Blood Important Notes
1. Heparin
- It is a powerful anticoagulant
- Effective both in vivo and vitro
- Present in all tissues containing mast cells
- In high doses, inhibits platelet aggregation and prolongs bleeding time
- Activates plasma antithrombin III
- This inactivates dotting factors of common and intrinsic pathways
- It does not cross the blood-brain barrier or placenta
- Thus it is safer during pregnancy
Blood MCQ questions and answers
Read And Learn More: Pharmacology Question and Answers
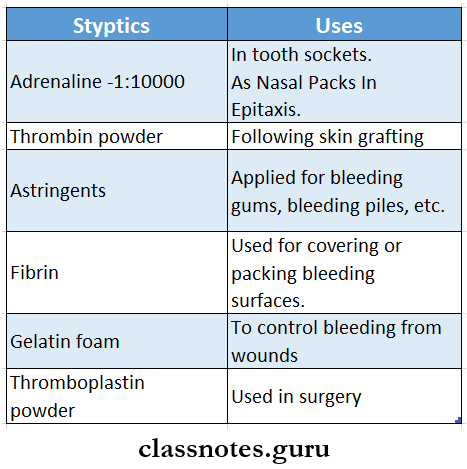
2. Styptics:
- They are local hemostatic agents
- Particularly effective on oozing surfaces
- Examples: thrombin, fibrin, gelatin foam, astringents like tannic add, vasoconstrictors like adrenaline
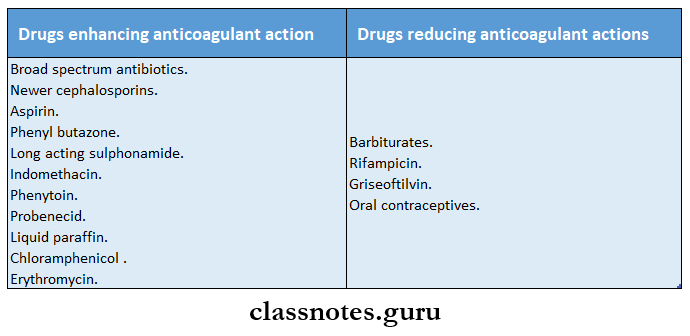
3. Drugs and anticoagulant action
4. Contraindications of vasoconstrictors
- Hypertension
- Hyperthyroidism
- Angina
- Patients receiving beta-blockers
- During anesthesia with halothane
3. Antiplatelet drugs
- Uses
- Coronary artery disease
- Cerebrovascular disease
- Coronary angioplasty, bypass implants
- Prosthetic heart valves
- Venous thromboembolism
- Peripheral vascular diseases
- Examples
- Aspirin
- Dipyridamole
- Ticlopidine
- Clopidogrel
- Abcbdmab
- Glycoprotein receptor antagonist
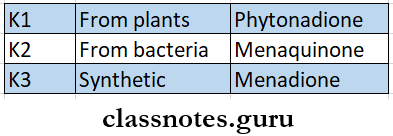
4. Vitamin K
5. Anticoagulants
- In vitro – Citrate, oxalate, EDTA
- In vivo – Coumarin, warfarin
- Both Vivo and vitro – heparin
6. Antifibrinolytics
- Epsilon amino Caproic acid
- Tranexamic acid
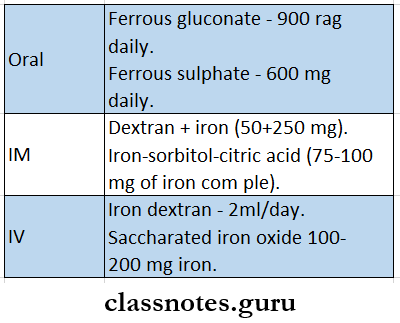
7. Iron preparation
8. Blood substitutes
- Blood products
- Whole blood
- Plasma
- Plasma proteins
- colloidal plasma substitutes
- Dextran
- Gelatin
- Fluid plasma substitutes
- 0.9% saline
- 5% dextrose
9. Daily dose of iron
- Adult male – 0.5-1 mg
- Adult female – 1-2 mg
- Pregnancy – 3-5 mg in the last two trimesters
10. Megaloblastic anemia
- Occurs due to deficiency of vitamin B12 or folic acid
- Treatment includes vitamin B12 + folic acid
- Folic acid given alone may worsen the neurological deficit
Blood short notes for nursing students
Blood Long Essays
Question 1. Explain the mechanism of iron absorption in the body. Add a note on different iron preparations
Answer:
Iron Absorption:
- Dietary iron is in the ferric form bound to proteins or organic acids
- The acidic medium of gastric juice releases this ferric ion
- Later it is converted to ferrous form by reducing substances like ascorbic acid and cysteine
- The ferrous form is soluble and is readily absorbed by mucosal cells
