Oral Medicine Salivary Glands Short Essays
Question 1. Sialolith.
(or)
Clinical features and Investigations of submandibular sialolithiasis.
Answer:
Sialolith
- Sialoliths are calcified organic matter that forms within the secretory system of the major salivary glands
Sialolith Etiology:
- It is unknown
- Several factors like:
- Inflammation,
- Irregularities in the duct system
- Local irritants and anti-cholinergic medication
- May contribute to stone formation
Sialolith Composition:
- Hydroxyapatite
- Calcium phosphate and carbon
- A trace amount of magnesium, potassium chloride, and ammonium
Salivary Glands Diagnosis:
- Occlusal radiograph for submandibular gland
- AP view of face for parotid
- CT images have 10 folds with greater sensitivity for detect¬ing
- calcification
- FNAC is used when differential diagnosis includes: a cyst or tumor
- Sialoendoscopy:
- It is a relatively new technique
- Small probe(<l mm diameter) attached to a specially designed endoscopic unit can explore the primary and sec¬ondary ductal system
- The unit has a surgical tip to obtain soft tissue biopsy and help to remove calcified material
Sialolith Occurrence:
- Submandibular gland(80-90%): Because
- The torturous course of Wharton’s duct
- Higher calcium and phosphate level
- Position of gland
- Parotid (5-15%)
- Sublingual(2-5%)
Salivary Glands Clinical Presentation:
- Acute, painful, and intermittent swelling
- Eating initiates salivary gland swelling
- Stone totally or partially blocks the flow of saliva, causing salivary pooling within the ductal system
- There is little space for expansion, so enlargement causes pain
- Stasis of saliva may lead to infection, fibrosis, and gland atrophy
- Fistula, sinus tract or ulceration may occur over the stone in chronic cases
- The soft tissue surrounding the duct may show edema and inflammation
Read And Learn More: Oral Medicine Question and Answers
Sialolith Complications:
- Suppurative or non-suppurative retrograde bacterial infection can occur
- Acute sialadenitis
- Ductal stricture
- Ductal dilatation
Differential Diagnosis Of Sialolithiasis:
- Gas Bubbles:
- Introduced during sialography
- Hyoid Bone:
- Seen bilaterally on panoramic film
- Myositis Ossificans:
- Restriction of mandibular movements occurs
Sialolith Treatment:
- Acute phase:
- Supportive treatment: it includes analgesics, antibiotics, hydration, and antipyretic
- In exacerbation:
- Surgical intervention or removal of stone
- Stones at or near the duct are removed transorally by milking the gland
- Deeper stones are removed by surgery or sailoendoscope
- Smaller stones are removed by gently massaging the gland
- Sialogogues, moist heat, and increased fluid intake may also promote the passage of stone
- Large sialoliths are surgically removed
- Ultrasonography – it will detect stones of diameter >2 mm
- Lithotripsy – it will fragment the stone
Question 2. Mumps.
Answer:
Mumps
- Mumps is an acute viral infection caused by RNA paramyxovirus
- Mumps is transmitted by direct contact with salivary droplets
- Prevention:
- By MMR (measles, mumps, rubella) vaccination
- Mumps is not recommended for severely immunocompromised children as the protective immune response does not develop and may lead to complications
Mumps Presentation:
- Age: 4-6 years
- Incubation period: 23 weeks
- Followed by salivary gland inflammation and enlargement
- Preauricular pain
- Fever
- Malaise
- Headache
- Myalgia
- Edema of the surrounding skin
- Ducts become inflamed but without purulent discharge
- Swelling is usually bilateral and lasts for approx. 7 days
Mumps Complications:
- Mild meningitis and encephalitis
- Deafness
- Myocarditis
- Thyroiditis
- Pancreatitis
- Oophoritis
- In males, epididymitis, and orchitis result in testicular atrophy and infertility
Mumps Diagnosis:
- Demonstration of antibodies against mumps S and V an¬tigens and to the hemagglutination antigen
- An oral fluid assay using a mumps-specific IgM capture enzyme immunoassay has demonstrated good sensitiv¬ity and specificity.
- A salivary test using reverse transcriptase PCR and loop-mediated isothermal gene amplification may help in the calculation of viral loads
Mumps Treatment:
- Symptomatic treatment done
Question 3. Pleomorphic adenoma of the palate.
