Temporomandibular Joint Important Notes
1. Myofascial Pain Dysfunction Syndrome
- Masticatory muscle tenderness
- Pain in TMJ
- Limitation of motion
- Clicking noise present
Temporomandibular Joint Long Essays
Question 1. Describe the etiology, clinical features, differential diagnosis, and treatment of myofascial pain dysfunction syndrome.
Answer:
Myofascial Pain Dysfunction Syndrome
- It is a disorder characterized by facial pain limited to the mandibular function, muscle tenderness, joint sounds, absence of significant organic and pathologic changes in TMJ
- It may be due to functional derangement of dental articulation, psychological state of mind, or physiological state of the joint
- Coined by Laskin
Etiology:
- Extrinsic Factors
- Occlusal disharmony
- Trauma
- Environmental influences
- Habits
- Intrinsic Factors
- Internal derangement of TMJ
- Anterior locking of disc
- Trauma
Myofascial Pain Dysfunction Features:
- Unilateral preauricular pain
- Dull constant sound
- Muscle tenderness
- Clicking noise
- Altered jaw function
- Absence of radiographic changes
- Absence of tenderness in ext. auditory meatus
Myofascial Pain Dysfunction Management:
- Reassurance
- Soft diet
- Occlusal correction: 7 ‘R’s
- Remove-extract the tooth
- Reshape grind the occlusal surface
- Reposition orthodontically treated
- Restore conservative treatment
- Replace by prosthesis
- Reconstruct TMJ surgery
- Regulate control habits
- Isometric exercises
- Opening and closing of mouth 10 times a day
- Medicaments
- Aspirin: 0.3-0.6 gm/ 4 hourly
- NSAIDS: For 14-21 days
- Pentazocine: 50 mg/ 2-3 times a day
Read And Learn More: Oral Medicine Question and Answers
- Heat application
- It increases circulation
- Diathermy
- Causes heat transmission to deeper tissues
- LA injections
- 2% lignocaine into trigger points
- Steroid injection
- As anti-inflammatory
- Anti-anxiety drugs
- Diazepam-2-5 mg * 10 days
- Tens
- Acupuncture
Question 2. Define trismus. Discuss various causes and management of trismus.
(or)
Define trismus. Discuss various causes and differential diagnoses of trismus.
Answer:
Trismus
Trismus is a condition in which muscle spasm prevents the opening of the mouth
Trismus Causes:
- Orofacial infection
- Trauma
- Inflammation
- Myositis
- Tetany
- Tetanus
- Neurological disorders
- Drug-induced
- Extra articular fibrosis
- Mechanical blockage
Pathogenesis:
Injection of inferior alveolar nerve block
↓
Bleeding at the site
↓
Haematoma
↓
Fibrosis
↓
Trismus
Trismus Differential Diagnosis:
- Internal derangement of TMJ
- Fracture of mandibular condyle
- TMJ dislocation
- Septic arthritis
- Osteoarthritis
- Ankylosis
- Hematoma
- Acute infections
Trismus Treatment:
- May resolve on its own
- Manipulation of the jaw by jaw stretcher
Temporomandibular Joint Short Essays
Question 1. Articular disc disorders of the temporomandibular joint.
Answer:
Articular Disc Disorders Of The Temporomandibular Joint
In osteoarthritis, an articular disc of TMJ is affected
Etiopathogenesis:
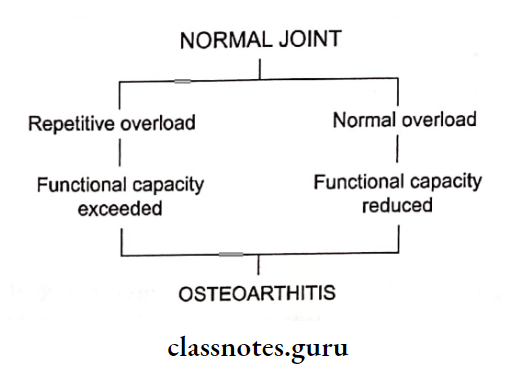
Temporomandibular Joint Types:
- Primary: Due to wear and tear
- Secondary: Due to local and systemic factors
Temporomandibular Joint Clinical Features:
- Age: Older age
- Site: common in TMJ
Temporomandibular Joint Presentation:
Unilateral painful joint
↓
Interference in biting and
mandibular movements
↓
Sensitive to palpation
↓
Crepitation of joint
↓
Spasm of muscle
↓
Limitation of joint movements
Temporomandibular Joint Management:
- Elimination of cause
- Relief of pressure
- Physiotherapy
- Myotherapy
- Doxycycline
Question 2. Internal dearangement of temporomandibular joint.
Answer:
Temporomandibular joint Definition:
The temporomandibular joint is the anteromedial displacement of the interarticular disc associated with the posterosuperior displacement of the condyle in the closed jaw position
temporomandibular Joint Features:
- Pain on biting
- Clicking sound over the joint
- Deviation of mandible
- Restricted mouth opening due to pain
temporomandibular Joint Management:
1. Anterior Repositioning Appliances
- Placed on occlusal surfaces
2. Supportive Therapy
- NSAIDs to relieve pain
- Heat application
3. Occlusal Correction
Question 3. Ankylosis Of Temporomandibular Joint.