- It is oxidized to ferric form by ferroxidase
- This ferric form then combines with apoferritin and forms ferritin
- Iron from the mucosal cells may enter the bloodstream
- The ferric form is- Fe3+
- The ferrous form is Fe2+
- Gastric acid, reducing substances, and amino acids facilitate iron absorption
- Antacids, tetracyclines, phosphates, and phytates decrease iron absorption
Iron Preparations:
1. Oral iron preparations
It is the preferred route of administration
Oral iron Preparations:
- Ferrous sulfate -200 mg tab
- Contains 20% hydrated salt and 32% dried salt
- It is inexpensive
- Produces a metallic taste in the mouth
- Ferrous gluconate -300 mg tab
- Contains 12% of iron
- Causes less gastric irritation
- Ferrous fumarate -200 mg tab
- Contains 33% iron
- It is less water soluble and tasteless
- Ferrous succinate -100 mg tab, 35% iron
- Better absorbed and expensive
- Iron calcium complex -5% iron
- Better absorbed and expensive
- Ferric ammonium citrate -45 mg tab
- Better absorbed and expensive
Iron Dose:
- Total -200 mg given daily in 3 divided doses
- Prophylactic dose -30 mg daily
Iron Indications:
- Iron deficiency anemia
Iron Preparations Adverse Effects:
- Nausea, vomiting, epigastric pain
- Heartburn
- Staining of teeth
- Metallic taste
- Constipation
2. Parenteral iron preparations
- Intramuscular injection of iron is given deep in the gluteal region using the Z technique
- Intravenous is given slowly over 5-10 minutes
Blood long essay questions and answers
Parenteral Preparations:
- Iron dextran
- It is a colloidal solution containing 50 mg of elemental iron
- It is given intravenously and Intramuscularly
- Iron sorbitol citric acid complex
- Contains 50 mg of elemental iron
- Can be given only IM
- If given IV it quickly saturates transferrin stores
- Due to it free iron levels in the plasma rise and cause toxicity
Parenteral Dose:
- It is calculated using the formula:
- Iron requirement (in mg] = 4.4 * body weight (in kg) * Hb deficit (in g/dl)
Parenteral Indications:
- When oral iron is not tolerated
- Failure of absorption of oral iron
- Noncompliance
- In the presence of severe deficiency with chronic bleeding
- Along with erythropoietin
Parenteral Adverse Effects:
- Pain at the site of injection
- Pigmentation of skin
- Sterile abscess
- Fever
- Headache
- Joint pain, flushing, palpitation
- Chest pain, dyspnoea
- Anaphylactic reaction
2. Systemic agents
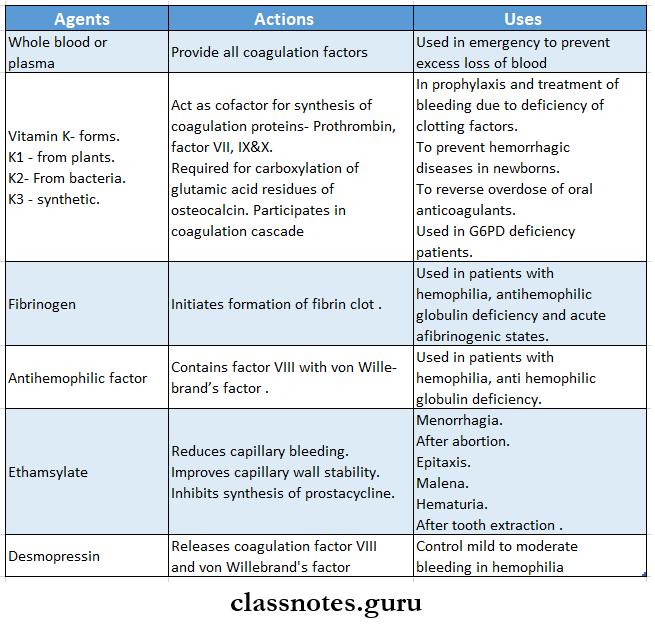
Question 2. Enumerate the agents used to control bleeding. Discuss their actions and uses.
