majority of lesions occur on the face, usually above a line joining lobe of the ear and the angle of the mouth.
- Common sites are inner and outer canthus of the eye, the eyelids bridge of the nose, and around nasolabial fold.
- Most common pattern is a nodule-ulcerative lesion a slow-growing small nodule that undergoes central with pearly, rolled margins.
- Tumour enlarges in size by burrowing and by destroying the tissues locally like a rodent and hence the name “rodent ulcer”.
Basal Cell Carcinoma Investigations:
- Histopathological examination of the lesion
Basal Cell Carcinoma Treatment:
- Tumours are usually treated with complete local excision.
- BCC responds well to radiation. Radiation is indicated in elderly patients with extensive lesions, does – 4000 – 6000 gy units.
- Cryosurgery
- Local chemotherapy
- Laser beam destruction of the tumour.
Question 7. Discuss clinical features and management of jaw tumours.
(or)
Classify the tumours of the alveolar bone and describe its clinical features and management of it.
Answer:
Tumours Classification:
1. Benign Tumours:
- Epithelial origin
- Ameloblastoma
- CEOT
- AOT
- With mesenchymal origin
- Ameloblastic fibroma
- CEOC
- Odontoma
- With epithelial and mesenchymal origin:
- Odontogenic fibroma
- Myxoma
2. Malignant Tumours:
- Odontogenic carcinoma
- Malignant ameloblastoma
- Primary intraosseous carcinoma
- Odontogenic sarcoma
- Ameloblastic fibro asrcoma
- Ameloblastic fibro dentinosarcoma
- Odontogenic carcinosarcoma
Jaw Tumours Clinical Features:
- Commonly occurs in the mandible
- Slow enlarging, painless mass occurs
- Bony hard swelling of the jaw
- Expansion and distortion of the cortical plates
- Pain
- Paresthesia
- Mobility of the regional teeth
- Presence of cyst
- Pathological fractures may occur
- The overlying mucosa appears normal
- Larger lesions may perforate the cortical plates
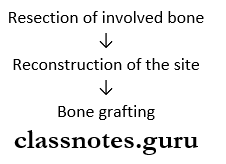
Jaw Tumours Management:
- Enucleation
Jaw Tumours Technique:
- Currettagc
Question 8. Describe the classification, clinical features, and treatment of odontoma.
Answer:
Odontoma
Odontomes are common hamartomatous odontogenic lesions with limited growth potential
Odontoma Types:
- Complex odontome:
- Consists of a massof haphazardly arranged enamel, dentin, and cementum
- Compound odontoma:
- Consists of collections of numerous small, discrete, tooth-like structures
Odontome Clinical Features:
- Age: Children and young adults
- Sex: Both
- Site: Compound- in maxilla
- Complex- mandible
Odontome Presentation:
- Small asymptomatic lesion
- Expansion of cortical plates
- Displacement of teeth
- Impacted or retained deciduous teeth
- Pain, inflammation
- Ulceration
- Fistula formation
Radiographic Features:
- Compound- A bag of teeth appearance
- Complex- sunburst appearance
Radiographic Treatment:
- Surgical enucleation
Cystic neck swellings questions and answers
Question 9. Describe clinical features, diagnosis, and treatment of ameloblastoma.
Answer:
Ameloblastoma Clinical Features
- Sex: Both sex
- Age- 1st to 7th decade
Ameloblastoma Types:
- Solid or multicystic ameloblastoma
- Slow-growing locally invasive tumours
- High recurrence rate
- Unicystic type
- Lesion can be enucleated
- Rarely seen in maxilla
- Recurrence rate is low
- Peripheral ameloblastoma
- Does not invade bone
- Treated in the early stages of development
Ameloblastoma Features:
- Swelling and pain in the region
- Inflammation
- Tension
- Dental trauma
- Ulceration of mucosa
- Loosening of teeth
- Epistaxis
- Nasal obstruction
Radiological Features:
- Unilocular or multi locular radiolucency
- Soap bubble appearance of the lesion
- Border is clear
- Resorption of the teeth
Radiological Management:
- Forintraosseous- marginal resection
- Segmental resection
- Aggressive resection
Jackson’s Guidelines:
- Tumour confined to maxilla without orbit floor involvement- Partial maxillectomy
- Tumour involving orbital floor- Total maxillectomy
- Tumour involving orbital contents- Total max-lobectomy.
- Tumour involving skull bone- Neurological procedure
Question 10. Describe the pathology, clinical features, and management of adamantinoma.