Answer:
Temporomandibular Joint Classification:
- False or true ankylosis
- Extra articular or intra articular
- Fibrous or bony
- Unilateral or bilateral
- Partial or complete
Etiology:
- Trauma Congenital
- Infections -Osteomyelitis
- Inflammation osteoarthritis
- Rare causes measles
- Systemic diseases typhoid
- Other causes of prolonged trismus
Temporomandibular Joint Pathogenesis:
Trauma
↓
Extravasation of blood into joint space
[haemarthosis]
↓
Calcification of joint space
↓
Obliteration of joint space
↓
Immobility of joint
↓
Ankylosis of joint
Temporomandibular Joint Features:
- Unilateral:
- Deviation of the chin on the affected side o Fullness of the face on the affected side
- Flatness on the unaffected side
- Crossbite
- Angle’s class malocclusion
- Condylar movements absent on the affected side
- Bilateral:
- Inability to open mouth
- Neck chin angle reduced
- Class 2 malocclusion
- Protusive upper incisors
- Multiple carious teeth
Temporomandibular Joint Management:
1. Condylectomy
- Pre auricular incision given
- Horizontal osteotomy cut given over condylar neck
- The condylar head is separated
- Smoothened the remaining structures
- Close the wound in layers
- If required bilateral condylectomy done
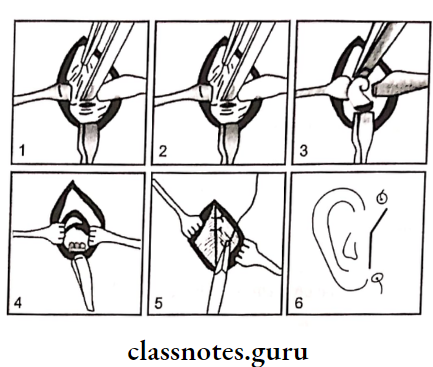
- Exposure of the condylar head via a preauricular incision
- Sectioning of condylar head,
- Breaking the fibrous adhesions
- Condylectomy complete
- Suturing the capsule
- Final skin suturing
1. Gap Arthroplasty:
- Two horizontal cuts are given
- Removal of a bony wedge between the glenoid fossa and ramus
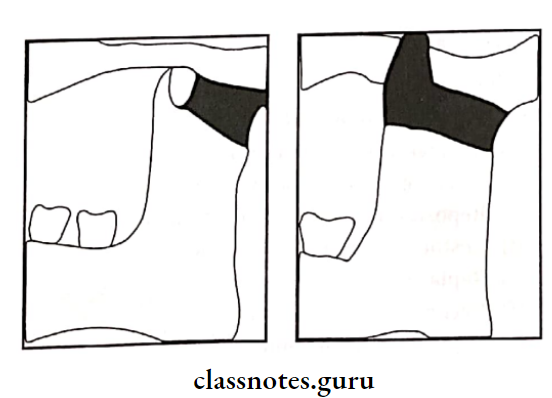
Interposition Arthroplasty
- Creation of gap
- Insertion of barrier (autogenous or alloplastic)
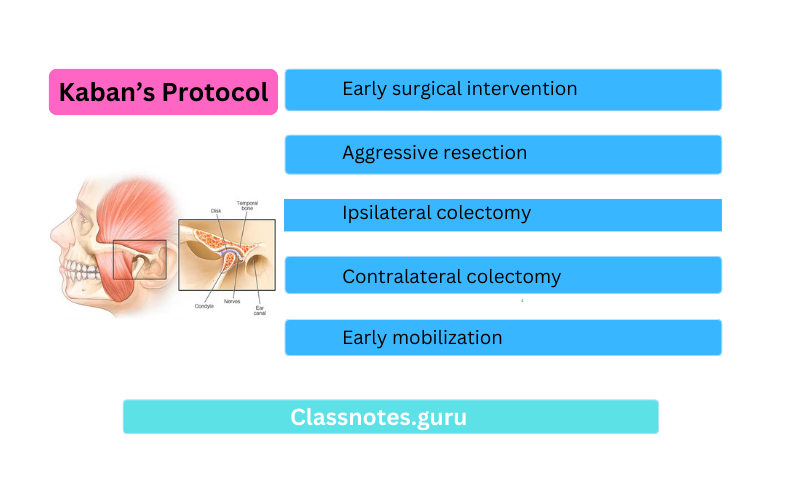
Kaban’s Protocol:
- Early surgical intervention
- Aggressive resection
- Ipsilateral colectomy
- Contralateral colectomy
- The lining of the glenoid fossa with temporalis fascia
- Reconstruction of ramus with a costochondral graft
- Early mobilization
- Regular follow up
Kaban’s Complications:
- Frey’s syndrome
- Parotid fistula
- Facial palsy
Question 6. Clinical features and management of degenerative arthritis.