Answer:
- Agents that help in controlling bleeding and are used in preventing or treating hemorrhagic conditions are known as coagulants
Control bleeding Classification:
1. Local agents or styptics
Control bleeding Actions:
- These materials provide a meshwork
- This activates the clotting mechanism and checks bleeding.
Question 3. Classify Anticoagulants. Discuss the mechanism of action, uses, and adverse effects of the coumarin derivatives.
Answer:
Anticoagulants:
- Anticoagulants are drugs used to reduce the coagulability of blood
Anticoagulants Classification:
- Used in vivo
1. Parenteral Anticoagulant
- Heparin, low molecular weight heparin, heparan sulfate
2. Oral Anticoagulants .
- Coumarin derivatives- Dicoumarol, warfarin, acenocoumarol, ethylbiscoumacetate
- Indandione derivative- Phenindione
- Used in vitro
1. Heparin
2. Calcium complexing agents
- Sodium citrate, sodium oxalate, sodium edetate.
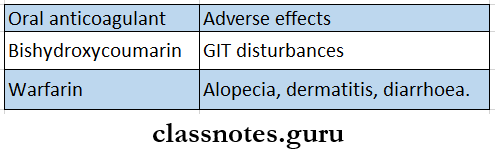
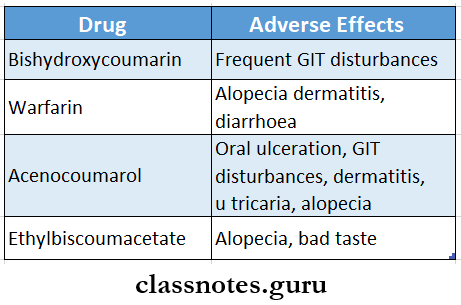
Anticoagulants Coumarin Derivatives:
- Coumarin derivatives are
- Bishydroxycoumarin- Dicoumarol
- Warfarin
- Acenocoumarol- nicoumalone
- Ethylbiscoumacetate
Anticoagulants Mechanism of Action:
- They act only in vivo
- They interfere with the synthesis of vitamin K-dependent clotting factors in liver
- Act as a competitive antagonist of vitamin K
- Reduces plasma levels of clotting factors
- Interferes with the regeneration of the active hydro, quinone form of vitamin K.
- Blocks the gamma-carboxylation of glutamate residues in prothrombin, factors VII, IX, and X
- This gamma-carboxylation is needed by these factors for coagulation
Anticoagulants Uses:
- Deep vein thrombosis and pulmonary embolism
- Myocardial infarction
- Unstable angina,
- Rheumatic heart disease, atrial fibrillation
- Vascular surgery, prosthetic heart valves, retinal vessel thrombosis, extracorporeal circulation, hemodialysis
Blood components questions and answers
Anticoagulants Adverse Effects:
- Bleeding- ecchymosis, epistaxis, hematuria, bleeding in the GIT, intracranial bleeding
- Gastrointestinal disturbances
- Teratogenicity
- Skin necrosis
Question 4. Classify styptics. Describe the role of vitamin K when bleeding is due to oral anticoagulant therapy.
Answer:
Styptics:
- Styptics are local hemostatic substances used to stop bleeding from a local approachable site
- Commonly used styptics are
- Thrombin
- Fibrin
- Oxidized cellulose
- Gelatin foam
- Adrenaline
- Astringents
Role of Vitamin K
- Oral Anticoagulants interfere with the synthesis of vitamin K-dependent clotting factors in liver
- Act as a competitive antagonist of vitamin K
- Reduces plasma levels of clotting factors
- Interferes with the regeneration of the active hydroquinone form of vitamin K.