Answer:
Adamantinoma: Adamantinoma is a relatively uncommon, well-circumscribed, odontogenic neoplasm characterized by the formation of multiple duct-like structures by the neoplastic epithelial cells
Adamantinoma Clinical Features:
- Age- common in young age
- Sex: females are commonly affected
- Site- commonly occurs in the maxillary anterior region
- It is slow enlarging tumour
- Small, bony hard swelling is present in the maxillary anterior region
- Causes elevation of the upper lip on the involved side
- Displacement of regional teeth
- Mild pain and expansion of the cortical plates
- Severe expansion of bone in severe cases
- Associated with unerupted teeth
- It also has extra osseous involvement in the anterior maxillary gingiva
- Produces solitary painless, asymptomatic nodular swelling on the gingiva
Adamantinoma Pathology:
- Spindle-shaped, neoplastic odontogenic epithelial cells appears to proliferate in multiple duct-like patterns
- These ducts are lined by tall columnar cells
- Central lumen is filled with eosinophilic coagulum
Adamantinoma Management
- Adamantinoma Management is treated by surgical enucleation
- The associated tooth is removed
Oral and neck tumors short questions
Question 11. Discuss the clinical features and management of cysts of the jaw.
Answer:
Cysts Of The Jaw: Cysts of The Jaw is pathological cavity containing fluid, semi-fluid or, gas, which is usually lined by epithelium and is not formed by the accumulation of pus
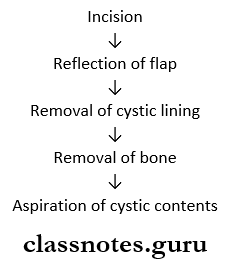
Cysts Of The Jaw Management:
Enucleation Of cyst:
- Smaller single cyst through intraoral approach
- Unilocular lesions through marginal excision
- Large multilocular lesions
Cysts of The Jaw Marsupialization:
- It refers to creating a surgical window in the wall of the cyst and evacuation of the cystic contents
Question 12. Name the swellings arising from the jaw. Describe clinical features, diagnosis, and treatment of dentigerous cyst.
Answer:
Dentigerous Cyst Clinical Features
- Sex: Common in males
- Age: 1st and 3rd decade
- Site: Mandibular 3rd molar, maxillary canines, maxillary 3rd molar
- Expansion of bone
- Facial asymmetry
- Displacement of adjacent teeth
- Resorption of adjacent teeth
Radiological Features:
- The unilocular, well-defined radiolucency
- Margins- sclerotic
Radiological Types:
- Central- covering the crown of an unerupted tooth
- Circumferential- covering the crown from all the sides
- Lateral- covering crown from side
Radiological Management:
- Marsupialization- in children
- Enucleation – in adults
Question 13. Describe the midline swellings of neck. Discuss etiology, clinical features, and management of thyroglossal cyst.
Answer:
Midline Swellings Of The Neck:
- Ludwig’s angina
- Enlarged submental lymph nodes
- Sublingual dermoid
- Thyroglossal cyst
- Subhyoid bursitis
- Goitre
- Lipoma
- Retrosternal goitre
- Thymic swellings
- Bony swelling arising from manubrium sterni
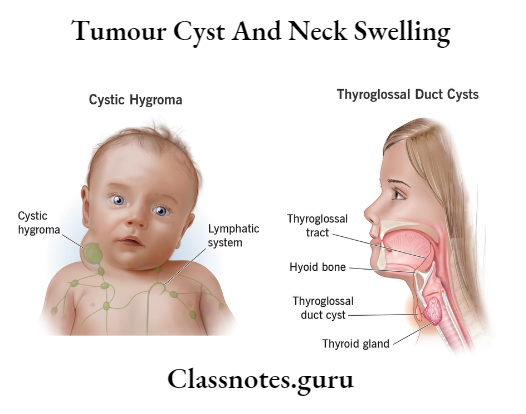
Thyroglossal Cyst:
Thyroglossal Cyst is a cystic swelling developed in the remnant of the thyroglossal tract
Thyroglossal Cyst Etiology:
Develops from the ventral portion of the endoderm between the first and second branchial arch
Thyroglossal Cyst Clinical Features:
- Age- common between 15-30 years of age
- Sex- common in women
- Pain in cyst
- Size: 0.5 cm to 5 cm in diameter
- Shape: spherical or oval
- Cyst becomes tender
- It may develop anywhere along the thyroglossal tract
- Firm or hard in consistency
- Cyst moves with deglutition
Thyroglossal Cyst Management:
Excision of the cyst
Neck swelling differential diagnosis Q&A
Tumour Cyst And Neck Swelling Short Essays
Question 1. Dermoid cyst