Answer:
Degenerative Arthritis Clinical Features:
- Age and sex: Older women are more affected
- Site: Many joints are affected but it is not found often in TM]
Degenerative Arthritis Features:
- Unilateral pain over the joint
- It is sensitive on palpation
- Pain on movement or biting
- Pain aggravates during the evening
- There is the deviation of the jaw towards the affected side
- The affected joint is swollen and warm to the touch
- There is the presence of crepitation of the joint
- There is a limitation of jaw movements
- It results in stiffness and locking of the jaw
Degenerative Arthritis Management:
- Elimination Of The Causative Agent:
- Occlusal adjustment or grinding of teeth
- Replacement of missing teeth
- Replacement of ill-fitted dentures
- Treatment of caries and periodontal problems
- Drugs
- Analgesics and anti-inflammatory drugs are given.
- Physiotherapy
- Myotherapy
- Arthroscopic lavage
- A low dose of doxycycline
- Others
- Glucosamine
- Chondroitin sulfate
Question 7. Rheumatoid arthritis.
Answer:
Rheumatoid Arthritis
Rheumatoid Arthritis is a systemic disease that usually affects many joints including the TMJ and the disease is characterized by progressive destruction of the joint structures
Rheumatoid arthritis Clinical Features:
- Age And Aex: women from 20-50 years of age are affected
- Site: small joints of fingers and toes
- Presentation
- Bilateral stiffness
- Crepitus
- Tenderness and swelling over the joint
- Fever, malaise, fatigue
- Weight loss
- Polyarthritis affecting large and weight-bearing joints
- Formation of subcutaneous nodules on the pressure points
- The joint may become red, swollen, and warm to the touch
- Muscle atrophy around the jaw
- Bursitis
- TMJ Involvement
- Bilateral stiffness of the joint
- Deep-seated pain and tenderness on palpation
- Swelling over the joint
- There is a limitation of mouth opening
- Pain on biting is referred to the temporal region, ear, and angle of the mandible
- There is a deviation of the jaw on the opening
- Inability to perform lateral movements
- Anterior open bite
- Fibrous ankylosis of the joint
Rheumatoid Arthritis Complications:
- Subluxation
- Secondary arthritis
- Muscular atrophy
- Bird-like face
Rheumatoid Arthritis – Radiographic Features:
- Joint space is reduced
- There is a flattening of the head of the condyle
- Erosion of the condyle
- Hollowing of the condylar cartilage
- Bony destruction of the articular eminence
- The condylar outline is irregular and ragged
- Synovial lining resembles a “sharpened pencil” or “mouthpiece of the flute”
- Subchondral sclerosis and flattening of articular surface may occur
Rheumatoid Arthritis Management:
- Supportive treatment:
- Provide adequate rest
- Advice soft diet
- Medical
- Local injection of methyl prednisone acetate
- 20-80 mg for large joint
- 4-10 mg for small joint
- Salicylates for pain relief
- NSAIDs
- Phenylbutazone, indomethacin
- Anti Rheumatic
- Hydroxyl chloroquine sulfate sulphasalazine: 500 mg/day
- Local Therapy
- Diathermy
- Jaw exercises
- Mouth stretchers
- Surgical
- Synovectomy: for removal of synovial membrane
Oral Medicine Temporomandibular Joint Short Answers
Question 1. Myositis ossificans.
Answer:
Myositis Ossificans
- Myositis Ossificans is a condition in which fibrous tissue and hetero-tropic bone form within the interstitial tissue/ muscle as well as in associated tendons and ligaments
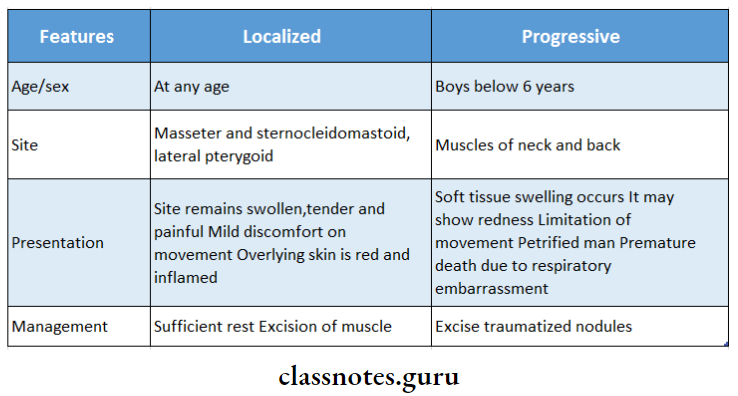
Myositis Ossificans Types:
- Localized
- Progressive
Question 2. Laskins criteria for MPDS.
Answer:
- Four Cardinal Signs
- Unilateral pain – dull ache in the ear or preauricular area or angle of the mandible
- Muscular tenderness
- Clicking noise in TMJ
- Limitation of jaw movements
- Negative Characteristics
- No radiographic changes
- No tenderness in TMJ on palpation
Oral Medicine Temporomandibular Joint Viva Voce
- Temporalis and geniohyoid are most often involved in MPDS