- Blocks the gamma-carboxylation of glutamate residues in prothrombin, factors VII, IX, and X ‘
- This gamma-carboxylation is essential for the ability of the clotting factors to bind Ca ions and to get the bound phospholipid surface necessary for the coagulation sequence to proceed
- Vitamin K acts as an antidote for Warfarin
- Administration of vitamin K by competitive antagonism with oral Anticoagulants reduces the anticoagulant action and brings about carboxylation of glutamate residues of prothrombin and factor VII, IX, and X necessary for the coagulation sequence to proceed.
- Hence vitamin K is used for bleeding due to oral Anticoagulants
Physiology of blood questions
Question 5. Describe how heparin and dicumarol act as Anticoagulants. Indicate their route of administration, duration of action and name their antagonists.
Answer:
- Heparin
- It is a mucopolysaccharide found in the mast cells of the liver, lungs, and intestinal mucosa
Heparin Mechanism of Action:
- Heparin activates plasma antithrombin III
- Anti-thrombin III binds and inhibits activated Thrombin and coagulation factors Xa and IXa
- Heparin antithrombin III complex inhibits activated factor X and thrombin
- Low molecular weight heparin inhibits only factor X and not thrombin
Heparin Route of Administration:
- Heparin is given IV or SC
Heparin Duration of Action:
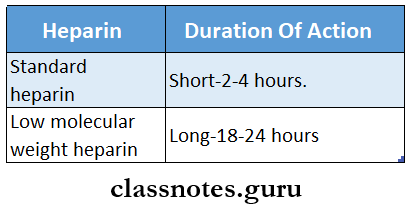
Heparin Antagonists:
- Protamine sulfate is an antagonist of heparin
- It is a low molecular-weight protein
- When given IV it neutralizes heparin
- It is used when heparin action needs to be terminated rapidly
- Dicoumarol:
- Dicoumarol is a Coumarin derivative
Dicoumarol Mechanism of Action:
- It interferes with the synthesis of vitamin K-dependent clotting factors in liver
- Act as a competitive antagonist of vitamin K
- Reduces plasma levels of clotting factors
- Interferes with the regeneration of the active hydro-quinone form of vitamin K
- Blocks the gamma-carboxylation of glutamate residues in prothrombin, factors VII, IX, and X
- This gamma-carboxylation is needed by these factors for coagulation
Dicoumarol Route of Administration:
- It is given orally
Dicoumarol Duration of Action:
- Duration of action -4-7 day
Dicoumarol Antagonists:
- Vitamin K acts as an antagonist for Dicoumarol
- Administration of vitamin K by competitive antagonism reduces the anticoagulant action and brings about carboxylation of glutamate residues of prothrombin and factor VII, IX, and X necessary for the coagulation sequence to proceed
Important questions on blood for BSc Nursing
Question 6. Explain in detail about pharmacological action, pharmacodynamics, therapeutic uses, and toxicity of heparin.