Answer:
Dermoid Cyst
- Dermoid cyst is a cyst that lies deep to the skin and is lined by the skin
- Dermoid cyst is lined by squamous epithelium and contains toothpaste-like material
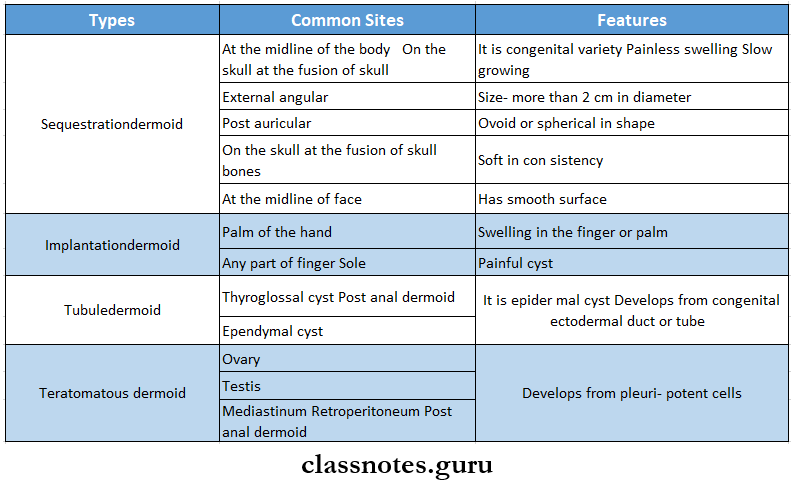
Dermoid Cyst Types:
- Sequestration dermoid
- Implantation dermoid
- Tubule-dermoid
- Teratomatousdermoid
Question 2. Sublingual dermoid
Answer:
Sublingual Dermoid
- Sublingual dermoid is a congenital swelling
- Sublingual Dermoid is formed at the point of fusion of the two mandibular arches
- Sublingual Dermoid develops from the secretion of the sequestrated surface ectoderm at the fusion site
Sublingual Dermoid Clinical Features:
- Present below or above the hyoid bone
- Causes swelling of the floor of the mouth
- Color- whitish in color
- It is opaque
- Age: 10-25 years of age
- Sex: both sex are equally affected
- It is painless swelling
- Rarely the contents become infected and the cyst becomes painful and tense
Sublingual Dermoid Types:
- Median variety
- Supramylohyoid variety
- Midline swelling on the floor of the mouth
- Inframylohyoid variety
- Swelling is present in the submental region resulting in double chin appearance
- Supramylohyoid variety
- Lateral variety
- Supramylohyoid variety
- Opaque cystic swelling in the floor of the mouth
- Inframylohyoid variety
- Cystic swelling present in the submandibular region
- Supramylohyoid variety
Sublingual Dermoid Treatment:
- Total excision
- Supramy lohyoidvarities- approached through floor of the mouth
- Infra mylohyoid varieties approached through the neck by curved incision
Question 3. Preauricular dermoid
Answer:
Preauricular Dermoid
Preauricular dermoid is type of sequestration dermoid
Preauricular Dermoid Etiology:
- Imperfect fusion of 1st and 2ndbranchial arches in formation of the auricle communicating with an ear pit on the surface
Preauricular Dermoid Clinical Features:
- Painless swelling
- Slow growing
- Size- more than 2 cm in diameter
- Ovoid or spherical in shape
- Soft in consistency
- Has smooth surface
Preauricular Dermoid Complications
- Infection
- Suppuration
- Ulceration
- Pressure symptoms to the surrounding structures
Preauricular Dermoid Treatment
- Surgical excision
Common neck swellings MCQs
Question 4. Postauricular dermoid and External angular dermoid
Answer:
Postauricular Dermoid
- Postauricular Dermoid is type of sequestration dermoid
- Site: behind the ear- at the site of fusion of the mesodermal hillocks
External Angular Dermoid
- External angular dermoid is type of sequestration dermoid
- External angular dermoid is present above the outer canthus of the eye- at the line of fusion of the frontonasal and maxillary processes
Question 5. Lipoma
Answer:
- Lipoma is a benign neoplasm of adipose tissue
- Lipoma is composed of mature fat cells
Lipoma Clinical Features:
- Age: above 40 years of age
- Sex: both sex are equally affected
- Lipoma is soft, well-defined, movable mass
- Smooth-surfaced
- Nodular, pedunculated or sessile lesion
- These are painless swelling
- Color
- Superficial lesions- yellow in color
- Deep lesions- pink in color
- Size: less than 3 cm in diameter
- It floats in aqueous solution
Lipoma Pathology:
- Lipoma presents well-circumscribed areas of proliferating mature fat cells within loose areolar tissue stroma
- Cells has round, vacuolated clear cytoplasm
- Lobules of cells are separated by fibrous tissue septa
- May contain benign lip blasts which results in soap bubble appearance
Lipoma Treatment: Surgical excision
Question 6. Basal cell carcinoma
Answer:
Basal Cell Carcinoma Etiology:
- Prolonged exposure to strong sunlight
- UV rays
- Arsenic used in skin ointments.