Answer:
Pleomorphic Adenoma Of The Palate
- Pleomorphic Adenoma Of The Palate is the most common tumor
- Pleomorphic Adenoma Of The Palate is a mixed tumor as it contains both epithelial and mesenchymal component
- The majority found in the parotid, then in the submandibular, sublingual, and minor salivary gland
Pleomorphic Adenoma Of The Palate Presentation:
- Palatal tumors almost always are found on the poste¬rior lateral aspect of the palate as smooth-surfaced, dome-shaped masses
- Because of the tightly bound nature of the hard palate, it is immovable
Pleomorphic Adenoma Differential Diagnosis:
- Other parotid masses
- If calcification occurs in MRI, it is pleomorphic
Pleomorphic Adenoma Of The Palate Treatment:
- Surgical removal
- Wide resection to avoid recurrence
- Local enucleation is avoided because the entire tumor may not be removed or the capsule may be violated, resulting in the seeding of the tumour bed
- Tumours of the hard palate usually are excised down to the periosteum, including the overlying mucosa
Question 4. Xerostomia
Answer:
Xerostomia
Xerostomia refers to a subjective sensation of a dry mouth, but not always, associated with salivary hypofunction
Xerostomia Etiology:
1. Developmental:
- Salivary gland aplasia
2. Water/ Metabolic Loss:
- Impaired fluid intake
- Hemorrhage
- Vomiting/diarrhea
3. Latrogenic:
- Medications
- Antihistamines: diphenhydramine
- Decongestants: pseudoephedrine
- Antidepressants: amitriptyline
- Antipsychotic: haloperidol
- Antihypertensive: methyldopa, CCB
- Anticholinergic: atropine
4. Radiation Therapy Of The Head And Neck:
- Both stimulated and unstimulated salivary flow decreases with increasing radiotherapy.
- Systemic Diseases:
- Sjogren’s syndrome
- Diabetes mellitus
- Diabetes insipidus
- HIV infections
- Psychological disorders
- Graft-versus-host disease
- Systemic Diseases:
5. Xerostomia Local factors:
- Decreased mastication
- Smoking
- Mouth breathing
Xerostomia Clinical Features:
- Reduction in salivary secretion
- Residual saliva is either foamy or thick
- Mucosa appears dry
- The dorsal tongue is fissured with atrophy of filiform pa¬pilla
- Difficulty in mastication and swallowing
- Food adheres to the oral membranes while eating
- Some patients who complaints of dry mouth may appear to have adequate salivary flow
- The degree of saliva production can be assessed by measuring resting and stimulated saliva
- Increased prevalence of candidiasis because of reduction in cleansing and antimicrobial activity
- More prone to dental decay, especially cervical and root caries
Xerostomia Treatment:
- Artificial saliva may help the patient
- Sugarless candy can stimulate salivary flow
- Use of oral hygiene products like Biotene toothpaste, oral balance gel
- If dryness is secondary to medications, discontinue it or reduce its dose
- Systemic pilocarpine is used:
- It is a parasympathomimetic agonist
- Doses: 5-10 mg, 3-4 times a day
- ADR: excessive sweating,
- Increased heart rate and BP ^ Cevimeline hydrochloride
- Acetylcholine derivative
- Approved by the U.S. Food and Drug Administration
- Both these drugs are contraindicated in narrow-angle glaucoma
- To prevent dental decay, office, and daily home fluoride application
- Chlorhexidine mouthwash minimizes plaque buildup
- Local stimulation of saliva
- Chewing gums, mints, paraffin, and citric acid
Question 5. Sialometaplasia.
Answer:
Sialometaplasia Description:
- Sialometaplasia is a benign, self-limiting, reactive inflammatory dis-order of salivary tissue
Sialometaplasia Etiology:
- Unknown
- It may represent a local ischemic event
- Infectious process or
- Immune response to an unknown antigen
Sialometaplasia Presentation:
- Site:
- Common on palate
- Other include anywhere in the salivary gland tissue including lips, retromolar region
- Initially, lesion is present as a tender erythematous nodule
- Once the mucosa breaks, deep ulceration with a yellowish base forms
- The lesion can be large and deep
- The lesion can occur shortly after oral surgical procedure, restorative dentistry or administration of LA
Sialometaplasia Diagnosis:
- Adequate biopsy
- Histopathologic diagnosis
- Complete clinical history
Sialometaplasia Treatment:
- Self-limiting condition
- Healing by secondary intention occurs in approx. 6 weeks
- Debridement and saline rinses may help the healing process
Oral Medicine Salivary Glands Short Answers
Question 1. Causes of Sialorrhea.
Answer:
Causes of Sialorrhea
- Sialorrhea Drugs
- Lithium
- Cholinergic agonists
- Sialorrhea Local factors
- Stomatitis
- AUG
- Erythema multiforme
- Sialorrhea Systemic diseases
- Paralysis
- Alcoholic neuritis
- Parkinson’s disease
- Epilepsy
- Down’s syndrome
- Protective buffering system
- Miscellaneous
- Psychic factor
- Metal poisoning
- Facial paralysis
Question 2. Sialosis.