Answer:
Anticoagulants:
- Anticoagulants are drugs used to reduce the coagulability of blood
Heparin
- It is a mucopolysaccharide found in the mast cells of the liver, lungs, and intestinal mucosa
Heparin Pharmacological Actions:
1. Anticoagulants
- Heparin is a powerful anticoagulant
- It is effective in vivo and in vitro
- At low concentrations, it prolongs activated partial thromboplastin time
- At high concentrations, it prolongs prothrombin time as well as partial thromboplastin time
2. Antiplatelet action
- Heparin inhibits platelet aggregation
- this prolongs the bleeding time
3. Lipaemia clearing
- Heparin activates lipoprotein lipase
- This hydrolyses triglycerides present in the plasma and thus clears the plasma of lipids
Heparin Pharmacodynamics:
- Heparin activates plasma antithrombin III
- Anti-thrombin III binds and inhibits activated Thrombin and coagulation factors Xa and IXa
- Heparin antithrombin III complex inhibits activated factor X and thrombin
- Low molecular weight heparin inhibits only factor X and not thrombin
Heparin Uses:
Heparin Low molecular weight heparin is used in:
- Prophylaxis of deep vein thrombosis and pulmonary embolism
- Treatment of established deep vein thrombosis
- Unstable angina
- To maintain patency of cannula and shunts in dialysis patients
Heparin Toxicity:
- Bleeding
- Thrombocytopenia
- Osteoporosis
- Alopecia
- Hypersensitivity reactions
- Hypoaldosteronism
Blood Short Essays
Question 1. Cyanocobalamin
Answer:
Coenzyme Forms:
- 5′- Deoxyadenosyl cobalamin
- Methylcobalamin
Functions:
1. Synthesis of methionine from homocysteine
- Vitamin B12 is used as Methylcobalamin in this reaction
2. Isomerization of methyl malonyl CoA to succinyl CoA
- It occurs in the presence of vitamin B12 Coenzyme, deoxy adenosylcobalamin
Cyanocobalamin Dietary Requirements:
- Adults- 3 micrograms/day
- Children-0.5-1.5 microgram/day
- During pregnancy and lactation- 4 micrograms/day
Cyanocobalamin Uses:
- Prevention and treatment of B12 deficiency
- Mega doses used in neuropathies, psychiatric disorders, cutaneous sarcoid
Blood question bank with answers
Question 3. List two Anticoagulants acting by different mechanisms. Mention any two uses of them.
Answer:
- Heparin
- It is a mucopolysaccharide found in the mast cells of the liver, lungs, and intestinal mucosa
Heparin Mechanism of Action:
- Heparin activates plasma antithrombin III
- Anti-thrombin III binds and inhibits activated Thrombin and coagulation factors Xa and IXa
- Heparin antithrombin III complex inhibits activated factor X and thrombin
- Low molecular weight heparin inhibits only factor X and not thrombin
Heparin Uses:
Heparin Low molecular weight heparin is used in:
- Prophylaxis of deep vein thrombosis and pulmonary embolism
- Treatment of established deep vein thrombosis
- Unstable angina
- To maintain patency of cannula and shunts in dialysis patients
- Dicoumarol
- Dicoumarol is a Coumarin derivative
Dicoumarol Mechanism of Action:
- It interferes with the synthesis of vitamin K-dependent clotting factors in liver
- Act as a competitive antagonist of vitamin K
- Reduces plasma levels of clotting factors
- Interferes with the regeneration of the active hydro-quinone form of vitamin K.
- Blocks the gamma-carboxylation of glutamate residues in prothrombin, factors VII, IX, and X
- This gamma-carboxylation is needed by these factors for coagulation.
Dicoumarol Uses:
- Deep vein thrombosis and pulmonary embolism
- Myocardial infarction.
- Unstable angina.
- Rheumatic heart disease, atrial fibrillation
- Vascular surgery, prosthetic heart valves, retinal vessel thrombosis, extracorporeal circulation, hemodialysis
Question 4. Iron-sorbitol-citric acid
Answer:
- Iron sorbitol citric acid complex is parenteral iron preparation.
- Contains 50 mg of elemental iron
- Can be given only IM
- If given IV it quickly saturates transferrin stores
- Due to it free iron levels in the plasma rise and cause toxicity
Iron-sorbitol-citric acid Dose:
- It is calculated using the formula:
- Iron requirement ( in mg) = 4.4 * body weight (in kg) * Hb deficit (in g/dl)
Iron-sorbitol-citric acid Indications:
- When oral iron is not tolerated
- Failure of absorption of oral iron
- Noncompliance
- In the presence of severe deficiency with chronic bleeding
- Along with erythropoietin
Iron-sorbitol-citric acid Adverse Effects:
- Pain at the site of injection
- Pigmentation of skin
- Sterile abscess
- Fever
- Headache
- Joint pain, flushing, palpitation
- Chest pain, dyspnoea
- Anaphylactic reaction
Composition of blood short answer
Question 5. Anticoagulants
Answer:
- Anticoagulants are drugs used to reduce the coagulability of blood
Anticoagulants Classification:
- Used in vivo
1. Parenteral Anticoagulant
- Heparin, low molecular weight heparin, heparan sulfate
2. Oral Anticoagulants
- Coumarin derivatives- Dicoumarol, warfarin, acenocoumarol, ethylbiscoumacetate
- Indandione derivative- Phenindione
- Used in vitro
1. heparin
2. Calcium complexing agents
- Sodium citrate, sodium oxalate, sodium edetate.