- Dysregulation of PTCH pathway.
- Inherited effects of PTCH gene causing BCC, gorlin syndrome.
Basal Cell Carcinoma Clinical Features:
- Majority of lesions occur on the face, usually abore a line joining lobe of the ear and the angle of the mouth.
- Common sites are the inner and outer canthus of the eye, eyelids bridge of the nose, and around the nasolabial fold.
- Most common pattern is a nodule-ulcerative lesion a slow-growing small nodule that undergoes central with pearly, rolled margins.
- Tumour enlarges in size by burrowing and by destroying the tissues locally like a rodent and hence the name “rodent ulcer”.
Basal Cell Carcinoma Investigations
- Histopathological examination of the lesion
Basal Cell Carcinoma Treatment:
- Tumors are usually treated with complete local excision.
- BCC responds well to radiation. Radiation is indicated in elderly patients with extensive lesions, does – 4000 – 6000 gy units.
- Cryosurgery
- Local chemotherapy
- Laser beam destruction of the tumour
Question 7. Premalignant lesions of the oral cavity
Answer:
Premalignant Lesions Of The Oral Cavity
- Premalignant lesions of the oral cavity is defined as morphologically altered tissue in which cancer is more likely to occur than its apparently normal counterpart.
- They are
- Leukoplakia
- Leukoplakia is a white patch or plaque which cannot be scrapped off or stripped off easily and cannot be characterized clinically or pathologically as any other disease
- They can be nonpalpable, faintly translucent, white areas
- Many lesions are thick, fissured, indurated
- Size is variable
- The surface may be smooth or finely wrinkled
- Color- white or grayish or yellowish-white in color
- Erythroplakia
- Erythroplakia is red patch or plaque which cannot be characterized clinically or pathologically as any other condition and which has no apparent cause
- Erythroplakia has clearly defined margins
- Types
- Homogenous erythroplakia
- Erythroplakia interspersed with patches of leukoplakia
- Speckled erythroplakia
- Stomatitis nicotine
- Stomatitis nicotine is tobacco-related keratosis
- Stomatitis nicotine affects both hard and soft palate
- There is hyperkeratosis of the epithelium and inflammatory swelling of the palatal mucous glands
- Surface has elevated keratotic rings
- Chronic candidiasis
- It is fungal infection
- Seen in the palatal mucosa of the denture-wearing persons
- Common in females
- Appears as bright red, edematous, velvety area
- Leukoplakia
Benign and malignant tumors Q&A
Question 8. Epulis
Answer:
Epulis
- Epulis is a swelling situated on the gum
- It arises from the alveolar margin of the jaw
Epulis Types:
- Fibrous epulis
- Arises from the periosteum at the neck of an incisor or premolar tooth
- V is a firm nodule at the junction of the gum and tooth
- Polypoid in shape
- Slow growing tumour
- Adjacent teeth are slightly separated and loosen
Epulis Complications:
Fibrosarcoma
Epulis Treatment:
- Excision
- Granulomatous epulis
- Epulis is a mass of granulation tissue around a carious tooth
- Epulis looks bright red in color
- Epulis is soft to firm in consistency
- Epulis easily bleeds on touch
- Associated with carious teeth
- Regional lymph nodes are enlarged and tender
- Extraction of the carious tooth
- Replacement of ill-fitted denture
- Maintenance of oral hygiene
- Removal of granulation tissue
- Diathermy of granulation tissue
- Myeloid epulis
- It is an osteoclastoma and arises from the underlying bone
- Overlying mucosa becomes hyperaemic, edematous and soft to touch
- It is sessile
- Rapidly growing
- Plum colored
- Adjoining teeth are loosen and separated
Epulis Complication:
- Ulceration
- Serious haemorrhage
Epulis Treatment:
- Currettage of small swelling
- Radical excision of large swellings
- Carcinomatous epulis
- It is epithelioma of the gum
- Present as lump or ulcer
- Painful lesion
- Invades bone
- Regional lymph nodes are involved
- Adequate resection of the lesio
- Radiotherapy
Question 9. Burkitt’s tumour
Answer:
Burkitt’s Tumour
- Burkitt’s Tumour is a distinctive type of B-cell lymphoma caused by Epstein-Barr virus (EBV) infection.