Answer:
- Sialosis Synonym: sialadenosis
- It is a rare chronic inflammatory disease of the sub-mandibular salivary gland
Sialosis Presentation:
- Enlarged, firm, and painful unilateral or bilateral salivary gland
Sialosis Treatment:
- No treatment is generally required
- Elimination of causative agent
- In some cases, surgical excision of the gland is required
Question 3. Why is sialolith common in the submandibular gland?
Answer:
- Sialolith is common in the submandibular gland due to
- The torturous course of Wharton’s duct
- Higher calcium and phosphate levels e Position of the gland
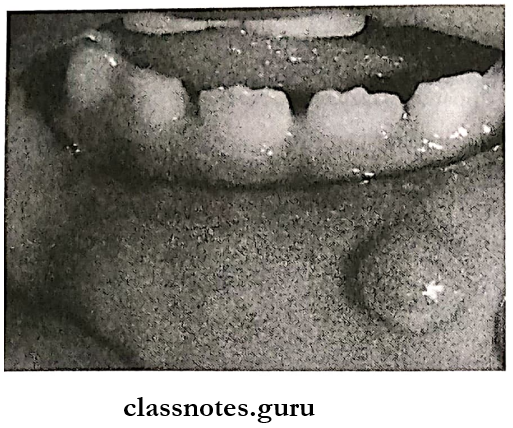
Question 4. Mucocele.
Answer:
Mucocele Description:
- Mucocele is a swelling caused by the accumulation of saliva at the site of a traumatized or obstructed minor salivary gland duct
Mucocele Types:
1. Extravasation:
- Extravasation is formed as a result of trauma to a minor sali¬vary gland excretory duct
- Extravasation is more common
- Extravasation does not have an epithelial cyst wall
2. Retention:
- Caused by obstruction by the calculus of duct
Mucocele Clinical Presentation:
- Site:
- Extravasation: lower lip is more common
- Other sites involve buccal mucosa, the tongue, the floor of the mouth, and the retromolar area
- Retention: palate or floor of the mouth
- Appearance:
- Discrete, painless, smooth-surface swelling
- Size:
- Ranges from a few millimeters to a few centimeters
- Color:
- Superficial lesions have a blue hue
- Deeper lesions can be more diffuse, covered by nor¬mal appearing mucosa without blue color
Mucocele Treatment:
- Surgical excision to prevent a recurrence
- Aspiration of fluid does not provide long-term benefit
- Surgical management may cause trauma to adjacent structures and can lead to the development of new lesions
- Intralesional injections of corticosteroids.
Question 5. Ranula
Answer:
Ranula
- A special type of mucocele
- Resembles the belly of a frog
Ranula Site:
- The floor of the mouth
- Superficial or deep to the mylohyoid muscle
Ranula Cause:
- Trauma to duct
Ranula Features:
- Slow-growing unilateral lesion
- Soft and freely movable
- Superficial lesions:
- Thin-walled bluish lesion
- Deeper lesions:
- Well circumscribed
- Covered by normal mucosa
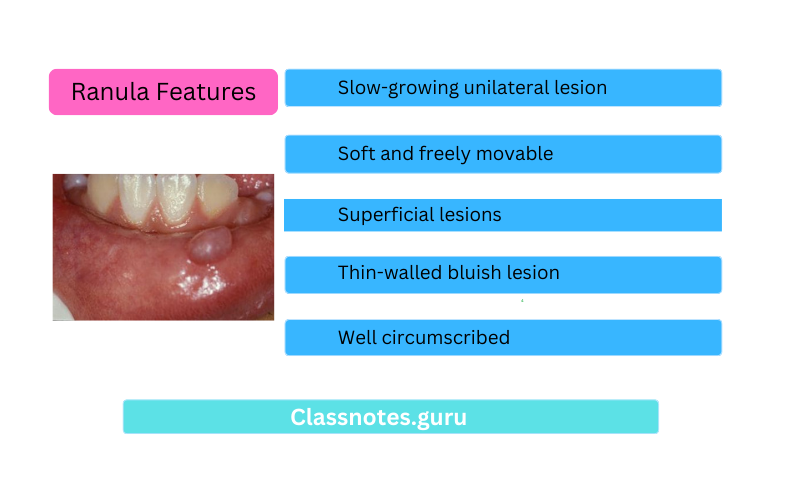
Ranula Types:
- Simple type
- Plunging ranula
Ranula Treatment:
- Marsupialization
Oral Medicine Salivary Glands Viva Voce
- Sialoliths are common in submandibular glands
- Mucous extravasation cysts are usually found on the lower lip
- Sialoadenosis is a noninflammatory disease
- Salt and pepper appearance is seen in Sjogren’s syndrome
- Pleomorphic adenoma is the most common parotid gland tumor
- Sjogren’s syndrome shows cherry blossom appearance in sialography
- In MRI, Sjogren’s syndrome shows salt and pepper appearance
- The Schimmer test is used for Sjogren’s syndrome