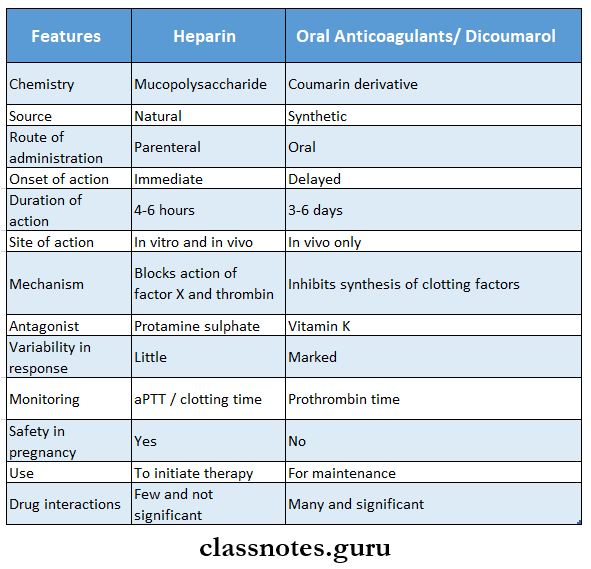
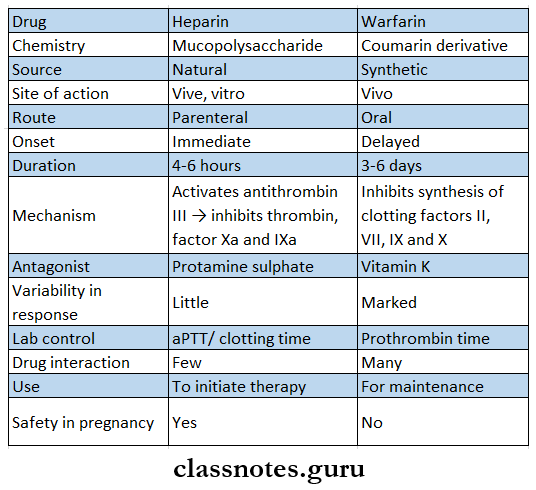
Question 6. Compare heparin and oral anticoagulants.
(or)
Compare heparin and dicumarol
Answer:
Question 7. Explain the mechanism of action of streptokinase and mention one use of it.
Answer:
Streptokinase:
- Streptokinase is a fibrinolytic drug
Streptokinase Mechanism of Action:
- Streptokinase is antigenic
- It combines with plasminogen to form tissue plasminogen activator complex
- This complex then causes limited proteolysis of other plasminogen molecules to plasmin
- Plasmin degrades fibrin thereby dissolving the clot
Streptokinase Uses:
- Acute Myocardial infarction
- Deep vein thrombosis
- Pulmonary embolism
Blood diseases questions for nursing
Question 8. Name two oral anticoagulants. Mention one drug treating toxicity of oral anticoagulants.
(or)
Dicumoral poisoning
Answer:
Oral Anticoagulants:
1. Coumarin derivatives- Dicoumarol, warfarin, acenocoumarol, ethylbiscoumacetate
2. Indandione derivative- Phenindione
Drug Used to Treat Toxicity of Oral Anticoagulants:
- Vitamin K is used to treat toxicity of oral anticoagulant
- Administration of vitamin K by competitive antagonism with oral Anticoagulants reduces the anticoagulant action and brings about carboxylation of glutamate residues of prothrombin and factor VII, IX, and X necessary for coagulation sequence to proceed
Question 9. Heparin and Warfarin.