- 3 sub-groups of Burkitt’s lymphoma are:
- African endemic
- Sporadic
- Immunodeficiency associated.
- Etiology – EBV infection and immune suppression.
Burkitt’s Tumour Features:
- The disease affects children and adolescents
- Involves extranodal sites, particularly the jaw, gastrointestinal tract, and gonads.
Histological Appearances:
Tightly packed lymphoblasts interspersed with phagocytic macrophages which impart a starry-sky appearance in histological sections.
Question 10. Adamantium
Answer:
Adamantium
Adamantium is relatively uncommon, well-circumscribed, odontogenic neoplasm characterized by the formation of multiple duct-like structures by the neoplastic epithelial cells
Adamantium Clinical Features
- Age- common in young age
- Sex: females are commonly affected
- Site- commonly occurs in maxillary anterior region
- It is slow enlarging tumour
- Small, bony hard swelling is present in maxillary anterior region
- Causes elevation of the upper lip on the involved side
- Displacement of regional teeth
- Mild pain and expansion of the cortical plates
- Severe expansion of bone in severe cases
- Associated with un erupted teeth
- Adamantium also has extra osseous involvement in the anterior maxillary gingiva
- Produces solitary painless, asymptomatic nodular swelling on the gingiva
Adamantium Management:
- Adamantium is treated by surgical enucleation
- The associated tooth is removed
Question 11. Epidermoid cyst
Answer:
Epidermoid Cyst
These are small, hard lumps that develop under the skin
Epidermoid Cyst Causes:
- Excessive keratin production Acne
- Excessive sun exposure
Epidermoid Cyst Clinical Features:
- Site involved
- Face
- Head
- Neck
- Back
- Genitals
- Slow growing
- Painless swelling a Size- 1/2 -2 inch in diameter
- Color- tan to yellow in color
- Filled with thick smelly matter
Epidermoid Cyst Treatment:
- Epidermoid cyst heals on its own
- In case of infection- antibiotics and steroid injection is used
- Rarely removed for cosmetic purposes
Epidermoid Cyst Prognosis: If drained it recurs again
Questions on cystic lesions of head and neck
Question 12. Adenoma
Answer:
Adenoma
- Adenoma is benign tumour of glandular tissue
- Adenoma consists of dense mass of acini lined by exuberant epithelium which may be columnar or cuboidal
Adenoma Types:
- Fibroadenoma
- Fibroadenoma occurs in breast
- The specialised connective tissue surrounding the glandular epithelium is involved
- Fibroadenoma occurs due to excessive stromal reaction
- Fibroadenoma is further divided into two types
- Hard pericanalicula rfibroadenoma
- The ducts are surrounded by dense connective tissue
- Soft intracanlicular fibroadenoma
- Loose connective tissue is impinged into the ducts
- The connective tissue shows rapid growth and enlarges to a great extent
- Cystadenoma
- Adenoma forms cystic spaces into which papillary in the growth of neoplastic epithelium occurs
- Cystadenoma is called cystadenoma
- Sites involved
- Ovary
- Pancreas
- Parotid gland
- Kidney
- Adenoma Types
- Serous cystadenoma- serous-producing adenoma
- Pseudomucinous cystadenoma- mucin-producing adenoma
Question 13. Sequestration dermoid
Answer:
Sequestration Dermoid
- Sequestration dermoid is congenital type of dermoid cyst formed by inclusion of epithelium at the line of embryonic fusions
Sequestration Dermoid Common Sites:
- At the midline of the body
- External angular
- Post auricular
- On the skull at the fusion of skull bones
- At the midline of face
Sequestration Dermoid Clinical Features:
- Sequestration dermoid is congenital variety
- Painless swelling
- Slow growing
- Size- more than 2 cm in diameter
- Ovoid or spherical in shape
- Soft in consistency
- Has mooth surface
Sequestration Dermoid Complications:
- Infection
- Suppuration
- Ulceration
- Pressure to the surrounding structures
Sequestration dermoid Treatment:
- Complete excision of the cyst
Question 14. Implantation dermoid
Answer:
Implantation Dermoid
- Implantation dermoid is acquired dermoid
- Implantation dermoid arises from indriven epithelium beneath the skin due to puncture injury
Implantation Dermoid Common Sites:
- Palm of the hand
- Any part of finger
- Sole
Implantation Dermoid Clinical Features:
- Swelling in the finger or palm n Painful cyst
- Cyst is tensed n Consistency is firm to hard
- There may be scar over the skin
Implantation Dermoid Complication:
- Infection
- Suppuration
- Bursting
Implantation Dermoid Treatment:
Complete excision of the cyst
Question 15. Sternomastoid tumour
Answer:
Sternomastoid Tumour
- Sternomastoid tumour is also called congenital torticollis
Sternomastoid Tumour Etiology:
- Infarction of the central portion of one sternomastoid muscle
- Congenital anomaly
- Infarction of the sternomastoid branch of the superior thyroid artery
- Trauma
Sternomastoid Tumour Clinical Features:
- Age- several days to several months after birth
- A lump is produced
- Site: in the middle of the sternomastoid muscle
- Torticolis- head is turned to one side
- It is painful lesion
- Size: 1-2 cm in diameter
- It is fusiform in shape
- Surface is smooth
- It is firm in consistency
- Regional lymph nodes are normal
Sternomastoid Tumour Treatment:
- At birth
- Manipulation of head of the child
- After the development of torticollis
- Use of brace
- Sternomastoid muscle is divided
- Subcutaneous tenotomy
- Deep fascia or neighboring muscles are divided
Short notes on neck tumors and swellings
Tumour Cyst And Neck Swelling Short Answers
Question 1. Nasopalatine cyst
Answer:
Nasopalatine Cyst
- A nasopalatine duct cyst is a relatively common, nonodontogenic intraosseous, cystic lesion arising within the nasopalatine duct or incisive canal
Nasopalatine Cyst Clinical Features:
- Age- fourth, fifth and sixth decade of life
- Sex: Males are commonly affected
- It is small, painful, fluctuant swelling present in the midline of the anterior part of the hard palate near the opening of the incisive foramen
- Causes pressure sensation on the floor of the nose and displacement of the upper central incisors
- There may be purulent discharge
- Swelling in the soft tissue between upper central incisors occurs
- The regional teeth are vital
Nasopalatine Cyst Treatment:
Surgical excision
Question 2. Neurofibroma
Answer:
Neurofibroma
- Neurofibroma is the tumour arising from the connective tissue of the nerve sheath
Neurofibroma Types:
- Local or solitary neurofibroma
- Found in the subcutaneous tissue
- Usually seen in the extremities
- Cranial nerves may be involved
- Generalised neurofibromatosis/ Von Recklinghausen’s disease
- In it there are multiple neurofibromas arising from the cranial, spinal, and peripheral nerves
- It comprises of two types
- Type 1- Von Recklinghausen’s disease
- Type 2- acoustic neurofibromatosis
- Plexiform neurofibromatosis
- Plexiform neurofibromatosis is an excessive overgrowth of neural tissue in the subcutaneous fat
- Common in branches of trigeminal nerve
- Elephantiasis neurofibromarosa
- Severe form of plexiform neurofibromatosis affecting subcutaneous nerves of the limbs
- Cutaneous neurofibromatosis
- These are multiple subcutaneous nodules, sessile or pedunculated over the chest, abdomen, or back
Question 3. Spread of malignant tumors
Answer:
1. Lymphatic Spread: In general, carcinomas metastasize by the lymphatic route
- Involvement of lymph nodes by malignant cells may be of two forms.
2. Haemategenous Spread:
- Sarcomas spread through hematogenous spread
- Common sites for blood-borne metastasis are
- Lung
- Breast
- Thyroid
- Kidney
- Liver
- Prostrate and
- Ovary.
Question 4. Glomus tumour
Answer:
Glomus Tumour
- Glomus tumour is rare, benign, and painful tumour of the skin and subcutaneous tissue
- Occurs in the extremities
- It is circumscribed
- Blue or reddish in color
- Size- not more than 1 cm in diameter
- Pain occurs spontaneously or with pressure or trauma
- Pain is stabbing and burning type
- Pain is caused by dilated glomus vessels pressing on the numerous nerve endings
Glomus Tumour Treatment:
Surgical excision of the lesion
Question 5. Carcinoid tumour
Answer:
Carcinoid Tumour
They are rare tumors of the neuroendocrine system
Carcinoid Tumour Causes:
- Hereditary
- Neurofibromatosis
- Tuberous sclerosis
- Lymphoma
Carcinoid Tumour Risk Factors:
- Diabetes
- Gastritis
- Smoking
- Obesity
Carcinoid Tumour Clinical Features:
- Slow growing
- Patient remains asymptomatic for many years
- Individuals above 60 years are affected
- Sites involved are
- GIT
- Lung
- Pancreas
- Kidney
- Ovaries
- Testicles
- Spread to liver, lymph nodes, and bone
- Carcinoids of lung cause
- Cough
- Breathlessness
- Chest pain
- Wheezing
- Tiredness
- Weight gain
- Carcinoid of stomach
- Weight loss
- Pain
- Fatigue
Oral pathology tumors and cysts questions
Question 6. Malignant melonoma
Answer:
Malignant Melonoma
Malignant melanomal is a tumour arising from pigment-forming cells i.e., melanoblast which are desired from the neural crest.
Malignant Melonoma Etiology: Unknown but there is role of excessive exposure of white skin to sunlight.
Malignant Melonoma Common Site:
- Oral and anagenital mucosa,
- Oesophagus,
- Conjuctiva,
- Orbit,
- Leptomeninges.
Malignant Melanoma Clinical Features:
- Flat/slightly elevated nerves which has variegated pigmentation, and irregular borders and has undergone secondary changes of ulceration, bleeding and increase in size.
- Depending upon clinical course and prognosis, cutaneous malignant melanomas are of 4 types.
- Lentigo maligna melanoma
- Superficial spreading melanoma
- Aeralcontigenous melanoma
- Nodular melanoma.
- Spread: Metastatic spread in very common via lymphatics.
Malignant Melanoma Treatment:
- Surgery – main modality.
- Palliative and supportive – other modalities.
Question 7. Potato tumour
Answer:
Potato Tumour
- Carotid body tumour is called potato tumour because
- It looks yellow or orange on cut surface
- It is firm, homogenous, and compact tumor
- Well capsulated
- Potato Tumour is adherent to the carotid artery
Potato tumour Clinical Features:
- Age- 40-60 years of age
- Sex: Both sex are equally affected
- There is slow growing painless swelling at the bifurcation of common carotid artery
- Horner’s syndrome may be present
- Patient may suffer from transient cerebral ischaemia
Potato tumour Treatment: Surgical excision
Question 8. Osteoclastoma
Answer:
Osteoclastoma
Osteoclastoma is rare tumour of jaw
Osteoclastoma Clinical Features:
- Age- 25-40 years of age
- Sex: males are commonly affected
- Osteoclastoma is rapidly growing tumour
- Mandible is commonly affected
- There is an expansion of cortical plates
- Osteoclastoma is painless lesion
Osteoclastoma Differential Diagnosis:
- Giant cell reparative granuloma
- Adamantionoma
Question 9. Cavernous haemangioma
Answer:
Cavernous Haemangioma
- Arises from veins
- Cavernous haemangioma consists of multiple dilated venous channels
- Cavernous haemangioma is a spongy swelling
Cavernous Haemangioma Management: Conservative treatment
- Injection of sclerosing agent
- Cautery
- Surgery
- Ligation of feeding vessels
- Excision of the lesion
- Diathermy to control haemorrhage
- Surgery
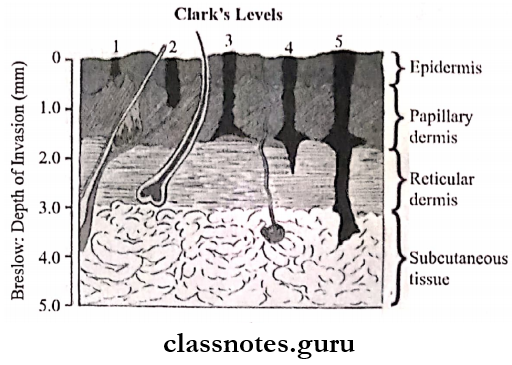
Question 10. Clarke’s level of invasion of malignant melonoma
Answer:
Clarke’s Level Of Invasion Of Malignant Melonoma
- Malignant melanoma can be staged according to Clarke’s level of invasion
- Level 1- all tumour cells are above the basement membrane
- Level 2- Tumour extends into the papillary but not the reticular dermis
- Level 3- Tumour cells reach the interface between the papillary and reticular dermis
- Level 4- tumour cells reaches the reticular dermis
- Level 5- tumour cells invade the subcutaneous fat
Question 11. Microscopic picture of squamous cell carcinoma
Answer:
Microscopic Picture Of Squamous Cell Carcinoma
Microscopic picture of squamous cell carcinoma is characterised by malignant cells
- These cells show variable degree of differentiation
- Cells invade through the basement membrane into the dermis
Squamous Cell Carcinoma Arrangement:
- Cells are arranged in concentric layers called epithelial pearls
- They contain keratin material in the center of the cell masses
- Cells are separated by lymphocytes
Question 12. Hamartoma
Answer:
Hamartoma
- Hamartoma is a developmental malformation consisting of a tumor-like overgrowth in which tissues of a particular part of the body are arranged haphazardly
- Hamartoma is present since birth
- Growth is co-ordinated
- Hamartoma may regress on its own
- Hamartoma may be multiple- like neurofibroma
- Hamartoma grows along with its surrounding
- Hamartoma is associated with a chromosomal abnormality
Hamartoma Examples
- Vascular hamartoma- haemangioma
- Benign nevus
- Angiomatous syndromes
- Glomus tumour
- Lymphangioma
- Neurofibroma
- Skeletal hamartoma
- Adenoma sebaceous
Thyroglossal cyst short questions
Question 13. Osteoid osteoma
Answer:
Osteoid Osteoma
Osteoid osteoma are benign intraosseous neoplasms
Osteoid Osteoma Clinical Features:
- Occurs among young individuals
- Males are commonly affected
- Develop in long bones
- Causes bony expansion
- Lesion is painful
- Size: 1 cm in diameter
- It don’t grow further
Osteoid Osteoma Treatment:
- Surgical excision
- Curettage
Question 14. Fibrous epulis
Answer:
Fibrous Epulis
- Fibrous epulis is common type of epulis
- Fibrous Epulis arises from the periosteum at the neck of an incisor or premolar tooth
- Fibrous Epulis is a firm nodule at the junction of the gum and tooth
- Polypoid in shape
- Slow growing tumour
- Adjacent teeth are slightly separated and loosen
Fibrous Epulis Complications: Fibrosarcoma
Fibrous Epulis Treatment: Excision
Question 15. Branchial Cyst
Answer:
Branchial Cyst
Branchial cyst is congenital cyst
Branchial Cyst Clinical Features:
- Age- symptoms appears at the age between 20-25 years
- Sex: equal in both sex
- Appears as painless swelling
- Site- upper and lateral part of the neck deep to the upper third of the sternocleidomastoid
- Branchial cyst is round or oval in shape
- Size– 5-10 cm in diameter
- Soft in consistency
- Regional lymph nodes are not palpable
Branchial Cyst Complications:
- Recurrent infections
- Branchial fistula
Branchial Cyst Treatment: Excision
Question 16. Digastric Triangle
Answer:
Digastric Triangle
- Boundaries
- Anteroinferior – anterior belly of digastric
- Posteroinferior – posterior belly of digastric
- Superior or base
- Base of mandible
- The line joining angle of the mandible to the mastoid process
- Roof
- Skin
- Superficial fascia containing
- Platysma
- Cervical branch of the facial nerve
- Ascending branch of the transverse cutaneous nerve of neck
- Deep fascia
- Floor
- Anterior – mylohyoid muscle
- Posterior – Hyoglossus muscle
- Floor – middle constrictor of the pharynx
Question 17. Types of neck dissections
Answer:
Types Of Neck Dissections
- Neck dissection is a major surgery done to remove lymph nodes that contain cancer
- Types: based on the amount of tissue and lymph nodes removed
- Radical neck dissection
- AI the tissues on the side of the neck from the jawbone to the collarbone is removed
- The muscles, nerve, salivary gland, and major blood vessel in this area are all removed
- Modified radical neck dissection
- Radical neck dissection
- Types Of Neck Dissections is most common type
- All lymph nodes are removed
- Less tissue is removed
- Nerves, blood vessels, or muscles are spared
- Selective neck dissection
- Fewer lymph nodes are removed
- Muscles, nerves, and blood vessels are saved
Tumour cyst and neck swelling Q&A
Question 18. Ganglion Cyst
Answer:
Ganglion Cyst
- Ganglion cyst is a cystic swelling occurring in relation to tendon sheath or synovial sheath or joint capsule
- Contains clear gel-like fluid
Ganglion Cyst Common Sites
- Dorsum of wrist
- Flexor aspect of wrist
- Around ankle joint
Ganglion Cyst Clinical Features
- Well-localized, smooth, soft, cystic swelling
- Ganglion cyst is non-tender, mobile and transilluminate
- Often pain, tenderness, and restricted joint movements may be present
Ganglion Cyst Treatment: Excision
Tumour Cyst And Neck Swelling Viva Voce
- Infection is the most common complication of cyst
- Multiple cysts is a characteristic feature of sebaceous cyst