Answer:
Blood Short Question And Answers
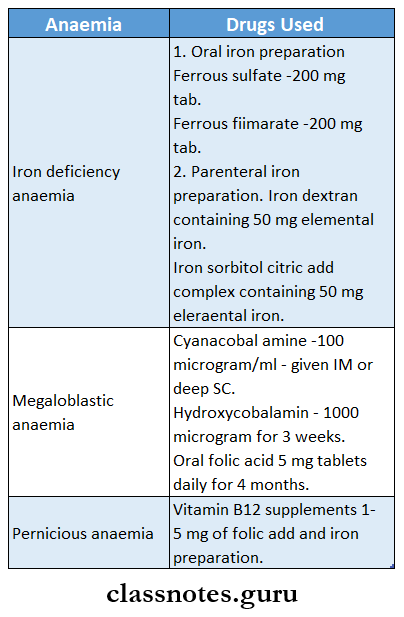
Question 1. Drugs for anemia.
Answer.
Question 2. Ferrous sulfate.
Answer:
Ferrous sulfate is oral iron preparation
Ferrous sulfate Dose:
- 200 mg tab, 3-4 tablets daily
Ferrous sulfate Indication:
- Prophylactic use in iron deficiency Anemia
Ferrous sulfate Adverse Effects:
- Nausea, vomiting, epigastric pain
- Heartburn
- Staining of teeth
- Metallic taste
- Constipation
Question 3. Folic acid
Answer:
Folic acid is important in one-carbon metabolism
Folic acid Sources:
- Green vegetables, liver, yeast, egg, milk, and some fruits
Folic acid Functions:
- The Coenzyme of it, tetrahydrofolate( THF], serves as an acceptor or donor of one carbon units
- It is involved in the synthesis of important compounds like
- Purines- Incorporated into DNA and RNA
- Pyrimidine nucleotide- deoxythymidylic acid- Involved in the synthesis of DNA
- Aminoacids- Glycine, serine, ethanolamine, and choline
- N-Formylmethionine- Initiator of protein biosynthesis
Folic acid Deficiency Manifestations:
- Megaloblastic anemia
- Glossitis
- Diarrhea
- Weakness
Blood group compatibility questions
Question 4. Drugs used in microcytic anemia.
Answer.
1. Oral iron preparation
- Ferrous sulfate-200 mg tab
- Ferrous fumarate -200 mg tab
2. Parenteral iron preparation
- Iron dextran containing 50 mg of elemental iron
- Iron sorbitol citric acid complex containing 50 mg of elemental iron
Question 5. Drugs used for pernicious anemia.
Answer:
- Vitamin B12 supplements
- 1-5 mg of folic acid and iron preparation
Question 8. Indications for parenteral use of iron.
Answer:
- When oral iron is not tolerated
- Failure of absorption of oral iron
- Noncompliance
- In the presence of severe deficiency with chronic bleeding
- Along with erythropoietin
Question 6. Mention two oral and parenteral preparations.
Answer:
Oral Preparations:
- Ferrous sulfate
- ferrous gluconate
- Ferrous fumarate
- Colloidal ferric hydroxide
Parenteral Preparations:
- Iron dextran
- Iron sorbitol citric acid complex
Question 7. Vitamin C is given with iron in the treatment of anemia.
Answer:
- Vitamin C Improves Absorption Of Iron In The Intestine
- It maintains ferrous salts in a reduced state
- So vitamin C is used in the treatment of anemia along with iron,
Question 8. Vitamin K deficiency.
Answer:
Causes of Vitamin K Deficiency:
- Liver diseases
- Obstructive jaundice
- Malabsorption
- Long-term antimicrobial therapy altering intestinal flora
Vitamin K Deficiency Manifestations:
- Bleeding tendencies- hematuria, GIT bleeding, epistaxis, ecchymosis
Question 9. Heparin
Answer:
- It is a mucopolysaccharide found in the mast cells of the liver, lungs, and intestinal mucosa
Heparin Uses:
- Low molecular weight heparin is used in:
- Prophylaxis of deep vein thrombosis and pulmonary embolism
- Treatment of established deep vein thrombosis
- Unstable angina
- To maintain patency of cannula and shunts in dialysis patients
Heparin Toxicity:
- Bleeding
- Thrombocytopenia
- Osteoporosis
- Alopecia
- Hypersensitivity reactions
- Hypoaldosteronism
Mechanism of blood clotting questions
Question 10. Vitamin K
Answer:
- It is a fat-soluble vitamin
Vitamin K Sources:
Vitamin K
1. Animals sources
- Egg yolk, meat, liver, cheese and dairy products
2. Plant sources
- Cabbage, cauliflower, tomatoes, alfa, spinach
Vitamin K Functions:
- It helps in blood coagulation
Vitamin K Daily Requirements:
- 70-140 micrograms/day
Question 11. Fibrinolytic
Answer:
- Fibrinolytic are drugs that lose the clot or thrombus by activating the natural fibrinolytic system
- Fibrinolytic agents are:
- Streptokinase
- Urokinase
- Alteplase
- Replace
- Tenecteplase
Fibrinolytic Uses:
- Acute Myocardial infarction
- Deep vein thrombosis
- Pulmonary embolism
Fibrinolytic Adverse Effects:
- Bleeding
- Hypotension
- Fever
- Anaphylactic reactions
Fibrinolytic Contraindications:
- In recent surgeries
- Injury
- GIT bleeding
- Stroke
- Severe hypertension
- Bleeding disorders
Question 12. Hemostasis
Answer:
- Hemostasis is the process of stopping bleeding postsurgically or from a site of injury
- It can be achieved by
- Applying pressure at the bleeding site
- Suturing
- Use of styptics
- It occurs by
- Contraction of the injured vessel wall
- Adhesion and aggregation of platelets to form a plug
- Formation of a blood clot
- Dissolution of the clot by fibrinolysis
Question 13. Warfarin sodium
Answer:
- It is a Coumarin derivative
Warfarin sodium Uses:
- Deep vein thrombosis and pulmonary embolism
- Myocardial infarction
- Unstable angina
- Rheumatic heart disease, atrial fibrillation
- Vascular surgery, prosthetic heart valves, retinal vessel thrombosis, extracorporeal circulation, hemodialysis
Warfarin sodium Adverse Effects:
- Bleeding- ecchymosis, epistaxis, hematuria, bleeding in the git, intracranial bleeding
- Gastrointestinal disturbances
- Teratogenicity
- Skin necrosis
Blood clotting cascade steps questions
Question 14. Oral anticoagulants
Answer:
- Oral anticoagulants are:
- Coumarin derivatives- Dicoumarol, warfarin, acenocoumarol, ethylbiscoumacetate
- Indandione derivative- Phenindione
Question 15. Uses of vitamin K
Answer:
- Act as a cofactor for the synthesis of coagulation proteins- Ffrothrombin, factor VII, IX, and X
- Required for carboxylation of glutamic acid residues of osteocalcin
- Participates in the coagulation cascade
Question 16. Vitamin K used in the overdosage of Warfarin
Answer:
- Warfarin interferes with the synthesis of vitamin K-dependent clotting factors in liver
- Act as a competitive antagonist of vitamin K
- Reduces plasma levels of clotting factors
- Interferes with the regeneration of the active hydro-quinone form of vitamin K
- Blocks the gamma-carboxylation of glutamate residues in prothrombin, factors VII, IX, and X v
- This gamma-carboxylation is essential for the ability of the clotting factors to bind Ca ions and to get the bound phospholipid surface necessary for the coagulation sequence to proceed
- Vitamin K acts as an antidote for Warfarin
- Administration of vitamin K by competitive antagonism with Warfarin reduces the anticoagulant action and brings about carboxylation of glutamate residues of prothrombin and factor VII, IX, and X necessary for the coagulation sequence ta proceed
Pulmonary and systemic circulation questions
Question 17. Adverse effects of vitamin B12.
Answer:
- Vitamin B12 is used
- In the treatment of vitamin B12 deficiency
- Cyanacobalamine -100 ml in. daily
- Hydroxocobalamin -100-500,1000 mg daily
- Multivitamins for oral use
- B12 deficiency – Prophylaxis 3-10 mg daily
- Treatment of megaloblastic anemia
- B12 neuropathies, psychiatric disorders, cutaneous sarcoid, and as a general tonic to allay fatigue and improve growth
vitamin B12 Adverse Effects:
- Anaphylactoid reaction on IV injection occurs due to sulfite contained in the formulation
Question 18. Name two oral anticoagulants. Mention two adverse effects.
Answer: